Does the Villalta scale capture the essence of postthrombotic syndrome? A qualitative study of patient experience and expert opinion
Summary
Background
The Villalta scale is recommended for diagnosing and grading of postthrombotic syndrome (PTS) in clinical studies, but with limitations in specificity and sensitivity.
Objectives
To explore the typical complaints of PTS through patients experience and expert opinion and relate this to the items of the Villalta scale.
Patients/Methods
A qualitative study design with focus group interviews including patients with PTS and health care workers experienced in PTS patient care.
Results
Typical PTS complaints were reflected within four main domains: (a) agonizing discomforts; patients without venous ulcers often described other discomforts than pain; (b) skin changes; these were common and sometimes present before deep vein thrombosis (DVT). Except for venous ulcers, skin changes were considered of less importance; (c) fluctuating heaviness and swelling during the day and with activity; (d) post-DVT concerns; fear of DVT recurrence, health services failing to meet the patients’ expectations, and psychological and social restrictions. These findings are not necessarily captured or well reflected in the Villalta scale.
Conclusion
Our findings indicate that the Villalta scale does not capture typical PTS complaints or their importance to the patients. A revision of the diagnosis and grading should be considered.
Essentials
- The Villalta scale is recommended for diagnosing postthrombotic syndrome (PTS).
- We studied PTS complaints by group interviews and related them to the Villalta scale.
- Physical limitations, various and chronic leg problems, and concerns were among the main findings.
- Common patient complaints and the impact of PTS are not well reflected in the Villalta scale.
1 INTRODUCTION
The postthrombotic syndrome (PTS) is a common long-term complication following acute deep vein thrombosis (DVT) of the lower limb, and develops in 20%-50% of patients.1, 2 PTS is associated with increased health care costs and a reduction in quality of life.3-6 PTS includes a spectrum of symptoms and signs: pain, heaviness, itching, cramping, paresthesia, edema, erythema, venous ectasia, varicose veins, hyperpigmentation, skin induration, and, in severe cases, leg ulcers. The symptoms can be persistent or intermittent, changing throughout the day, and develop over the years.7-9 There is no gold standard test available for diagnosing and grading PTS in clinical practice or studies.10 Various clinical tools have been used, which limits the possibility to compare results across studies.11, 12 To standardize the definition of PTS for research purposes, the International Society on Thrombosis and Haemostasis has recommended the use of the Villalta scale for diagnosis and grading of PTS (Table 1).13 The Villalta scale is reported to be reproducible, sensitive to clinical changes, have a good interrater agreement, and include a severity grading.14, 15 The validity of the scale was established by demonstrating a correlation with relevant health outcomes (e.g., generic and disease-specific quality of life)16, 17 and anatomic and physiologic abnormalities.15
| Symptoms (scored by the patient) | Clinical signs (scored by caregiver, nurse/physician) |
|---|---|
| Pain | Pretibial edema |
| Cramps | Skin induration |
| Heaviness | Hyperpigmentation |
| Paresthesia | Redness |
| Itching | Venous ectasia |
| — | Pain on calf compression |
Note
- The symptoms and clinical signs in the Villalta scale are scored from 0 (= absent) to 3 (= severe) to produce a summary score ranging from 0 to 33 points. A total score of ≥5 points corresponds to any grade of PTS; 5-9 points mild PTS, 10-14 points moderate PTS, and ≥15 points or the presence of a venous ulcer to severe PTS. A score <5 indicates no PTS.13
The Villalta scale is widely accepted and has been used in cohort studies and landmark multicenter randomized trials.12, 18, 19 However, typical symptoms and signs of PTS may resemble leg symptoms commonly associated with other conditions including acute DVT, congestive heart failure, primary chronic venous disease, obesity, arthrosis, and injury.8, 20-24 Because the scale does not consider possible comorbidities or reflect on the chronology of DVT versus symptoms, the specificity is limited. Accordingly, the obtained score may diagnose PTS even when it is apparent to both the patient and the consultant that the patient's leg problems do not relate to PTS, but other conditions.9, 25-27 In addition, the sensitivity of the scale has limitations as it may not capture venous claudication.28 Venous claudication is associated with postthrombotic venous outflow impairment and involves pain and tightness in the thigh or calf on exercise, and typically subsiding with rest. During physical exertion, venous outflow impairment can also lead to a reduced cardiac preload leading to (pre-)syncope.29 Our concerns regarding these limitations are shared by others.11, 28, 29 In the present study, we aimed to improve PTS assessment by exploring how patients, and health care workers experienced in PTS patient care, experience PTS. Second, we related our findings to the items of the Villalta scale.
