Three-dimensional printing enhances preparation for repair of double outlet right ventricular surgery
Abstract
Objective
To assess the clinical value of three-dimensional (3D) printing technology for treatment strategies for complex double outlet right ventricle (DORV).
Methods
Twenty-five patients with complex double outlet right ventricle were enrolled in this study. The patients were divided into two groups: 3D printing group (eight patients) and a non-3-D printing control group (17 patients). The cardiac images of patients in the 3D printing group were transformed to Digital Imaging and Communications and were segmented and reconstructed to create a heart model. No cardiac models were created in the control group. A Pearson coefficient analysis was used to assess the correlation between measurements of 3D printed models and computed tomography angiography (CTA) data. Pre-operative assessment and planning were performed with 3D printed models, and then operative time and recovery time were compared between the two groups.
Results
There was good correlation (r = 0.977) between 3D printed models and CTA data. Patients in the 3D printing group had shorter aortic cross-clamp time (102.88 vs 127.76 min, P = 0.094) and cardiopulmonary bypass time (151.63 vs 184.24 min; P = 0.152) than patients in the control group. Patients with 3D printed models had significantly lower mechanical ventilation time (56.43 vs 96.76 h, P = 0.040) and significantly shorter intensive care unit time (99.04 vs 166.94 h, P = 0.008) than patients in the control group.
Conclusions
3D printed models can accurately demonstrate anatomic structures and are useful for pre-operative treatment strategies in DORV.
1 INTRODUCTION
Double outlet right ventricle (DORV) is a type of cono-truncal anomaly in which both the aorta and the pulmonary artery arise from the right ventricle.1 The anatomy of DORV differs from patient to patient so that a thorough understanding of spatial anatomical structures is essential for the surgical management of DORV.
The 3D printing technique is a process of creating 3D solid objects from digital files and this technology has been applied to cardiovascular surgery in recent years. 3D printing technology can print precise heart models which can provide detailed information of intracardiac and extracardiac structures. This has aided in the surgical resection of cardiac tumors and has been used to assist in the repair of type A dissections.2, 3 This study was undertaken to assess the role of 3D printed models in planning pre-operative strategies for the surgical repair of DORV.
2 METHODS
2.1 Patient selection
This study was approved by the Institutional Review Board in Henan province. From July 2015 to December 2016, 25 patients with DORV, aged 1 month to 2 years, were enrolled in the study. Patients were divided into two groups. 3D printing group: eight patients (three males, five females, mean age 13.62 ± 4.47 months). Control group: 17 (11 males, six females, mean age 22.00 ± 5.81 months) underwent surgery without 3D printing (Table 1).
| Variables | Total cohort (n = 25) | 3D printing (n = 8) | Control group (n = 17) | P-value |
|---|---|---|---|---|
| Mean age, years | 19.32 ± 6.65 | 13.62 ± 4.47 | 22.00 ± 5.81 | 0.002 |
| Mean weight, kg | 10.64 ± 2.90 | 8.10 ± 0.97 | 11.81 ± 2.77 | 0.001 |
| Relationship between VSD and great vessels | 1.000 | |||
| Subaortic | 6 | 2 | 4 | |
| Subpulmonary | 3 | 1 | 2 | |
| Remote | 16 | 5 | 11 | |
| Pulmonary stenosis | 8 | 3 | 5 | 1.000 |
| Previous operation | 1.000 | |||
| PA banding | 2 | 1 | 1 | |
| Modified B-T shunt | 1 | 0 | 1 | |
- Values are mean ± standard deviation. AO, ascending aortic; B-T shunt, Blalock-Taussig shunt; PA, pulmonary artery; VSD, ventricular septal defect.
2.2 Image acquisition
All patients underwent echocardiography and contrast-enhanced computed tomography angiography (CTA) by dual-source CT (SOMATOM Definition Flash, Munich, Germany). The nonionic contrast medium (300 mg iodine/mL) at a volume of 1.5-2.0 mL/s was injected through the peripheral veins using an automatic injector at a speed of 0.8-1.2 mL/s. The scan was performed at 80-120 kV with automatic mAs modulation depending on age and weight. Electrocardiography (ECG) gating was utilized to enhance image acquisition (Table 1).
