A translational research framework for nurse practitioners
Abstract
Aims
This study aims to explore a proposed translational research continuum for nurse practitioners.
Background
Nurse practitioners are acknowledged as clinical leaders responsible for transforming health care delivery. It is important that nurse practitioners contribute to health care knowledge using scientific processes for the implementation of evidence-based practice and evaluation of outcomes of interventions for their patient groups.
Evaluation
This paper provides a review of translational research literature including implementation science to align nurse practitioner activities to a modified translational research framework.
Key Issues
A translational research framework has the potential to strengthen nursing research in the nurse practitioner role. Adapting an accepted translational research continuum for nurse practitioners places the clinical nursing leaders in an equitable research position with all health care professionals.
Implications for Nursing Management
The translational research continuum provides nursing management with a structure to benchmark nursing research. The continuum applies a modern research framework to support research engagement for the nurse practitioner role.
1 INTRODUCTION
The role of the nurse practitioner has been defined by the International Council of Nurses (ICN) as an advanced practice nurse (APN) who integrates nursing and medical clinical skills, to assess, diagnose and manage patients in primary health care, acute care and chronic illness populations (ICN, 2020). The nurse practitioner role is identified as the most senior clinical nursing role across several countries and is supported with regulatory frameworks (Carney, 2016). The evidence suggests that nurse practitioners are an excellent conduit to implement evidence-based practice (EBP) in clinical situations, resulting in the corresponding positive patient outcomes (Ryder et al., 2020a). Core attributes of the nurse practitioner role include leadership and research (Ryder et al., 2020a).
The role of nurse practitioners as nursing leaders has been well defined. Recent research has acknowledged nurse practitioners as clinical leaders, facilitating change and health care transformation (Elliott, 2017; Lamb et al., 2018; Ryder et al., 2019, 2020b; Steinke et al., 2018). Part of their clinical leadership role includes accessing, assessing and implementing EBP in the clinical setting, as independent autonomous practitioners, to improve quality patient care and achieve optimal treatment for defined patient groups (Ryder et al., 2019, 2020a). The importance of leadership to the nurse practitioner role has been identified in research to date from Canada, Ireland and Australia (Lamb et al., 2018; Ryder et al., 2019).
The research role of nurse practitioners is less clearly defined. While there is a scarcity of literature exploring the research role, Ryder et al. (2019) reported that nurse practitioners across Ireland and Australia perceived it to be important to their role. It is reasonable to expect as change leaders in health care, nurse practitioners are researching and publishing the impact of such changes for patient populations. Despite nurse practitioners valuing research in their role, little work time for nurse practitioners is allocated to research (Chattopadhyay et al., 2015; Johnson et al., 2016; Kleinpell et al., 2018; Martin-Misener et al., 2015; Middleton et al., 2011, 2016; Ryder et al., 2020b). This lack of research is due to workload, lack of understanding of the value to the nurse practitioner role and a misunderstanding that research is limited to empirical knowledge (Ryder et al., 2019; Weiss et al., 2018).
Literature related to the integration of research into clinical nursing in Ireland and Australia is lacking. However, it is arguably an opportunity for nursing management to engage with structures and clinical roles that are ripe to embrace opportunities to lead on research and EBP implementation. Emerging evidence from the United States indicates that translational research leverages the efforts of implementing EBP for applied health care disciplines, including nursing (Weiss et al., 2018). Nursing management must understand and support nurse practitioner research, as the outcome reflects the care delivered and stimulates changes in health care delivery.
2 AIMS
The aim of the article is to discuss the research role of nurse practitioners in the Irish and Australian context. The article will debate the traditional definition of research as perceived by nurse practitioners that includes a focus on empirical knowledge. The purpose is to discuss nurse practitioner research through the lens of the continuum of translational research (Khoury et al., 2007) and propose a modified continuum for nurse practitioner research across Ireland and Australia.
3 BACKGROUND
Research is arguably fundamental to the nurse practitioner role to inform the health care professions and the public of the outcomes of improvement to patient care. It may be reasonable to expect nurse practitioners, as transformers of health care practices, to produce an abundance of literature related to health care improvements for defined patient groups (Masso & Thompson, 2017). However, Ryder et al. (2020a) identified a paucity of published literature over two decades despite significant changes to the management of different patient groups led by nurse practitioners.
