Androgens and COVID-19
Funding information
None.
Abstract
Background
The humans have been disproportionately affected by the coronavirus disease (COVID-19) pandemic. The novel coronavirus or the severe acute respiratory syndrome coronavirus 2 (SARS-COV2) causing coronavirus disease (COVID-19) has spread across the globe. Androgens have been suggested to have a role in COVID-19 pathogenesis.
Objective
The objective of this review article is to study the link between androgens and COVID-19.
Methodology
PubMed and Google Scholar search was performed to retrieve literature related to the topic. Review articles, clinical trials, retrospective studies, observational studies, and case–control studies were considered for the review.
Results
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infected men are more inclined to be hospitalized for intensive care unit (ICU) as compared with women. This difference in the ICU admissions provides some clue for possible influence of androgens in the severity of COVID-19. The contribution of androgen and androgen receptor in COVID-19 disease and its severity, as well as the numerous medications targeting androgen and its receptor for lowering COVID-19 disease severity, are discussed in this review. Available literature suggests the role of androgen in the pathogenesis and severity of COVID-19. Sensitivity for androgen may be an important factor in regulating the severity of COVID-19 disease.
Conclusion
There is a scope for the development of COVID-19 treatments based on androgen suppression. Clinical trials may furnish pivotal data and add more evidence-based options for the management of COVID-19.
1 INTRODUCTION
The novel coronavirus or the severe acute respiratory syndrome coronavirus 2 (SARS-COV2) causing coronavirus disease (COVID-19) has spread over the world, affecting millions of individuals. The truncated rates of prepubertal deaths and the certitude that SARS-CoV-2 infected men are more inclined to be hospitalized in the intensive care unit (ICU) as compared with women are consistent results. It should be kept in mind that variations in smoking, cardiovascular disease, and drinking habits between men and women are not the only facets which lead to more disease severity in men.1, 2 Similar gender difference was identified in the Middle East respiratory syndrome outbreak, where variations in sex hormones have been demonstrated to have a role in illness susceptibility.3 Androgens are chemically steroids which are produced in both genders, and their endogenous levels escalate during puberty. Males have larger levels of androgens than females, which contributes to increased severity of COVID-19 disease.4 The discovery of SARS-COV-2 entry sites piqued curiosity in the involvement of androgens. Following that, research has revealed that androgens have a contribution in the progression of COVID-19 disease and a noteworthy quota of bedridden patients have an underlying androgen-mediated condition.5, 6
The objective of this article is to discuss the link between androgens and COVID-19. PubMed and Google Scholar search were performed to retrieve literature related to the topic. Review articles, clinical trials, retrospective studies, observational studies, and case–control studies were considered for the review.
2 NOVEL CORONAVIRUS DISEASE AND ANDROGEN
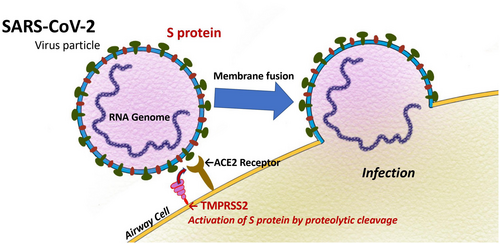
The new coronavirus infects host cells by priming spike proteins with the enzyme transmembrane protease serine 2 (TMPSS2) and connecting to ACE2 receptors. Cellular entry of the virus is facilitated by ACE2.7 The TMPRSS2 gene codes for transmembrane protease, serine 2. TMPSS2 gene expression is increased by androgens.8 TMPRSS2 expression is reduced by androgen deprivation therapy (ADT), used for the management of treat prostate cancer patients. Testosterone and TMPPRSS2 expression influence and change the propensity of the novel coronavirus to infect cells and the spike proteins' affinity to hold on to the ACE2 receptors.9 All androgens work via attaching to the androgen receptors alias nuclear receptor subfamily 3, group C, member 4 abbreviated as NR3C4.10 The AR gene (Xq11–12) codes for androgen receptors. This gene's variants are linked to divergent androgen responsiveness.11 This sort of changes intensify the likelihood of androgen conciliated diseases viz. androgenic alopecia (AGA) and prostate cancer. COVID-19 disease has also been linked to androgen sensitivity changes. AGA has been linked to progression of COVID-19 disease to severe forms especially in hospitalized patients. In addition, prostate cancer patients who were being managed by ADT were less likely to be affected from severe COVID-19 infection in contrast to prostate cancer without ADT therapy.12
The interconnection between androgen levels in circulation, cell's androgen sensitivity, and COVID-19 disease gravity is not at all plain sailing. As androgens upregulate the transcriptional activity of androgen receptor, it can be made out that that androgen impecunious patients will carry a lesser level of activated androgen receptors and thus the transcription capability of TMPRSS2 would be contracted and in return there would be less risk of novel coronavirus ingress in to host cells. Howbeit, reports from European countries such as Germany and Italy had contrasting end results. Testosterone magnitude was less in most of COVID-19 patients bedridden in ICU.13, 14 While both research outcome had impediments viz. absence of control groups or testosterone levels preceding COVID-19 infection, and hence, the outcome and conclusion need pondering. Customarily, androgen levels in blood correspond to androgen sensitivity, but scores of elements can out-turn this consortium.15 Even though testosterone levels get truncated with senility, there is no exact gold-standard that foretells androgen-sensitive phenotypes, and management is chiefly based on symptoms.16 A plausible factor that can augment SARS-CoV-2 infection is inflammation. Systemic inflammation and high levels of pro-inflammatory cytokines correlate with truncated androgens amount in males both young and old.17, 18Furthermore, there is proof that interpersonal disparity in androgen receptor's susceptibility as a result of polymorphisms in cysteine adenine guanine (CAG) can result in sensitivity even with truncated testosterone levels.19, 20
Figure 1 briefly explains the possible role of androgens in the pathogenesis of COVID-19.
