Validation of a focused echocardiographic training program in first opinion practice
Funding information: Boehringer Ingelheim, Grant/Award Number: N/A
Abstract
Background
The EPIC study defines criteria, including echocardiographic assessments of left atrial to aortic ratio (LA: Ao) and left ventricular internal diameter in diastole normalized for body weight (LVIDdN), for dogs with preclinical myxomatous mitral valve disease (MMVD) likely to benefit from pimobendan therapy. Access to echocardiography by a cardiologist is not universally available.
Hypothesis/Objectives
Completion of a focused echocardiographic training program would result in accurate identification of dogs fulfilling the EPIC criteria by primary care veterinarians (PC).
Participants
Six PCs with no previous echocardiographic experience.
Methods
Prospective diagnostic test accuracy study. After training, each PC evaluated ≤10 dogs that they believed to have preclinical MMVD. The evaluation was repeated by 1 of 3 cardiology diplomates, blinded to the PC's findings. Agreement between clinical assessments and echocardiographic measurements was assessed.
Results
Fifty-seven dogs were evaluated by PCs; 1 dog was withdrawn because of congestive heart failure. The median time between PC and cardiologist evaluation was 0 days (range, 0-8). One incorrect diagnosis of MMVD was made by a PC (this dog had dilated cardiomyopathy [DCM]); preclinical MMVD was confirmed by the cardiologist in 55 dogs. No difference in LA: Ao (P = .96; CV = 6.9%) was detected between PCs and cardiologists. LVIDdN (1.69 cm/kg0.294 (1.26-2.21) vs 1.73 cm/kg0.294 (1.32-2.73); P = .001; CV = 6.5%), was significantly lower when measured by PCs vs cardiologists. PCs and cardiologists agreed regarding assessment of EPIC criteria in 49/56 dogs (Alpha = .761, 95% confidence interval 0.697-0.922).
Conclusions and Clinical Importance
The program effectively trained PCs to accurately assess EPIC criteria in dogs with preclinical MMVD.
Abbreviations
-
- ACVIM
-
- American College of Veterinary Internal Medicine
-
- Ao
-
- aortic root
-
- CHF
-
- congestive heart failure
-
- CI
-
- confidence interval
-
- CV
-
- coefficient of variation
-
- DCM
-
- dilated cardiomyopathy
-
- ELISA
-
- enzyme linked immunosorbent assay
-
- K-EDTA
-
- potassium ethylenediaminetetraacetic acid
-
- LA
-
- left atrial
-
- LA: Ao
-
- left atrial to aortic root ratio
-
- LVIDd
-
- left ventricular internal dimension in diastole
-
- LVIDdN
-
- left ventricular internal dimension in diastole, normalized for body weight
-
- MMVD
-
- myxomatous mitral valve disease
-
- PC
-
- primary care veterinarian
-
- VHS
-
- vertebral heart sum
1 INTRODUCTION
The EPIC study demonstrated a benefit of treatment with pimobendan in dogs with preclinical myxomatous mitral valve disease (MMVD) meeting the study inclusion criteria.1 These criteria include physical examination findings (eg, murmur intensity), calculation of vertebral heart sum (VHS) from right lateral thoracic radiographs and echocardiographic measurement of left atrial and ventricular dimensions. The high prevalence of MMVD in dogs2 and the relatively small number of cardiology diplomates (eg, 253 in the United States [https://www.vetspecialists.com/home], 41 in the United Kingdom [https://findavet.rcvs.org.uk/home/]) means that specialist echocardiographic assessment of every dog with suspected preclinical MMVD is not feasible. Access to specialist assessment is further limited by additional factors, such as financial or geographical constraints. Accurate assessment of heart size by primary care veterinarians, using echocardiography and radiography, therefore has the potential to improve management of this common condition.