Developing nursing research in the clinical setting has been a long-standing conundrum for the profession (Cowman, 2019). Leading research to inform clinical practice has been identified as an important outcome indicator for nurse practitioners (Elliott et al., 2014). Elliott et al. (2014) proposed that research is part of the nurse practitioner role including demonstrating an increased use and application of evidence, knowledge generation to inform clinical practice and leading evaluation of changes to patient care. Yet other authors suggest that the nurse practitioner role is related only to implementation of EBP (Lambert & Housden, 2017). The ICN (2020) guidelines on advanced practice nursing acknowledge that the four domains that characterize these roles are education, practice, research and leadership. These domains, along with professional regulation, differentiate advanced practice from generalist nursing practice. However, the guidelines provide little explanation of the role of APNs apart from requiring the ability to integrate research into practice (ICN, 2020). While this document acknowledges the work of Gardner et al. (2016) in delineation of advanced practice nursing roles and supports the affirmation that the nurse practitioner role is the highest clinical nursing role, it falls short in its recommendations of research leadership and activities for nurse practitioners, supporting their engagement in research and influencing research (ICN, 2020).
The research outcomes proposed by Elliott et al. (2014) and supported by Ryder et al. (2020a) may be considered aspirational as nurse practitioner standards internationally lack clarity in specifying the research role for nurse practitioners (American Association of Nurse Practitioners, 2019; Lambert & Housden, 2017; Nursing and Midwifery Board of Australia, 2014; Nursing and Midwifery Board of Ireland, 2017). The nurse practitioner standards and requirements in Australia are clinically focused, specifying nurse practitioners are to contribute to research that addresses and identifies gaps in care provision (Nursing and Midwifery Board of Australia, 2014). In the Irish nurse practitioner standards and requirements, the word research only receives one mention, stating that the vision for the role is developing a knowledge base through research (Nursing and Midwifery Board of Ireland, 2017). Interestingly, research appears to have been downgraded since the inception of the role in both Ireland and Australia, where the original role concept and competency practice standards identified research as a core concept, expecting nurse practitioners to lead, conduct and disseminate research (Carryer et al., 2007; National Council for the Professional Development of Nursing and Midwifery, 2008). The research role of nurse practitioners in international standards and requirements continues to vary from developing research questions, conducting research, participating in research projects, journal clubs and communities of practice, disseminating and incorporating EBP into clinical practice, to attending professional conferences (American Association of Nurse Practitioners, 2019; College of Nurses of Ontario, 2018; Nursing and Midwifery Board of Australia, 2014; Nursing and Midwifery Board of Ireland, 2017). The recent International Council of Nurses Guidelines on Advanced Practice roles provide no clarification on this matter, instead focusing on the clinical leadership activities related to the role, with no acknowledgement of the research role (ICN, 2020).
It is crucial that senior clinical nurses, recognize the importance of research in demonstrating the effectiveness of the nurse practitioner role and how it can transform the delivery of health important that the nursing profession, including care and benefit patient care (Carrick-Sen et al., 2015). While there is evidence of some nurse practitioner research, Smigorowsky et al. (2019) argue that research to support the role is lacking and falling behind clinical practice. There is a lack of knowledge pertaining to the outcomes of nurse practitioner health care services, and the research is often poor quality (Masso & Thompson, 2017; Smigorowsky et al., 2019). Replying on single-centre research, reporting positive outcomes for patients over a limited time, does not support transferability of evidence to different patient population groups (Masso & Thompson, 2017; Ryder et al., 2020a).
Despite the lack of clarity regarding research in the nurse practitioner role, Ryder et al. (2020b) reported that the majority of nurse practitioners across Ireland and Australia were research active and engaged with clinical outcomes research. However, this is not reflected in the number of peer-reviewed publications produced by nurse practitioners in these countries (Ryder et al., 2020a). A science-based profession, such as nursing, relies on evidence-based, peer-reviewed publication to underpin clinical practices. The absence of evidence to support nurse practitioner-implemented health care transformation does not support transferability of knowledge for larger patient populations and sustainability of the role for the future.
