E-Poster Presentations – B3) Biliary
# P-0033
Changes in the distribution of interstitial cells of Cajal apoptosis in acute cholecystitis in guinea pigs
Zhenpeng Huang1, Hu Qiu2, Yan Yang2 and Bao-Ping Yu2
1Department of Gastroenterology, ZhuJiang Hospital of Southern Medical University, China; 2Department of Gastroenterology, Renmin Hospital of Wuhan University, China
Background: Acute cholecystitis is commonly observed in patients with gallbladder disorders. Interstitial cells of Cajal (ICCs) in the gallbladder are important for regulating gallbladder motility and have a close relationship with acute cholecystitis. Aim: The aim of this study was to explore changes in the distribution of gallbladder ICCs apoptosis in a model of acute cholecystitis. Materials and Methods: Thirty guinea pigs were randomly divided into three groups: the sham-operated group and the study groups. Animals in the study groups underwent bile duct ligation followed by laparotomy and cholecystectomy 24 or 48 h after surgery. Immunohistochemistry was performed to observe the shape, size, morphology, and numbers of gallbladder ICCs, and terminal deoxynucleotidyl transferase dUTP nick-end labeling was performed to detect apoptosis in gallbladder ICCs. Results: There were no differences in the shape, size, and morphology of the gallbladder ICCs in all groups. The numbers of gallbladder ICCs were significantly decreased, and gallbladder ICC apoptosis was significantly increased in the acute cholecystitis model at both 24 and 48 h (P < 0.05). Additionally, the densities of gallbladder ICCs were reduced, and gallbladder ICC death was increased from the neck of the gallbladder to the fundus of the gallbladder owing to apoptosis in the acute cholecystitis model (all P < 0.05). Conclusion: Acute cholecystitis reduced the density of gallbladder ICCs and increased the frequency of apoptotic gallbladder ICCs from the neck of the gallbladder to the fundus of the gallbladder; these alterations may affect gallbladder ICC function.
| Group | Part of gallbladder | ||
|---|---|---|---|
| Upper part | Middle part | Lower part | |
| Sham group* | 5.6667 ± 2.51661 | 16.3333 ± 2.08167 | 19.6667 ± 1.15470 |
| CBDL-24-h group* | 6.6667 ± 1.52753 | 20.6667 ± 3.51188 | 23.6667 ± 2.51661 |
| CBDL-48-h group* | 10.6667 ± 0.57735 | 26.3333 ± 2.08167 | 28.6667 ± 2.08167 |
- * F-values respectively were 7.000, 10.778, and 15.250; P-values were 0.027, 0.01, and 0.04, respectively.
# P-0035
Clinical significance of location of cystic duct in recurrent common bile duct stone
Jai Hoon Yoon
Department of Internal Medicine, Division of Gastroenterology and Hepatology, Gwangmyeong Sungae Hospital, Seoul, South Korea
Background: We know that there is a variation in the aspect of insertion of the cystic duct. There are many patients who suffered from recurrent cholangitis with CBD stones. We investigated the clinical significance of the location of the cystic duct in view of the recurrence of CBD stones. Method: Consecutive ERCP procedures for extractions of common bile duct stones were studied at one university hospital. We reviewed the medical charts retrospectively about the correlation between the recurrence rate of CBD stones and inserted location of the cystic duct. A total of 959 patients were included who received ERCP because of biliary problems such as cholangitis and choledocholithiasis. After the exception of cases due to malignancy and follow-up loss, we enrolled 347 patients in this study. Results: A total of 347 patients were enrolled for analysis. Among them, 108 patients (31.1%) had a cystic duct that is located in the upper one-third of CBD, 223 patients (64.3%) had cystic ducts in the middle one-third of CBD, and 16 patients (4.6%) in the lower one-third of CBD. There was an association between the location of cystic duct and recurrence rates of calculous cholangitis (12.9% in the upper one-third of CBD, 23.7% in the middle one-third of CBD, and 25.0% in the lower one-third of CBD). The recurrence rate in patients with cystic duct located in the upper one-third was lower than those in the lower two-thirds (P = 0.016). Age–sex-adjusted multivariate analysis for the recurrence of calculous cholangitis showed meaning value according to cystic duct that located upper one third (P = 0.011). Conclusions: The recurrence rate of calculous cholangitis in patients who have the cystic duct located in the lower two-thirds of CBD is significantly higher than the upper one-third. We are sure that this is one of the risk factors for estimating the recurrence rate of calculous cholangitis.
