A systematic review of the effect of early mobilisation on length of stay for adults in the intensive care unit
Abstract
Background
EM has been hypothesized to help prevent the development of ICU acquired weakness and may therefore result in positive outcomes for ICU patients.
Aim
To establish the impact of Early mobilisation (EM) on adult Intensive Care Unit (ICU) patients in terms of ICU length of stay (LOS), as well as hospital LOS, duration of mechanical ventilation, mortality, and functional independence.
Study design
A Systematic Review. EMBASE, MEDLINE, CINAHL, and the Cochrane Library were searched on 24th November 2020. Included studies and other systematic reviews were hand-searched for further includable studies. The primary outcome was ICU LOS whilst secondary outcomes were duration of MV, mortality, hospital LOS and functional independence. The PRISMA guidelines were utilized to perform the review. Ten randomized controlled trials with a combined total of 1291 patients met inclusion criteria and were scrutinized using the Joanna Briggs Institute (JBI) Checklist for Systematic Reviews. Revman 5.4.1 was used to conduct meta-analysis were possible.
Results
Results were limited by the evidence available for inclusion, in particular small sample sizes. However, a trend towards a shorter duration of ICU LOS and duration of mechanical ventilation emerged. There was also a trend towards higher rates of functional independence for intervention groups. Mortality rates appeared unaffected and results of meta-analysis were statistically non-significant (p = 0.90).
Conclusion
By applying a stricter time limit than previous systematic reviews a trend emerged that the commencement of EM has a positive effect on patient outcomes, in particular ICU LOS.
Relevance to clinical practice
The evidence base surrounding EM remains poor; however on the balance of the available evidence the application of EM should not be delayed.
What is known about the topic
- Evidence regarding the application of EM in ICU is mixed
What this paper adds
- The evidence base for the application of EM in ICU remains poor; however trends towards improved outcomes in terms of ICU LOS, Hospital LOS as well as duration of MV emerge from this review.
- Mortality rates are unaffected by EM.
- Disease severity may have an impact on the outcomes of EM.
1 INTRODUCTION
Early mobilisation (EM) has not been universally defined.1 Hodgson et al., (2013, p.1)12 defined it as: “the application of traditional modes of physiotherapy at an earlier stage than and delivered more regularly than conventional practice”.
EM has been hypothesized to prevent the development of Intensive Care Unit (ICU) acquired weakness (ICU-AW), and may therefore lead to improved patient outcomes both in terms of length of stay (LOS) and functional independence.18 ICU-AW is common among ICU survivors and many studies reported functional deficits, even five years post discharge.6, 8 In addition, a negative impact on family income was reported by 33% of all patients at 6 months and 28% at 12 months.18 ICU-AW can develop within 24 h of ICU admission and carries significant implications, both in terms of quality of life and cost.6, 8, 29 Passive exercise has been standard care in most ICUs; however, the implementation of EM has shown promising results.26
Several systematic reviews (SR) have explored the effectiveness of EM. Tipping et al. included 14 trials and concluded that activity limitations decreased and muscle strength increased for patients that received EM.31 However, a Cochrane review reported that evidence was too weak to draw any conclusions, but only included four randomized controlled trials (RCTs), due to their stricter inclusion criteria.3 Zhang et al. reviewed 23 trials and concluded that EM reduces the duration of mechanical ventilation (MV) and incidence of ICU-AW, and leads to improvements in physical function.34 However, they advised caution when interpreting results due to the mixed quality of the available evidence.34 Wang et al. included 39 RCTs and showed that EM does not affect mortality rates but significantly reduces rates of pressure sores and deep vein thrombosis.33 They did not impose a language limit and were able to include a large number of non-English publications, particularly from China.33 Their results were limited by high levels of heterogeneity.33
A SR of 48 publications and 7546 patients established that EM is safe, even when patients are fully ventilated.22 Ding et al. conducted a SR on the optimum time for enrolment to EM protocols and found that enrolment within 48–72 h was likely to be most effective at reducing ICU-AW.2
The overall evidence, to date, is weak, due to the underpowered nature of included trials, high heterogeneity and the fact that previous SRs did not apply a time limit on enrolment time.31, 33, 34 A SR by Ding et al. analysed the optimum time for initiation of EM and found that initiation within 48–72 h was optimal.2 However previous SRs on EM included studies with late interventions, for example, both Tipping et al. and Zhang et al. included The trial by Moss et al., where patients did not receive their first intervention until day eight of ICU admission.21, 31, 34 While this is likely worthwhile in its own right, it cannot be considered “early” in the strictest sense of the word. The Inclusion of these studies may have skewed results for Tipping et al. and Zhang et al.31, 34 The present review, therefore, aims to apply more stringent inclusion criteria and different outcome measures to previous reviews, and will, therefore, contribute to a deeper understanding of the effects of EM on adult ICU patients, thereby informing future research and clinical practice. In particular, this review will use a strict limit on enrolment time.