Studies demonstrate benefits of focused echocardiographic training of noncardiologists, both in terms of increased clinician confidence3 and improved diagnostic accuracy in distinguishing cardiac from noncardiac causes of respiratory distress.4 Accuracy of left atrial and ventricular measurements by internal medicine specialists after a focused echocardiographic training program was good.5 However, these studies were all conducted in veterinary teaching hospitals and the effectiveness of echocardiographic training programs for primary care veterinarians remains unknown. Furthermore, clinical trials such as the EPIC study were conducted by specialists in a referral environment, using high quality ultrasound equipment. This equipment might not be available to all primary care practitioners, which might limit the “generalizability” of the results of these clinical trials.
We hypothesized that completion of a focused echocardiographic training program would enable primary care veterinarians to accurately assess whether dogs with MMVD meet the inclusion criteria for the EPIC study in the context of their own practice. Our objectives were to train a cohort of primary care veterinarians, who then recruited and assessed, unsupervised, dogs presenting to them with suspected preclinical MMVD in the course of their regular practice. Each dog was then reassessed by a cardiology diplomate and the primary care veterinarians' diagnostic accuracy assessed.
2 METHODS
This study was approved by the University of Bristol Faculty of Health Sciences Research Ethics Committee (FREC 61102; human participants) and the University of Bristol Animal Welfare and Ethical Review Body (VIN/16/055; animal participants) and informed participant and owner consent was obtained.
Primary care veterinarians with no previous echocardiographic experience and working in practices which are part of the HeartVets peripatetic network were recruited. Each primary care veterinarian underwent a focused echocardiographic training program, delivered by 3 cardiology diplomates (DD, JH, and MP). Briefly, this program comprised a combination of 2 hours of didactic lectures and 1 hour of practical training in echocardiography and was focused on the following elements: the American College of Veterinary Internal Medicine (ACVIM) scheme for staging of MMVD,6 the EPIC study (including inclusion criteria and key findings),1 measurement of VHS7 and pertinent echocardiographic skills (comprising the criteria used to diagnose MMVD and the methods for accurate assessment of left atrial and ventricular dimensions, according to the EPIC study inclusion criteria, detailed below). Briefly, the ACVIM staging scheme comprises stages A (at risk for future development of MMVD), B1 (evidence of preclinical MMVD without cardiomegaly), B2 (evidence of preclinical MMVD with cardiomegaly), C (evidence of congestive heart failure [CHF] secondary to MMVD) and D (evidence of refractory CHF secondary to MMVD). The focused nature of the training was highlighted in the didactic lectures; it was made clear to participants that they were only being taught to assess preclinical MMVD. Lectures and practical training sessions were standardized before delivery.
Echocardiographic evidence of MMVD was defined as characteristic abnormalities of the valve leaflets (thickening, prolapse, or both) and evidence of regurgitant flow across the valve detected by Doppler echocardiography, assessed using the right parasternal long axis view.8 The left atrial to aortic root ratio (LA: Ao) was measured from the right parasternal short axis view at the level of the aortic valve cusps, using the first frame after aortic valve closure.9 M-mode measurements of the left ventricle were obtained from the right parasternal short axis view at the level of the papillary muscles and the maximum dimension used to derive left ventricular internal dimension in diastole (LVIDd). The mean of 3 consecutive measurements was used for all analyses. LVIDd was normalized for body weight (LVIDdN) by the formula: LVIDd/(body weight [kg])0.294.10
After completion of the focused echocardiographic training program, each primary care veterinarian was asked to recruit up to 10 dogs presenting to them in the course of their regular clinical practice that they suspected to have preclinical MMVD. The inclusion criteria for dogs in the study were a left apical systolic murmur of grade ≥ III/VI, age ≥ 6 years, body weight < 20 kg, heart rate 60 to 160 beats/min, and a regular rhythm or rhythm compatible with sinus arrhythmia (ie, small and medium-sized dogs with at least moderately loud left apical systolic murmurs consistent with mitral regurgitation). The weight range was expanded from that of the EPIC study (≥4.1 and ≤15 kg) to reflect the full range of body weights of dogs most likely to have MMVD. Exclusion criteria were evidence of current or previous CHF, treatment with corticosteroids, pimobendan, or diuretics in the 4 weeks prior to presentation, general anesthesia or intravenous fluid therapy in the 7 days prior to presentation, any other cardiac disease, evidence of any significant systemic disease and estrus, pregnancy, or lactation. Dogs were included in the study if, in the opinion of the primary care veterinarian, all inclusion criteria were met and there was no evidence of any of the exclusion criteria. For each dog, the following were performed by the primary care veterinarian: the history was taken followed by physical examination, echocardiography, and thoracic radiography. All examinations were performed without sedation with the exception of thoracic radiography, for which sedation was permitted. If sedation was deemed necessary for thoracic radiography this was always performed after all other examinations were complete, including those of the cardiology diplomate if their assessment was performed on the same day, to ensure that no dog was sedated at the time of echocardiography by either veterinarian. Sedation for radiography with butorphanol ± acepromazine was recommended, but sedation protocols were not standardized to better reflect primary care practice.