The DNA-binding domain, the ligand-binding domain, and the transactivation domain are the three primary domains of the androgen receptor. A polymorphic CAG nucleotide repeat region is found in the N-terminal transactivation domain. Intriguingly, the length of polymorphic CAG nucleotide repeats is linked to the pathophysiology of prostate cancer, since shorter CAG repeats negatively correlate with androgen receptor expression and, as a result, increase the risk of prostate cancer.21 Increased androgen receptor expression, which promotes TMPRSS2 transcription, may increase the likelihood of developing a severe COVID-19 disease. Furthermore, CAG repeat length was suggested as a possible cause of racial differences in COVID-19 death rates. In comparison with other ethnic groups in the United States, African Americans have been disproportionately afflicted by SARS-COV-2. This ethnic group appears to have a higher risk of prostate cancer progression and has shorter CAG repeats. An in vitro diagnostic test clinical trial based on the length of CAG repeats is now being conducted to assess the severity of COVID-19 disease.22, 23 It's worth noting that the implications of the length of the polymorphic CAG repeat sequence in lung tissue are still unclear, and there's no clinical evidence to back up this theory. As a result, the outcomes of the ongoing trials are critical in determining the mechanism's potential as a COVID-19 severity measure.
3 ANDROGEN SUPPRESSING MANAGEMENT FOR COVID-19
Various medications have been proposed for treatment since the beginning of the pandemic, but no universal therapy has been licensed. However, some drugs, such as hydroxychloroquine, nitric oxide (NO), and dexamethasone, have garnered attention due to their allegedly helpful benefits. Antimalarial medicine hydroxychloroquine has been shown to reduce the risk of SARS-COV-2 infections and block virus entrance.12, 24 The FDA first approved this medicine on a temporary basis; however, it was eventually revoked owing to complications and documented deaths.25 The role of androgen, on the other hand, could be important. Hydroxychloroquine has also been shown to reduce testosterone output gradually over time. NO also has an effect on androgen receptor activity. NO synthesis and activities are influenced by androgen receptors to some extent and inhibiting these receptors lowers NO production. Furthermore, NO inhibits the actions of androgen receptor promoters, which can alter the expression of TMPRSS2 gene and ACE2 gene, reducing the ability of virus to enter host cells. SARS-COV-2 replication has been demonstrated to be inhibited by NO. NO also has an effect on the spike proteins contained around the virus and their interactions with ACE2, implying that it has several functions against COVID-19. These findings suggest that androgen pathways may be the key mechanism underlying the observed NO positive effect.5
The prefatory outcomes of the randomized evaluation of COVID-19 therapy (RECOVERY) trial were recently hailed as a scientific success, and the trial's encouraging results drew international attention. Dexamethasone, a glucocorticoid reduced mortality in patients in ventilator by one-third and in those under oxygen therapy without ventilators by one-fifth.26 In human patients and animal models, dexamethasone has been shown to reduce testosterone synthesis. Lower androgen levels may play a role in the positive benefits of dexamethasone, but these initial outcomes should be regarded with caution.12
Screening for drugs that can lower ACE-2 levels demonstrated that many of the medications can fire at the androgen signaling pathway. Furthermore, androgen inhibiting medications were capable of lowering ACE2 levels, implying that this method is helpful.27 Androgen suppression has been shown to have therapeutic potential in ongoing clinical trials. Because the majority of these medications are popular and widely accessible, if approved, they can provide a therapy that is both accessible and effective. Table 1 shows the classes of anti-androgen drugs with their examples.
