The role of family support in medication adherence and quality of life among tuberculosis patients: A scoping review
Abstract
Background
Tuberculosis (TB) remains one of the leading infectious diseases globally, causing high mortality rates. A significant factor contributing to this issue is nonadherence to treatment, which is influenced by family support and impacts the quality of life (QoL) of patients.
Aim
The purpose of this study was to describe the role of family support in enhancing medication adherence and improving QoL in individuals with TB.
Methods
This study utilized a scoping review method to examine literature from the PubMed, Scopus, and EBSCO databases. The keywords used in the search included “social support OR online social support OR perceived social support OR family support” AND “Tuberculosis OR TB OR TBC” AND “medication adherence OR medication compliance OR drug adherence OR drug compliance OR adherence OR compliance OR lost to follow-up” AND “QoL OR HRQoL OR health-related QoL.” The inclusion criteria were full-text articles in English, primary research studies, and publications from the last 10 years (2012–2022).
Results
Thirteen articles met the inclusion criteria, with sample sizes ranging from 50 to 1342 respondents, predominantly using cross-sectional methods. The study found that family support is crucial in promoting medication adherence and positively influencing the QoL of TB patients. Family members provide emotional and practical support, including supervision of medication intake and encouragement of healthy habits. This support enhances patients' confidence, motivation, and overall treatment outcomes.
Conclusions
The findings underscore the indispensable role of family support in addressing the complex interplay between medication adherence and QoL for individuals with TB.
1 INTRODUCTION
Tuberculosis (TB) remains a significant global public health challenge, recognized as one of the top 10 causes of death worldwide (Addo et al., 2022). TB is a communicable infectious disease that continues to cause high mortality rates, particularly in low- and middle-income countries (WHO, 2021; Yusmaniar & Kurniawan, 2020). According to the World Health Organization (WHO), more than 80% of TB cases occur globally, with almost 90% of these cases concentrated in 84 countries (WHO, 2023). In 2020, it was estimated that 10 million people contracted TB, including 5.6 million men, 3.3 million women, and 1.1 million children. Thirty countries with a high burden of TB account for 86% of new TB cases, with two-thirds of these cases reported in eight countries: India, China, Indonesia, the Philippines, Pakistan, Nigeria, Bangladesh, and South Africa (WHO, 2023).
The effective management and treatment of TB pose significant challenges due to the lengthy treatment regimens required (Lutfian & Nurfika, 2024; Nezenega et al., 2020). Standard TB treatment typically lasts 6 months for drug-sensitive TB and can extend to 2 years for drug-resistant TB (Yusmaniar & Kurniawan, 2020). This prolonged treatment duration often leads to various side effects, which, coupled with the extended commitment required, can result in decreased adherence among TB patients. Nonadherence to TB treatment is a major cause of treatment failure and relapse, which further exacerbates the public health burden of the disease (Addo et al., 2022; Yusmaniar & Kurniawan, 2020). Several factors contribute to the discontinuation of treatment among TB patients, including the misconception of being cured, geographical barriers to accessing healthcare facilities, and notably, the lack of family support (Araia et al., 2021).
Family support plays a crucial role in the treatment adherence and overall quality of life (QoL) of TB patients. Adequate support from family members can significantly enhance a patient's commitment to the treatment regimen, thereby improving treatment outcomes (Chen et al., 2020; Lestari et al., 2020). Conversely, low levels of family support are associated with poor adherence to treatment, which can adversely affect patients' recovery and QoL (Chen et al., 2020). Encouragement and assistance from family members can help mitigate the psychological and logistical challenges faced by TB patients, promoting better health outcomes (Rachmawati et al., 2019).
Previous systematic reviews have explored various factors contributing to nonadherence in TB patients (Pariyana et al., 2020; Shringarpure et al., 2016). However, there has been a paucity of comprehensive reviews focusing specifically on the role of family support in enhancing treatment adherence and QoL among TB patients. This scoping review aims to fill this gap by systematically examining the existing literature on the impact of family support on medication adherence and QoL in TB patients. By providing an in-depth analysis of this critical factor, this review seeks to highlight the importance of family involvement in the treatment process and its potential to improve health outcomes for TB patients (Pariyana et al., 2020). This updated review not only addresses the need for a deeper understanding of the role of family support but also aims to provide valuable insights for healthcare practitioners and policymakers. Enhancing family support mechanisms could be a key strategy in improving treatment adherence and QoL for TB patients, ultimately contributing to better disease management and control efforts globally. The findings of this review are intended to inform future research, clinical practice, and policy development aimed at optimizing TB treatment outcomes through strengthened family support systems.