The primary care veterinarian recorded their physical examination findings and whether or not, in their opinion, each dog met each inclusion and exclusion criterion. Each dog's microchip was scanned and the number recorded. For echocardiographic assessment, dogs were placed in right lateral recumbency on an ultrasound examination table, provided by the investigators for the duration of the study (The HeartVets Echocardiography Table, HeartVets, Whitestone, Exeter, UK). The ultrasound examination was performed using the primary care practices' ultrasound units equipped with 4.5 to 7.5 MHz phased array transducers and simultaneous electrocardiographic monitoring. A minimum quality of available ultrasound equipment was not a prerequisite for entering the study. Standard imaging planes were digitally stored. Assessment of mitral valve structures was performed from the right parasternal long-axis view. The primary care veterinarians recorded their echocardiographic diagnosis and their measurements of LA: Ao and their calculations of LVIDdN from measurements of LVIDd, using the criteria listed above. Left and right lateral and dorsoventral thoracic radiographic projections were obtained. Primary care veterinarians recorded their radiographic assessment of the presence of pulmonary perihilar infiltrates, interstitial or alveolar pulmonary patterns and pulmonary vascular congestion, plus their measurement of VHS, calculated using a right lateral projection of the thorax. Finally, the primary care veterinarian recorded their assessment of the dog's ACVIM stage and whether they recommended treatment with pimobendan. Initiation of treatment with pimobendan was not permitted before assessment by a cardiology diplomate.
Each dog was subsequently assessed by 1 of 3 cardiology diplomates (DD, JH, or MP) within 14 days of the primary care veterinarian's assessment. Each dog's microchip was scanned to confirm its identity. The cardiologist was blinded to all other primary care veterinarian findings. For each dog, the following were performed by the cardiology diplomate: the history was taken followed by physical examination, blood pressure measurement, blood sampling, and echocardiography. Blood pressure measurement was performed using Doppler sphygmomanometry (C-60 Doppler Ultra Vet 8.2 MHz, Parks Medical Electronics, Inc, Aloha, Oregon) using a thoracic limb and the inflatable cuff closest to 40% of the antebrachial circumference was chosen. Blood was collected by venipuncture and divided between serum and K-EDTA containers. Serum biochemistry and routine hematology was performed by the Langford Vets Diagnostic Laboratory, University of Bristol to rule out systemic disease. Echocardiographic examinations were performed as described above. All physical and echocardiographic examinations were performed without sedation.
