MRI topography of lesions related to internuclear ophthalmoplegia in patients with multiple sclerosis or ischemic stroke
Acknowledgments and Disclosure:
Open access funding enabled and organized by Projekt DEAL.
All authors declare no conflict of interests relevant to the manuscript.
Marie T. Kleinsorge reports no disclosures. Anne Ebert reports no disclosures. Alex Förster reports no disclosures. Claudia E. Weber reports no disclosures. Christina Roßmanith reports no disclosures. Michael Platten has a consultant relationship with Novartis, Merck, Genentech/Roche, has received nonpersonal, institutional honoraria from Medac, Merck, Novartis, TEVA, Genentech/Roche, and has research agreements with Bayer Health Care. Achim Gass has received honoraria for lecturing, and financial support for research from Bayer, Biogen, Celgene, Merck Serono, Novartis, Roche, and TEVA Neurosciences and serves on the Editorial Board of Frontiers in Neurology, section “Applied Neuroimaging” and Journal of Neuroimaging. Philipp Eisele has received travel expenses from Bayer Health Care.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Abstract
Background and Purpose
Internuclear ophthalmoplegia is a dysfunction of conjugate eye movements, caused by lesions affecting the medial longitudinal fasciculus (MLF). Multiple sclerosis (MS) and ischemic stroke represent the most common pathophysiologies. While magnetic resonance imaging (MRI) allows for localizing lesions affecting the MLF, comprehensive comparative studies exploring potential different spatial characteristics of lesions affecting the MLF are missing until now.
Methods
We retrospectively investigated MRI examinations of 82 patients (40 patients with MS and 42 patients with ischemic stroke). For lesion localization, the brainstem was segmented into (1) ponto-medullary junction, (2) mid pons, (3) upper pons, and (4) mesencephalon.
Results
Corresponding lesions affecting the MLF were observed in 29/40 (72.5%) MS and 38/42 (90.5%) stroke patients. Compared to stroke patients, MS patients had significantly more lesions in multiple locations (P < .001). Stroke patients showed more lesions at the level of the mesencephalon (P < .001), while lesions at the level of the ponto-medullary junction, mid, and upper pons did not statistically differ between the groups.
Conclusion
Our results demonstrate that multiple lesions affecting the MLF make inflammatory-demyelination due to MS more likely, while lesion localization at the level of the mesencephalon favors ischemia.
INTRODUCTION
Internuclear ophthalmoplegia (INO) is a common ocular movement disorder caused by lesions affecting the medial longitudinal fasciculus (MLF), a highly myelinated tract that connects the ipsilateral third nerve nucleus in the midbrain to the contralateral sixth nerve nucleus in the pons.1 It is characterized by impaired adduction of the ipsilateral eye and a dissociated nystagmus of the contralateral abducting eye.
Multiple sclerosis (MS) and ischemic stroke represent the most common pathophysiologies of INO.2 Even though the MLF cannot be directly visualized on conventional magnetic resonance imaging (MRI) due to its small diameter and the lack of contrast to the surrounding neural tissue,3 MRI has the ability to demonstrate lesions affecting the MLF in both MS4, 5 and ischemic stroke.2, 6 However, comparative studies exploring the potential different spatial characteristics of lesions affecting the MLF are missing until now. Therefore, the aim of this study was to investigate the topographical MRI characteristics of lesions affecting the MLF in patients with MS or ischemic stroke presenting with INO as an isolated or predominant clinical manifestation.
METHODS
Patients
We retrospectively screened our MRI- and clinical database to identify patients with an acute ischemic stroke or confirmed MS (according to the 2010 McDonald criteria) or a clinically isolated syndrome (CIS) suggestive of central nervous system demyelination presenting with a clinically confirmed INO. Exclusion criteria were under 18 years of age and missing or unsatisfactory MRI (eg, due to motion artifacts). The study was approved by the local institutional review board, patient consent was waived due to the retrospective nature of the study and the lack of patient interaction.