2 METHODS
2.1 Study design
This study was designed as a systematic scoping review. A scoping review is a methodological technique that aims to explore new topics that are relevant to current events (Levac et al., 2010). The scoping review framework is effective in achieving diverse research objectives by accommodating a wide conceptual range in the discussion of various studies (Tricco et al., 2018). Following the methodological framework proposed by Arksey and O'Malley (2005) and further refined by Levac et al. (2010) the review progresses through five stages: (i) defining the research question; (ii) identifying relevant studies; (iii) selecting studies; (iv) charting the data; and (v) collating, summarizing, and reporting the results.
2.2 Search methods
A comprehensive search strategy was employed using the PubMed, Scopus, and EBSCO databases. The search terms included both Medical Subject Heading (MeSH) terms and relevant keywords. The search terms used were variations of “social support,” “online social support,” “perceived social support,” “family support,” “Tuberculosis,” “TB,” “TBC,” “medication adherence,” “medication compliance,” “drug adherence,” “drug compliance,” “adherence,” “compliance,” “lost to follow-up,” “QoL,” “HRQoL,” and “health-related QoL.” These terms were combined using Boolean operators to ensure a thorough retrieval of relevant studies. The research question guiding this search was: “What is the impact of family support on medication adherence and QoL for individuals with tuberculosis, and how does this support influence treatment outcomes?”
2.2.1 Inclusion and exclusion criteria
The study integrates the PRISMA Extension for Scoping Reviews (PRISMA-ScR) to ensure a transparent and visually represented review of various topics exploring the impact of family support on medication adherence and QoL among TB patients. Article selection was guided by specific inclusion criteria: accessibility of the full text for review, publication in English, categorization as a primary research study, and publication within the last 10 years (2012–2022). Two independent reviewers meticulously screened titles and abstracts, followed by the retrieval and evaluation of full-text articles based on predefined eligibility criteria. Discrepancies between reviewers were resolved through discussion, and a third reviewer was consulted if necessary, ensuring rigorous adherence to the PCC (Population, Concept, and Context) framework.
PCC framework
Population (P): Adult patients aged 18 years or older, diagnosed with TB and currently undergoing treatment, form the study population. Demographic details, including age range, gender distribution, and diverse TB conditions (e.g., newly diagnosed TB, Multidrug-resistant TB (MDR-TB), provide a comprehensive overview.
Concept (C): Studies exploring the relationship between family support and medication adherence, as well as QoL for TB patients, constitute the core concept. Family support, encompassing emotional and practical assistance, medication supervision, and promotion of healthy habits, significantly enhances patients' confidence, motivation, and overall treatment outcomes.
Context (C): The studies were conducted in various healthcare settings, including hospitals and community clinics. The sociocultural context, particularly in countries like Indonesia and China, underscores the crucial role of family dynamics in TB patient care. Moreover, the discussion on the impact of family support on TB patients' QoL extends to the broader context of global TB prevalence, offering insights into potential implications for public health policies and interventions.
2.2.2 Data extraction
The data extraction process involved a meticulous manual review of articles, organized using a structured table to catalog key information systematically. Each study was comprehensively analyzed before inclusion in the table. The tabular format included essential elements such as authors, year of publication, country of study, study design, population, sample characteristics, age range, gender distribution, questionnaires utilized, and key findings (Table 1). Authors provided concise summaries of study contents, ensuring clarity and consistency.
| Author, published year | JBI critical appraisal tool | Study design |
|---|---|---|
| Chen et al. (2020) | (6/8) 75% | Cross-sectional |
| Rachmawati et al. (2021) | (7/8) 87.5% | Cross-sectional |
| Sofiana et al. (2022) | (6/8) 75% | Cross-sectional |
| Tornu and Quarcoopome (2022) | (6/8) 75% | Cross-sectional |
| Zarova et al. (2018) | (6/8) 75% | Cross-sectional |
| Qiu et al. (2018) | (7/8) 87.5% | Cross-sectional |
| Chen et al. (20212021) | (6/8) 75% | Cross-sectional |
| Widani & Sianturi, 2020 | (7/9) 77.7% | Quasi-experimental |
| Yadav et al. (2021) | (6/8) 75% | Cross-sectional |
| Chen et al. (2016) | (6/8) 75% | Cross-sectional |
| Colson et al. (2013) | (9/13) 76.15% | RCT |
| Li et al. (2018) | (9/13) 76.15% | RCT |
| Lestari et al. (2018) | (6/8) 75% | Cross-sectional |
- Abbreviations: JBI, Joanna Briggs Institute; RCT, randomized controlled trial.