2 METHODS
2.1 Study design and participants
From March until December 2016, we conducted a qualitative, explorative study with focus group interviews to generate an understanding of health care workers (i.e., clinical experts’ and patients’ experiences of PTS). The clinical experts were senior consultants in circulation physiology, hematology, radiology, and vascular surgery, respectively, plus one thrombosis nurse. The patients were recruited by senior consultants in outpatient clinics (thrombosis, dermatology, and vascular surgery) at the Oslo University Hospital, Norway, and among participants of previous studies on long-term outcomes after DVT within the South-Eastern Norway Regional Health Authority. Five of the 16 patients were included in a previous RCT, the CaVenT study (Catheter-Directed Venous Thrombolysis). Six of the 16 patients were recruited by senior consultants participating in the expert focus group. All recruited patients had sought health care because of their leg problems and were considered to present with clinically relevant PTS. All invited patients were included, and no patients withdrew from the study. All participants were considered to provide rich and thorough information relevant to the research question.30 The southeastern Norway Regional Committee for Medical and Health Research Ethics approved the study (no. 2015/1567).
2.2 Interviews
In the focus groups, we searched for an understanding of what complaints and concerns patients and experts experience with PTS.31 The focus group interviews lasted for 2 hours in a seminar room outside the outpatient clinics. The interviews were audio recorded and transcribed verbatim by ME. We had two sources of data; the audio-recorded verbal communication and field notes summarizing the nonverbal communication. ME conducted the interviews, and TE and HSW served as moderators and facilitated the discussions within the groups. The clinical experts were interviewed in a focus group before the patient focus groups. We had an interview guide to ensure that similar questions were phrased in an open-ended manner in each group (Table S1). The interview guide was flexible (i.e., during the data collection process, we revised the interview guide by incorporating themes revealed in the previous focus group to explore these issues within the following focus groups). After each patient focus group, HSW and ME scored the affected limb with the Villalta scale, and the participants were asked if their functioning and quality of life was reduced because of postthrombotic problems (Table 2).
| Characteristics | N = 16 |
|---|---|
| n (%) | |
| Age, yrs | — |
| 30-49 | 7 (44) |
| 50-69 | 7 (44) |
| 70 and older | 2 (12) |
| Male | 11 (69) |
| PTS diagnosed by the Villalta scale | — |
| PTS not present | 0 (0) |
| Mild PTS | 5 (32) |
| Moderate PTS | 2 (12) |
| Severe PTS | 9 (56) |
| Venous ulcer | 6 (36) |
| Healed | 4 (25) |
| Open | 2 (12.5) |
| Localization of DVTa | 13 (81.3) |
| Proximal | 9 (56.3) |
| Distal | 4 (25) |
| Time interval from the first DVT, median, yrs (min-max)b | 8.5 (2-49) |
| Self-reported level of function resulting from PTS | — |
| Not reduced | 2 (12) |
| Mildly reduced | 7 (44) |
| Moderately reduced | 5 (32) |
| Severely reduced | 2 (12) |
| Self-reported quality of life due to PTS | — |
| Not reduced | 2 (12) |
| Mildly reduced | 5 (32) |
| Moderately reduced | 6 (36) |
| Severely reduced | 3 (20) |
| Regular use of elastic compression stockings | 14 (87.5) |
Note
- Postthrombotic syndrome (PTS) diagnosed by the Villalta scale: total score of ≥5 points corresponds to any grade of PTS, 5-9 points mild PTS, 10-14 points moderate PTS, and ≥15 points or the presence of a venous ulcer to severe PTS. A score <5 indicates no PTS.13
- a Missing data in three patients.