2.3 3D printing
The image data were formatted in DICOM and then the 3D virtual model was postprocessed using segmentation software (Mimics, Materialise, Leuven, Belgium) to obtain various anatomical structures. The generated 3D digital model was exported as a stereolithographic file and printed at a 1:1 scale using a ZPrinter 650 (Z Corporation, Burlington, MA).
2.4 Model evaluation
Measurements of the size of the ventricular septal defect (VSD) and diameter of the aortic arch and pulmonary artery were taken from 3D printed models. These measurements were compared with CTA data. The surgeons evaluated the 3D models to determine the relationship of the great arteries, the relationship between the VSD and great arteries, and determine the distance between the pulmonary valve and the VSD. The 3D printing group was compared to the control group in terms of operative time, cardiopulmonary bypass (CPB) time, aortic cross-clamping (ACC) time, mechanical ventilation time, and intensive care unit stay post-operatively.
The indications for extubation following surgery were as follows: (i) Hemodynamics and cardiac function were stable, and there were no serious arrhythmias; (ii) there was no significant effect on the circulatory function during spontaneous breathing; (iii) in the artery blood gas analysis, arterial oxygen partial pressure (PaO2) was more than 70 mmHg (1 mmHg = 0.133 kPa), arterial carbon dioxide partial pressure (PaCO2) was less than 45 mmHg, and pH was arranged from 7.35 to 7.45, when fraction inspired oxygen concentration was less than 0.4; (iv) patients were conscious and had no serious neurological complications; and (v) there was no active bleeding and the quantity of thoracic drainage was less than 2 mL/kg/h. The indications for transferring out of the intensive care unit (ICU) were as follows: (i) Hemodynamics was stable and blood pressure was normal with low dose or without vasoactive drugs; (ii) cardiac rhythm was sinus rhythm or regular. Blood pressure was normal without a temporary pacemaker; (iii) renal function was normal without peritoneal dialysis or high-dose intravenous diuretics.
2.5 Statistics
A Pearson correlation analysis was used to evaluate the agreement between 3D models and the CTA measurements. The t-test was used to compare means and standard deviations. The categorical variable was performed with the χ2 test or the Fisher's exact test. Analysis was done using a statistical software (SPSS, verson 19.0, IBM Corp, Armonk, NY). A P value <0.05 was considered statistically significant.
3 RESULTS
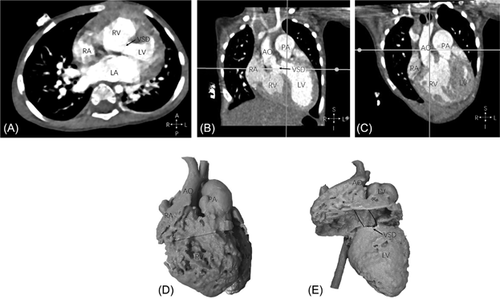
A Pearson analysis showed good correlation between the CTA and 3D data with a Pearson correlation coefficient of 0.977. The size and location of the VSD, the relationship between the main pulmonary artery, and the aorta were clearly demonstrated in the 3D models (Figure 1).
The relationship between the VSD and great vessels are shown in Table 1. In the 3D group, pulmonary artery banding was undertaken in one patient. In the control group, one patient underwent Pulmonary artery banding and a modified Blalock-Taussig shunt was performed in another patient.
In the 3D printing group, an intracardiac tunnel connected to the aorta was created in two cases. Four cases were treated by an intracardiac tunnel connected to the aorta and the right ventricular outflow tract enlargement. Two cases underwent an intracardiac tunnel connected to the pulmonary artery and the arterial switch operation. In the control group, six cases underwent an intracardiac tunnel connected to the aorta. An intracardiac tunnel connected to the aorta, along with right ventricular outflow tract enlargement, was performed in seven cases. Four cases were treated by an intracardiac tunnel connected to the pulmonary artery and the arterial switch operation. There were no early deaths in the 3D printing group. There was one early death (30 days after surgery) due to the low cardiac output syndrome and one case required reoperation for bleeding in the control group (shown in Table 2).
