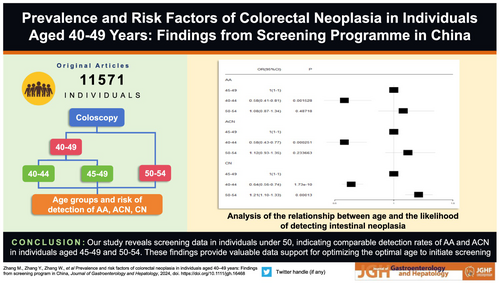
Prevalence and risk factors of colorectal neoplasia in individuals aged 40–49 years: Findings from screening program in China
Mingqing Zhang
Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin, China
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China
Search for more papers by this authorYongdan Zhang
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
Search for more papers by this authorWen Zhang
Center for Applied Mathematics, Tianjin University, Tianjin, China
Search for more papers by this authorYong Zhang
Center for Applied Mathematics, Tianjin University, Tianjin, China
Search for more papers by this authorLizhong Zhao
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
Search for more papers by this authorHaoren Jing
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
Search for more papers by this authorXinyu Gao
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
Search for more papers by this authorZhenguo Nie
Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin, China
School of Medicine, Nankai University, Tianjin, China
Search for more papers by this authorCorresponding Author
Siwei Zhu
Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin, China
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China
Correspondence
Siwei Zhu, The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China. Email: [email protected]; Shiwu Zhang, Department of Pathology, Tianjin Union Medical Center, Tianjin 2755-7131, China. Email: [email protected]; Xipeng Zhang, Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin 2755-7131, China.
Email: [email protected]
Search for more papers by this authorCorresponding Author
Shiwu Zhang
The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China
Department of Pathology, Tianjin Union Medical Center, Tianjin, China
Correspondence
Siwei Zhu, The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China. Email: [email protected]; Shiwu Zhang, Department of Pathology, Tianjin Union Medical Center, Tianjin 2755-7131, China. Email: [email protected]; Xipeng Zhang, Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin 2755-7131, China.
Email: [email protected]
Search for more papers by this authorCorresponding Author
Xipeng Zhang
Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin, China
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China
Correspondence
Siwei Zhu, The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China. Email: [email protected]; Shiwu Zhang, Department of Pathology, Tianjin Union Medical Center, Tianjin 2755-7131, China. Email: [email protected]; Xipeng Zhang, Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin 2755-7131, China.
Email: [email protected]
Search for more papers by this authorMingqing Zhang
Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin, China
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China
Search for more papers by this authorYongdan Zhang
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
Search for more papers by this authorWen Zhang
Center for Applied Mathematics, Tianjin University, Tianjin, China
Search for more papers by this authorYong Zhang
Center for Applied Mathematics, Tianjin University, Tianjin, China
Search for more papers by this authorLizhong Zhao
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
Search for more papers by this authorHaoren Jing
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
Search for more papers by this authorXinyu Gao
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
Search for more papers by this authorZhenguo Nie
Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin, China
School of Medicine, Nankai University, Tianjin, China
Search for more papers by this authorCorresponding Author
Siwei Zhu
Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin, China
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China
Correspondence
Siwei Zhu, The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China. Email: [email protected]; Shiwu Zhang, Department of Pathology, Tianjin Union Medical Center, Tianjin 2755-7131, China. Email: [email protected]; Xipeng Zhang, Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin 2755-7131, China.
Email: [email protected]
Search for more papers by this authorCorresponding Author
Shiwu Zhang
The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China
Department of Pathology, Tianjin Union Medical Center, Tianjin, China
Correspondence
Siwei Zhu, The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China. Email: [email protected]; Shiwu Zhang, Department of Pathology, Tianjin Union Medical Center, Tianjin 2755-7131, China. Email: [email protected]; Xipeng Zhang, Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin 2755-7131, China.
Email: [email protected]
Search for more papers by this authorCorresponding Author
Xipeng Zhang
Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin, China
School of Medicine, Nankai University, Tianjin, China
Tianjin Institute of Coloproctology, Tianjin, China
The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China
Correspondence
Siwei Zhu, The Institute of Translational Medicine, Tianjin Union Medical Center of Nankai University, Tianjin, China. Email: [email protected]; Shiwu Zhang, Department of Pathology, Tianjin Union Medical Center, Tianjin 2755-7131, China. Email: [email protected]; Xipeng Zhang, Department of Colorectal Surgery, Tianjin Union Medical Center, Tianjin 2755-7131, China.
Email: [email protected]
Search for more papers by this authorDeclaration of conflict of interest: The authors disclose no conflicts. The funding source had no role in study design, data collection, analysis, or interpretation, report writing, or the decision to submit this paper for publication.