To ensure accuracy, two independent reviewers performed the data extraction. Any discrepancies were resolved through discussion or consultation with a third reviewer if necessary. The extracted data was then synthesized into a detailed narrative, exploring the impact of family support on medication adherence, QoL for TB patients, and overall treatment outcomes. This narrative aimed to highlight significant trends, insights, and implications derived from the included studies, providing a comprehensive understanding of the role of family support in TB patient care.
2.2.3 Quality appraisal
To assess the quality of the included studies, we employed the critical appraisal approach developed by the Joanna Briggs Institute (JBI) (Joanna Briggs Institute, 2017). Modifications were made to align the JBI criteria with the Cochrane Risk of Bias (RoB) and Risk of Bias in Nonrandomized Studies of Interventions standards. Each criterion was rated as “Yes,” “No,” “Unclear,” or “Not Applicable.” For each criterion marked “Yes,” a score of ‘1’ was assigned, while “No” or “Unclear” received a score of ‘0.’ Scores for each criterion were tallied to calculate the cumulative score for each study.
The JBI Critical Appraisal tools have undergone rigorous scrutiny and approval by the JBI Scientific Committee through an extensive peer-review process. Articles were deemed high quality if they achieved a score exceeding 75%, based on the criteria and topic relevance (Joanna Briggs Institute, 2017; Yosep et al., 2022). The two independent reviewers assessed the articles separately, ensuring an objective evaluation process. Any discrepancies between their scores were thoroughly discussed and resolved in collaboration with a third reviewer to reach a consensus. This method ensured that all articles meeting the predetermined inclusion criteria were included in the final selection. Therefore, the reliability and validity of the selected studies were ensured, minimizing the RoB and enhancing the overall credibility of the research findings.
2.2.4 Data analysis
Following the literature search and selection process, all included articles underwent a thorough examination and analysis by the entire author team. This process began with a detailed review of each study to extract and summarize essential insights and findings related to the impact of family support on patient medication adherence, QoL, and overall treatment outcomes.
The authors then engaged in an in-depth discussion to synthesize the extracted data. Key themes and patterns were identified, and a concise summary for each article was crafted to capture critical insights. To enhance clarity and facilitate synthesis, interventions identified from the literature were carefully grouped based on their commonalities. This process resulted in the creation of distinct categories of similar interventions.
Each category was subsequently explained and detailed, providing a comprehensive understanding of the various interventions and their effects. This categorization aimed to highlight significant trends and common strategies, contributing to a holistic view of how family support influences TB treatment adherence and patient QoL. Furthermore, to ensure rigor and consistency, all steps of the analysis were independently verified by multiple authors. Discrepancies were resolved through discussion, and consensus was achieved to ensure the reliability of the findings. This systematic approach to data analysis ensured that the review was thorough, transparent, and adherent to high standards of scientific rigor.
3 RESULTS
The comprehensive search yielded a total of 3855 articles. After identifying and removing 25 duplicates, the selection process is outlined in the review flowchart (Figure 1). Of the initial articles, 30.56% (n = 1178) were sourced from Scopus, 0.70% (n = 21) from EBSCO, and the majority, 68.74% (n = 2650), were retrieved from PubMed. The initial screening, conducted collaboratively by two researchers (A.Z. and F.W.), resulted in the exclusion of 99.3% of the articles (n = 3805) based on title and abstract.
