Advancing value in oral health through meaningful measurement
Abstract
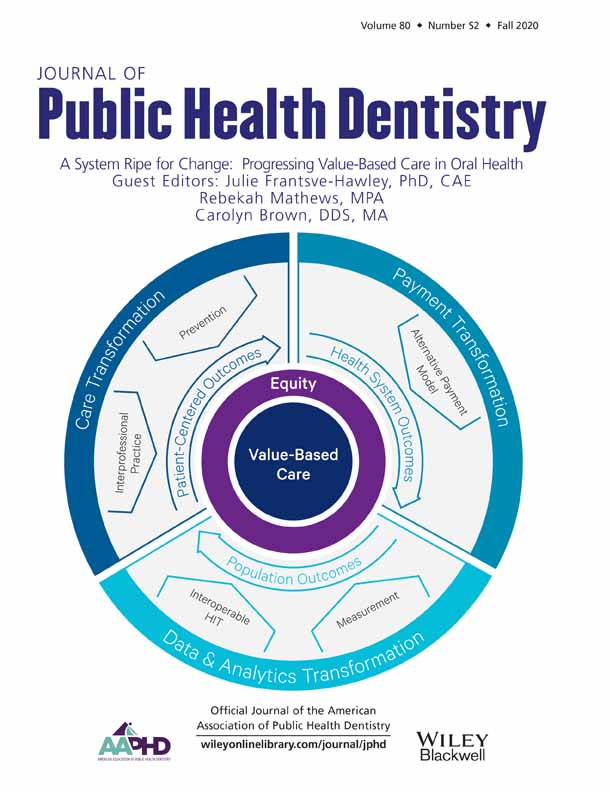
Central to all value-based purchasing (VBP) approaches are value metrics, the measurements used to drive improvement, facilitate payment, and evaluate results of VBP programs. This article outlines approaches for adopting meaningful measurement systems that can be used to support VBP in the near term and identifies systemic changes critical to developing more robust measurement systems to advance VBP in the future.
Introduction
The US healthcare system is moving away from paying for volume to paying for value. Value is not a novel concept. It is the basic idea of “bang for the buck” – evaluating what you are getting (outcomes) relative to what you are paying (costs). Yet in health care, value has been an elusive goal. Delivery systems are historically grounded in procedure-based fee-for-service payment that incentivizes procedure volume rather than outcomes that matter to patients, with little regard to the costs of care. Consequently, providers are not adequately rewarded for engaging in value-promoting activities.
Alternative payment methodologies, including value-based purchasing (VBP), are increasingly being adopted by public payers, such as the Centers for Medicare and Medicaid Services (CMS). Given that public financing plays a smaller role in dentistry than medicine1 and the current limitations in measuring oral healthcare outcomes, a wholesale shift from fee-for-service to comprehensive VBP is not likely or currently feasible in dentistry. Phased approaches are frequently used to introduce VBP and gradually shift the delivery-payment paradigm.2 The path toward VBP in dentistry will likely involve such incremental approaches. Central to all VBP approaches are value metrics, the measurements used to drive improvement, facilitate payment, and evaluate results of VBP programs.
Meaningful measurement
Measurement burden and attendant provider frustration, as evidenced in the broader healthcare system, can be reduced in dentistry by adopting the principles of meaningful measurement.3, 4
Identify care goals and high-impact measures
Ideally, VBP is based on stakeholder-engaged processes to identify patient-centered care goals and a carefully selected set of measures that reflects the desired results from quality improvement efforts. The selected measures should be supported by evidence that the care system can influence the outcomes. VBP measures should provide usable information focused on high-priority areas that are selected based on such considerations as prevalence (percentage of individuals affected), impacts on physical health and quality of life, and identified variations and disparities in care.