- b Missing data in one patient.
2.3 Data analysis
The interviews were analyzed using Kvale and Brinkman's method for thematic analysis. We performed an inductive analysis process to generate meanings from the raw data to identify patterns and themes.32 First, the transcribed interviews underwent multiple readings to get an overall impression of the data. Second, the participants’ responses were divided into units of meaning. Third, all responses were read, and themes dominating the units of meaning were stated as clearly as possible. Fourth, we analyzed the units of meaning regarding the specific purpose of our study; exploring the typical patients’ experience of living with PTS and relating these findings to the Villalta scale. In the fifth and final step, the most important themes (i.e., the main domains with related categories) were incorporated into a descriptive statement. An example of the data analysis is shown in Table 3. HSW, TE, and ME reviewed the data analyses to ensure that the results captured all primary data and selected quotations that best illustrated our findings.
| Statements | Units of meaning | Main domains (theoretical reflections) |
|---|---|---|
| “The pain following the presence of an ulcer is much more limiting than the pressure in my leg” | The patients experienced that other than venous ulcers, skin changes located in the lower limb following the PTS were of less importance to them. | Skin changes |
| “Of course, if it had appeared in my face, it would definitely have had an impact on my quality of life” | — | — |
| “I would rather have blue and green legs than legs not working.” | — | — |
| “It's not what's outside that is my problem. It's what it feels like inside my leg - that's the problem” | — | — |
3 RESULTS
We initially interviewed the five clinical experts in a separate focus group. The clinical experts had several years of clinical and research experience with PTS patients. The 16 patients with a previous objectively verified DVT of the lower limb were interviewed in 3 focus groups of 4-7 patients. Patient characteristics are presented in Table 2. All patients were fully mobile without any walking aids.
3.1 Interview data and interpretation
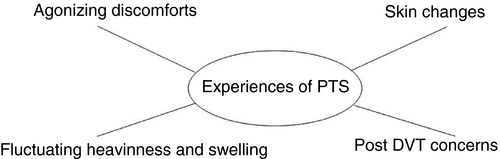
The authors agreed that further interviewing and data gathering after four focus groups would add little to the conceptualization and that the data collection had reached the point of saturation.30 Thematic analysis revealed four main domains; agonizing discomforts, skin changes, fluctuating heaviness and swelling, and post-DVT concerns (Figure 1).
3.1.1 Agonizing discomforts
I find myself constantly moving my legs to keep my muscles going so I don't feel that pain. Or, it's not correct calling it pain. It's milder than pain. It's discomfort that is what I feel, not pain. Pain is like when you pinch yourself, that is what I call pain.
Some patients reported activity-related discomfort leading to limited physical performance, either from the affected limb or as symptoms of presyncope. This increased the more demanding the activity was. The study population ranged from people with a sedentary lifestyle to a more athletic lifestyle. Five previously active and fit patients reported that they had been forced to give up sports because of limitations in physical performance following the DVT. For some, such restrictions represented a loss in their life. Physical performance or activity limitations are not included in the Villalta scale.
It's like before my first DVT: I was out running, playing football, or bicycling, eventually with nothing more to give. All worn out! I get that feeling now, but sooner. I was never any high performing athlete in school but sometimes ran the 800 meters. The feeling at 600 meters into the race, it's the same feeling now, but only after running 40-50 meters.
The first time I exercised after a (venous) stent insertion I was in heaven. I could go bicycling again and felt physical fit. But after a couple of months, everything tightened; I couldn't get enough oxygen. It was excruciating! I cold sweated, got pale, felt I was about to faint even in activities with low workloads.
3.1.2 Skin changes
When you have an ulcer, it's the worst pain. Avoiding these ulcers is the most important, for my part. Then it's not so painful. It's discomfort that I can live with. But when the ulcer evolves, it's hell.
I had skin changes and varicose veins in both legs before the DVT. My mum had varicose veins as well.
3.1.3 Fluctuating heaviness and swelling
The swelling is extremely big compared to the other leg. When I go downhill skiing and take off my skiing-boot at lunch, I have developed a sausage up to my knee. When unbuckling my ski boot, hell breaks loose with all the fluid returning to my foot. The enormous pressure makes me stop skiing for the rest of that day.