Ethics approval: Given that our study involved only a descriptive analysis of individual data without direct or indirect patient intervention, we did not require approval from a research ethics committee. Additionally, we ensured that all investigations and methods employed in the study adhered to the principles outlined in the Declaration of Helsinki.
Informed consent: Obtaining informed consent from individuals when participating in screening program.
Abstract
Background and Aim
The incidence of colorectal cancer (CRC) in individuals under 50 is increasing worldwide. We conducted an analysis of colonoscopy findings in high-risk individuals under 50 in the CRC screening program in Tianjin, China, to determine the detection rate and risk factors of advanced adenomas (AA), advanced colorectal neoplasia (ACN), colorectal neoplasia (CN).
Methods
Our study investigated individuals aged 40–49 who underwent CRC screening and completed colonoscopy, 2012–2020, while the 50–54 age group served as a control. We compared the detection rates of AA, ACN, and CN among three age groups using univariate and multivariable logistic regression analyses, and investigated the risk factors associated with AA, ACN, and CN among individuals aged 40–49.
Results
We found a gradual increase in the detection rate of AA, ACN, and CN among individuals aged 40–54. The detection rates for AA (OR 0.58; 95% CI 0.41–0.81), ACN (OR 0.58; 95% CI 0.43–0.77), and CN (OR 0.64; 95% CI 0.56–0.74) were lower in individuals aged 40–44 compared to 45–49. The detection rates of AA (OR 1.08; 95% CI 0.87–1.34) and ACN (OR 1.12; 95% CI 0.93–1.35) in individuals aged 45–49 were comparable with 50–54. Besides, lifestyle factors, BMI, and FIT are not associated with the detection rates of AA, ACN, and CN among individuals aged 40–49.
Conclusions
Our study reveals screening data in individuals under 50, indicating comparable detection rates of AA and ACN in individuals aged 45–49 and 50–54. These findings provide valuable data support for optimizing the optimal age to initiate screening.
Graphical Abstract
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Supporting Information
| Filename | Description |
|---|---|
| JGH16468-sup-0001-manuscript-S.docxWord 2007 document , 347.7 KB |
Table S1. Distribution of colonoscopy-detected diseases in the 40–54 age group, n(%). Table S2. Distribution of colonoscopy-detected diseases by age group, n(%). Table S3–1. Characteristics of the age groups Before and After Propensity Score Matching, n(%). Table S3–2. Age-specific risk of AA detection, n(%). Table S3–3. Age-specific risk of ACN detection, n(%). Table S3–4. Age-specific risk of CN detection, n(%). Table S3–5. Age-specific risk of CN detection within Propensity Score Analyses, n(%). Table S4–1. Risk factors associated with the detection of AA in individuals aged 50–54 years, n(%). Table S4–2. Risk factors associated with the detection of ACN in individuals aged 50–54 years, n(%). Table S4–3. Risk factors associated with the detection of CN in individuals aged 50–54 years, n(%). Table S5–1. Risk factors associated with the detection of AA in individuals aged 40–49 years, n(%). Table S5–2. Risk factors associated with the detection of ACN in individuals aged 40–49 years, n(%). Table S5–3. Risk factors associated with the detection of CN in individuals aged 40–49 years, n(%). Table S6–1. Risk of AA detection in 40–49 age group with lifestyle and other factors included, n(%). Table S6–2. Risk of ACN detection in 40–49 age group with lifestyle and other factors included, n(%). Table S6–3. Risk of CN detection in 40–49 age group with lifestyle and other factors included, n(%). Table S6–4. Characteristics of individuals with BMI ≥ 25 or BMI<25 Before and After Propensity Score Matching, n(%). Table S6–5. Risk of AA detection in the 40–49 age group, including lifestyle and other factors through Propensity Score Analyses, n(%). Table S6–6. Risk of ACN detection in the 40–49 age group, including lifestyle and other factors through Propensity Score Analyses, n(%). Table S6–7. Risk of CN detection in the 40–49 age group, including lifestyle and other factors through Propensity Score Analyses, n(%). Table S7–1. Risk of AA detection in 50–54 age group with lifestyle and other factors included, n(%). Table S7–2. Risk of ACN detection in 50–54 age group with lifestyle and other factors included, n(%). Table S7–3. Risk of CN detection in 50–54 age group with lifestyle and other factors included, n(%). |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
References
- 1Parekh A, Hochheimer CJ, Espinoza JM et al. Primary care provider knowledge and practice in risk assessment for early age onset colorectal cancer: opportunities for improvement. J Cancer Prev. 2021; 26: 298–303.
- 2Araghi M, Soerjomataram I, Bardot A et al. Changes in colorectal cancer incidence in seven high-income countries: a population-based study. Lancet Gastroenterol. Hepatol. 2019; 4: 511–518.