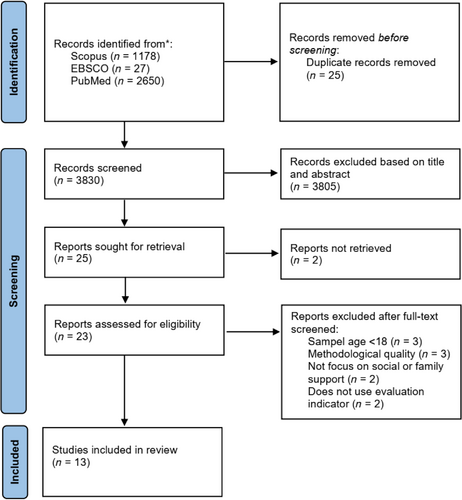
The remaining 50 articles were subjected to full-text review based on predefined selection criteria. Of these, 27 articles were excluded for the following reasons: three due to unavailability of the full text, three based on sample age, three due to methodological quality (involving review and report papers), two not focused on social or family support, and two lacking proper questionnaires or evaluation methods. This meticulous exclusion process resulted in 23 records undergoing further in-depth analysis and synthesis. Ultimately, 13 studies met the stringent inclusion criteria and were included in this scoping review. The quality of the included studies was appraised using the JBI critical appraisal tool, with articles scoring above 75% in terms of criteria and relevance to the topic (Table 1).
The final set of 13 articles specifically focused on family interventions aimed at improving medication adherence and enhancing the QoL for individuals with TB. The importance of family support within these interventions is underscored by the insights gleaned from our thorough analysis of these 13 articles.
3.1 Study characteristics
The included studies encompassed a range of designs, including randomized controlled trials (RCTs) (n = 2), cross-sectional studies (n = 10), and quasi-experimental designs (n = 1). The geographic scope of the included studies spanned multiple countries, with a focus on China (n = 5), Indonesia (n = 4), the USA (n = 1), Nepal (n = 1), Zimbabwe (n = 1), and Ghana (n = 1). Detailed characteristics of the literature are presented in Table 2.
| Author | Location | Design | Population | Age | Gender (%) | Sample |
|---|---|---|---|---|---|---|
| Chen et al., 2020 | China | Cross-sectional | Newly diagnosis TB | 26.6 | M: 298 (62) F: 183 (38) |
481 |
| Rachmawati et al., 2021 | Indonesia | Cross-sectional | TBC | 27.4 | M: 42 (57.5) F: 31 (42.5) |
73 |
| Sofiana et al., 2022 | Indonesia | Cross-sectional | TBC | 18–45(9.4%) >45 (9.6%) |
M: 26 (50) F: 26 (50) |
52 |
| Tornu & Quarcoopome, 2022 | Ghana | Cross-sectional | Suffering TB | ≥15 | M: 150 (60) F: 100 (40) |
250 |
| Zarova et al., 2018 | Zimbabwe | Cross-sectional | Suffering TB | 40.1 (12.5) | M: 176 (53) F: 156 (47) |
332 |
| Qiu et al., 2018 | China | Cross-sectional | Suffering TB | 47.72 (17.06) | M: 905 (67.44) F: 437 (32.56) |
1342 |
| Chen et al., 2021 | China | Cross-sectional | TB-laten, MDR, newly diagnostic, etc | Years 107 (22.62%) 31–44 years 82 (17.34%) ≥45 years 284 (60.04%) |
M: 327 (69.13) F: 146 (30.87) |
473 |
| Widani & Sianturi, 2020 | Indonesia | Quasi-experimental | Suffering TB | 25–49 years 60 (59.4) 50–70 years 41 (40.6) |
M: 64 (63.4) F: 37 (36.6) |
101 |
| Yadav et al., 2021 | Nepal | Cross-sectional | Suffering TB | ≥15 years | M: 117 (65) F: 63 (35) |
180 |
| Chen et al., 2016 | China | Cross-sectional | MDR-TB | ≤19 years 8 (3.77) 20–39 years 66 (31.13%) 40–59 years 93 (43.87%) ≥60 years 45 (21.23%) |
M: 148 (69.81) F: 64 (30.19) |
212 |
| Colson et al., 2013 | USA | RCT | LTBI | <40 years 134 (53.6%) >40 years 118 (46.4%) |
M: 176 (69.85) F: 76 (30.15) |
252 |
| Li et al., 2018 | China | RCT | Newly diagnosed TB | 71, 77 (5.49) | M: 109 (59.56) F: 74 (40.44) |
183 |
| Lestari et al., 2018 | Indonesia | Cross-sectional | Suffering TB | 17–25 years 17 (34%) 26–35 years 12 (24%) 36–45 year 3 (6%) 46–55 years 5 (10%) 46–65 years 13 (26%) |
M: 25 (50) F: 25 (50) |
50 |
3.2 Outcomes
The analysis of the included studies reveals that family and social support significantly improve medication adherence among TB patients. Table 3 illustrates that patients receiving robust family support demonstrate higher adherence rates (p < .05) (Chen et al., 2020; Qiu et al., 2018; Sofiana et al., 2022). Furthermore, several studies highlight the enhancement of the QoL for TB patients with strong family and social support networks (Chen et al., 2016; Lestari et al., 2020; Rachmawati et al., 2021; Sofiana et al., 2022; Yadav et al., 2021; Zarova et al., 2018). This support not only aids in the management of the disease but also contributes to the overall well-being and psychological health of the patients (Chen et al., 2021). Importantly, the studies show a positive correlation between medication adherence and QoL. Higher adherence levels are associated with significantly better QoL outcomes, indicating that adherence to treatment regimens directly influences the patients' overall health and satisfaction (Widani & Sianturi, 2020; Sofiana et al., 2022). These findings underscore the critical role of family and social support in both adherence and QoL for TB patients, emphasizing the need for integrated care approaches that involve the patient's social environment.
