Poorer objective but not subjective driving performance in drivers vulnerable to sleep loss effects during extended wake
Nicole Lovato and Andrew Vakulin are senior co-authors.
Summary
Sleepiness-related errors are a leading cause of driving accidents, requiring drivers to effectively monitor sleepiness levels. However, there are inter-individual differences in driving performance after sleep loss, with some showing poor driving performance while others show minimal impairment. This research explored if there are differences in self-reported sleepiness and driving performance in healthy drivers who exhibited vulnerability or resistance to objective driving impairment following extended wakefulness. Thirty-two adults (female = 18, mean age = 33.0 ± 14.6 years) completed five × 60-min simulated drives across 29-hr of extended wakefulness. Subjective sleepiness (Karolinska Sleepiness Scale) and subjective driving performance ratings (nine-point Likert scale) were assessed at 10-min intervals while driving. Cluster analysis using simulator steering deviation and crash data categorised participants as vulnerable (n = 16) or resistant (n = 16) to driving impairments following extended wakefulness. No differences in self-ratings between the vulnerable and resistant groups were observed except during the last drive (25 hr awake), where the vulnerable group reported higher sleepiness (p = 0.008) and worse driving performance (p = 0.001) than the resistant group. For each 1-point increase on the Karolinska Sleepiness Scale and subjective driving scales, the vulnerable group showed about threefold greater steering impairment relative to resistant drivers. Although self-reported sleepiness and driving performance were correlated with objective driving performance, vulnerable drivers reported similar sleepiness and driving performance as resistant drivers. Thus, self-reported sleepiness and driving performance are not reliably sensitive to sleep loss effects on objective driving performance, which may impact the vulnerable driver's decisions to continue driving and delay engagement in countermeasures to reduce crash risk (e.g. napping), warranting further research.
1 INTRODUCTION
Errors due to driver sleepiness and fatigue are associated with approximately 20% of motor vehicle accidents worldwide (Thomas et al., 2021). Insufficient sleep impairs driving performance by increasing sleepiness, which in turn increases the frequency of attentional lapses and slowed reaction times. The adverse effects of heightened sleepiness greatly elevate motor vehicle crash risk (Fairclough & Graham, 1999; Marando et al., 2022). Therefore, drivers' self-perception of sleepiness, as well as more objective methods, are needed to prompt countermeasures to improve the safety of themselves, their passengers, and other road users. However, the effectiveness of self-monitoring as a road safety strategy largely depends on drivers being able to accurately monitor their sleepiness and driving performance, and take appropriate action to minimise sleepiness-related driving risks.
Previous simulated driving studies and real on-road driving studies have evaluated the relationship between subjective (self-reported) sleepiness and objective driving performance. In a systematic review, which included both simulated driving and on-road driving studies (n = 37 studies included), Cai et al. (2021) reported a small–moderate correlation between subjective sleepiness and lane positioning outcomes (i.e. lane deviations and standard deviation of lateral position; rweighted = 0.46). Howard et al. (2014) found, when using a low-fidelity driving simulator, that subjective sleepiness and various driving performance metrics (e.g. crashes and lane deviations) are moderately correlated. Using a high fidelity moving base driving simulator, Anund et al. (2017) showed that for every 1-point increase on the Karolinska Sleepiness Scale (KSS), the odds of a lane crossing event increased 5.4 times. In contrast, naturalistic driving studies have reported conflicting results. One naturalistic on-road driving study in professional drivers found no correlation between subjective sleepiness and lane deviation (Mulhall et al., 2020), and another study in shift workers found a small negative correlation (Anund et al., 2013). Heterogeneity in study designs (e.g. different sleep duration conditions and study populations) and methodologies (driving simulator versus on-road driving) are likely contributors to these inconsistent findings. High inter-individual differences in driving performance following extended wakefulness may also, in part, contribute to the mixed findings.
Some individuals exhibit trait-like vulnerability to the vigilance performance declines observed during extended wakefulness, while others are more resistant (Tkachenko & Dinges, 2018; Van Dongen et al., 2004). This phenotypic difference in performance during extended wakefulness has a possible genetic basis (Goel & Dinges, 2011), is consistent within individuals in the short and long term (Yamazaki & Goel, 2020), and appears to be task-dependent (Hudson et al., 2020). For example, Hudson et al., (2020) found that individuals who showed vulnerability to vigilant attention deficits as measured on the Psychomotor Vigilance Task (PVT) did not show vulnerability in other cognitive tasks, such as the Digit Symbol Substitution Task.
However, there is limited research that systematically examines inter-individual differences in subjective ratings of sleepiness and how they relate to driving performance during extended wake. Manousakis et al. (2021) examined the temporal relationships between subjective sleepiness and both physiological sleepiness (microsleeps and slow eye movements) and reaction time performance PVT in 18 participants during 40 hr of extended wakefulness. The authors found strong within-subject (r = 0.6–0.75) and modest between-subject (r < 0.28) correlation between subjective sleepiness and both physiological sleepiness and vigilance performance, which became stronger with longer extended wakefulness. Driving performance, however, was not assessed. A study by Ingre et al. (2006) did examine the relationship between subjective sleepiness and objective driving simulator performance on an individual level in 10 participants. Participants were tested on a 2-hr driving simulator test following a normal night sleep or a night of work showing that there was a curvilinear relationship between subjective sleepiness ratings and driving simulator performance (crash and incident events). Taken together, current literature suggests that drivers are aware of their sleepiness levels, which increase during extended wakefulness and correlate with concurrent deterioration in driving performance (Åkerstedt et al., 2014; Cai et al., 2021). Nonetheless, the relationship between subjective sleepiness and objective driving performance has not been examined in drivers identified as either vulnerable or resistant to objective driving impairment following sleep loss based on their objective driving performance.