| Class of drugs | Drug name |
|---|---|
| 5-α reductase inhibitors | Dutasteride, Finasteride |
| Androgen receptor blockers | Apalutamide, Bicalutamide, Darolutamide, Enzalutamide, Flutamide, Nilutamide, Proxalutamide, Abiraterone, Canrenone, Cyproterone, Nomegestrol, Spironolactone |
| TMPRSS2 blocker | Camostst, Nafamostat, Bromhexine |
4 REVIEW OF RECENT STUDIES
Several studies have pointed toward the association of androgens with COVID-19. McCoy et al.28 found extended CAG repetitions in the androgen receptor to be linked to poor outcomes. In another study McCoy et al.29 found that 5-alpha reductase inhibitors are correlated with curtailed frequency of COVID-19 manifestations in men with androgenetic alopecia. According to Baldassarri et al.30 extended CAG repetitions are linked with poor outcome and elevated testosterone levels in men who were aged <50 years. Wabier et al.6 found high generality of AGA in SARS-CoV-2 bedridden patients. In a study by Goren et al 8% males undergoing anti-androgen therapy were admitted to the ICU due to COVID-19 as compared with 56% for men who were not under the same.31
In a study conducted by Vicenzi et al.32 survival rate among 30 patients who used canrenone (steroidal antimineralocorticoid) was 87% as compared with 6% in 39 controls. According to the results of the EAT-DUTA AndroCoV trial addition of dutasteride early to azithromycin-nitazoxanide combination significantly improves outcome of COVID-19 infected patients.33 Another study reported that advanced stages of AGA are linked with COVID-19 test positivity in severe COVID-19.34 Association of alopecia and gray hairs with COVID-19 severity has also been reported.35 Ramos et al.35 concluded that AGA was associated with poor por prognosis is COVID-19 patients. In a cross-sectional case–control study, Cadegiani et al discovered that hyperandrogenic women have more symptomatic COVID-19.36 Higher rates of conjunctival congestion, upper back pain, anorexia, drug cough, low grade fever, and few other symptoms were significantly more in patients with hypeandrogenic women.36
Ansarin et al.37 established that there were decreased number of ICU hospitalizations and mortalities in the quota randomized to bromhexine supplemental therapy, when compared with hydroxychloroquine for hospitalized COVID-19 pneumonia patients. In this open-label randomized clinical trial study, oral bromhexine was given as 8 mg 3 times daily in addition to standard treatment (n = 39) versus only standard treatment (n = 39). Bromhexine was significantly better than control group in terms of primary outcome of admission rate in ICU admissions (P = 0.006), intubation (P = 0.007), and mortality (P = 0.027).37 In another open label randomized study, Li et al. evaluated efficacy and safety of oral bromhexine 32 mg three times a day for 2 weeks in patients with COVID-19. In this study, 18 patients with moderate COVID-19 received either bromhexine in addition to the routine care (n = 12) whereas others (n = 6) received routine care acted as control group. Patients receiving bromhexine showed improvement in chest computed tomography (CT) scan, truncated oxygen requirement, lower liver injury, and a swift discharge rate. There was not statistically significant difference between two groups. Small sample size is an important limitation of this study.38
5 CONCLUSION
TMPRSS2 gene is influenced by androgen activity. As ACE2 gene and TMPRSS2 gene are essential for SARS-CoV-2 entrance into host cells, these could be used as COVID-19 therapeutic targets. Androgen's TMPRSS2-mediated effects may account for both the low fatality rate in prepubescent children and the gender variations in COVID-19 disease. Sensitivity for androgen may be a key factor in regulating the severity of COVID-19 disease, and androgen's sensitivity investigations can aid in foretelling patient outcomes. Although there is still a lot of room for the development of COVID-19 treatments based on androgen suppression to be developed, proceeding trials will furnish pivotal data that will lead to better management options.
ACKNOWLEDGMENTS
Open Access funding enabled and organized by ProjektDEAL.[Correction added on 21 July 2022, after first online publication: ProjektDEAL funding statement has been added.]
AUTHOR CONTRIBUTION
Kinnor Das, Anant Patil, Andy Goren, and Clay J. Cockerell involved in writing and revising the manuscript. Mohamad Goldust involved in conception, writing, review, and revising the manuscript.
CONFLICT OF INTEREST
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
ETHICAL APPROVAL
This work is a review article and there is no ethical approval needed for it.
DISCLAIMER
We confirm that the manuscript has been read and approved by all the authors, that the requirements for authorship as stated earlier in this document have been met and that each author believes that the manuscript represents honest work.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