Select valid measures
Lack of valid performance measures has hindered incentive-based payments in dentistry.1, 5 There has been a dearth of measures, tested for their reliable and valid use, to guide quality improvement and accountability efforts. Since the Dental Quality Alliance's (DQA) establishment in 2010, oral healthcare performance measurement has progressed significantly with the development of standardized and validated measures.6 DQA measures are now being used by CMS, the US Health Resources and Services Administration, Covered California Health Insurance Marketplace, and state Medicaid programs.
Emphasize outcome measures that are meaningful to patients and providers
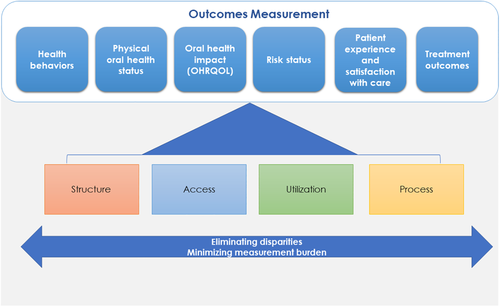
Most oral healthcare measures address utilization, access, or processes of care.7 However, outcomes-focused measurement, which is essential in measuring value, is lacking in dentistry. Lack of routine capture of standardized diagnosis codes is a long-recognized barrier to clinically assessed oral healthcare quality measurement.8 Future development of quality measures, and their use in VBP, will benefit from widespread adoption of diagnosis codes and their capture in oral healthcare databases. There also is a need for more high-quality evidence to support linkages between oral healthcare interventions and patient outcomes.1, 5
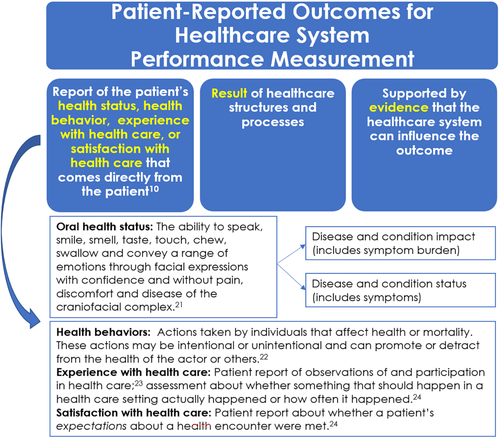
VBP is predicated on focusing not just on outcomes, but on the outcomes that matter to patients.9 Consequently, there is increasing emphasis on patient-reported outcomes (PROs). These include patient reports of the impact of health care on their health state, quality of life (including pain, function, and psychosocial well-being), health behaviors, and experiences and satisfaction with the care delivery system (Figure 1).10, 11 There are a range of oral health focused survey instruments that are well-validated in research contexts, but validation for use in clinical quality applications is lacking. With the exception of measures of patient experience or satisfaction, PROs are not widely used for routine quality assessment or as part of VBP. There are efforts underway to establish reliable and valid use of dental PRO performance measures in quality improvement applications.12, 13
Account for patient characteristics
A range of clinical and nonclinical patient characteristics may influence outcome measures.14 They may yield unintended consequences if VBP penalizes providers serving more vulnerable populations with greater risk for disease and higher barriers to securing recommended care. Risk adjusting measures takes into account the characteristics of the populations served but may have its own unintended consequences by masking disparities. Measurement can play a critical role in supporting efforts to identify and eliminate disparities. Approaches that promote both fair comparisons between providers and quality improvement efforts to eliminate disparities include: a) stratifying measures by patient characteristics, b) risk adjusting only after “appropriate measures for monitoring care to vulnerable groups have been fully implemented to avoid institutionalizing substandard care,”15 or c) risk adjusting for clinical factors and then reporting the risk-adjusted measure score overall and stratified by non-clinical factors.14 DQA measures include stratifications for reporting measures by population sub-groups to aid in identifying disparities in care and sharpening the focus of quality improvement efforts. Measure development and use in VBP must consider the role of patient characteristics in outcomes measurement and identify methodologies that promote value-based care for all patients.