Subjective ratings of driving performance are rarely assessed in driver sleepiness research, despite their importance for influencing driver decisions to continue driving or to employ sleepiness countermeasures (e.g. cease driving, take a nap or consume caffeine; Sagaspe et al., 2007). Vakulin et al. (2007) used a repeated-measures design in a sample of healthy sleepers to compare subjective driving performance ratings obtained during 70-min simulated drives between a control condition (time-in-bed mean ± SD = 511.5 ± 19.1 min) and a sleep-restricted condition (time-in-bed mean ± SD = 243.8 ± 7.4 min). Perceived driving impairment was higher in the sleep-restricted condition than the control condition. Self-reports related to deteriorating driving performance (e.g. difficulty keeping to the centre of the lane) are also predictive of near-crash events (receiver operator characteristic area under the curve [AUC]: 0.88; Anderson et al., 2023). Overall, the literature suggests that participants are subjectively aware of their impaired driving performance under extended wakefulness in controlled laboratory environments. However, it remains unclear if subjective driving performance ratings differ between participants who are objectively vulnerable versus resistant to driving impairment following sleep loss. Addressing this knowledge gap is important given the potential adverse consequences if drivers who are vulnerable to driving deficits with extended wakefulness are not sensitive to their driving impairment while driving.
This study aimed to assess if subjective sleepiness and subjective driving performance ratings collected during repeated driving simulator assessments across extended wakefulness differed between participants identified as vulnerable versus resistant to extended wakefulness effects. We also explored whether pre-drive subjective sleepiness ratings differ between the vulnerable and resistant groups to help determine the potential utility of pre-drive sleepiness ratings for evaluating fitness to drive.
2 METHODS
This study was conducted as part of a larger trial approved by the Flinders University Human Ethics Research Committee (HREC: 4648). All participants gave written, informed consent.
2.1 Participants
Thirty-two participants (14 males, 18 females) aged 19–69 years old were recruited through the Flinders Health and Medical Research Institute: Sleep Health volunteer registry, online advertisements on Facebook and Gumtree, and posters on Flinders University campus noticeboards. Fifty-four participants were initially screened as eligible for the study, 39 of which participated in the laboratory protocol. Thirty-one participants completed the full extended wakefulness protocol, while eight participants withdrew due to reports of headaches and tiredness. However, data from 32 participants were analysed as one of the participants who withdrew during the laboratory completed the necessary number of drives (four drives) required for analysis.
2.1.1 Screening materials
All prospective participants completed the Epworth Sleepiness Scale (ESS), an eight-item questionnaire to assess an individual's propensity to doze off during multiple scenarios (Johns, 1991), and the Insomnia Severity Index (ISI), a seven-item questionnaire to assess insomnia-related sleeping difficulties and impacts on daily life (Morin, 1993). All participants screened into the study were healthy sleepers with little to no symptoms of insomnia (ISI < 10; Morin et al., 2011) or excessive daytime sleepiness (ESS < 10; Johns, 1991).
2.1.2 Inclusion criteria
Study inclusion required participants to self-report a regular nocturnal sleep pattern with habitual bedtime from 20:00 hours to 00:00 hours, and wake-up time from 05:00 hours to 09:00 hours, hold a full class C (Australian) driver's licence at the time of participation, and drive at least 2 hr per week.
2.1.3 Exclusion criteria
Participants who met any of the following criteria were excluded: physical or mental health problems or sleep conditions that could affect sleep; body mass index (BMI) > 35 kg/m2 (Marando et al., 2022); active use of illicit substances or prescription medication that alter sleep; excessive use of alcohol or caffeine (> 4 drinks a day), or cigarettes (non-casual smoking); trans-meridian travel (> 2 time zones) in the past 2 months, or nightshift work (23:00 hours–06:00 hours) one or more times a week in the past 2 months. Individuals who were pregnant, lactating or caring for a newborn (< 12 months) were also excluded.
2.2 Design and protocol
This study used a 2 (vulnerability group: vulnerable, resilient) × 5 (drive number: 1, 2, 3, 4, 5) mixed repeated-measures design to examine whether subjective sleepiness and subjective driving performance differed between individuals categorised as vulnerable and resistant to extended wakefulness-induced driving impairment over five simulated drives.
2.2.1 Pre-laboratory consent meeting
Eligible prospective participants attended a 2-hr consent meeting held 2 weeks before their scheduled laboratory stay that involved an explanation of the procedures and obtaining written informed consent. Participants practised the assessments in the main protocol, including a 10–30-min practice session of the driving simulator, to reduce learning effects and establish potential sensitivity to simulator sickness.
2.2.2 Pre-laboratory baseline period
Participants completed a 2-week baseline monitoring period before the main protocol. Baseline sleep was monitored using GENEActiv monitors (Rowlands et al., 2014) and a morning sleep diary (Rogers et al., 1993) that was completed daily throughout the baseline period.
2.2.3 Laboratory stay and main protocol
Participants commenced with a 9-hr in-lab sleep opportunity, anchored according to their self-reported habitual sleep and wake times. The extended wakefulness protocol commenced immediately following their sleep opportunity. Participants completed five test batteries (Figure 1). Each test battery consisted of two testing phases and two blocks of free time. During the testing phases, participants completed a 10-min virtual reality goggles test of vestibular ocular motor system function related to the aims of the main trial before completing their driving simulator task, followed by sustained attention assessments. These assessments were the PVT (10 min), a simple reaction time task, and the attentional network task (~15 min), which assesses alerting, orienting and executive attention. Timing of the 9-hr in-lab sleep opportunity and all assessments conducted during extended wakefulness were scheduled based on the participant's self-reported habitual sleep and wake times. Participants undertook the first battery of testing at 1 hr after their wake time. This 1-hr buffer was incorporated to help to minimise the effects of sleep inertia, which is a temporary period of decreased alertness and performance following an awakening (Tassi & Muzet, 2000).