- 3Sung JJY, Chiu H-M, Jung K-W et al. Increasing trend in young-onset colorectal cancer in asia: more cancers in men and more rectal cancers. Am. J. Gastroenterol. 2019; 114: 322–329.
- 4Zhang L, Cao F, Zhang G et al. Trends in and predictions of colorectal cancer incidence and mortality in china from 1990 to 2025. Front. Oncol. 2019; 9: 98.
- 5Bhandari A, Woodhouse M, Gupta S. Colorectal cancer is a leading cause of cancer incidence and mortality among adults younger than 50 years in the USA: a SEER-based analysis with comparison to other young-onset cancers. J. Invest. Med. 2017; 65: 311–315.
- 6Pearlman R, Frankel WL, Swanson B et al. Prevalence and spectrum of germline cancer susceptibility gene mutations among patients with early-onset colorectal cancer. JAMA Oncol. 2017; 3: 464–471.
- 7Lortet-Tieulent J, Soerjomataram I, Lin CC, Coebergh JWW, Jemal A. U.S. Burden of cancer by race and ethnicity according to disability-adjusted life years. Am. J. Prev. Med. 2016; 51: 673–681.
- 8Reif de Paula T, Haas EM, Keller DS. Colorectal cancer in the 45-to-50 age group in the United States: a National Cancer Database (NCDB) analysis. Surg. Endosc. 2021.
- 9Brenner DR, Ruan Y, Shaw E, De P, Heitman SJ, Hilsden RJ. Increasing colorectal cancer incidence trends among younger adults in Canada. Prev. Med. 2017; 105: 345–349.
- 10Brenner DR, Heer E, Sutherland RL et al. National trends in colorectal cancer incidence among older and younger adults in Canada. JAMA Netw. Open 2019; 2: e198090.
- 11You YN, Xing Y, Feig BW, Chang GJ, Cormier JN. Young-onset colorectal cancer: is it time to pay attention? Arch. Intern. Med. 2012; 172: 287–289.
- 12Murphy CC, Lund JL, Sandler RS. Young-onset colorectal cancer: earlier diagnoses or increasing disease burden? Gastroenterology 2017; 152.
- 13Abualkhair WH, Zhou M, Ahnen D, Yu Q, Wu X-C, Karlitz JJ. Trends in incidence of early-onset colorectal cancer in the United States among those approaching screening age. JAMA Netw. Open 2020; 3: e1920407.
- 14Cho MY, Siegel DA, Demb J, Richardson LC, Gupta S. Increasing colorectal cancer incidence before and after age 50: implications for screening initiation and promotion of “on-time” screening. Dig. Dis. Sci. 2021.
- 15Siegel RL, Fedewa SA, Anderson WF et al. Colorectal cancer incidence patterns in the United States, 1974–2013. JNCI: J. Nat. Cancer Inst. 2017; 109.
10.1093/jnci/djw322 Google Scholar
- 16Shaukat A, Kahi CJ, Burke CA, Rabeneck L, Sauer BG, Rex DK. ACG clinical guidelines: colorectal cancer screening 2021. Am. J. Gastroenterol. 2021; 116: 458–479.
- 17Wolf AMD, Fontham ETH, Church TR et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J. Clin. 2018; 68: 250–281.
- 18Patel SG, May FP, Anderson JC et al. Updates on age to start and stop colorectal cancer screening: recommendations from the U.S. multi-society task force on Colorectal Cancer. Gastroenterology 2022; 162: 285–299.
- 19Peterse EFP, Meester RGS, Siegel RL et al. The impact of the rising colorectal cancer incidence in young adults on the optimal age to start screening: microsimulation analysis I to inform the American Cancer Society colorectal cancer screening guideline. Cancer 2018; 124: 2964–2973.
- 20Knudsen AB, Zauber AG, Rutter CM et al. Estimation of benefits, burden, and harms of colorectal cancer screening strategies: modeling study for the US Preventive Services Task Force. JAMA 2016; 315: 2595–2609.
- 21Screening for colorectal cancer: recommendation and rationale. Ann. Intern. Med. 2002; 137: 129–131.
- 22Siegel RL, Torre LA, Soerjomataram I et al. Global patterns and trends in colorectal cancer incidence in young adults. Gut 2019; 68: 2179–2185.
- 23Zhao L, Zhang X, Chen Y, Wang Y, Zhang W, Lu W. Does self-reported symptom questionnaire play a role in nonadherence to colonoscopy for risk-increased population in the Tianjin colorectal cancer screening programme? BMC Gastroenterol. 2021; 21: 117.
- 24Yang JJ, Yu D, Shu XO et al. Reduction in total and major cause-specific mortality from tobacco smoking cessation: a pooled analysis of 16 population-based cohort studies in Asia. Int. J. Epidemiol. 2022; 50: 2070–2081.
