Oral health care in adult intensive care units: A national point prevalence study
Abstract
Background
The importance of good oral hygiene for patients in Intensive Care Units (ICUs) is well recognized, however, the most effective way to achieve good oral care in the ICU is unclear.
Aim
This study aimed to provide a national picture of oral care practices in adult ICUs in the United Kingdom (UK) to identify areas for improvement.
Study Design
A national one-day point prevalence study was undertaken in adult ICUs in the UK in the period from 30th September to 14th October 2021. Data were collected on all patients in the ICU on the date of data collection. Using a validated electronic data collection form, anonymised data were collected on methods and frequency of oral care provided, and the use of oral care protocols within the ICU. Data were analysed using descriptive analysis.
Results
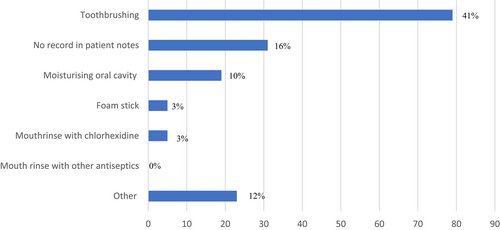
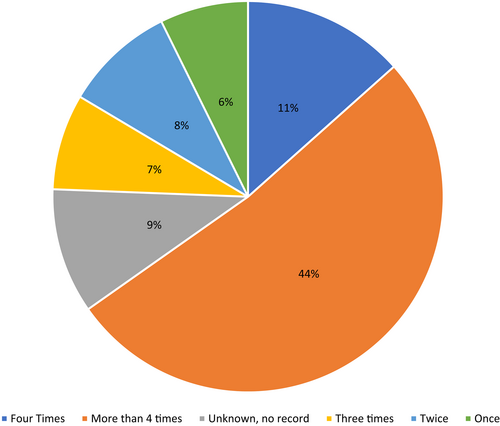
Data from 195 patients in 15 ICUs in England, Wales and Northern Ireland were collected. Written oral care protocols were available for use in the care of 65% (n = 127) of patients. 73% (n = 142) of patients received oral care within the 24-h period. Oral care methods included toothbrushing 41% (n = 79), foam sticks 3% (n = 5), moisturizing the oral cavity 10% (n = 19) and mouth rinse with chlorhexidine 3% (n = 5) and other oral care methods not specified 12% (n = 23). 44% (n = 85) of patients had an oral assessment within the 24-h period and variable assessment methods were used.
Conclusion
There is large variability in oral care provision and methods for intubated ICU patients and a lack of consensus was revealed in the study. Oral assessment is conducted less frequently using multiple tools. Optimal oral care standards and further research into oral care provision is pivotal to address this important patient-relevant practice.
Relevance to Clinical Practice
Oral care is a fundamental part of care for ICU patients, however, there is a large degree of variability, and oral care is often not based upon oral assessment. The use of an oral care protocol and oral assessments would help to improve patient care, ease of use for staff and provide a tailored oral care plan for patients, improving efficiency and preventing wasted resources.
What is known about the topic
- Oral heath frequently deteriorates on admission to ICU
- Oral care provision by ICU staff is fundamental.
- There is currently limited information on the gold standard of oral care for intubated patients in ICU
What this paper adds
- Provides a snapshot of oral care practices in a sample of UK ICUs.
- Reveals variability and lack of consensus on oral care practices and oral assessment methods in participating ICUs.
- Highlights the need for further research on oral care provision and its impact on patient outcomes in the ICU setting.