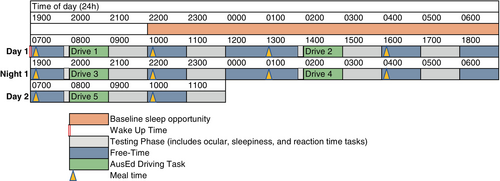
The driving simulator assessments were undertaken at 1, 7, 13, 19 and 25 hr into wakefulness, capturing sleepiness and driving performance across a 24-hr period, thus reflecting periods of high and low sleepiness due to homeostatic and circadian influences (Borbély & Achermann, 1992; Stiller & Postolache, 2005). During the drive, participants were prompted by an audio beep at 5, 15, 25, 35, 45 and 55 min into the drive. At each beep, participants verbally stated their sleepiness level and perceived driving performance based on scales displayed at eye level on the monitor next to the driving simulator screen.
Participants received meals at regular intervals throughout their stay. They were not permitted to consume caffeine or alcohol, sleep or vigorously exercise during the protocol, and were asked to limit caffeine consumption in the week before their laboratory stay. Rooms were kept at dim lighting (< 10 lux) and set to an ambient temperature of ~23°C during extended wakefulness. These factors were controlled to minimise the effect of external factors on alertness and subsequent performance.
2.2.4 Polysomnography (PSG)
The sleep prior to the extended wakefulness was recorded using PSG (Compumedics Grael, Victoria, Australia). Participants were set up with electrodes to record brain waves (electroencephalography; EEG), eye movements (electrooculography), chin muscle activity (electromyography), and a nasal cannula and thermistor to record airflow, and abdominal and thoracic bands for respiratory effort. Sleep was scored in accordance with the 2007 AASM criteria (Iber et al., 2007). The cut-off used to define obstructive sleep apnea (OSA) was an apnea–hypopnea index (AHI) > 10 events per hr, in which case participants were still included and followed up with the sleep physician on the project (n = 2).
2.3 Outcome measures
2.3.1 AusEd driving simulator
The AusEd driving simulator is a basic driving simulator task that assesses driving performance in a night-time highway driving setting (Desai et al., 2007). The task was performed on a desktop computer (Dell OptiPlex 7080 MT) on a 21-inch computer monitor with a steering wheel (Logitech Momo Force Feedback) mounted to the desk, and brake and acceleration pedals fixed to the floor. The drive duration was 60 min. Participants were instructed to maintain their vehicle position in the left-hand lane (in line with Australian Road Rules), keep their speed between 60 and 80 km/hr, and to brake as quickly as possible whenever a slow-moving truck appeared ahead of them in the driving lane. The trucks were presented a total of five times during the drive at 10-min intervals. The primary performance measures obtained were average steering deviation from the median lane position (cm) and number of crashes. Crashes were defined as instances when the vehicle moved completely off-road, stayed still for > 3 s, or collisions with a truck.
2.3.2 Subjective sleepiness and driving performance perception scales
Similar to previous studies (Banks et al., 2004; Vakulin et al., 2007), brief auditory beeps were played at 10-min intervals during the drive to prompt participants to verbally rate their sleepiness/alertness (KSS) and driving performance for capture via audio recording with minimal intrusion to driving performance (Keeler et al., 2015). All participants have received instructions on how to respond to the subjective sleepiness (KSS) and driving performance scales during the initial pre-laboratory visit, and again prior to beginning each driving simulator test during the extended wakefulness protocol. A paper (420 × 297 mm) displaying the performance questions and perception scales was attached to the left or right side of the computer screen that the driving task was performed on.
Participants rated sleepiness levels using the KSS, which asked participants to “Rate your alertness or sleepiness since the last tone” on a nine-point Likert-type scale from “1 = extremely alert” to “9 = very sleepy, great effort to stay awake, fighting sleep” (Åkerstedt et al., 2014).
The subjective driving performance question was “Rate your driving performance since the last tone” and nine-point Likert-type scale with labels on every other step (1 = Excellent, 3 = Good, 5 = Okay, 7 = Very bad and 9 = Terrible), as used previously to measure perceived driving performance during the drive (Banks et al., 2004).
Participants also provided a KSS rating through an online survey immediately prior to each drive. We used the Qualtrics online survey platform to administer the pre-drive KSS scales.
2.4 Statistical analysis
IBM Statistical Package for Social Sciences (IBM SPSS, version 25) software was used to perform statistical analyses. A two-step cluster analysis was used to categorise participants into the vulnerable or resistant group. Two-step cluster analysis is an approach that identifies homogeneous groups of cases based on the distributions of the input variables (Kent et al., 2014). Two variables were inputted into the cluster analysis models: mean steering deviation and number of crashes obtained from each participant's worst driving performance assessments. The log-likelihood distance measure and Bayesian (BIC) clustering criteria were applied with automatically determined number of clusters and with a silhouette coefficient of > 0.5, which is defined by SPSS as good data partitioning (Figures S1A–C and S2). All data were checked for normality and log(10)-transformed if normality was violated. For all driving simulator assessments, the first minute of the drive was excluded from analysis to account for initial acceleration and lane positioning (Desai et al., 2007). Independent samples t-tests were utilised to compare demographical data between the vulnerable and resistant groups. To examine the change in subjective ratings across the extended wakefulness protocol, linear mixed models (LMMs) were conducted to compare the average subjective sleepiness and subjective driving performance between the two vulnerability groups across the five driving simulator tests during extended wakefulness. Separate LMMs were run for each individual drive to compare changes in subjective sleepiness and subjective driving performance ratings that were collected at 10-min intervals within the drives. Additional exploratory analyses using LMMs were used to examine if single pre-drive KSS ratings differed between vulnerability groups. The models included interactions between group and time into wake, and between group and time into each drive. Participants were specified as a random factor(s). Statistical significance was set at the p < 0.05 level, and two-sided p-values were used. Separate individual and group level linear regressions were performed to further explore regression slopes, intercepts, and the strength of relationships between subjective sleepiness and driving performance and objective continuous steering deviation outcome in vulnerable and resistant driving groups.