2 AIMS
This SR aims to establish the effect of EM in adult ICU patients on ICU LOS. The primary outcome measure will be ICU LOS, followed by the duration of MV, hospital LOS, mortality, and functional independence.
3 METHODS
- Population: Adult ICU patients.
- Intervention: Any form of EM that promotes active exercise
- Comparison: Normal care or no EM intervention
- Primary outcome measure: ICU LOS
-
Secondary outcome measures:
- Duration of MV
- Mortality
- Hospital LOS
- Functional independence
Research Question:
What is the effect of early mobilisation on the length of stay of adults in the ICU?
3.1 Criteria for inclusion and exclusion
To be included in this SR, studies had to be RCTs and utilize early and active mobilisation on critically ill adult patients. Studies had to be published in English and report ICU LOS. Lastly, they had to enrol their patients within 4 days of admission or intubation.
Non-RCT studies were excluded, as were passive exercise only regimes, or studies that focused on post ICU-discharge interventions. Studies that did not report on ICU LOS were also excluded. Furthermore, studies utilizing cycle ergometry as their only intervention were also excluded. Tipping et al. excluded cycle ergometry while Zhang et al. included it. For this work, the argument presented by Tipping et al. was followed; cycle ergometry on its own cannot be considered as EM, as it does not involve the same complexities as the active mobilisation of ICU patients.31, 34
3.2 Search strategy
Searches were carried out on December 31, 2021. CINAHL, MEDLINE, EMBASE, and the Cochrane Database were searched. Searches were limited to human, adult and RCT studies published in English. For CINAHL the following Medical Subject Heading (MeSH) terms were used: rehabilitation, early ambulation, physical therapy specialty, and critical care. For MEDLINE and EMBASE the following Emtree terms were used: mobilisation, rehabilitation, intensive care, and randomized controlled trial. For Cochrane, the terms early mobilisation and ICU were utilized. Boolean operators were used in conjunction with the selected search terms. Both search terms and Boolean operators were verified with a second reviewer.
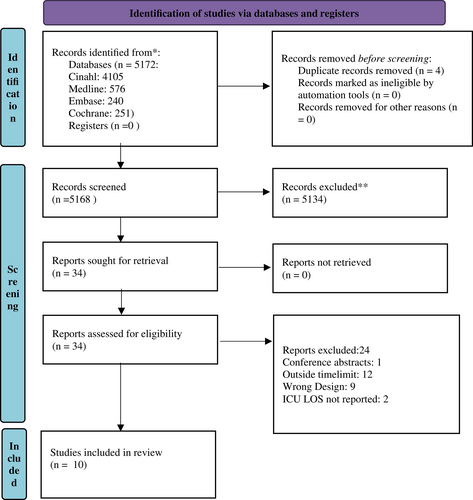
Reference lists of included studies and SRs on the topic were hand-searched. Search Results were recorded in the Preferred Reporting of Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart.23 Please see Data S1 for details of searches and results
3.3 Data collection and extraction
A data extraction table was utilized to extract all necessary data to complete the review. The Data extraction table contains summary information for each article, patient characteristics, the nature of the utilized EM protocol, and data as regards the primary and secondary outcome measures. Electronic databases were searched to retrieve studies in accordance with the eligibility criteria outlined above. Then the data were extracted by one reviewer and validated by a second reviewer.