The cardiology diplomate recorded their physical examination findings and whether or not, in their opinion, each dog met each inclusion and exclusion criterion. They also recorded their echocardiographic diagnosis and their measurements of LA: Ao and their calculations of LVIDdN from measurements of LVIDd. The radiographs obtained by the primary care veterinarians were reviewed by the cardiology diplomate, who recorded their assessment of the presence of pulmonary perihilar infiltrates, interstitial or alveolar pulmonary patterns and pulmonary vascular congestion. Finally, the cardiology diplomate recorded their assessment of the dog's ACVIM stage and whether they recommended treatment with pimobendan. For the purposes of statistical analysis, vertebral heart sum was calculated by a single cardiology diplomate (MJH) using the right lateral thoracic radiographs obtained by the primary care veterinarians.
The primary endpoint was agreement between primary care veterinarians and cardiology diplomates regarding whether treatment with pimobendan was indicated in dogs with MMVD (ie, accurate differentiation of dogs in stage B1 and stage B2). Secondary endpoints included assessment of agreement in recorded LA: Ao, LVIDdN and VHS between primary care veterinarians and cardiology diplomates.
A sample size calculation suggested that recruitment of 40 dogs would be sufficient to demonstrate a 20% difference between measurements obtained by primary care veterinarians and by cardiology diplomates. A recruitment target of 60 dogs was chosen to mitigate against smaller observed differences.
2.1 Statistical analysis
For continuous data, normality was assessed graphically and using the Shapiro-Wilk test. Agreement was assessed using Krippendorff's alpha and intraclass correlation coefficients to account for clustering of pairs of assessors. Confidence intervals (CI) for Krippendorf's alpha were calculated using a bootstrapping approach with 10 000 repetitions. For the purposes of interpretation of Krippendorff's alpha value, the categorization suggested by Landis and Koch was used,11 wherein values 0.41 to 0.6 indicate moderate agreement, values 0.61 to 0.8 indicate substantial agreement and values >0.8 indicate near perfect agreement. Intraclass correlations were calculated using a 2-way mixed effects model in which people effects were random and measures effects fixed. Agreement was interpreted using the same criteria as for Krippendorff's alpha. Between groups comparisons were performed using Mann-Whitney U tests and Wilcoxon signed-rank tests, as appropriate. Proportions were compared using chi-square or Fisher's exact test, as appropriate. Statistical analyses were performed using commercially available software (IBM SPSS 26, IBM [UK], Ltd, Portsmouth; GraphPad Prism 8, GraphPad Software, Inc, San Diego, California), and a custom written program (Krippendorf's alpha; Python [http://www.python.org]). All tests were 2-tailed and significance was set at P < .05.
3 RESULTS
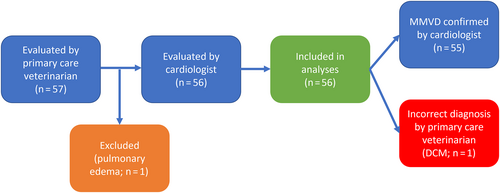
Six primary care veterinarians from 6 different primary care practices were recruited to the study and underwent the focused echocardiographic training program. Each primary care veterinarian subsequently recruited 8 to 10 dogs (median = 9.5 dogs, n = 57) over a median period of 7.6 months (3.2 to 9.5 months). Thoracic radiography revealed evidence of congestive heart failure in 1 dog; this dog was removed from the study and not evaluated by the cardiologist. The remaining 56 dogs were included in analyses (Figure 1). All dogs were deemed to meet all inclusion criteria and no exclusion criteria by the primary care veterinarians. One dog had a grade II/VI murmur on auscultation by the cardiology diplomate. No evidence of significant other systemic disease was found on physical examination in any dog and the results of hematological and serum biochemical analysis were normal in all dogs. The median time between primary care veterinarian assessment and assessment by the cardiologist was 0 days (minimum 0, maximum 8 days).