3 RESULTS
From the 140 respondents screened for eligibility for the main trial, 52 were ineligible and 34 declined to participate. Thirty-nine participants completed the 2-week baseline period. The final sample consisted of 32 healthy participants (82% completion rate). Based on the cluster analysis, 16 participants were assigned into the vulnerable group and 16 participants in the resistant group (Table 1; Figure S1). The Silhouette measure of cohesion and separation of the two clusters was 0.6, which corresponds to Good cluster quality (Figure S1). The vulnerable group consisted of six males and 10 females, and the resistant group consisted of eight males and eight females.
| Variable | Full sample | Resistant | Vulnerable | df | t | p |
|---|---|---|---|---|---|---|
| N | 32 | 16 | 16 | |||
| Gender (M/F) | 14/18 | 8/8 | 6/10 | |||
| Age | 33.0 ± 14.6 | 34.1 ± 14.2 | 32.0 ± 15.4 | 30 | 0.39 | 0.70 |
| BMI | 24.3 ± 3.6 | 24.8 ± 3.3 | 23.7 ± 3.9 | 30 | 0.86 | 0.40 |
| Years with a full driver's licence | 11.4 ± 15.8 | 14.2 ± 15.3 | 8.6 ± 16.2 | 30 | 1.01 | 0.32 |
| Hours driven per week | 6.4 ± 6.3 | 7.1 ± 5.3 | 6.2 ± 6.9 | 30 | 0.43 | 0.67 |
| ESS score | 5.0 ± 2.8 | 4.3 ± 2.1 | 5.7 ± 3.3 | 30 | −1.49 | 0.15 |
| ISI score | 4.8 ± 3.1 | 4.9 ± 3.0 | 4.8 ± 3.3 | 30 | 0.06 | 0.96 |
| Two-week baseline (GENEActiv) | ||||||
| SOL (min) | 22.9 ± 2.4 | 22.9 ± 1.9 | 23.0 ± 3.3a | 24 | −0.16 | 0.88 |
| WASO (min) | 81.8 ± 52.3 | 75.8 ± 39.5 | 91.5 ± 75.1 | 24 | −0.90 | 0.38 |
| TST (hr) | 7.0 ± 2.1 | 7.3 ± 1.7 | 6.5 ± 2.7 | 24 | 2.09 | 0.11 |
| Week prior to study (Sleep Diary) | ||||||
| SOL (min) | 22.1 ± 20.5 | 22.3 ± 21.9 | 21.8 ± 19.2 | 213 | −0.16 | 0.87 |
| WASO (min) | 21.4 ± 27.2 | 17.7 ± 27.1 | 24.5 ± 27.1 | 213 | 1.60 | 0.11 |
| Sleep quality rating (1–5) | 3.6 ± 0.8 | 3.6 ± 0.7 | 3.6 ± 1.0 | 56 | −0.16 | 0.88 |
| Refreshing sleep rating (1–5) | 3.5 ± 0.8 | 3.5 ± 0.8 | 3.4 ± 0.8 | 212 | −1.4 | 0.17 |
| TST (hr) | 8.6 ± 1.1 | 8.5 ± 1.0 | 8.7 ± 1.2 | 213 | 1.27 | 0.21 |
| Sleep efficiency (%) | 93 ± 7 | 94 ± 6 | 93 ± 7 | 213 | −1.09 | 0.28 |
| Count of sleep diaries included | 215 | 104 | 111 | |||
| In-laboratory sleep (PSG) | ||||||
| SOL (min) | 58.3 ± 47.4 | 61.7 ± 52.4 | 55.1 ± 43.8 | 29b | 0.39 | 0.35 |
| WASO (min) | 93.9 ± 67.5 | 97.1 ± 62.6 | 90.8 ± 73.7 | 29 | 0.26 | 0.80 |
| TST (hr) | 7.32 ± 1.16 | 7.17 ± 1.08 | 7.46 ± 1.25 | 29 | −0.68 | 0.50 |
| Sleep efficiency | 0.75 ± 0.13 | 0.74 ± 0.13 | 0.76 ± 0.14 | 29 | −0.44 | 0.66 |
| N1 (%) | 9.1 ± 4.4 | 9.0 ± 5.2 | 9.2 ± 3.6 | 29 | −0.10 | 0.92 |
| N2 (%) | 49.1 ± 7.9 | 49.2 ± 8.9 | 48.9 ± 7.1 | 29 | 0.10 | 0.92 |
| N3 (%) | 21.6 ± 7.9 | 22.6 ± 8.1 | 20.6 ± 7.9 | 29 | 0.70 | 0.50 |
| REM (%) | 20.2 ± 6.8 | 19.1 ± 6.8 | 21.2 ± 6.8 | 29 | −0.84 | 0.41 |
| Total AHI (/hr) | 3.0 ± 4.2c | 2.1 ± 1.5 | 3.9 ± 5.6 | 29 | −0.14 | 0.89 |
| Total sleep arousal index (/hr) | 11.7 ± 7.2 | 12.0 ± 7.5 | 11.3 ± 7.1 | 29 | 0.27 | 0.79 |
- All metrics are mean ± standard deviation unless otherwise specified.
- AHI, apnea–hypopnea index; BMI, body mass index; ESS, Epworth Sleepiness Scale; ISI, Insomnia Severity Index; PSG, polysomnography; REM, rapid eye movement; SOL, sleep-onset latency; TST, total sleep time; WASO, wake after sleep onset.
- a Full GENEActiv baseline data missing for six participants in the vulnerable group.
- b PSG recording file for one participant was lost due to technical failure and therefore not included in the PSG analysis.
- c Two participants were found to have a slightly elevated AHI (< 16) but were included as they met all other inclusion criteria.
Subjective driving performance data were missing for four participants in the resistant group as these were incorporated into the protocol to address the current study objectives after the main trial had already commenced. No significant differences were found in demographic data, driving experience, subjective and objective sleep variables between the original sample and the sample without the four participants missing subjective driving performance data. One participant did not complete the full protocol but was included in the analysis given they completed four out of the five drives.