1 INTRODUCTION
The contribution of oral bacteria to pneumonia and respiratory infections is well known, with many studies showing a strong association between poor oral health and respiratory disease.1-4 The oral cavity hosts many bacterial species that co-exist in a complex bacterial biofilm known as dental plaque, which contributes to conditions associated with poor oral health such as caries and periodontal disease. Direct aspiration of oral bacteria into the lungs is a suggested mechanism by which oral bacteria may contribute to the development and progression of pneumonia.1 Recent studies have concluded that patients with good oral hygiene have a significantly lower risk of developing pneumonia,5 and good oral health is associated with a reduction in the risk of nosocomial pneumonia (NP) and ventilator-associated pneumonia (VAP), in high-risk patients.1
Oral health is an important aspect of overall patient care during hospital admission. Despite this, current evidence suggests that, throughout a patient's hospital stay, their oral health often deteriorates. Unfortunately, this is frequently the case in a critical care setting, particularly in patients who require mechanical ventilation.6 Due to prolonged mouth opening and reliance of ventilated patients on clinical staff to provide oral hygiene intervention and care, oral health can rapidly deteriorate, with plaque able to form within 48 h.7
Therefore, the importance of adequate oral care has been recognised in guideline interventions for the prevention of VAP.8 Different oral practices have been adopted for intubated patients, including toothbrushing and the use of oral care solutions, such as antiseptic mouthwash. However, the most effective way to achieve good oral care in the ICU is not known, and there is currently a lack of consensus.9 In a recent consensus paper, the British Association of Critical Care Nurses (BACCN) emphasized the importance of good oral care practice for the critically ill and provided guidance on different oral care practices for intubated and non-intubated patients.10, 11 A number of oral care protocols have been produced; however, most are not validated, or have been adapted for use in ICU from other hospital settings. There is also a large amount of variability and heterogeneity between protocols, related to a lack of consensus and evidence-based recommendations on the use of specific oral care practices that lead to differing oral care practices in ICUs across the UK.
Therefore, this study aimed to undertake a point prevalence study to provide a national picture of oral care practices in adult ICUs in the UK. This information would be useful for obtaining baseline current practice prior to producing and testing the effectiveness of a validated oral care protocol for use in the ICU.
The objectives of this point prevalence study were to determine the methods and frequency of oral care interventions, the oral assessment tools used, and whether an oral health assessment was carried out on admission and within the previous 24 h. We also aimed to gain insights into the scope and extent of the variations in practice.
2 METHODS
2.1 Study design
This was a national, prospective, observational 1-day point prevalence study of current oral care practices across UK ICUs. Anonymised data were collected over a 24-h period on a day that was suitable for the unit, within the data collection window (30th September–14th October 2021). All patients ≥18 years in ICU for the 24-h period were eligible; there were no exclusion criteria.
2.2 Study settings
This study was conducted in the United Kingdom where healthcare is predominantly delivered in a publicly funded system, the National Health Service. Within this system, critical care services are delivered in 300 specialist Intensive Care Units, which care for patients with single, and multiple organ failure or who require advanced respiratory support.12 Registered nurse to patient ratios are typically 1:1 or 1:2 depending on the patient's severity of illness.13 Standards of oral care across NHS Acute Trusts are informed by NHS Health Education England Mouth Care Matters Program.14 Data on the nature of the ICUs (medical, surgical or combination) were collected, but to preserve anonymity we did not collect data to identify the National Health Service Trusts that contributed to the study.
2.3 Recruitment
ICU nurses were recruited to participate in the study by collecting oral health audit data from ICU patient notes. Invitations to participate were distributed through the British Association of Critical Care Nurses (BACCN) and the Critical Care National Network Nurse Leads Forum (CC3N). A convenience sampling approach was adopted in which only nurses who agreed to participate were included. Nurses were provided with clear guidance and information on the study, including how to obtain local clinical governance approvals and how to complete and submit the data collection forms.
2.4 Study instrument
An electronic data collection form (Data S1) was designed. The form contained 14 items and data could be obtained from patients' notes. The items included methods and frequency of oral care provided and use of oral care protocols within ICU settings in the U.K. The face and content validity of the questionnaire was reviewed by an expert panel of six critical care nurse academics and clinicians who agreed on minor changes. In the period from 27th May to 14th June 2021, a pilot was conducted in five ICUs to report on the questionnaire's clarity, specificity, and comprehensiveness. Six ICU nurses trialled the data collection form. Five nurses agreed that the questionnaire included key questions related to oral care for intubated patients. One participant suggested the addition of medications to reduce secretions; however, this was not considered part of oral care and was therefore not included. All participants agreed that the tool did not miss any element of oral care related to intubated patients in the ICU. All participants reported that the tool enabled them to collect all the pertinent data. Two questions were reworded for clarity and the questionnaire was re-assessed before final distribution. The test and retest of the questionnaire showed no evidence of consistency and reliability.