3.4 Quality appraisal
The Joanna Briggs Institute (JBI) Checklist for Randomized Controlled Trials Tool was used to assess for bias in the included studies.14
3.5 Data analysis
Meta-analysis was performed with the Review Manager 5.4.1.30 Continuous variables were presented as Standard Mean Difference, while dichotomous variables were expressed as risk ratios. Results of comparable trials were pooled using the fixed-effect or random effect model and 95% confidence intervals. Heterogeneity was investigated by calculating the I2.9 A funnel plot to test for publication bias should only be used when there are at least 10 studies included in the meta-analysis,10 therefore we did not assess the publication bias.
Continuous data, not presented as a mean and standard deviation (SD), were not mathematically converted due to correspondence with authors and examination of articles, confirming that the data were not normally distributed.7, 16, 19 Therefore, it was not suitable for mathematical conversion to mean and SD.32 A narrative synthesis was adopted for data that was unsuitable for meta-analysis. For data reported as median and interquartile range (IQR), bar charts were prepared to express the difference in median days between intervention and control groups for ICU LOS, hospital LOS, and duration of MV.
4 RESULTS
4.1 Search results
The searches yielded 5172 articles. 5134 articles were excluded based on title, or abstract. 34 full text articles were assesed, 10 of which were suitable for inclusion, based on the inclusion and exclusion criteria. See Figure 1 PRISMA flow diagram, summarizing the search outcomes. The most common reason for exclusion on full-text review was enrolment time after 4 days of ICU admission or intubation.
4.2 Study characteristics
Ten RCTs enrolling a total of 1291 patients were included in this review. Study sizes ranged from 4017 to 300.20 Four studies were set in general mixed ICUs,4, 11, 25, 27 three in medical ICUs,13, 20, 28 and the remaining three in surgical ICUs.17, 24, 26 The three surgical RCTs varied considerably in their settings. Maffei et al. performed their trial in a liver transplant unit, while Schaller et al. included a wide variety of surgical specialties. Patman et al. on the other hand included cardiac surgery patients only.17, 24, 26 The included studies were set in nine different countries on four continents. See Table 1 for the summary of characteristics.
| Study | Patients main diagnosis, if specified | Sample size | Mean APACHE IIa | Country | Age | Percentage female | Type of intervention |
|---|---|---|---|---|---|---|---|
| Schujmann et al.27 | General (mixed) | 135 | Brazil | 51c | 37% | Progressive mobilisation regime | |
| Eggmann et al.4 | General (mixed) | 115 | 22 | Switzerland | 64c | 41% | Progressive mobilisation regime |
| Santos et al.25 | General (mixed) | 51 | 15.9 | Brazil | 53c | 32% | 1 physiotherapy session/day |
| Maffei et al.17 | Liver transplant | 40 | France | 53c | 22.5% | 2 physiotherapy sessions/day | |
| Morris et al.20 | Respiratory | 300 | 18b | USA | 56c | 55% | 3 physiotherapy sessions/day |
| Hodgson et al.11 | General (mixed) | 50 | 18 | Australia, New Zealand | 61c | 40% | Progressive mobilisation regime |
| Schaller et al.26 | Surgical (mixed) | 200 | 20 | Austria, Germany, USA | 65d | 47% | Progressive mobilisation regime |
| Dong et al.13 | Medical | 60 | 15 | China | 55c | 31% | Progressive mobilisation regime |
| Schweickert et al.28 | Medical | 104 | 19 | USA | 56d | 50% | Progressive mobilisation regime |
| Patman et al.24 | Cardiac surgery | 236 | Australia | 63c | 22% | 1 physiotherapy session/day |
- a Acute Physiology and Chronic Health Evaluation II (APACHE II).
- b proportionally converted from APACHE III.
- c Mean.
- d Median.
4.3 Nature of interventions
Seven of the included RCTs utilized progressive mobilisation regime that generally involved a stepwise approach: gradually building up the duration and level of the exercises.4, 11, 17, 26-28 The remaining three studies increased the amount of physiotherapy in comparison to the control group, without following a stepwise mobilisation program.20, 24, 25 Furthermore, Santos et al. divided their intervention groups into an EM group called EX, and a group that received neuromuscular stimulation in addition to the EM protocol called NMES+EX.25 These subgroups have been listed separately for the purpose of the meta-analysis. Neuromuscular stimulation was also part of the EM interventions in Schujmann et al.27
5 PRIMARY OUTCOMES
5.1 ICU LOS
Four of the included studies reported their ICU LOS suitably for meta-analysis.13, 17, 24, 25 The results for Santos et al. were split into two different subgroups of EM.25 The meta-analysis indicated a benefit for intervention groups, but results were statistically non-significant with high heterogeneity of I2 = 53% (Figure 2).