The groups did not differ on demographic characteristics, driving experience, or any objective and subjective sleep variables. About 63% of participants displayed their worst steering deviation at 25 hr, 25% at 19 hr, 3% at 13 hr, 3% at 7 hr and 6% at 1 hr into wake.
3.1 Objective driving performance in vulnerable versus resistant groups
By design based on cluster analysis, the vulnerable group consisted of participants with greater steering deviation and crashes than the resistant group (main effect of vulnerability group [F1,30 = 30.3, p < 0.001]; Figure 2a). There were significant interactions of vulnerability group by drive number on steering deviation (F4,109 = 12.6, p < 0.001) and crashes (F4,92 = 12.0, p < 0.001). Pairwise comparisons showed increases in steering deviation for the vulnerable group from drive 3 (13 hr) to drive 4 (19 hr; mean difference [95% confidence interval (CI)]; −38.8 [−50.1 to −27.5], p < 0.001) and from drive 4 (19 hr) to drive 5 (25 hr; −24.0 [−35.3 to −12.7], p < 0.001). In contrast, the steering deviation of the resistant group remained stable throughout and did not differ from drive to drive. For the driving simulator crashes, pairwise comparisons showed increased crashes in the vulnerable group from drive 4 to drive 5 (mean difference [95% CI]; −1792 [−2.72 to −0.86], p < 0.001), whereas the crashes of the resistant group did not differ from drive to drive.
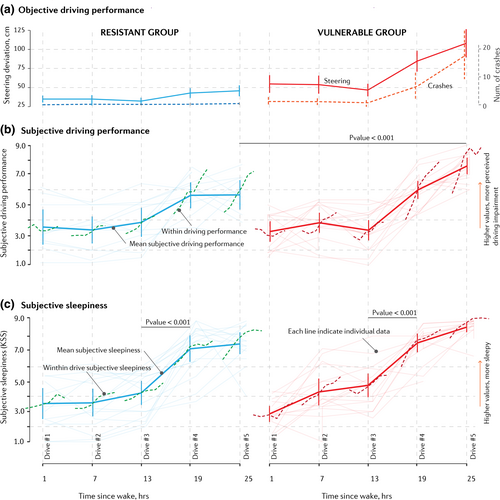
3.2 Subjective driving performance across wake
Subjective driving performance over the five drives for the resistant and vulnerable groups is shown in Figure 2(b). There was a main effect of time since wake (F4,62 = 40.4, p < 0.001), but not vulnerability group (F1,27 = 1.1, p = 0.30). There was a significant interaction between vulnerability group and time since wake (F4,62 = 4.8, p = 0.002). This reflected a sustained deterioration of subjective driving performance from drive 4 (19 hr) to drive 5 (25 hr) in the vulnerable group (mean difference [95% CI], 1.6 [0.9 to 2.3], p < 0.001, d = 0.9 [0.4 to 1.5]), but not in the resistant group (p = 0.84).
3.3 Subjective sleepiness across wake
Subjective sleepiness (KSS) ratings over the five drives for the groups are shown in Figure 2(c). There was a significant main effect of time since wake (F4,74 = 76.1, p < 0.001), but no significant group-by-time-since-wake interaction effect (F4,74 = 2.4, p = 0.06) or group main effect (F1,31 = 1.5, p = 0.24). Subjective sleepiness increased with extended wake. Pairwise comparisons showed no significant differences in KSS between drives 1 and 2 (p = 0.09), drives 2 and 3 (p = 0.51), and drives 4 and 5 (p = 0.23), but an increase in KSS from drive 3 to drive 4 (2.9 [2.1 to 3.7], p < 0.001, d = 2.1 [1.5 to 2.7]).
3.4 Within-drive subjective driving performance
Within-drive subjective driving performance ratings are represented by the individual dashed lines in Figure 2(b). No significant interactions were found between vulnerability group and subjective driving performance in drive 1 (F5,62 = 0.1, p = 1.0), drive 2 (F5,77 = 0.8, p = 0.6), drive 3 (F5,74 = 0.9, p = 0.5), drive 4 (F5,73 = 0.7, p = 0.6) or drive 5 (F5,72 = 1.2, p = 0.3). There were no main effects of time-on-task in drive 1 (p = 0.3). However, there were main effects of time-on-task in drive 2 (F5,77 = 5.2, p < 0.001), drive 3 (F5,74 = 5.9, p < 0.001), drive 4 (F5,73 = 16.6, p < 0.001) and drive 5 (F5,72 = 11.4, p < 0.001). During these drives, both groups reported increased driving impairment the longer they spent driving. There were no significant main effects of vulnerability group on subjective driving performance in drives 1–4 (p > 0.05). However, there was a significant main effect of vulnerability group in drive 5 (F1,24 = 14.2, p = 0.001), such that the vulnerable group reported higher overall impairment in subjective driving performance than the resistant group.
The strength of within-subject associations between steering deviation and subjective driving performance ratings ranged from (mean ± SD) r2 = 0.33 ± 0.30 in drive 1 to r2 = 0.63 ± 0.29 in drive 4, with no differences between vulnerable versus resistant driving groups.
3.5 Within-drive subjective sleepiness (KSS)
Within-drive subjective sleepiness ratings are represented by the individual dashed lines in Figure 2(c). There were no significant interactions between vulnerability group and subjective sleepiness in drive 1 (F5,65 = 1.0, p = 0.4), drive 2 (F5,77 = 0.7, p = 0.6), drive 3 (F5,90 = 0.6, p = 0.7), drive 4 (F5,137 = 0.9, p = 0.5) or drive 5 (F5,87 = 0.3, p = 0.9).
There were significant main effects of time-on-task in drive 1 (F5,65 = 3.6, p = 0.006), drive 2 (F5,77 = 6.7, p < 0.001), drive 3 (F5,90 = 3.6, p = 0.005), drive 4 (F5,137 = 12.1, p < 0.001) and drive 5 (F5,87 = 6.4, p < 0.001). Both groups reported increased KSS the longer they spent driving, but there were no significant main effects of vulnerability group in drives 1–4 (p > 0.05). Only during drive 5 (25 hr into wakefulness) did the vulnerable group report greater sleepiness than the resistant group main effect of vulnerability group (F5,29 = 8.2, p = 0.008).