Summary statistics are shown in Table 1. Seventeen breeds were represented, with Cavalier King Charles spaniels (n = 18), cross breeds (n = 12), and Cocker spaniels (n = 4) most frequent. Dogs ranged in age from 6.2 to 15.3 years and in body weight from 3.3 to 19.8 kg. Significant differences in values recorded by primary care veterinarians and cardiologists were detected for body weight (P = .007), rectal temperature (P = .001), murmur grade (P = .04), left atrial diameter (P < .001), aortic root diameter (P = .004), LVIDd (P = .003), and LVIDdN (P = .001).
| Variable | Primary care veterinarian | Cardiologist | |||
|---|---|---|---|---|---|
| Number (%) | Median (minimum, maximum) | Number (%) | Median (minimum, maximum) | P value (between groups) | |
| Age | 10.3 (6.2, 15.3) | N/A | N/A | ||
| Breed | N/A | N/A | |||
|
18 (32%) | ||||
|
12 (21%) | ||||
|
4 (7%) | ||||
|
3 (5%) | ||||
|
3 (5%) | ||||
|
3 (5%) | ||||
|
2 (3%) | ||||
|
2 (3%) | ||||
|
9 (16%) | ||||
| Sex (male/female) | 34 (60%)/22 (39%) | N/A | N/A | ||
| Body weight (kg) | 9.95 (3.30, 19.80) | 9.95 (3.35, 19.90) | .007 | ||
| Body condition score (1-9) | N/A | 5 (3, 7) (n = 46) |
N/A | ||
| Heart rate (beats/min) | 120 (60, 160) (n = 52) |
120 (84, 160) | .91 | ||
| Rectal temperature (°C) | 38.2 (37.0, 40.0) (n = 51) |
38.1 (37.0, 39.0) | .001 | ||
| Intensity of heart sounds (quiet, normal, loud) | Normal (quiet, loud) (n = 52) |
Normal (quiet, loud) (n = 55) |
.32 | ||
| Murmur grade (I-VI) | IV (III, V) (n = 55) |
IV (II, VI) | .05 | ||
| Murmur intensity (soft, moderate, loud) | Moderate (soft, loud) (n = 52) |
Moderate (soft, loud) | .81 | ||
| Precordial thrill (yes/no) | 14 (25%)/39 (69%) | 9 (16.1%)/47 (83.9%) | <.001 | ||
| Apex beat intensity (weak, normal, strong) | Normal (weak, strong) (n = 53) |
Normal (weak, strong) (n = 55) |
.16 | ||
| Systolic blood pressure (mm Hg) | N/A | 136 (118, 170) (n = 43) |
N/A | ||
| Vertebral heart sum | 11.1 (9.1, 13.6) (n = 52) |
11.0 (9.1, 13.6) (n = 41) |
.24 | ||
| Echocardiographic evidence of MMVD (yes/no) | 56/0 (100%) | 55/1 (98.2%) | >1 | ||
| Left atrial diameter (cm) | 2.54 (1.22, 3.61) | 2.76 (1.68, 4.55) | <.001 | ||
| Aortic root diameter (cm) | 1.64 (.99, 3.34) | 1.73 (1.11, 3.13) | .004 | ||
| LA: Ao | 1.59 (1.09, 2.46) | 1.59 (1.20, 2.22) | .96 | ||
| LVIDd (cm) | 3.24 (1.79, 5.14) | 3.42 (1.42, 5.80) | .003 | ||
| LVIDdN (cm/kg0.294) | 1.69 (1.26, 2.21) | 1.73 (1.32, 2.73) | .001 | ||
- Note: P values < .05 are highlighted in bold.