4 EVALUATION
Recent research identified that nurse practitioners reported nursing management prioritized audit and quality improvement over research for their services (Ryder et al., 2019). Understanding this, it is acknowledged that nursing managers are focused on professional leadership, health care operations and quality care delivery. Many may not have been exposed to the emergence of translational research and implementation science. This paper provides a brief review of the literature on the history of translational research and implementation science and relates it to the more commonly understood quality improvement framework. The manuscript will then propose a translational research continuum that has emerged from research conducted across nurse practitioners in Ireland and Australia.
The nurse practitioner role is related to the transformation of health care and improving access to quality health care for patient populations. Nurse practitioner research should therefore be focused on the outcomes of quality improvement projects and health care transformations, both for patients and for health care. Translational research, also referred to as clinical outcomes research, is described as researching relevant knowledge and its application to real-life health care (Rubio et al., 2010). A translational research continuum captures the breadth of research and can be used to identify where individual research projects fit within the sequence.
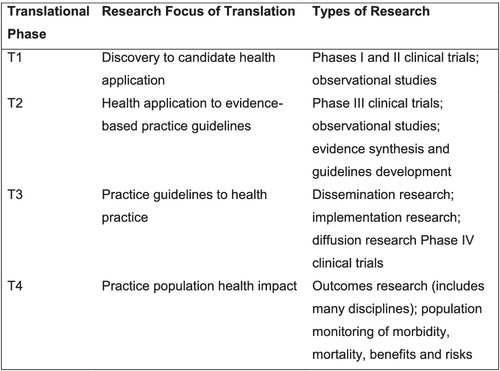
4.1 Translational research
Translational research is defined as the research steps to take new knowledge from the bench to the bedside and back again (Fort et al., 2017). Translational research as a framework presented in the traditional ‘bench-to-bedside’ model was the interface between basic science and clinical medicine (Woolf, 2008). However, Woolf (2008) believed the broader interpretation of translational research for all health care researchers, ensured that treatments and research knowledge actually reach the intended populations and were implemented correctly. In 2007, Khoury et al. presented a framework for the continuum of multidisciplinary translational research in genomic medicine (Figure 1). This continuum focused on enabling evidence-based research to be implemented into clinical practice, evaluated and disseminated, irrespective of research methods (Khoury et al., 2007). The epidemiological translational research continuum is constructed with four phases that evolve around the development of evidence-based guidelines (Khoury et al., 2007).
Translational research is not a new concept in nursing. It has been proposed as the dynamic interplay between research and practice, and the key to improve the quality of practice by rapidly translating research into widespread use in practice (Weiss et al., 2018). This differs from traditional research, whereby scholars discover new knowledge for the profession, often challenging particular assumptions (Florczak et al., 2014). Yet the two are rarely distinguished amongst the profession, or in standards and requirements, that arguably focus on research activities as opposed to research methods. Nursing management in Ireland are currently engaged with Magnet for Europe® Standards. Weiss et al. (2018) proposes that aligning the EBP activities of nursing policies with translational research activities will assist organisations toward achieving strategic Magnet objectives by increasing research capacity within organisations.
4.2 Implementation science
Implementation science is about understanding the process and methods of successfully embedding evidence into health care practice, focusing on internal and external control factors to enhance reproducibility (Casey et al., 2018). This relates to one phase of translational research, Phase T3, which is linked to implementation of the research findings in clinical practice (Fort et al., 2017; Khoury et al., 2007). Implementation science is described as the scientific study of methods to support the uptake of scientific evidence and EBP into clinical practice, to improve the quality and effectiveness of health services (Demiris et al., 2014; Weiss et al., 2018).
Quality improvement and implementation science are of a complimentary nature, as they have similar approaches to implement change in practice, but challenges exists in blending the two mainly due to inconsistent terminology (Check et al., 2019). Both quality improvement and implementation science observe a systematic theoretical approach, model or framework to facilitate the application of evidence into practice (Nilsen, 2015). The purpose of a theory/model/framework is to describe/guide the process of translating basic research into practice, to understand/explain influences on the outcomes of implementation and to evaluate the implementation (Nilsen, 2015). Using a theory/model/framework also fosters interdisciplinary dialogue during the consultative phases throughout the interactive implementation process working within a context (May et al., 2016). Although quality improvement has been described as a subcategory of clinical outcomes research, some would propose that this has now evolved into what is commonly referred to as implementation science research (Peters et al., 2013). Just as quality improvement is part of clinical outcomes, implementation science research is part of the translational research continuum (Lane-Fall et al., 2019).