| Group | 3D printing | Control | P-value |
|---|---|---|---|
| Operative strategy | 1.000 | ||
| LV-AO | 2 | 6 | |
| LV-AO + RVOT enlargement | 4 | 7 | |
| LV-PA + ASO | 2 | 4 | |
| Operative time, min | 251.75 ± 35.80 | 285.06 ± 83.40 | 0.294 |
| CPB time, min | 151.63 ± 37.15 | 184.24 ± 56.44 | 0.152 |
| ACC time, min | 102.88 ± 31.42 | 127.76 ± 33.98 | 0.094 |
| Mechanical ventilation time, h | 56.43 ± 19.74 | 96.76 ± 50.26 | 0.040 |
| ICU stay, h | 99.04 ± 16.13 | 166.94 ± 90.30 | 0.008 |
| Renal insufficiency | 1 | 1 | 1.000 |
| Pulmonary infection | 1 | 3 | 1.000 |
| Low cardiac output syndrome | 1 | 2 | 1.000 |
| Reoperation | 0 | 1 | 1.000 |
| Early mortality | 0 | 1 | 1.000 |
- Values are mean ± standard deviation. ACC, aortic cross-clamping; CPB, cardiopulmonary bypass; ICU, intensive care unit; LV-AO, intracardiac tunnel connect to aorta; LV-AO + RVOT enlargement, intracardiac tunnel connect to aorta + right ventricular outflow tract enlargement; LV-PA + ASO, intracardiac tunnel connect to pulmonary artery + arterial switch operation.
In the 3D printing group, the operative time (251.75 min) was lower than that in the control group (285.06 min, P = 0.294), the CPB time (151.63 min) was shorter than in the control group (184.24 min, P = 0.152), and the ACC time was shorter in the 3D printing group than in the control group (102.88 vs 127.76 min, P = 0.094). The ICU time was significantly shorter in the 3D printing group than in the control group (99.04 vs 166.94 h, respectively, P = 0.008), and the mechanical ventilation time was significantly shorter in the 3D printing group than in the control group (56.43 vs 96.76 h, respectively, P = 0.040; Table 2).
4 DISCUSSION
The surgical approach to DORV can be challenging, especially in DORV with a non-committed ventricular septal defect and ventricular imbalance.4 Complicated relationships in patients with complex DORV make pre-operative assessment difficult.
The surgical planning of DORV relies on the specific understanding of anatomical spatial relationships. It is difficult to use traditional imaging techniques to evaluate the complex cardiac spatial anatomy.5
3D printing technology, which is also known as stereolithography, can create precise models which show accurate anatomical spatial relationships.6 The complex anatomic structures including the location of VSDs and the relationships of great vessels were precisely demonstrated in all 3D models. It is possible to access the potential baffle pathways with the 3D models.
In patients with DORV, 3D printed models demonstrated the complex anatomy which is useful in pre-operative evaluation in patients with complex DORV.7 In transverse aortic arch hypoplasia, 3D printed models have improved interventional strategies in stenting.8
In this study, intracardiac and extracardiac anatomies were clearly demonstrated in 3D printed models. 3D printed models can be used to simulate techniques before surgery in DORV. Surgical planning based on 3D printing could save about 30 min during surgery and decrease bypass and cross clamp times. Mechanical ventilation time and stay in the cardiac intensive care unit were significantly lower than in the control group.
The small sample size is a limitation of this study. To achieve high-quality images, images were acquired with ECG gating, which might increase X-ray exposure. The material for the models in this study was polylactic acid which is different from cardiac tissue. Cardiac valve leaflets cannot be well demonstrated in 3-D models.
5 CONCLUSIONS
3D printed models accurately replicate patients' anatomic structures and are helpful in surgical planning in complex DORV. 3D printing technology has the potential to improve surgical efficiency and post-operative outcomes.
ACKNOWLEDGMENT
Programs for Medical Science and Technology Development of Henan Province, Grant number: 162102310023.