3.1.4 Post-DVT concerns
A topic that frequently came up was how PTS had changed the patients’ way of thinking about their health, body, and self. These concerns could be divided into fear of DVT recurrence, health services failing to meet patients’ expectations, and psychological and social restrictions in daily life. The Villalta scale does not incorporate aspects of post DVT concerns.
Fear of DVT recurrence
Suddenly I can feel something pinching inside my leg. Could it be a new clot? I control my INR at home, but if the symptoms persist over days, I go to the private hospital for a checkup. Ruling out a new DVT is important for my wellbeing, thus I consider the money I spend on this purpose, as money well spent.
Health services failing to meet patients’ expectations
I was supposed to take those pills for six months, and then I was done. I didn't get more information than that. I thought, blood clots, that's serious! At least I got scared, and then; no more information.
Psychological and social restrictions
I can adjust to a lot, but if I had gotten this ten years ago, I would have been on constant sick leave. I've decided that this can't affect my life with family, work, and friends. I constantly suppress my discomforts; it reduces my quality of life. You know, quality of life is complex. For me, it's the feeling of not doing what everybody else my age does. I can live with itching and heaviness, but my issue is the overall experience of my limitations.
4 DISCUSSION
We identified four main domains when interviewing PTS patients and clinical experts: agonizing discomforts, skin changes, fluctuating heaviness and swelling, and post-DVT concerns. The contribution of each of these aspects when diagnosing and grading PTS are not well reflected in the recommended Villalta scale.
In the Villalta scale, leg discomfort is reflected in the three items pain, restlessness, and heaviness. Our study patients without venous ulcers instead used pressure, pulsation, and burning sensations to describe their chronic leg discomforts. Thus, this may lead to an undergrading of nonulcer PTS. We are not aware of other studies that have looked into the different symptom experience of PTS patients with and without venous ulcers. The impact of venous ulcers with pain and impaired mobility and a reduction in quality of life was recently emphasized in a systematic review.33 Tired limb, heaviness, pain, and impaired endurance were the most frequent clinical findings in a recent cross-sectional study of pediatric PTS.34 The extent of limited physical performance following acute DVT of the lower limb is unknown. It is acknowledged that venous claudication can have a significant impact on daily functioning,29 and that this symptom should be included in a diagnostic tool for PTS.11, 28 Delis et al conducted a treadmill stress test on 39 patients with an iliofemoral DVT during the past 10 years. Forty-four percent experienced symptoms, 15% had to discontinue the treadmill test because of severe symptoms of venous claudication, and they all reported a reduction in quality of life.29 In our study, one patient reported severe limited physical performance with bursting pain and tightness in the thigh and calf on exercise subsiding with rest as the only symptom of PTS. However, because the Villalta scale does not capture venous claudication or limited physical performance, his score indicated nonsevere PTS. Physical limitations in PTS patients may also come from restricted venous return causing a reduced cardiac preload, and this may represent an underrecognized complication of extensive DVT.35 The Ginsberg measure, another diagnostic scale for diagnosing PTS in clinical studies, includes the assessment of pain (and swelling) made worse by standing/walking and relieved by rest/elevation of the leg.36 Thus, the Ginsberg measure can be more sensitive than the Villalta scale regarding venous claudication and physical limitations from PTS.11, 37
The various skin changes in PTS are reflected in the Villalta scale.7, 38 However, if leaving out venous ulcers, skin changes and the appearance of the legs were reported by patients to be of little importance compared with, for example, limitations in physical performance. This indicates that the Villalta scale does not capture the experienced severity of PTS, even if skin changes might be a sign of more severe PTS. Among the 11 Villalta scale items, 5 of the 6 clinical signs involve skin changes and weigh more than symptoms when summing up the score; thus, skin changes may contribute disproportionately to the overall score. Moreover, lower limb skin changes, including hyperpigmentation, redness, and venous ectasia are common in the general population.28, 39 Studies that have looked into the ability of the Villata scale to differentiate between PTS and chronic venous disease of nonthrombotic etiology have found diverging results. Galanaud et al found a strong correlation between the Villalta scale in the ipsilateral and contralateral limb (39.7% of the patients), suggesting that patients diagnosed with PTS by the Villalta scale could have a pre-existing chronic venous disease and not PTS.27 In another study using the Villalta scale, 27 of 92 patients diagnosed with PTS also had Villalta score above four in the contralateral limb not previously affected by DVT.40
The fluctuation of chronic venous leg problems has been reported by others,7, 9, 28 and was what best distinguished chronic venous disease from other diseases of the lower limb.22 As in our study, the patients were more likely to experience symptoms at the end of the day. Heaviness and swelling are both included in the Villalta scale, but the typical fluctuation is not. In contrast, the Ginsberg measure includes fluctuation of swelling made worse by standing/walking and relieved by rest/elevation of the leg.36, 37
The Villalta scale is reported to be sensitive to clinical change.14, 15 Nevertheless, one of our patients presented with a healed venous ulcer and will therefore always be regarded as having severe PTS by the Villalta scale. However, thanks to successful endovenous treatment, this patient suffered little PTS complaints with no reduction in quality of life or restriction in general functioning.