2.5 Ethics statement
No participant identifiable data were collected in this study. Anonymous study codes were assigned in patient forms within the ICU. As this was a service evaluation project, National Research ethical approval was not required. Approval to undertake the study and share anonymized data with the research team was obtained from the Audit and Quality Improvement Departments of each participating National Health Service Trust.
2.6 Data collection
Nurses were instructed to collect data on oral care interventions performed over one 24-h period for all patients in their ICU during the period from 30th September to 14th October 2021. One nurse from each participating ICU was selected as the contact point for data collection and submission. Nurses were provided with detailed instructions sent as an attached word document, with invitations on how to access and fill in the electronic data collection form. The instruction sheet provided systematic instructions on how to complete and submit the forms. Oral care data, including the type and frequency of the intervention, were obtained from the patients' notes. The type and duration of intubation were also collected as variables in the study. The data were entered into an electronic data collection form. The form was hosted in a secure Google drive folder and clinical nurses collecting the data were provided with a link to the form.
2.7 Data analysis and management
Data were stored on password protected computers in Queen's University Belfast. Data were transferred to Microsoft Excel (Microsoft Corporation, WA, USA) and descriptive analyses were performed by one of the investigators (NK). The data were accessible to the research team only and were used only for the purpose of the study. Data were backed up automatically on a secure encrypted hard drive and will be stored for 10 years.
3 RESULTS
In total 15 out of 300 UK, ICUs participated and provided data for 195 patients. In England, data were obtained from 12 ICUs for 158 patients, in Northern Ireland from 1 ICU for 24 patients and in Wales from 2 ICUs for 14 patients. The study recruitment strategy relied on details of the study being seen on social media and disseminated by network leads to the individual ICU's. We cannot say with any degree of certainty how many individual ICU’'s actually received the study invitation and, therefore, it is impossible to calculate a precise recruitment rate. All the participating ICUs were mixed medical-surgical. Most patients received ventilation via oral endotracheal tube (94), tracheostomy tube,25 non-invasive ventilation mask,15 and type of ventilation not specified in (61). A total of 197 responses were recorded in total; however, 2 responses had no data recorded for any of the 14 questions included in the questionnaire so were excluded from analysis. 57% (n = 112) of patients did not wear dentures, 3% (n = 6) had full dentures (dental plate) and 2.6% (n = 5) had partial dentures (dental plate).
3.1 Provision of oral care
Within the 24-h study period, 73% (n = 142) of patients received oral care. Written oral care protocols were used in ICUs for 65% (n = 127) patients.
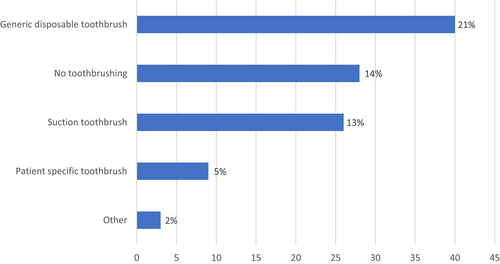
A range of oral care methods was employed, including toothbrushing 41%(n = 79) moisturizing the oral cavity 10% (n = 19), mouth rinse with chlorhexidine 3% (n = 5), foam sticks 3% (n = 5) and other oral care methods not specified 12% (n = 23) (Figure 1). The frequency of oral care carried out for patients also varied greatly between patients, ranging from once daily 6% (n = 12), twice 8% (n = 15), three times daily 7% (n = 13), four times 11% (n = 22) and greater than 4 times 44% (n = 85) (Figure 2). When toothbrushing was employed, a range of different tools were used including a generic disposable toothbrush 21% (n = 40), patient specific toothbrush 5% (n = 9) or suction toothbrush 13% (n = 26). For 14% (n = 28) of patients, toothbrushing was not carried out during the 24-h period (Figure 3).