Seek system-wide measure alignment and harmonization
Alignment (using similar measures across and within public and private purchasers) and harmonization (using standardized measure specifications) are key to reducing measurement burden by preventing unnecessary variation and duplicative reporting of measures by practices.16 Without alignment, practices will be asked to report a broader, more diverse range of measures; without harmonization, practices will be asked to report variations of the same measure concept. Achieving focused measurement requires the oral healthcare stakeholder community to work on measurement collaboratively. Ideally, stakeholder engagement is used to develop consensus around population health and care system goals. Coordinated efforts by public and private purchasers play an important role to identify aligned and harmonized measures in support of those goals.
The path forward
It will take considerable time until true VBP can be broadly implemented due to challenges in measuring oral healthcare outcomes. Rather than having the barriers serve as a hard stop, however, intermediate steps are possible now.
Begin payment reform with currently validated performance measures
The Health Care Payment Learning and Action Network developed a framework that provides a graduated structure for moving from traditional fee-for-service approaches to population-based, outcomes-oriented payments.17 Modified fee-for-service, where reimbursement is partially tied to quality metrics (i.e., pay-for-performance), is an example of a first step. A portion of payment is based on meeting performance targets for existing quality measures, such as the percentage of individuals who receive recommended preventive care.2, 18 The oral healthcare delivery system can thereby move forward on the path toward a value agenda while developing outcome measures and the associated measurement infrastructure. Figure 2 illustrates the longer-term vision of an outcomes-oriented measurement system in which structure, access, utilization, and process measures play a supporting role.
Carefully vet proposed VBP plans
Before using a measure for accountability purposes, it is strongly recommended that the accountability application be preceded by a period during which reporting entities gain experience with measure implementation, data are collected to establish baseline values, and appropriate benchmarks for comparison and performance goals are identified. Incorporating quality measures for accountability applications should be tested using multiple years of measure data to evaluate whether the application achieves the intended goals and whether there are unintended consequences that may undermine quality improvement efforts. It is incumbent upon the users of performance measures to carefully evaluate these impacts prior to implementing the accountability application. Development of benchmarks for quality measures used in any reporting applications should be guided by historical data evaluation for the population being served.19
VBP goals and approaches should be carefully considered for their impact on provider trust and morale, and on unintended consequences for care quality, outcomes, and disparities. All stakeholders, especially dental providers, should be educated about and involved in the development of new payment approaches. The DQA offers quality measurement and improvement educational resources that are designed for the provider community, including webinars and a course developed in partnership with the Institute for Healthcare Improvement.20
Build supportive health information technology infrastructure
Critical to supporting the transition to VBP and associated performance measurement are integrated and accessible health information systems. Current electronic records systems are typically confined to a practice and make it difficult to gain comprehensive documentation of care over time and across providers. Although practice management billing systems feed into administrative claims databases, these databases capture only a subset of clinical data and little information on outcomes that matter to patients. Much of the meaningful patient information is not aggregated beyond the practice to a broader systems level. Porter has commented that “siloed IT systems make cost and outcomes measurement virtually impossible, greatly impeding value improvement efforts.”9 Terminology, data fields, and definitions need to be standardized across platforms, and data collected should be accessible to both data analysts and clinicians to support quality improvement efforts. The American Dental Association Clinical Data Registry initiative is being developed with the intent to close these gaps.
Concluding remarks
We are cautiously optimistic about the implementation of VBP in dentistry. There are innovative efforts occurring around the country to improve oral healthcare outcomes, quality, and patient experience while also being cognizant of the costs of care. But the implementation of VBP, if not carefully designed, may lead to unintended adverse consequences that frustrate providers and fail to improve outcomes. Opportunities to advance oral health measurement that supports VBP include capturing diagnostic codes in a consistent and standardized manner, expanding the evidence base to confirm relationships between care interventions and outcomes, developing PROs that reflect outcomes meaningful to patients, developing methodologies to promote fair outcomes comparisons and eliminate disparities, and building the information technology infrastructure to support high-quality care and performance measurement.