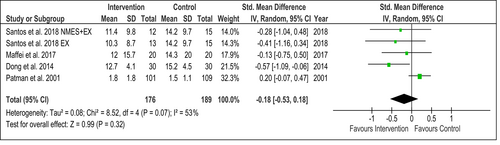
Patman et al. was the only trial to report an increase in ICU LOS, although this was by 0.3 mean days and statistically not significant (p = 0.56).24 Maffei et al. reported a reduction by 2.3 mean days (p = 0.690), while Santos et al. reported a reduction by 2.8 mean days for the NMES+EX group and 3.9 mean days for the EX group (p = 0.03).17, 25 Dong et al. also reported a reduction of ICU LOS by 2.5 mean days (p = 0.01).13
The remaining six studies reported results in median days with IQR ranges. All studies reported a reduced ICU LOS for intervention groups. Morris et al. (p = 0.68) and Eggmann et al. (p = 0.595) both reported a reduction by 0.5 median days, Schweickert et al. (p = 0.08) and Hodgson et al. (p = 0.28) reported a reduction by 2 median days, and Schujmann et al. (p = 0.003) and Schaller et al. (p = 0.0054) reported a reduction by 3 median days (Figure S1).4, 11, 20, 26-28
However, of the ten included studies only Dong et al., Schaller et al. and Schujmann et al.'s results were statistically significant.13, 26, 27
All trials, aside from Patman et al. reported reductions of ICU LOS.24 In Dong et al., Schaller et al. and Schujmann et al. these reductions were statistically significant.13, 26, 27
6 SECONDARY OUTCOMES
6.1 Mortality
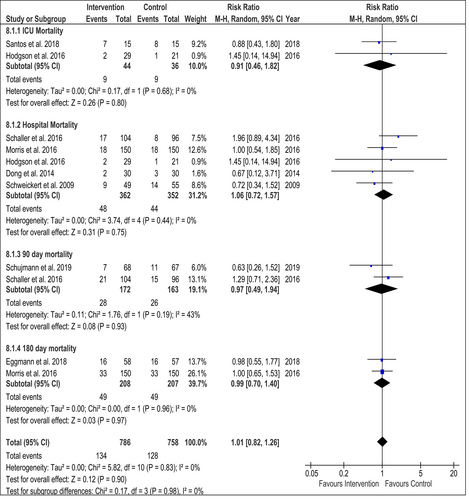
All included studies reported mortality rates; however, endpoints for reporting varied from ICU mortality to 180 day mortality. In Figure 3, mortality has been meta-analysed according to the specific endpoints. Overall during the meta-analysis, a Risk Ratio of 1.01 (95% CI 0.82–1.26) was calculated, indicating that EM does not affect mortality rates. I2 of 0% indicates that there is no variability due to heterogeneity. However, results were not statistically significant for the overall calculation, nor various endpoints.
6.2 Hospital LOS
Hospital LOS was reported by eight studies. Only Patman et al. and Maffei et al. reported their data suitably for meta-analysis (Figure S2).17, 24 Results favoured intervention treatment but were not statistically significant (p = 0.53). There was no heterogeneity (I2 = 0%).
Of the remaining six trials, Eggmann et al. and Schweickert et al. reported an increase of 3.9 (p = 0.723) and 0.6 (p = 0.93) median days on Hospital LOS. Morris et al. reported no difference in terms of Hospital LOS (p = 0.41).4, 20, 28 The other three trials all reported reduced Hospital LOS for intervention groups. Schujmann et al. reported a reduction of 3 median days (p = 0.1), Hodgson et al. reported a reduction by 10 median days (p = 0.33) and Schaller et al. reported a reduction of 6.5 median days (p = 0.011) (Figure S3).11, 26, 27
Overall, only Morris et al. showed no difference in Hospital LOS; Eggmann et al. and Schweickert et al. reported an increase, while five trials reported a reduced Hospital LOS.4, 11, 17, 20, 24, 26-28
6.3 Duration of mechanical ventilation
Seven trials reported duration of MV, of which four were suitable for inclusion into meta-analysis. Santos et al.'s data for the two different EM groups were included separately.25
Results of the meta-analysis show a statistically significant reduction of duration of MV in intervention groups (p = 0.0002). However heterogeneity among studies was very high (I2 = 82%) (Figure S4).