Within-subject associations between steering deviation and subjective sleepiness ranged from r2 = 0.27 ± 0.28 in drive 1 to r2 = 0.53 ± 0.30 in drive 4, with no differences between vulnerable versus resistant driving groups.
3.6 Associations between subjective ratings and steering deviation
Linear regression relationships between average objective steering deviation and subjective sleepiness ratings (KSS) determined across all five drives for the vulnerable and resistant groups are presented in Figure 3(a). The resistant group showed a significantly steeper relationship (greater sensitivity) between steering deviation and KSS compared with the vulnerable group (mean ± SD slope 0.23 ± 0.15 versus 0.07 ± 0.05 KSS units/cm, p < 0.001; r2= 0.51 ± 0.30 versus 0.71 ± 0.23, p = 0.042), such that for each 10-cm increase in steering deviation KSS increased by 2.3 in the resistant group compared with 0.7 in the vulnerable group. Thus, at a mid-scale KSS rating of 5, steering deviation in the vulnerable group was approximately twice that of the resistant group (33 ± 13 versus 63 ± 23 cm, p < 0.001).
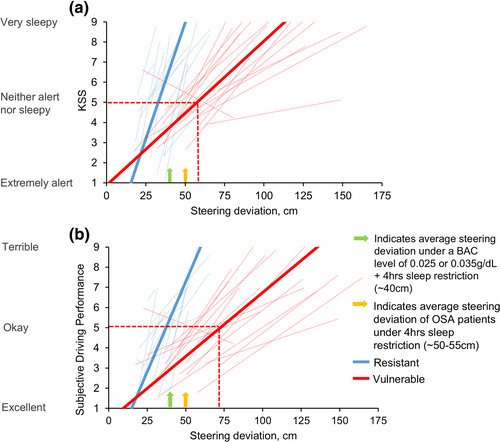
The slope of the relationship between objective and subjective driving performance showed similar results (Figure 3b), with a significantly steeper slope in the resistant compared with vulnerable group (0.18 ± 0.14 versus 0.06 ± 0.04, p = 0.018; r2 = 0.64 ± 0.28 versus 0.81 ± 0.20, p = 0.1), such that for every 10-point increase in steering deviation, subjective driving performance increased by 1.8 compared with 0.6. At a mid-scale subjective driving performance rating of 5, steering deviation in the vulnerable group was more than twice that of the resistant group (32 ± 15 versus 77 ± 25 cm, p < 0.001).
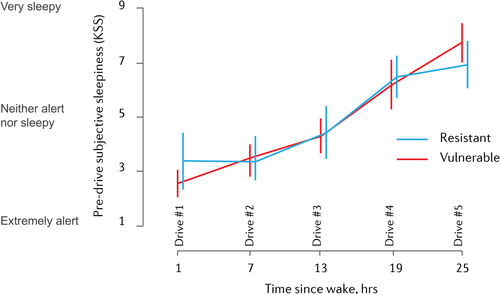
3.7 Pre-drive subjective sleepiness (KSS)
There was no significant interaction between vulnerability group and time since wake on KSS obtained just prior to driving tests (F4,75 = 2.0, p = 0.1). Pre-drive KSS did not differ between vulnerability groups (F1,31 = 0.02, p = 0.9), but did increase the longer the participants were awake (F4,75 = 42.1, p < 0.001; Figure 4).
4 DISCUSSION
This study provides a novel comparison of subjective sleepiness and perceptions of driving performance between groups that were categorised as being vulnerable versus resistant to objective driving simulator impairment across extended wakefulness. This insight is important for road safety, particularly given evidence of potentially reduced perceptual sensitivity of both sleepiness and driving performance in the vulnerable group over the course of extended wakefulness compared with the resistant group.
Consistent with previous findings, the participants' subjective sleepiness and subjective driving performance impairment increased across the protocol. Ratings of sleepiness and driving performance impairment rose at drive 4 (19 hr since wake) compared with the previous drive (13 hr since wake), with drive 4 occurring in the early morning, likely close to the circadian nadir in alertness (Gradisar & Lack, 2004; Manousakis et al., 2021).
For the most part, the vulnerable and resistant groups did not differ in their subjective sleepiness or driving performance perceptions across the first four drives, and were also no greater in the vulnerable group than the resistant group with increasing time spent awake, or time spent driving. Only on drive 5 (25 hr into wake) did the vulnerable group report worse overall driving performance than the resistant group, despite markedly poorer objective performance. Perhaps the ability to perceive sleepiness and driving impairment is hindered in the vulnerable group the longer they were awake. We saw no evidence of this; however, the objective driving simulator performance was already significantly impaired in the vulnerable drivers even at rested baseline (drives 1 and 2), but subjectively they did not report more sleepiness or driving impairment during these drives. Overall, our findings may suggest that the resistant group might be more sensitive, and overestimate their sleepiness and impairment (Boardman et al., 2018) despite relatively unimpaired objective driving. Alternatively, the vulnerable group might underappreciate their sleepiness and impairment despite having greatly impaired objective driving. This is purely speculative as it is not possible to determine which scenario from the data, but our findings likely reflect the subjective nature of perceptual responses of individual momentary sensations relative to prior experiences.