Magnetic Resonance Imaging
All MRI studies were performed on a 3.0T MR system (MAGNETOM Skyra/Trio, Siemens Healthineers GmbH, Erlangen, Germany; n = 8/42 stroke patients, 20/40 MS patients) or a 1.5T system (MAGNETOM Sonata/Avanto, Siemens) with varying protocols across the scanners. Protocols included for all patients axial diffusion-weighted images (DWI; mean repetition time [TR]: 4,075 milliseconds [range 3,000-5,300 milliseconds], mean echo time [TE]: 89 milliseconds [range 68-110 milliseconds], mean slice thickness [ST]: 3.5 mm [range 3-5 mm]), fluid-attenuated inversion recovery (FLAIR) images (mean TR: 8,875 milliseconds [range 8,500-9,000 milliseconds], mean TE 106 milliseconds [range 88-136 milliseconds], ST: 5 mm), and T2-weighted images (mean TR: 4,642 milliseconds [range 3,790-6,000 milliseconds], mean TE: 99 milliseconds [range 93-103 milliseconds], ST: 5 mm). Proton density images (mean TR 3,486 milliseconds [range 3,320-3,790 milliseconds], mean TE 19 milliseconds [range 11-34 milliseconds], ST: 5 mm) were available in 23/40 (57.5%) MS patients.
Postprocessing Analysis
Postprocessing analysis was performed offline. In all patients, best possible lesion identification was performed on the available MRI sequences by a doctoral student (MTK) and supervised by an experienced reader (PE) to ensure accuracy. For lesion localizations, the brainstem was segmented into (1) ponto-medullary junction, (2) mid pons, (3) upper pons, and (4) mesencephalon referring to previous studies.6, 7 In all patients, the pathway of the MLF was derived from a neuroanatomical atlas,8 lesions affecting the MLF were identified by a semiautomated assistance with the drawing tool of MRIcron. Clinical and demographical data were extracted from medical records.
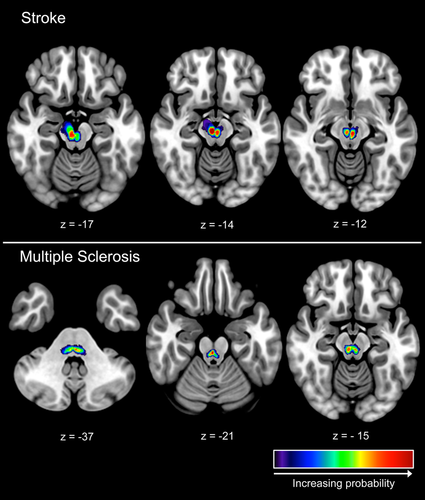
To demonstrate relative probabilities of lesions affecting the MLF, a heat map was computed for all MS and stroke patients. Therefore, images were registered to the MNI152 template using the automated FLIRT tool, part of FSL (version 5.0.2.1). Qualities of the registrations were approved by visual inspection by an experienced reader. The same registration was applied to the lesion masks. The relative probability of the lesions occurring at a given voxel location was determined by combining the corresponding masks over all patients.
Statistical Analysis
Statistical analysis was performed with IBM SPSS Statistics Version 25. Group comparisons of age and sex across the study groups were analyzed using a t-test and a chi-square-test. Between group-comparisons of lesion localization were assessed using chi-square-test and Fisher's exact test as appropriate. A P-value < .05 was considered statistically significant.
RESULTS
Overall, 82 patients were included in the analysis. These included 40 MS patients and 42 patients with an acute ischemic stroke. Stroke patients were significantly older than MS patients (78.29 ± 11.33 vs. 44.6 ± 13.79 years, P < .001), whereas sex did not differ between the two groups (stroke patients: 60% female vs. MS patients: 40% female, P = .07). Bilateral INO was significantly more frequent in MS compared to ischemic stroke (22/40 vs. 0/42, P < .001).