Of the three studies not suitable for inclusion into the meta-analysis, Eggmann et al. was the only one to report a negative effect of 0.4 median days (p = 0.83).4 In contrast Hodgson et al. reported a reduction of 1.6 median days (p = 0.18) and Schweickert et al. reported a statistically significant reduction of 2.7 median days (p = 0.02) (Figure S5).11, 28
Of the studies reporting mean results, Patman et al. reported no difference (p = 0.85), Dong et al. reported a shortened duration of MV by 1.7 mean days which was statistically significant (p = 0.005), and Maffei et al. reported an improvement of 0.8 mean days (p = 0.104).13, 17, 24 Santos et al. reported a shortening of 4.7 mean days for their EX group and a shortening of 9.1 mean days when compared to the control group; the latter result was statistically significant (p = 0.007).25
Overall, of the seven trials reporting on duration of MV, Eggmann et al. reported a longer duration of MV, Patman et al. reported no difference and the remaining five trials reported shorter duration of MV.4, 11, 13, 17, 24, 25, 28 Results for duration of MV found Santos et al. results for NMES+EX group, Dong et al. and Schweickert et al. to be statistically significant.13, 25, 28
6.4 Effect on functional independence
Of the included studies, two did not report on physical function outcomes.24, 25
Maffei et al. reported a trend for walking earlier (p ≥ 0.99), but did not report on performance at discharge.17 Similarly, Dong et al. reported that the intervention group was earlier to mobilise out of bed (p = 0.0), but reported no other functional outcomes.13
The effect of EM on functional independence was reported differently among the various studies. Schujmann et al. reported that at 3 months, 97.5% of the intervention group were functionally independent, while only 74.4% of the control group had achieved functional independence.27 This result was statistically significant (p = 0.003).
Eggmann et al. reported no functional benefits for the intervention group, but a trend towards better mental health was noted.4 Morris et al. initially reported no difference in terms of physical function.20 However, at 6 months follow up, they reported a statistically significant improvement in their Short Form (36) Health Survey (SF-36) score (p = 0.023).
Hodgson et al. reported that mobility milestones were achieved earlier by members of the intervention group, however, at 6 months there was no difference in terms of physical function between groups.11
Schaller et al. reported that 51% of the intervention group and 25% of the control group were functionally independent at hospital discharge, the difference between groups was statistically significant (p = 0.009).26 Furthermore, 61% of the intervention group were able to be discharged home directly, compared with 30% in the control group.26 This was also statistically significant (p = 0.0007).26
Schweickert et al. reported that 59% of the intervention group and 35% of the control group returned to their normal functional status at hospital discharge, the difference between groups was statistically significant (p = 0.02).28
Overall, of the six studies that reported on functional independence, Eggmann et al.'s was the only one that did not show any improvements.4 Hodgson et al. showed earlier achievement of mobility milestones, but this had balanced out again at six months.11
The remaining four studies all showed statistically significant improvements in physical independence at their individual endpoints.20, 26-28
See Table 2 for a summary of the effects of EM on functional independence.