Implementation of evidence is a complex process as it dependent on the context in which the intervention takes place and the persons involved (Rogers et al., 2020). Context is described as an important practical problem for complex interventions as there may be specific barriers and enablers for each different environment and situation (Rogers et al., 2020). Accounting for the influence of context is imperative to explain why certain implementation outcomes are successful in different situations, and failure to address this limits the generalizability and replicability of the findings (Nilsen & Bernhardsson, 2019). Interestingly, Masso and Thompson (2017) have previously reported that the lack of clear identification of the context of study in nurse practitioner research was an impediment to replicability of the research in other health care settings. Applying an implementation science framework to nurse practitioner led EBP health care transformation projects tackles the unique context of each organisation. For managers, the context will provide an insight into the variables that influenced the adoption of EBP in other organisations (Weiss et al., 2018) to enable critical judgement of the likely success in local context.
4.3 A translational research continuum for nurse practitioners
Clinical nurses engaged in the practice of real-world care delivery are essential to successful implementation of EBP (Zullig et al., 2020). The implementation of EBP, evaluation of outcomes and dissemination of the findings for other health professionals are important to improve patient outcomes internationally, but the clinical leaders of the nursing profession have not actively engaged with the dissemination of research to date (Zullig et al., 2020).
Active engagement in EBP to redesign health care structures and nursing research is part of the culture of nursing excellence within most organisations (Weiss et al., 2018). As a practice-based discipline, academic preparation of nurses has chosen to focus on EBP rather than research methods at master degree preparation level (Weiss et al., 2018). Gallen et al. (2019) have argued that nurses prepared to master's degree level are not sufficiently prepared in methods or statistics to undertake a significant lead in a research role. Therefore, the same question could be posed for nurse practitioners, where the minimum academic standard is master's degree level and they have been described as clinical leaders and champions of EBP (Ryder et al., 2020a). However, one author reports that nurse practitioners also lack the confidence to be independently research active (Ryder et al., 2019). Acknowledging that implementing EBP is a vital part of the translational research process clarifies the role that nurse practitioners are able to play in implementation research. Using the proposed translational research continuum provides clarity on nurse practitioner work allocation for nursing management who have struggled to differentiate between the range of scholarly endeavours by demonstrating they are all part of a research continuum where nurses contribute to evidence to improve patient outcomes (Carter et al., 2017).
Weiss et al. (2018) provides guidance clarifying where EBP aligns with translational research. EBP is the systematic process of reviewing, critiquing and synthesizing research evidence to develop best practice protocols incorporating local nuances (Weiss et al., 2018). This process is alternatively referred to guideline development. Guideline development is a small component of nurse practitioners work (Ryder et al., 2020b). Evidence identifies that nurse practitioner work is focused at leading on innovative health care transformation (Ryder et al., 2019). This manuscript proposes building on this work by presenting a translational research continuum for nurse practitioners (Figure 2) that has adopted the widely accepted interdisciplinary continuum to provide a research framework supporting nurse practitioners transformative activities. Importantly, the proposed translational research continuum for nurse practitioners retains the four phases of translational research to ensure nursing research is equivocal and mapped to accepted phases (Fort et al., 2017).
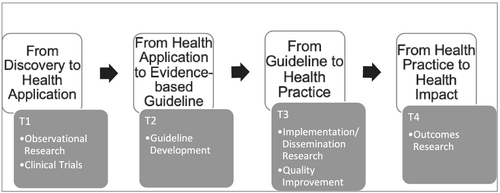
This proposed translational research continuum for nurse practitioners aligns activities with the four phases of translational research (Phases T1–T4). The continuum of research acknowledges the traditional research in the ‘discovery’ phase which is presented and applied in a small or single health care setting.