| Author | Measurement | Instruments | Findings |
|---|---|---|---|
| Chen et al., 2020 | Medication adherence, family support, social support, and national policy support | Social Support Rating Scale (SSRS) | The findings revealed that the mean adherence rate was 6.53 ± 1.85. Among the participants, 45.7% demonstrated good adherence to their medication regimen. |
| Rachmawati et al., 2021 | QoL and Subjective Well Being (SWB) of pulmonary TB patients and the affecting factors | Satisfaction with Life Scale (SWLS), Scale of Positive and Negative Experience (SPANE) | The study found that patient characteristics positively and significantly impact the QoL. The QoL was influenced by patient characteristics, family support, and functional fitness with path coefficients of 0.183, 0.158, and 0.243, respectively |
| Sofiana et al., 2022 | QoL, knowledge, self-efficacy, family support, and medication adherence | Self-made questionnaire that has been tested for validity and reliability | Higher obedience levels were associated with a significantly better QoL (RP = 8.333, 95% CI: 1.604–43.288). Among respondents with good family support, 43.8% (14 individuals) had a good QoL. |
| Tornu & Quarcoopome, 2022 | QoL | QoL Brief Version (WHOQOL-BREF) | A statistically significant positive correlation was found between respondents' Physical QoL and their Psychological QoL (r = .80, p < .001), Social Relationship QoL (r = .68, p < .001), and Environmental QoL (r = .43, p < .001). Additionally, receiving support from friends was positively correlated with Physical QoL (r = .18, p = .005). |
| Zarova et al., 2018 | QoL | Multidimensional Scale of Perceived Social Support (MSPSS) and the EQ-5D | Patients reported receiving the least amount of social support from friends (mean 2.8, SD 1.2) and the highest amount from family (mean 3.7, SD 1.0). The mean score for HRQoL measured by EQ-5D-VAS was 51 (SD 18.1). Patients who received adequate social support had higher HRQoL (r = .33, p < .001). |
| Qiu et al., 2018 | Medical Adherence and QOL | The questionnaire consisted of six sections: Demographic Characteristics, Family Function, Doctor-patient Communication, Knowledge about TB, TB-Related Stigma, Depressive Symptoms | There was a positive correlation between QoL and Medical Adherence (r = .31, p < .01). TB-related stigma had a negative indirect effect on medication adherence (standardized indirect effect = −0.16, 95% bias-corrected CI [−0.19, −0.13], p < .01). |
| Chen et al., 2021 | QOL Social support |
Oslo 3-item social support scale 9-item stigma questionnaire Kessler Psychological Distress Scale (K-10) 6-item QoL scale (QOL-6) |
Social support showed a positive correlation with QoL (r = .579, p < .01). The total effect of social support on QoL was 0.524 (95% CI: 0.435, 0.635), with a direct effect of 0.463 (95% CI: 0.386, 0.562), accounting for 88.36% of the total effect. |
| Widani & Sianturi, 2020 | Support and Obedience | Self-made questionnaire that has been tested for validity and reliability | There was a significant association between supervisors' support and patients' obedience to TB medication (p = .04, p < .05). |
| Yadav et al., 2021 | QOL Adherence | WHOQOL-BREF Morisky medication adherence scale (MMAS-8) | The overall QoL ranged from 10.75 to 89.25, with a mean ± SD of 55.96 ± 14.65. Among the patients, 114 (79.7%) adhered to treatment, with a confidence interval of 20.310 (7.742–53.285) and a p-value of less than 0.001. |
| Chen et al., 2016 | Social support | Attitudes toward MDR-TB disease, attitudes toward the disease, help from the health service, and the social support rating scale (SSRS) | MDR-TB participants with four or more family members had higher social support scores (p = .000). Participants with higher annual family income (≥50,001) had higher SSRS scores (p = .014). Participants who disclosed their MDR-TB status received more social support (p = .010). |
| Colson et al., 2013 | Social Support Adherence | 12 true-false questions regarding transmission, diagnosis, and treatment. Attitudinal items were based on the Health Belief Model, Social Learning Theory, Theory of Reasoned Action, and Social Action Theory | Overall, 60.9% of patients who received peer support completed the treatment. A substantial difference in adherence rates was observed between study groups (9.7%, p = .043). |