Chlorhexidine preparations were used in 21% (n = 41) of patients. Preparations included chlorhexidine mouthwash 3% (n = 6) and chlorhexidine gel 12% (n = 24). In 6% (n = 11) patients, the Sage oral care system with Corinz® Antiseptic Cleansing and Moisturizing Oral Rinse was used (Table 1). The Sage oral care system for ventilated patients is a comprehensive oral care kit designed to help promote oral health and reduce the risk of developing respiratory complications for patients requiring ventilator support.15
| Chlorhexidine preparation | Frequency of use n, (%) |
|---|---|
| Not used | 111 (57%) |
| 1% Chlorhexidine gel | 24 (12%) |
| Sage oral care system (includes chlorhexidine) | 11 (6%) |
| 0.2% Chlorhexidine mouthwash | 6 (3%) |
| No record in notes | 3 (1.5%) |
3.2 Mouth assessment
Written oral care protocols for assessment were available for use in ICUs in 65% (n = 127) of cases. Mouth assessments were reported for 44% (n = 85) of patients within the previous 24 h. Mouth assessments were reported to have been undertaken on admission to ICU for 35% (n = 69) of patients. Assessment tools used included the Bedside oral exam 10% (n = 19),16 Beck oral care assessment 2% (n = 4),17 and Mouth care matters 13% (n = 25).14 Other assessment tools 5% (n = 9) included Trust-specific ICU assessments tool and the All-Wales Adult Mouth Assessment tool.18 Mouth assessment methods were not recorded in patients' notes in 29% (n = 57) of cases.
There was incomplete data recorded across 12 of the 14 questions included in the questionnaire. “No response” ranged from 1% to 39% across the 14 questions. The highest “no response” frequencies were recorded for “record of oral health assessment tool used” (39%), chlorhexidine mouthwash preparation used (21%), oral health care carried out in the last 24 h (20%), and product used for toothbrushing (28%).
4 DISCUSSION
In the ICU, intubated, mechanically ventilated patients' oral health tends to deteriorate with time.6 Patients are reliant on ICU staff to provide appropriate medical treatment, including mouth care. It is therefore important that ICU staff have the appropriate training, tools, and protocols to provide a high standard of care to maintain patients' oral health.
Although appropriate oral care is important to reduce the risk of infection, particularly for mechanically ventilated patients, the most effective way to achieve good oral care in ICUs is not known, as there is currently a lack of consensus. The data provided by this point prevalence study confirmed this and highlights the high level of variability in oral care practices and protocols utilized in ICU settings across the UK.
The BACCN consensus statement published in 2021,10 aims to provide advice and guidance, and to standardize oral care practices and provide information on the oral care practices required to prevent ventilator-associated pneumonia. As the data from the point prevalence study were also collected in 2021, the recommendations and guidance from the consensus paper may not yet have been adapted into ICUs across the UK, which may explain the deviation in oral care practices from evidence-based guidance.
Written oral care protocols were used for 65% (n = 127) of patients across UK ICUs sampled in this study, and these protocols differed across units, as evidenced by the results shown for oral care provision and assessment. The BACCN consensus group10 also acknowledge the numerous oral assessment tools available and state that although they could not endorse a specific oral care protocol for use, the use and internal validation of a written oral care protocol is fundamental for use in ICU.
It is recommended that ventilated patients should have their teeth brushed twice daily11, 19 and that oral cleansing and moisturizing the oral cavity should occur every 2–4 h.20, 21 However, findings from our study showed that only 41% (79) of patients included in the study had toothbrushing carried out in the 24-h period analysed. The other methods used for provision of oral care such as moisturizing of the oral cavity, use of foam stick and rinsing with chlorhexidine, although useful, are not a substitute for tooth brushing for removal of the plaque and ensuring optimal oral health. The BACCN consensus paper,10 advises that foam sticks should not be stored in liquid as this can affect the strength of attachment between foam and stick, which may represent a potential choking hazard. This may account for the variability noted regarding oral care instruments, between different ICUs across the UK.
Among mouthwashes used, chlorhexidine is the most widely reported antiseptic agent in ICU.22 Chlorhexidine preparations were used in 21% (n = 41) of patients in the current study. Several studies have highlighted the effectiveness of chlorhexidine in reducing complications such as VAP and mortality.23 The limited use of chlorhexidine reported in this study may be due to the fear of suspected increased mortality, previously reported by Klompas et al 201424 and Price et al 2014.25 More recent reports have, however, demonstrated safe use of this agent for ICU patients.23, 26 The 2020 Cochrane23 review “Oral care for critically ill patients to prevent ventilator associated pneumonia”, concluded that oral hygiene with chlorhexidine probably prevents VAP from developing in very ill patients in ICUs and that it probably has little or no effect on mortality or length of stay in ICUs. However, the review also concluded that although evidence suggests that the use of chlorhexidine use with toothbrushing is superior to toothbrushing alone, evidence is of low certainty and there is insufficient robust evidence. There is insufficient evidence to conclude if any of the oral care interventions investigated in the review are associated with adverse effects.23
A lack of consensus was also evident in relation to mouth assessment. An oral health assessment should be completed frequently as an integral part of patient assessment, to identify patients at risk of oral complications.27 Mouth assessments were only carried out in 59% (n = 115) of cases within the 24-h timeframe of assessment in the ICUs. Furthermore, only 35% (n = 69) of patients received mouth assessment, on admission to ICU. The BACCN Consensus statement10 states that an oral care assessment should be completed within 6 h of admission for all ventilated patients10 however, it is worth noting that the statement was published in 2021 and will require time to be fully filter through the units.