| Effect on physical function | |
|---|---|
| Schujmann et al.27 | No difference in handgrip strength. In EM group better performance for sit to stand and 2-minand ^# walk test. Also more likely to be physically independent. At 3 months 97.5% versus 74.4% functionally independent (p = 0.003). |
| Eggmann et al.4 | No functional benefits found. SF-36 at 6 months no difference Trend towards better mental health for intervention group noted. |
| Santos et al.25 | Not reported. |
| Maffei et al.17 | In EM group trend for walking earlier, but no report on how performance compared at discharge. |
| Hodgson et al.11 | Mobility milestones achieved earlier for intervention group, however at 6 months there was no difference in terms of physical function between groups. |
| Morris et al.20 | No difference in physical function initially, but at 6 months SF-36 significantly better for EM group (p = 0.001). |
| Schaller et al.26 | Significant 51% EM versus 25% non-EM functionally independent at hospital discharge (p = 0.009). 61% EM versus 30% non-EM discharged home (p = 0.0007). No significant difference of SF-36. |
| Dong et al.13 | Earlier to get out of bed, but nil else reported. |
| Schweickert et al.28 | 59% versus 35% returned to functional normal status at hospital discharge (p = 0.02). |
| Patman et al.24 | Not reported. |
6.5 Results of quality appraisal
Quality appraisal results are presented in Figure 4. Findings were validated by a second reviewer. All studies suffered from performance bias, as personnel were unable to be blinded due to the nature of the intervention.4, 11, 17, 20, 24-28 Three of the included studies suffered from four sources of bias.13, 17, 24 Two studies suffered from three sources of bias,20, 27 while the remaining trials suffered from two or one source of bias.4, 11, 25, 26, 28
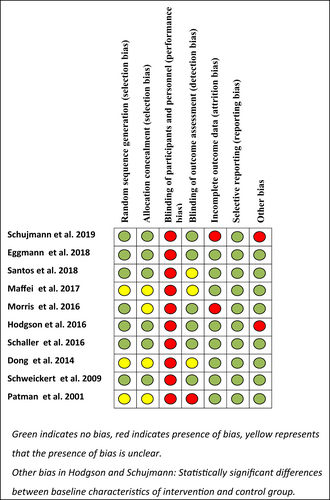
The other sources of Bias highlighted in the diagram are the statistically significant differences between baseline characteristics of intervention and control groups.11, 27 Overall, while the analysis did reveal moderate bias, with blinding being the main issue, it was decided to include all studies.
7 DISCUSSION
This review focused on EM in the strictest sense of the definition by only including trials that enrolled their patients within 4 days of ICU admission or intubation and by also excluding passive exercise regimes. Therefore, the results from this review differ from previous SRs.
From data analysed, a trend emerged towards reductions in ICU LOS, with only Patman et al. reporting an increase in ICU LOS.24 Unfortunately, not all studies could be included in the meta-analysis due to abnormal distribution of the data.
EM did not appear to have an effect on mortality, as the results of the meta-analysis were statistically non-significant. Reporting on functional independence was diverse, yet a majority of studies also showed improved outcomes for intervention groups. Similarly, there was a trend towards a reduction in duration of MV.
The data was less clear around Hospital LOS, but there was a trend towards improved outcomes. Interestingly, two studies reported a reduction of ICU LOS, but an increase in Hospital LOS.20, 25
The level of baseline PT varied among studies. Schweickert et al. and Patman et al. were the only ones without baseline PT.24, 28 All other trials included some level of PT at baseline.4, 11, 13, 17, 20, 25-27
It is noteworthy that Eggmann et al. was the only study that reported several disadvantageous results for their intervention groups.4 There are likely a number of reasons for this. Firstly, the mean APACHE II score of their participants was 22, which is the highest of any included trial. The disease severity of included patients was therefore higher. The level of baseline physiotherapy (PT) was also high with the control group receiving EM as part of the standard care. In the intervention group, resistance training was introduced as well as motor-assisted, or active in bed cycling. Overall, PT time increased from once a day, mostly on weekdays to up to three times a day, seven days a week. It is therefore likely that the high level of baseline PT combined with the level of disease severity led to fewer positive results when compared to other included studies.
Similar to this review, Tipping et al. found no difference in mortality, yet unlike this SR Tipping et al. showed no difference in functional outcomes.31 They were unable to analyse LOS and duration of MV due to the skewed nature of their data.
Wang et al. were able to show significance for their mortality data, but their meta-analysis on ICU LOS, hospital LOS and duration of MV suffered from high heterogeneity.33
Unlike this review, Zhang et al. reported that EM had no impact on duration of MV.34 Similar to the findings of this review, they also reported that EM improved rates of functional independence.