| Li et al., 2018 | Social Support | Social Support Rating Scale (SSRS) | The intervention group showed a significant increase in social support over time compared to the control group, evident in the dimensions of objective support (βgroup time = 0.15, p < .05), emotional support (βgroup time = 0.32, p < .05), and support utilization (βgroup × time = 0.16, p < .05). |
| Lestari et al., 2020 | Medication Adherence Family support | Family Support Questionnaire, Medication Adherence Questionnaire | The results showed a strong relationship between family support and medication adherence (r = .468, p < .001). |
4 DISCUSSION
4.1 Family support in improving medication adherence
Improving medication adherence in TB patients is crucial for effectively preventing and controlling the disease. Nonadherence can result in treatment failure, relapse, the emergence of drug-resistant TB strains, prolonging the infectious period, and contributing to the overall burden of drug resistance (Fang et al., 2019). Adherence to TB treatment is paramount for achieving desired treatment outcomes and preventing the spread of the disease within communities (Chen et al., 2021; Gashu et al., 2020; Tola et al., 2017).
Research conducted in Indonesia involving 52 family members of TB patients demonstrated that 49 TB patients who received support from their families had good medication adherence (Zamaa et al., 2023). Family members play a vital role in supporting and supervising the medication of TB patients (Lestari et al., 2020). Chen et al. (2020) found that patients who received frequent medication supervision and encouragement from their family members were more likely to exhibit higher adherence levels. This is particularly important as TB patients often face psychological burdens such as fear of treatment failure and a lack of confidence in their ability to recover. Family support can boost patients' confidence, positively influencing their treatment adherence (Chen et al., 2020; Widani & Sianturi, 2020).
Li et al. (2018) also found that patients with adequate family support felt more confident in adhering to their medication regimens. Studies have shown that directly observed therapy is commonly provided by family members, and well-trained family members offer better support than healthcare personnel (Yin et al., 2018). Therefore, training family members to provide comprehensive therapeutic and psychological interventions can enhance patient adherence (Chen et al., 2020).
Li et al. (2018) implemented a family-based intervention for TB patients over 6 months with a frequency of once every 2 weeks. The intervention included home visits, psycho-educational workshops, and health education focused on TB, encouraging patients to express their emotional distress. During these sessions, families shared personal experiences and provided valuable insights on problem-solving strategies and self-care practices. Close family relationships contribute to patients' life satisfaction, alleviate their concerns, and bolster their resilience in fighting the disease. Conversely, family dysfunction can lead to alienation and hinder positive treatment outcomes (Qiu et al., 2018).
4.2 Family support in improving QoL
Family and social support play a significant role in improving the QoL for TB patients. Family support, including stress reduction and the implementation of healthcare functions, has a dominant influence on patients' QoL with pulmonary TB (Rachmawati et al., 2021). The family's role in providing psychological well-being, reducing stress, and increasing family resilience contributes to patients' adherence to TB treatment (Rachmawati et al., 2021; Zarova et al., 2018).
Being the closest to the affected individual, family members offer invaluable support and empathy. Their high level of empathy motivates them to provide comprehensive care to family members suffering from TB, such as supervising medication intake and providing nutritious food. Moreover, families play a crucial role in providing motivation, promoting personal hygiene, and ensuring a clean environment for the patient (Devlin et al., 2022; Li et al., 2018; Samal, 2017; Samal & Dehury, 2016). Colson et al. (2013) also examined peer interventions where individuals were assigned to meet one-on-one with patients and their families on a weekly basis, showing that respondents experienced greater adherence.
