Adult-onset Still's disease presenting with “pencil sketch-like” arrangement of papules and geographic pigmentation
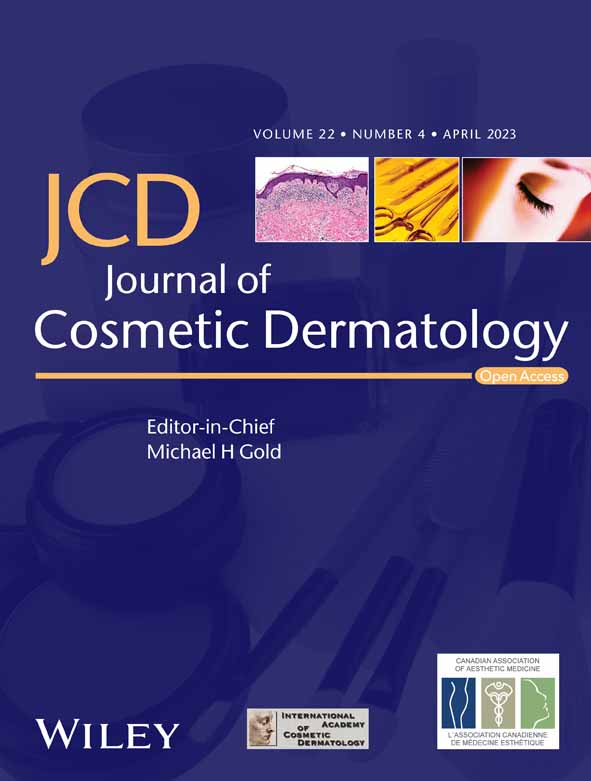
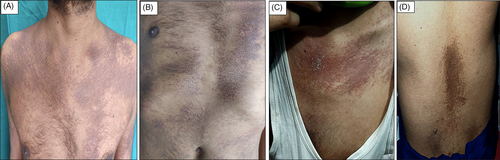
Adult-onset Still's disease is a rare entity with varied clinical manifestations. We encountered two cases of adult-onset Still's disease (AOSD) with bizarre pigmentation and grouped papules. Case 1 was a 28-year-old man with recurrent itchy papules over trunk and extremities for past 3 months. Case 2 was a 24-year-old man who presented with high-grade fever without chills and with poly-arthralgia for 1.5 months and itchy papules over trunk and extremities for past 1 month. Cutaneous examination of both cases revealed similar findings in the form of multiple closely set erythematous and lichenoid, follicular and non-follicular papules predominantly distributed over upper trunk in a bizarre linear manner and over the extensor aspects of bilateral extremities proximally. These lesions were admixed with geographic pigmentation present primarily on trunk, more extensively in case 1 (Figures 1A–D). Systemic examination was unremarkable in both the cases. Skin biopsy was performed with clinical differentials of atypical pityriasis rubra pilaris, follicular mycosis fungoides, secondary syphilis, Reiter's disease, dermatomyositis, and adult-onset Still's disease. Histological findings (as shown in Figure 2A,B) were supportive of a clinical diagnosis of AOSD. A definitive diagnosis of adult-onset Still's disease was made on the basis of Yamaguchi diagnostic criteria consisted of fever, arthralgia, typical rash and leucocytosis as major and sore throat, lymphadenopathy and/or splenomegaly, liver dysfunction, absence of rheumatoid factor and antinuclear antibody as minor criteria. Requiring five or more criteria including two or more major criteria yielded 96.2% sensitivity and 92.1% specificity.1 The first patient fulfilled three major and four minor, and the second fulfilled three major and two minor criteria. Complete clinical features and investigations are detailed in Table 1. Initially, both patients were started on non-steroidal anti-inflammatory drugs (paracetamol and aceclofenac) and topical steroids with significant improvement in joint pains and subsidence of papular lesions leaving behind post-inflammatory hyperpigmentation. Case 1 relapsed, within 2 months of stopping treatment, with joint pains and multiple papular eruptions, both of which subsided completely following oral prednisolone (0.5 mg/kg/day) tapered over 1 month. Subsequent relapse was treated with oral methotrexate (10 mg/week), and the patient remains symptom free at 2 years of follow-up. Case 2 is free of any lesions at 6-month follow-up. Adult-onset Still's disease (AOSD) is complex disorder with incompletely understood etio-pathogenesis. Even though a plethora of atypical cutaneous manifestations of AOSD have been reported in literature ranging from persistent erythematous to salmon-pink eruption to dermatomyositis-like and lichen amyloidosis-like pigmentation,2 a peculiar eruption likened to our patients does not find mention and therefore needs emphasis. A diagnosis of AOSD requires a combination of clinical and laboratory features, and due to its low prevalence, it is often misdiagnosed. In the right clinical context, a skin biopsy, though non-specific, may reveal minor clues like dyskeratotic cells in the upper epidermis and upper dermal neutrophilic and lymphocytic infiltrate indicating a possibility of AOSD.2 In view of paucity of literature, no consistent guidelines exist on the management of AOSD. The reported poor prognostic factors include systemic complications at the time of diagnosis such as pleuritis and interstitial pneumonia, failure of fever to respond to systemic prednisolone (at 1 mg/kg/day for 3 days) and elevated ferritin levels.3 Unusual clinical presentations practically seem more common in AOSD which may be in view of our incomplete understanding of the disorder per se. Hence, it may be inferred that AOSD can be kept as a clinical differential not only for blanchable maculopapular eruptions but also for the follicular papules arranged in a bizarre “pencil sketch-like” arrangement associated with geographic pigmentation.
| Case details | Case 1 | Case 2 |
|---|---|---|
| Clinical features | ||
| Age of the patient (years) | 28 | 24 |
| Total disease duration (months) | 3 | 1.5 |
| Duration of cutaneous eruption (months) | 3 | 1 |
| High grade fever | + | + |
| History of sore throat | + | + |
| Evening rise of temperature | + | + |
| Polyarthralgia (large joints) | + | + |
| Migratory arthralgia | + | + |
| Morning stiffness | - | - |
| Laboratory findings | ||
| Total leucocyte count (cells/μl) | 16 000 | 28 100 |
| Neutrophils (%) | 84 | >80 |
| Liver function tests | Deranged | Deranged |
| Kidney function tests | Normal | Normal |
| Ferritin level (ng/ml) | 2797 (normal range: 15–150) | 1518 (normal range: 30–400) |
| Rheumatoid factor (IU/ml; positive > 14) | - | - |
| USG abdomen | Borderline hepatomegaly | No abnormality detected |
| ESR (mm/h) | 100 | 60 |
| C-reactive protein (normal range 0–6) | 74.58 | 31.2 |
| LDH (u/L; normal range 230–460) | 410 | 620.1 |
| Anti-streptolysin O (normal range 0–200) | - | 728 |
| ANA | - | - |
| Yamaguchi's criteria | 3 Major + 4 Minor | 3 Major + 2 Minor |
| Relevant histopathological findings | Few necrotic keratinocytes higher up in the epidermis and eosinophilic spongiosis | Basal cell vacuolization with mild perivascular lympho-plasmacytic infiltrate and pigment incontinence in superficial dermis |
AUTHOR CONTRIBUTIONS
S.S. designed the study. F.A., M.N., and S.K. contributed essential reagents or tools. F.A., U.L., and S.S. wrote the paper.
CONFLICT OF INTEREST
None declared.
ETHICAL APPROVAL
None.
PATIENT CONSENT
Obtained.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.