When PTS severity is assessed, the Villalta scale does not consider the impact on the patient's life. We found that the PTS patients would grade their PTS based on limitations in physical performance, limitations in social functioning, and the degree of physiological distress following the PTS. This can be supported by previous studies; in a qualitative study exploring patients’ experience of acute venous thromboembolism and its psychological impact,41 Hunter et al found that venous thromboembolism was life-changing and traumatic, the patients experienced uncertainty and fear of recurrence, and felt let down by the health services.41
Because our study may indicate that both the specificity and the sensitivity of the Villalta scale are limited, results from studies reporting on PTS prevalence, risk factors, prophylaxis, and treatment should be interpreted with caution.11, 12, 37, 42, 43 The limitations have been recognized by others, and, in line with our findings, it has been suggested that a quality of life questionnaire in addition to the clinical evaluation may be superior to the Villalta scale alone for assessment of PTS severity.39
Qualitative research can be hypothesis generating, and this study sought a deeper understanding of the experience of PTS from a first-person perspective.44 Our results do not provide statistically representative numbers to generalize them to a wider population, but can be incorporated in further research. The results must be interpreted with caution as the reported symptoms of PTS are subjective, and responses may be influenced by the respondents’ culture, religion, socioeconomic group, and profession.45 The participants were recruited because they presented with clinically significant PTS, and 6 of 16 patients had active or healed ulcers. Thus, our study population is likely to represent moderate to severe PTS, and the experience of mild PTS may not be well reflected in our findings. When conducting focus group interviews, a possible bias is the preconceived opinions of experts and researchers. TE, PMS, and HSW were experienced working with PTS patients, which was a benefit, but also a challenge making it essential to be aware of possible preconceptions throughout the different stages of the research process. The power relationships between the researcher and research participants (health care professional and patient) may also have shaped the data while it was collected. The investigators of this study did not use any study participants that they were treating in their own clinical practice. We are aware of that our presence, the way we asked our open-ended questions and focus group dynamics may have influenced the participants’ behaviors and how much they shared.
We conclude that the Villalta scale does not seem to capture various typical PTS complaints or reflect on the importance of PTS symptoms and signs. Improvements in sensitivity and specificity seem warranted and, based on our findings, we suggest that the identified agonizing and fluctuating symptoms and signs, the patients’ post-DVT concerns, and leg comorbidity should be systematically assessed when studying PTS patients.
AUTHOR CONTRIBUTIONS
T. Enden, H. S. Wik. P.M. Sandset, and M. H. Andersen conceived the research study design. M. Engeseth, T. Enden, and H. S. Wik performed the focus group interviews. M. Engeseth performed the thematic analysis. M. Engeseth, T. Enden, M. H. Andersen, and H.S. Wik interpreted data. M. Engeseth drafted the manuscript, and all authors critically revised the manuscript.
CONFLICT OF INTERESTS
The authors state that they have no conflict of interest.