Oral care interventions should be based upon individual patient needs; therefore, a detailed mouth assessment should be carried out prior to provision of oral care to provide targeted and individualized oral care plans for patients.28 It is recognized that providing oral care for patients in ICU is challenging and time-consuming. Therefore, a mouth assessment prior to oral care provision may be beneficial both clinically and financially for ICUs.29
The current study highlighted a range of different assessment tools used, all of which have limited validity, as many of the assessment tools adapted for use in ICUs have not been validated. This highlights the need for an externally validated oral care protocol. Existing research also highlights the variability in oral care assessment tools employed between ICU settings, resulting in inconsistent assessments and incomplete documentation of care provided.28, 30
4.1 Strength and limitations
This study provided valuable information on the current oral care practices in ICUs in the UK but has some limitations. The study was a point prevalence study and only reported data within a 24-h period, rather than longitudinal data. Our data represents only a snapshot during the study period and cannot account for potentially influencing factors such as staffing levels. The data were incomplete for all the variables investigated, and some of the variables were not recorded in the patients' notes. We adopted a convenience sampling approach inviting nurses via their professional bodies and those who agreed to participate were included in the study. This results in contribution to the study from nurses in three of the UK nations and no contribution from Scotland. Therefore, the results of the study may not be generalized to all the ICUs in the UK. Furthermore, only 15 out of 300 ICUs in the UK participated in the study; however, there was a fair spread throughout and the ICUs included seemed fairly typical of ICUs around the country.
This study identified shortcomings in oral care, but not their causes and therefore future studies looking at nursing perspectives and perceptions to identify the causes and potential solutions to the issues identified are required. A further limitation was the potential for halo effect and bias. Fear of criticism or institutional censure may have affected objective reporting. We could also not rule out that variability in oral care methods may be related to severity of patients' conditions which was not identified in our survey.
The dissemination of the data collection instrument to ICUs across the UK may have provided a memoire aide for nurses promoting increased oral care practices. The data were also collected during the COVID pandemic, the effect of which we are unable to determine. Despite these limitations, we believe this survey provides a snapshot of oral care practices in ICUs in England, Wales, and Northern Ireland and identifies areas for improvement and future research.
4.2 Implications for Clinical Practice
This study has provided a snapshot picture of oral care practices in ICUs in England, Wales and N. Ireland, and demonstrated a degree of variability in practice. The data highlighted current practices and will help to guide areas for service improvements. These findings will be valuable for the design and implementation of future oral care protocols and to help design future observational and interventional studies.
5 CONCLUSIONS
In this small-point prevalence study, we identified variability in oral care regimes provided for patients and a lack of consensus on the written oral care protocols used. Variability and under reporting were observed for mouth assessment with only 35% of patients having had a mouth assessment on admission to ICU, thus indicating that oral care plans were not targeted or individualized. The impact of the current oral care practices and mouth assessment on outcomes for ventilated patients is not known. Further studies are warranted to investigate the effectiveness of standardized oral care practices based on oral health assessment.
ACKNOWLEDEGMENTS
The authors acknowledge the assistance of the British Association of Critical Care Nurses (BACCN) and Critical Care National Network Nurse Leads Forum (CC3N) in disseminating the online point prevalence questionnaire to ICUs in the UK. The authors were grateful for the help and support from all ICU staff and their supporting governance units for helping with the data collection for this study.
FUNDING INFORMATION
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interests to declare.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request. The data are not publicly available due to privacy or ethical restrictions.