Mean disease duration in the MS subgroup was 9.4 ± 7.5 years with a median Expanded Disability Status Scale score of 6.0 (range 2.0-8.5). Five patients had a CIS, 15/40 relapsing-remitting MS, 14/40 secondary-progressive MS, and 6/40 primary-progressive MS. In the stroke subgroup, the median National Institute of Health Stroke Scale score was 2.0 (range 0-20). Four patients were treated with intravenous thrombolysis on admission. Stroke etiologies included small vessel disease in 13/42, large vessel disease in 6/42, cardioembolic in 10/42, peri-interventional in 1/42, and undetermined source in 12/42 patients.
Corresponding lesions affecting the MLF were observed in 29/40 (72.5%) MS and 38/42 (90.5%) stroke patients (P = .04). Compared to stroke patients, more MS patients showed lesions in multiple locations (P < .001). More stroke patients showed lesions at the level of the mesencephalon (P < .001), while the number of patients with lesions at the level of the ponto-medullary junction, mid, and upper pons did not statistically differ between the groups (P > .05 for all comparisons), see also Table 1. Figure 1 shows a heat map representation of lesion probabilities superimposed on an MNI152 template.
| Stroke | Multiple Sclerosis | P-Value | |
|---|---|---|---|
| Ponto-medullary junction | 0/42 | 1/40 | .488 |
| Mid pons | 1/42 | 4/40 | .196 |
| Upper pons | 14/42 | 7/40 | .131 |
| Mesencephalon | 19/42 | 4/40 | .001 |
| Multiple lesions | 4/42 | 13/40 | .014 |
| No lesion | 4/42 | 11/40 | .047 |
DISCUSSION
In this study, we investigated topographical MRI characteristics of lesions affecting the MLF in patients with MS and ischemic stroke. Our results demonstrate that compared to stroke patients, significantly more MS patients showed lesions in multiple locations. With regard to lesion localization, more stroke patients showed lesions at the level of the mesencephalon. There are several points noteworthy in this regard.
In MS, the brainstem represents a typical predilection site for lesion development and INO is seen in ∼ 30% of MS patients.4, 9 As expected, bilateral INO was present significantly more often in MS than in stroke patients.10, 11 However, even though MS is nearly always the etiology of bilateral INO in young patients,12 about a third of all cases are caused by ischemic stroke and commonly observed in older patients.6 Acute ischemic brainstem stroke accounts for 10-15% of all ischemic strokes.13 While pontine infarction represents the most common type,14 in our study, the mesencephalon was frequently affected by ischemic stroke lesions causing INO, a finding that can be explained by the anatomic pathway of the MLF. In the mesencephalon, the MLF lies more ventral near the midline close to the cerebral aqueduct, while in the pons and medulla, it lies more dorsal just ventral to the fourth ventricle.1 It seems conceivable that occlusion of small arteries frequently affects the more ventrally located MLF in the mesencephalon. However, in line with previous studies, MS lesions affecting the MLF were present in the mid and upper pons and the mesencephalon.5, 15, 16 Since MS lesions typically develop in periventricular regions, the high frequency of lesions in these localizations is probably a result of the close-by periventricular location to the fourth ventricle and the aqueduct.12
However, this study is not without limitations: This was a retrospective study and the sample size was relatively small. Due to the retrospective character of our study, MR images were acquired on different scanners using different field strengths, parameters, and protocols. Therefore, the interpretation of our results should be done cautiously. Compared to ultra-high-field MRI, the MLF cannot be directly visualized on conventional images acquired on a 1.5 T or 3.0 T scanner due to its small diameter and the lack of contrast to the surrounding neural tissue.3 Therefore, lesions affecting the MLF were carefully investigated; however, segmentation of small and fine brainstem structures remains challenging due to “pseudo-hyperintensity” of the MLF and distracting adjacent sequences (eg, of the cerebrospinal fluid).17