QoL in TB patients improves with the implementation of family knowledge through the support provided to patients (Salehitali et al., 2019; Tornu & Quarcoopome, 2022). Family support includes informational, appraisal, instrumental, and emotional support. Rachmawati et al. (2021) reported that 68.5% of respondents had a good QoL, with family being the dominant factor affecting their QoL. Patients who experienced substantial social support and strong family support demonstrated more effective therapy compared to those with insufficient family support, as the latter group showed an increase in self-efficacy (Chen et al., 2016; Chen et al., 2020). Self-efficacy also has a positive influence on medication adherence, which is often bolstered by family motivation. The motivation provided by the family to patients with pulmonary TB is pivotal in improving patient recovery and increasing the motivation to recover (Young et al., 2020).
Previous studies have shown a link between medication adherence and overall QoL, with higher adherence associated with more effective therapy (Lestari et al., 2020; Yadav et al., 2021). Adherence and QoL have a reciprocal relationship, and findings indicate a strong association between medication adherence and QoL in TB patients (Salehitali et al., 2019; Sofiana et al., 2022; Yadav et al., 2021).
4.3 Limitations
While this scoping review provides valuable insights, several limitations should be considered. First, the existing literature on the structure and framework of family support for TB patients requires further exploration and clarification. Additional research is needed to develop and evaluate effective models of family support specifically tailored to the unique needs of TB patients. Moreover, it is essential to acknowledge that the majority of our study sample originated from Indonesia and China, potentially limiting the generalizability of our findings to individuals from regions with different social and cultural backgrounds. Although the inclusion of studies from Indonesia and China was extensive, these countries have larger populations compared to others, which may influence the representation of our sample. Additionally, our review focused exclusively on quantitative research studies, predominantly relying on self-reported data from patients, with limited inclusion of family involvement in data collection. This reliance on self-reported data may introduce bias and affect the accuracy of the findings. To attain a more comprehensive understanding of the family's experiences in supporting TB patients, future investigations should consider incorporating in-depth interviews and qualitative analyses. This approach would provide richer insights into the nuanced dynamics of family support, complementing the quantitative data presented in our review. Furthermore, the review did not consider the potential impact of socioeconomic factors, healthcare infrastructure, and policy differences across countries, which could influence the effectiveness of family support interventions. Addressing these factors in future research would help to contextualize the findings and enhance the applicability of family support models in diverse settings.
5 CONCLUSIONS
Family support positively impacts the QoL of TB patients, fostering greater adherence to medication regimens. The family unit plays several crucial roles in supporting the affected member, including enhancing psychological well-being, motivating medication compliance, providing dietary assistance, promoting personal hygiene, maintaining a clean environment, reducing stress, and reinforcing family resilience. Recognizing the significance of family involvement, health interventions should prioritize strategies that empower and educate families to provide effective support throughout the course of TB treatment. This holistic approach not only addresses challenges related to medication adherence but also contributes to the overall well-being and resilience of TB patients.
The recommendations in this study highlight the need for further research to explore and develop effective models and family support schemes that enhance patient QoL and promote medication adherence. Ultimately, realizing the full potential of family-centered care requires health systems to incorporate reliable measures that recognize and support the critical role of families in the care of TB patients. By doing so, treatment outcomes and the overall health and resilience of individuals affected by TB can be improved.
AUTHOR CONTRIBUTIONS
Lutfian Lutfian was responsible for conceptualization, methodology, formal analysis, original draft writing, supervision, and project administration. Aufa Azizah contributed to data curation, article screening, data extraction, manuscript review and editing, and visualization. Izdihar Javier Wardika also worked on data curation, article screening, data extraction, manuscript review and editing, and visualization. Fahmi Wildana contributed to data curation, article screening, manuscript review and editing, and visualization. Sidik Maulana was involved in methodology, formal analysis, manuscript review and editing, and validation. Riki Wartakusumah provided supervision, project administration, and contributed to manuscript review and editing.
ACKNOWLEDGMENTS
The authors would like to express their deepest gratitude to the Lembaga Pengelola Dana Pendidikan (LPDP)/Indonesia Endowment Fund for Education under the Ministry of Finance of the Republic of Indonesia for sponsoring my master's studies and the support for this paper and publication. The authors also extend their deepest gratitude to the Monash University Library for their support and facilitation in the publication of this paper.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.