Development of the evidence or basic research is the first requirement to enable any change in practice. The first phase translation (T1) in translational research is described as discovery to application phase (Khoury et al., 2007), incorporating clinical trials and observational research, where researchers observe human behaviours in a natural setting (Lopez & Whitehead, 2013).
Development of EBP guidelines is necessary to enable evidence to be assessed for implementation to practice. Phase T2, the second translational phase, measures the value of the application in practice leading to the development of an evidence-based guideline (Khoury et al., 2007). Guideline preparation is traditionally described as an EBP or a quality improvement project as distinct from research (Carter et al., 2017; Kredo et al., 2016). However, translational research acknowledges that using knowledge after discovery localized to a specific context to enable guideline development is required to enable implementing into practice. The acknowledgement of the importance of the development of evidenced-based guidelines as part of the research continuum is essential to value the impact nurses have in translation of research into practice (Weiss et al., 2018). This supports the nurse practitioner leadership activities identified by Elliott et al. (2014) in generating standards and guidelines to support clinical practice.
Implementation science theory/models/frameworks support the third phase of translational research (T3) into health practice and focusing and reporting on the context of the specific intervention, including organisational supports required to successfully implement changes to health care delivery. Quality improvement frameworks are arguably the more familiar to nurse managers, and they continue to have a platform. However, to build the nursing research agenda, quality improvement frameworks arguably should be replaced with implantation science frameworks for nurse practitioners in the proposed translational research continuum.
The latter two phases (T3 and T4) of the translational research continuum provide an opportunity for greater operational engagement during implementation and evaluation phases of interventions. The final phase of translation research (T4) relates to the real-world application of evidence reporting on patient outcomes to health care interventions. Phases T3 and T4 are essential for the profession to ensure the sustainability of the role, by demonstrating the outcomes of nurse practitioner implementations in health care.
4.4 Key issues
Translational research and implementation science have the potential to strengthen clinical nursing research to demonstrate the strengths of nursing care. Research is essential to the nurse practitioner role. As clinical leaders, they are the ideal conduit to strengthen the scientific evidence-base for the profession in the evolving health care structures. The proposed translational research continuum outlines an evidence-based framework capturing the breadth of nurse practitioner research. Adaptation of this translational research continuum by nurse practitioners guides and directs their research activities (Weiss et al., 2018; Zullig et al., 2020). This proposed translational research continuum provides a platform to enable nurse practitioners to identify areas of research activities incorporating their health care transformation agenda. Nursing management have a significant role in nurse practitioner integration (Lowe et al., 2018), and this provides an opportunity to address the gap in research support and understanding cited previously (Ryder et al., 2019). In addition, this provides nursing management with an opportunity to benchmark nursing research through the clinical leadership role of nurse practitioner.
5 CONCLUSION
This article identifies the need for nurse practitioner research to embrace a translational research framework/continuum to expedite the implementation of new evidence into clinical practice. The transformational health care clinical leadership role of the nurse practitioner is suitably placed to lead the translation of evidence-based knowledge in the clinical practice setting. This translational research continuum for nurse practitioners has the potential to bridge the ever present theory-practice gap in their role. In addition, the framework supports that nurse practitioners, as clinical leaders, are equipped to identify where their clinical work can fit in a research framework. Embracing this translational research continuum ensures the nursing profession contributes to health care scientific knowledge, using equivocal research language and cementing the sustainability of the nurse practitioner role in health care transformation.
6 IMPLICATIONS FOR NURSING MANAGEMENT
The translational research continuum provides nursing management with a platform to benchmark nursing research across organisational research strategies. Utilizing the continuum provides nursing management with a guide to appropriate use of evidence-based implementation frameworks and incorporates evaluation and dissemination of findings into the process. The translational research continuum provides reassurances to nursing management that much of the evidence-based work already in action can be appropriately applied to a research framework. The review enhances current knowledge by explaining the importance of the nurse practitioner research role in contributing clinical nursing research to the wider health care knowledge base and proposing a modern research framework to support this.
ACKNOWLEDGEMENT
No funding has been received for this project.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
ETHICS STATEMENT
No ethical approval was required for this review manuscript.
Open Research
DATA AVAILABILITY STATEMENT
Authors elect to not share data.