Doiron et al. did not draw any conclusions due to the poor quality of the four included studies.3
In the discussion of their trial, Schaller et al. proposed that disease severity may have an impact on outcomes.26 To explore this, outcomes were plotted against the APACHE score. The APACHE II score was thereby utilized to assess disease severity. The APACHE score was designed to predict mortality and disease severity on ICU admission.15
Six studies reported APACHE II scores.4, 11, 13, 25, 26, 28 Morris et al. reported APACHE III scores. Their APACHE III score was converted proportionally into an APACHE II score. APACHE scores were plotted in a graph against difference in ICU and Hospital LOS, as well as the difference in duration of MV in median days. Two RCTs could not be included in this plot as they did not report their patient outcomes in median values.13, 25 Schaller et al. and Schweickert et al. reported their APACHE score as median scores.26, 28 Their scores were converted to mean values using the method of Wan et al.32 Therefore, five studies encompassing 769 patients were included in the graphs.4, 11, 20, 26, 28 See Figures S6, S7 and S8 for results.
The trend lines strongly indicate more favourable outcomes for patients with lower disease severity for Hospital LOS, ICU LOS as well as duration of MV.
Overall, there appears to be a trend towards improved response to EM from patients with lower diseases severity, the analysis was limited as only 5 studies enrolling 769 patients were included. In addition, it is likely that other factors including age profile, admission diagnosis and EM protocols have an effect on patient outcomes.
However, it will be worthwhile to conduct further analysis on the impact of disease severity, once larger trials have been released.
7.1 Limitations
This SR was limited by research available for inclusion. Numbers in the individual trials were small and therefore results were mostly statistically non-significant.
Quality appraisal identified numerous sources of bias, thereby limiting the quality of the included data. Blinding of personnel and patients is impossible due to the nature of interventions; therefore performance bias cannot be excluded. However, further sources of bias were present in most studies.
The description of interventions was extremely brief in one study.24 The remaining nine RCTs provided a reasonable level of detail regarding their interventions; however, only three studies provided enough detail to allow for the application of their study protocol, based on the information provided within their articles.4, 11, 27
7.2 Future direction and Implications for clinical practice
At least one large, well-designed RCT is required to gain certainty of the effectiveness of EM. However, enrolling sufficient numbers for EM trials is difficult. Therefore, it may be several years until strong evidence will be available.
In their extensive review on the safety of EM, Nydahl et al. concluded that EM is safe.22 Furthermore, this SR indicates that EM has no effect on mortality. Other findings include a trend towards shorter ICU and Hospital LOS for patients undergoing EM, as well as a reduction of ventilator time for intervention groups. Further research is required to solidify findings; however, this review shows that no evidence of harm is assocated with EM and therefore the application of EM in ICU settings should not be delayed.
8 CONCLUSION
This review has applied stricter time limits than previous SRs for the commencement of EM protocols, as patients had to be enrolled within four days of ICU admission or intubation. The emerging results give a strong indication that the commencement of EM has a positive effect on ICU LOS. In addition, there is a trend towards improved outcomes for Hospital LOS, duration of MV, and increased functional independence, than was the case with previous SRs. EM remains a safe intervention and does not influence mortality rates. However, findings are limited by small sample sizes and sources of bias. Further research and large-scale trials are required to solidify findings. However, based on the evidence of this SR, the application of EM should be widely considered in ICU settings, as ongoing RCTs will likely require years to complete.
AUTHOR CONTRIBUTIONS
Jonas Monsees: Conceptualization (lead), Formal Analysis, Investigation (lead), Methodology (lead), Writing – Original Draft Preparation (lead), Writing – Review & Editing (lead); Zena Moore: Methodology (equal), Writing – Original Draft Preparation (equal); Declan Patton: Methodology (equal), Writing – Original Draft Preparation (equal); Chanel Watson: Methodology (equal), Writing – Original Draft Preparation (equal); Linda Nugent: Methodology (equal), Writing – Original Draft Preparation (equal); Pinar Avsar: Writing – Review & Editing (equal); Tom O'Connor: Conceptualization (equal), Formal Analysis (equal), Methodology (equal), Writing – Original Draft Preparation (equal), Writing – Review & Editing (equal).
ACKNOWLEDGEMENTS
Jonas Monsees received a research grant from Tallaght University Hospital. No further funding was awarded for this work. Open access funding provided by IReL.