- 25Siegel RL, Miller KD, Jemal A. Colorectal cancer mortality rates in adults aged 20 to 54 years in the United States, 1970-2014. JAMA 2017; 318: 572–574.
- 26Butterly LF, Siegel RL, Fedewa S, Robinson CM, Jemal A, Anderson JC. Colonoscopy outcomes in average-risk screening equivalent young adults: data from the New Hampshire colonoscopy registry. Off J Am Coll. Gastroenterol. ACG. 2021; 116: 171–179.
- 27Zhang M, Zhao L, Zhang Y et al. Colorectal cancer screening with high risk-factor questionnaire and fecal immunochemical tests among 5, 947, 986 asymptomatic population: a population-based study. Front. Oncol. 2022; 12: 893183.
- 28Rundle AG, Lebwohl B, Vogel R, Levine S, Neugut AI. Colonoscopic screening in average-risk individuals ages 40 to 49 vs 50 to 59 years. Gastroenterology 2008; 134: 1311–1315.
- 29Knudsen AB, Rutter CM, Peterse EFP et al. Colorectal cancer screening: an updated modeling study for the US Preventive Services Task Force. JAMA 2021; 325: 1998–2011.
- 30Basu P, Ponti A, Anttila A et al. Status of implementation and organization of cancer screening in The European Union Member States-Summary results from the second European screening report. Int. J. Cancer 2018; 142: 44–56.
- 31Elangovan A, Skeans J, Landsman M et al. Colorectal cancer, age, and obesity-related comorbidities: a large database study. Dig. Dis. Sci. 2021; 66: 3156–3163.
- 32Liu P-H, Wu K, Ng K et al. Association of obesity with risk of early-onset colorectal cancer among women. JAMA Oncol. 2019; 5: 37–44.
- 33Abdelnaby HB, Abuhussein AA, Fouad AM et al. Histopathological and epidemiological findings of colonoscopy screening in a population with an average risk of colorectal cancer in Kuwait. Saudi J. Gastroenterol. 2021; 27: 158–165.
- 34Bilal M, Singh S, Le TT, Al-Saadi Y, Guturu P. Select group of patients might benefit from early colonoscopic screening for colorectal cancer. Surg. Endosc. 2020; 34: 4463–4471.
- 35Jung YS, Yun KE, Chang Y, Ryu S, Park DI. Risk factors such as male sex, smoking, metabolic syndrome, obesity, and fatty liver do not justify screening colonoscopies before age 45. Dig. Dis. Sci. 2016; 61: 1021–1027.
- 36Wang SY, Zhang WS, Jiang CQ et al. Association of novel and conventional obesity indices with colorectal cancer risk in older Chinese: a 14-year follow-up of the Guangzhou Biobank Cohort Study. BMC Cancer 2023; 23: 286.
- 37Bai H, Xu Z, Li J et al. Independent and joint associations of general and abdominal obesity with the risk of conventional adenomas and serrated polyps: a large population-based study in East Asia. Int. J. Cancer 2023; 153: 54–63.
- 38Stoffel EM, Murphy CC. Epidemiology and mechanisms of the increasing incidence of colon and rectal cancers in young adults. Gastroenterology 2020; 158: 341–353.
- 39Zheng X, Hur J, Nguyen LH et al. Comprehensive assessment of diet quality and risk of precursors of early-onset colorectal cancer. J. Natl. Cancer Inst. 2021; 113: 543–552.
- 40Rosato V, Bosetti C, Levi F et al. Risk factors for young-onset colorectal cancer. Cancer Causes Control: CCC. 2013; 24: 335–341.
- 41Kim JY, Jung YS, Park JH et al. Different risk factors for advanced colorectal neoplasm in young adults. World J. Gastroenterol. 2016; 22: 3611–3620.
- 42Nguyen LH, Liu P-H, Zheng X et al. Sedentary behaviors, TV viewing time, and risk of young-onset colorectal cancer. JNCI Cancer. Spectrum 2018; 2: pky073.
- 43Zhang M, Zhang Y, Zhang W et al. Postponing colonoscopy for 6 months in high-risk population increases colorectal cancer detection in China. Cancer Med. 2023; 12: 11816–11827.
- 44Meng W, Cai SR, Zhou L, Dong Q, Zheng S, Zhang SZ. Performance value of high risk factors in colorectal cancer screening in China. World J. Gastroenterol. 2009; 15: 6111–6116.
- 45Murphy CC, Singal AG, Baron JA, Sandler RS. Decrease in incidence of young-onset colorectal cancer before recent increase. Gastroenterology 2018; 155: 1716–1719.
- 46Chen H, Zheng X, Zong X et al. Metabolic syndrome, metabolic comorbid conditions and risk of early-onset colorectal cancer. Gut 2021; 70: 1147–1154.