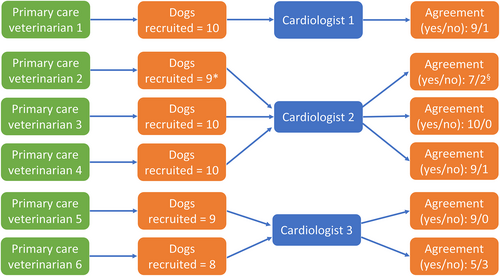
The number of dogs recruited by each primary care veterinarian, the cardiology diplomate with whom each was paired and the frequency of agreement of assignment to ACVIM stage for each pair of assessors are summarized in Figure 2. Thirty-three dogs were assigned to ACVIM stage B1 by both the primary care veterinarian and cardiologist and treatment with pimobendan was not recommended. Sixteen dogs were assigned to ACVIM stage B2 by both the primary care veterinarian and cardiologist and treatment with pimobendan was recommended. Four dogs were assigned to ACVIM stage B1 by the primary care veterinarian and stage B2 by the cardiologist. Two dogs were assigned to ACVIM stage B2 by the primary care veterinarian and stage B1 by the cardiologist. In 1 dog the primary care veterinarian's diagnosis of MMVD was incorrect; this dog was diagnosed with dilated cardiomyopathy (DCM) by the attending cardiologist. Overall, agreement in diagnosis and assignment to ACVIM stage between primary care veterinarians and cardiologists was substantial (Krippendorff's alpha = 0.761, 95% CI 0.697-0.922).
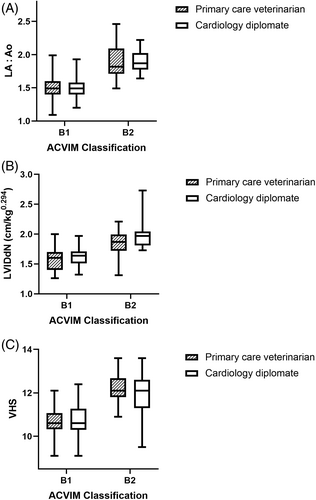
Intraclass correlation coefficients for LA: Ao, LVIDdN, and VHS between measurements obtained by primary care veterinarians and cardiologists were 0.809 (95% CI 0.674-0.888; P < .001), 0.789 (95% CI 0.641-0.877; P < .001), and 0.885 (95% CI 0.784-0.938; P < .001), respectively. Measurements of LA: Ao, LVIDdN, and VHS obtained by primary care veterinarians and cardiology diplomates for dogs assigned to ACVIM stages B1 and B2 by the cardiology diplomates are shown in Figure 3.
4 DISCUSSION
Myxomatous mitral valve disease is the leading cause of heart disease in dogs and treatment with pimobendan in the preclinical phase delays the onset of CHF in dogs with radiographic and echocardiographic evidence of cardiomegaly.1, 12 As universal access to echocardiographic assessment by cardiology diplomates is not practically achievable, training primary care veterinarians to accurately assess left atrial and ventricular dimensions has the potential to significantly improve the management of MMVD. The results of the present study demonstrate that, after completion of a focused training course, designed specifically to teach the skills required to differentiate stage B1 from stage B2 MMVD, agreement between primary care veterinarians and cardiology diplomates was substantial for differentiation of dogs with stage B1 vs stage B2 MMVD and substantial or excellent for measurements of LA: Ao, LVIDdN, and VHS. On an individual level, the primary care veterinarians each misclassified between 0% and 37.5% (3/8) of the dogs they recruited (Figure 2). It is therefore likely that the effectiveness of the program varied between participants, as might be expected with any training program.