When examining the relationship between steering deviation and subjective ratings, we found consistently flatter relationship slopes in the vulnerable group, suggesting potentially lower perceptual sensitivity, with subjective reports not adequately reflective of impaired performance in the vulnerable drivers relative to the resistant drivers. We can speculate that perhaps the vulnerable drivers may underappreciate their sleepiness and driving performance relative to their objective driving performance, and the resistant drivers may be more perceptive of sleepiness and performance decrements, but we cannot determine this from our data. Given that driving performance is relative and varies widely between individuals, the subjective ratings may actually reflect the individual participant's accurate perception of their best performance relative to themselves. Another possibility is the potential for non-linear perceptual relationships and ceiling effects compared with objective outcomes (Manousakis et al., 2021). Indeed, a previous study by Ingre et al. (2006) showed a curvilinear relationship between KSS and driving simulator accident event rates within a 2-hr drive in 10 participants. The authors did not however examine the relationships with continuous driving outcomes of steering performance over multiple drives across 24 hr of wakefulness as was the case in the present study. The relatively small sample further limited the capacity to examine inter-individual differences in poor performance risk. These methodological differences may partly account for the different patterns of relationship found in our study. For the most part, in our study, the perceptual relationships with steering deviation outcomes were relatively well described by linear relationships, with superior fit compared with a non-linear model, with most participants using the full range of each scale with limited evidence of ceiling effects, except perhaps in the final drives. Furthermore, even at and below mid-range subjective ratings of 5, the vulnerable group showed approximately twofold greater steering deviation compared with the resistant group.
A likely consequence of relatively lower perceptual sensitivity of poorer driving in vulnerable compared with resistant drivers is that vulnerable drivers may be more likely to continue to drive despite their larger decrements in performance. For example, using the same AusEd driving simulator, young healthy drivers studied following sleep restriction combined with alcohol (blood alcohol concentration [BAC] 0.035 g/dl) had an average steering deviation of 40–45 cm (Vakulin et al., 2007). In patients with OSA, the average steering deviation following sleep restriction (4 hr) was about 54 cm, and 51 cm following alcohol consumption (BAC = 0.05 g/dl; Vakulin et al., 2009). In this study, the vulnerable group's steering deviation was at or above these levels of impairment despite relatively low levels of self-reported sleepiness and driving impairment. Based on linear regression fits, when the vulnerable drivers reported a KSS score of 5 (“neither sleepy nor alert”, often used as a normal reference in previous literature; Cai et al., 2021), their steering deviation was about 63 cm, almost twice the steering deviation of the resistant group at the same KSS level. When the vulnerable group reported a score of 5 on the driving performance scale, their relative steering deviation was about 77 cm, well above impacts of sleep deprivation and/or alcohol conditions in previous studies (Vakulin et al., 2007; Vakulin et al., 2014). This suggests that the vulnerable group perceive their sleepiness and driving performance to be relatively unimpaired, which may be unlikely to prompt countermeasures.
Our exploratory analysis of sleepiness ratings obtained prior to the driving task revealed the expected increase in self-reported sleepiness prior to each of the five drives across extended wakefulness. However, there were no differences between the vulnerable and resistant drivers in their pre-drive ratings. This suggests that perceptions of sleepiness before driving are insufficient to distinguish between drivers who subsequently show significant versus minimal driving impairment.
Although participants perceived changes in sleepiness and driving performance over the course of driving during extended wake, it remains unknown if sleepiness is a sufficient cue to prompt countermeasures for those vulnerable to the effects of extended wakefulness. Thus, future studies should consider asking participants if their ratings of sleepiness or driving deficits become sufficient for them to decide they should stop driving. Research on subjective sleepiness levels while driving in high-risk populations such as people with sleep disorders (i.e. sleep apnea; Tregear et al., 2009; and insomnia; Léger et al., 2014) is also limited, and should be prioritised due to their greater risk of motor vehicle crashes. Finally, development of reliable objective markers to complement subjective self-assessment and risk mitigation is important to further reduce crash risk. Current literature shows some promise for the use of objective sleepiness assessments through analysis of EEG activity (Vakulin et al., 2016), ocular measures (Anderson et al., 2023; Mulhall et al., 2020) and electrocardiogram (Jung et al., 2014), with some fatigue-monitoring technologies being implemented in the transportation industry (Cori et al., 2021). However, their deployment and wider scale use is still limited due to practical constraints, lack of validation and sufficient evidence for predicting sleepiness on individual driver level (Cori et al., 2021). It is unknown whether objective sleepiness assessments or self-reports of sleepiness are more predictive of objective driving performance or if they could perhaps be used in combination to further predict alertness failure and driving impairment. A study by Anderson et al. (2023) recently showed that in shift workers who drove a real instrumented vehicle on a closed-loop track after a night shift, subjective sleepiness was moderately associated with a lane deviation in the next 15 min. Ocular measures, difficulty keeping to the centre of the road, and nodding off to sleep were also moderately associated with subsequent lane deviations. Further research is needed to determine the best objective and subjective measures, and their combination for optimising the accuracy for identifying poor driving.
Despite the strong repeated-measures design and carefully controlled laboratory conditions, there are limitations. Firstly, we used a relatively simple low-fidelity driving simulator to assess driving performance, which may have reduced the ecological validity of the study. The AusEd simulator simulates a monotonous night-time highway driving scenario, and is sensitive to performance impairments from factors such as sleep deprivation (Desai et al., 2006), alcohol consumption (Banks et al., 2004) and sleep disorders (Johns, 1991). Despite the extensive use and validation for detecting sleepiness-related driving impairment, it does not fully represent real driving, and is fundamentally a multidimensional vigilance task that, to a certain degree, represents driving a real car. Hence, future studies should be conducted in more realistic driving settings to confirm our findings. In general, however, direct comparison studies show that although driving simulators tend to exaggerate performance decrements relative to on-road driving, simulators do correlate well with on-road driving performance in both high- (Davenne et al., 2012) and low-fidelity driving simulators (Philip et al., 2005).
It is also possible that we have screened out participants who might have been more vulnerable to driving impairment due to sleep loss by recruiting healthy participants in this study. Furthermore, some participants may have self-selected to opt out of participating out of concerns or discomfort from the impact of extended wakefulness that may have also reduced the number of more vulnerable drivers. Despite this potential selection bias, our results likely underestimate the potential magnitude of driving vulnerability and potential discrepancy between self-reported sleepiness and driving impairment.