A study demonstrated acceptable agreement for measurements of LA: Ao (coefficients of variation [CV] = 4.0%-7.0%) and LVIDdN (CV = 10.7%-13.8%) between noncardiologists and cardiologists.5 However, there are important differences in study design between these 2 studies. First, the previous study was performed in a teaching hospital and the participants provided with 15 healthy research beagles on which to perform their measurements. The noncardiologists were a board-certified specialist in internal medicine and a resident, although neither had any previous experience in ultrasonography. Finally, the measurements used for calculation of CVs were obtained at the same time as the training program was delivered. In contrast, in the present study, the primary care veterinarians were responsible for identifying up to 10 dogs likely to have stage B MMVD from those presenting to them in the course of their routine clinical practice, which they each achieved during the 3.2 to 9.5 month period which followed the training program. The primary care veterinarians then independently evaluated each case, recording their echocardiographic diagnosis and determining whether radiographic and echocardiographic evidence of cardiomegaly was present. The design of the present study therefore reflects Continuing Education training delivered to primary care veterinarians, who then return to apply their knowledge to their own caseload. Measurement agreement was substantial or excellent, despite several months having elapsed between training and assessment of dogs, suggesting a sustained training effect, at least in the medium term. The observer variability we measured also compares favorably with that reported between experts: Visser and colleagues found intraclass correlation coefficients of 0.97 for LVIDd and 0.39 for LA: Ao13; Locatelli and colleagues reported intraobserver, between-day CVs up to 7.2% for LVIDd and up to 7.6% for LA: Ao.14
As well as being required to perform echocardiographic measurements and calculate VHS, the primary care veterinarians were asked to make a diagnosis of MMVD, requiring integration of a range of clinical information. It is noteworthy that the diagnosis was incorrect in only 1 dog, although this may have been facilitated by the high prevalence of MMVD and the primary care veterinarians' familiarity with its typical presentation.
Significant differences in body weight (P = .007), rectal temperature (P = .001), murmur grade (P = .04), detection of a precordial thrill (P < .001), left atrial diameter (P < .001), aortic root diameter (P = .004), and LVIDdN (P = .001) were detected. However, these differences were small and not considered clinically important; the impact on measurement inaccuracy resulted in clinical misclassification in 6/56 (10.7%) of dogs; in 4 of these 6 misclassified dogs, the primary care veterinarian underestimated the disease severity (ie, misclassified a stage B2 dog as stage B1), which would have resulted in undertreatment rather than overtreatment. It is of note that, although measurements of left atrial and aortic root diameter by primary care veterinarians were significantly smaller than those obtained by cardiologists, there was no difference in LA: Ao (P = .96).
The study has a number of limitations. A relatively small number of primary care veterinarians participated and each evaluated a relatively small number of dogs. The sample size calculation was based on the authors' estimates of likely percentage differences in echocardiographic measurements between those obtained by primary care veterinarians and cardiology diplomates, rather than previously published or pilot data. Additionally, the sample size calculation did not take into account the hierarchical nature of the data: dogs were evaluated by 6 separate pairs of primary care veterinarians and cardiology diplomates. The observed differences in measurements were smaller than our initial estimates and so the study may be underpowered to demonstrate differences in these measurements. All training was delivered by the same 3 cardiology diplomates, all of whom are highly experienced in both echocardiography and the delivery of echocardiographic training; it is possible that the training program would be less effective if delivered by less experienced trainers. Although the primary care veterinarians had no previous experience in echocardiography, it is possible that they were motivated to participate in the study by a keen desire to learn these skills. Finally, it is possible that the knowledge that each dog would be reevaluated subsequently by a cardiology diplomate, albeit blinded to the primary care veterinarians' assessment, might have motivated the primary care veterinarians to take greater pains to obtain accurate measurements.
In conclusion, completion of the focused training program resulted in primary care veterinarians making appropriate treatment recommendations in the majority of dogs with preclinical MMVD with substantial to excellent accuracy of measurements of VHS, LA: Ao and calculations of LVIDdN from measurements of LVIDd.
ACKNOWLEDGMENT
Funding provided by Boehringer Ingelheim.
CONFLICT OF INTEREST DECLARATION
Authors declare no conflict of interest.
OFF-LABEL ANTIMICROBIAL DECLARATION
Authors declare no off-label use of antimicrobials.
INSTITUTIONAL ANIMAL CARE AND USE COMMITTEE (IACUC) OR OTHER APPROVAL DECLARATION
Approved by the University of Bristol Faculty of Health Sciences Research Ethics Committee (FREC 61102; human participants) and the University of Bristol Animal Welfare and Ethical Review Body (VIN/16/055; animal participants).
HUMAN ETHICS APPROVAL DECLARATION
Authors declare human ethics approval was not needed for this study.