Another potential limitation is that we only examined performance under a single night of extended wakefulness in healthy sleepers. Therefore, applications of the findings cannot be generalised to chronic sleep restriction or insufficient sleep, which is often observed in shift workers and sleep-disordered populations.
5 CONCLUSION
In conclusion, we have demonstrated that drivers show considerable variability in their sensitivity to increasing sleepiness and driving performance impairment with repeated drives during extended wakefulness. We also found that although some drivers were more objectively vulnerable to extended wakefulness than others, perceptual ratings of sleepiness and driving performance were similar in both groups. We speculate that the vulnerable drivers may underappreciate their sleepiness and performance levels despite demonstrating clear objective driving impairment. These exploratory findings show perceptions of sleepiness and impairment may not be reliable cues to prevent risky driving in objectively vulnerable drivers. This needs to be verified in future studies and evaluation of more sensitive subjective and objective measures of sleepiness is required to prompt appropriate countermeasures.
AUTHOR CONTRIBUTIONS
Katrina Nguyen: Conceptualization; methodology; investigation; formal analysis; writing – original draft; writing – review and editing; visualization. Claire Dunbar: Supervision; writing – review and editing; formal analysis; project administration; investigation. Alisha Guyett: Investigation; writing – review and editing. Kelsey Bickley: Conceptualization; formal analysis; writing – review and editing; investigation; project administration; supervision; methodology. Duc Phuc Nguyen: Visualization; software. Amy C. Reynolds: Writing – review and editing. Peter Catcheside: Software; visualization; writing – review and editing. Hannah Scott: Writing – review and editing. Maslin Hughes: Investigation. Robert Adams: Writing – review and editing; funding acquisition. Leon Lack: Writing – review and editing. Jennifer Cori: Writing – review and editing. Mark E. Howard: Writing – review and editing; funding acquisition; resources. Clare Anderson: Funding acquisition; writing – review and editing. David Stevens: Funding acquisition; writing – review and editing. Nicole Lovato: Writing – review and editing; supervision. Andrew Vakulin: Supervision; writing – review and editing; funding acquisition; methodology; conceptualization; visualization; formal analysis.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the work of the research assistants at the Flinders Health and Medical Research Institute: Sleep Health and the participants involved in the study.
FUNDING INFORMATION
This work was supported by the Commonwealth Department of Infrastructure, Transport, Regional Development, and Communications, Office of Road Safety (ORS) grant Road Safety Innovation Fund −96 [RSIF2-96] and Neuroflex as the industry partner on the grant.
CONFLICTS OF INTEREST STATEMENT
KN, CD, AG and KB were supported by the Road Safety Innovation Fund (RSIF) grant (RSIF2-96). CD reports receiving scholarship support from The Hospital Research Foundation during her PhD, unrelated to the current manuscript. KB reports previously receiving scholarship support from the Cooperative Research Centre for Alertness, Safety and Productivity, unrelated to the manuscript. DPN, MH and LL have no conflicts of interest to declare. ACR reports research income from Sydney Trains, Compumedics, and the Sleep Health Foundation for research related to sleep and sleep disorders. PC reports grants unrelated to this study from National Health and Medical Research Council, Defence Science and Technology Group, Flinders University, Compumedics Ltd, Invicta Medical, Flinders Foundation, Medical Research Future Fund, Garnett Passe and Rodney Williams Memorial Foundation and Minister for Innovation and Skills, South Australia/Science, Technology and Commercialisation, and in-kind support of unrelated trials from REDARC and Re-Timer Pty Ltd. HS reports grants unrelated to this manuscript from the American Academy of Sleep Medicine Foundation and Flinders University, and in-kind support for unrelated work from Re-Time Pty Ltd, Compumedics Ltd and Withings Ltd. RA reports grants unrelated to this manuscript from the National Health and Medical Research Council, ResMed Foundation, The Hospital Research Foundation, Australian Government, the Defence Science and Technology Group, and Flinders Foundation, and in-kind equipment from Philips Respironics. JC reports grants unrelated to this manuscript from the Australian Automobile Association, Victorian Department of Transport and Planning and the national Transport Commission. MEH reports grants unrelated to this manuscript from the Victorian Department of Transport and Planning and the Australian Automobile Association. CA has contract research support from VicRoads, Transport Accident Commission, Rio Tinto Coal Australia, National Transport Commission, Tontine/Pacific Brands, and the Australian Automobile Association; industry funding through ARC Linkage scheme with Seeing Machines and Cogstate Ltd; lecturing fees from Brown Medical School/Rhode Island Hospital, Ausmed, Healthmed and TEVA Pharma Australia; and reimbursements for conference travel expenses from Philips Healthcare. In addition, she has served as a consultant to the Rail, Bus and Tram Union, the Transport Accident Commission (TAC), the National Transportation Committee (NTC), VicRoads/Department of Transport Victoria, and Melius Consulting. She has also served as an expert witness and/or consultant in relation to fatigue and drowsy driving, and was a Theme Leader in the Cooperative Research Centre for Alertness, Safety and Productivity, all unrelated to the current project. DS is the industry partner representative on this project, but was not involved in the current study protocol design, data collection or analysis. The project was investigator led and initiated. AV reports research supported by the National Health and Medical Research Council project grants and fellowship, and has received competitive research funding and equipment from ResMed, Philips Respironics Withings and Sleeptite for research unrelated to this project. NL reports grants from the National Health and Medical Research Council of Australia, and research supported by Philips Respironics, The Hospital Research Foundation and ResMed Foundation. CD is an HDR/ECR representative for executive meetings for the FHMRI: Sleep Health institute. ACR is on the Governing Council of the World Sleep Society. RA is a board member of the Sleep Health Foundation. MEH is a board member of the Institute for Breathing and Sleep. AV is the Academic Chair on the Sleep Health Foundation Consumer Reference Panel, the Chair of the Steering Committee, Australian Sleep and Alertness and a board member of the Sleep Health Foundation and Australasian Sleep Association.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