# P-0156
Combination therapy with capecitabine and cisplatin as second-line chemotherapy for advanced biliary tract cancer
Jang Han Jung1, Moon Jae Chung2, Seungmin Bang2, Seung Woo Park2, Si Young Song2 and Jeong Youp Park2
1Division of Gastroenterology, Department of Internal Medicine, Hallym University Dongtan Sacred Heart Hospital; 2Division of Gastroenterology, Yonsei Institute of Gastroenterology, Department of Internal Medicine, Yonsei University College of Medicine
Background/Aims: Palliative chemotherapy is the main treatment for advanced biliary tract cancer (BTC). However, there is a lack of established second-line chemotherapy to treat disease progression after first-line chemotherapy. We examined combination therapy with capecitabine and cisplatin for advanced BTC as a second-line regimen. Methods: We analyzed the medical records of 40 patients diagnosed with BTC who received palliative second-line chemotherapy with capecitabine and cisplatin. Results: The median overall survival from the start of second-line chemotherapy was 6.3 months. The median overall survival from diagnosis was 17.9 months. The median progression-free survival during second-line chemotherapy was 2.3 months. Nine (30%) patients experienced adverse events of grade ≥ 3. Eastern Cooperative Oncology Group (ECOG) performance score was an independent predictor of adverse events. Conclusions: Combination therapy with capecitabine and cisplatin may be an option for second-line chemotherapy in some of patients with advanced BTC.
# P-0169
EUS-guided gallbladder drainage for acute cholecystitis after placement of a metal stent for malignant biliary stricture
Fumisato Kozakai
Gastroenterology, Sendai City Medical Center, Japan
Background: It is often difficult to treat acute cholecystitis after metal stent (MS) placement for unresectable malignant biliary stricture. Although successful cases of EUS-guided gallbladder drainage (EUS-GBD) have recently been reported, its efficacy and safety have not been established. We aimed to evaluate a case series of EUS-GBD for such condition compared with percutaneous transhepatic gallbladder drainage with tube placement (PTGBD) and aspiration (PTGBA). Methods: Twenty-two patients who underwent intervention for acute cholecystitis after MS placement in the bile duct at our center from January 2011 to January 2017 were included in this study. As to EUS-GBD, PTGBD, and PTGBA, technical success, clinical success, procedure-related adverse events, and recurrence of acute cholecystitis were retrospectively analyzed. Results: In the 22 patients, 6 EUS-GBD procedures, 9 PTGBD procedures, and 13 PTGBA procedures were performed with overlap. All procedures were technically successful. The clinical success rate was 100% (6/6) in the EUS-GBD group, 89% (8/9) in the PTGBD group, and 62% (8/13) in the PTGBA group (P = 0.12). Adverse events were observed in some cases after EUS-GBD (33%, 2/6) and PTGBD (11%, 1/9), while PTGBA caused no adverse events (P = 0.10). During the mean follow-up period of 124 days, acute cholecystitis recurred in two patients of the EUS-GBD group and one patient in each of the other groups after interval periods of 22, 30, 37, and 27 days. The mean overall survival period after the procedure in the EUS-GBD, PTGBD, and PTGBA groups was 141, 101, and 114 days, respectively. Conclusions: Although EUS-GBD was found to be effective, this technique could induce adverse events. Therefore, PTGBA would be appropriate as a first step, possibly followed by EUS-GBD or PTGBD as an option for the next step.
# P-0208
“Over flow” is a new useful endoscopic finding to detect the early gastric cancers
Motohiro Sando, Toshiyuki Wakatsuki and Haruhiro Yamashita
Department of Gastroenterology and Hepatology, Okayama Medical Center, Japan
Introduction: We report a case that showed characteristic views in the contrast-enhanced transabdominal ultrasonography (CE-TU) of gallbladder metastasis from renal cell carcinoma (RCC). RCC often metastasizes to the lungs, a bone, the liver hematogenously, but the metastasis to the gallbladder is extremely rare. The present case is that of a growing gallbladder mass during postoperative chemotherapy of RCC. The characteristic views in the CE-TU enabled the successful diagnosis of the gallbladder metastasis from RCC in this case. Case description: A 65-year-old man underwent left nephrectomy for RCC 2 years ago. There was pulmonary metastasis, and he continued chemotherapy afterwards. Pulmonary metastases were stable, but the mass in the gallbladder increased in diameter from 5 to 15 mm. The contrasting computed tomography was impossible because of his chronic kidney failure. TU examination revealed an irregularly shaped, polypoid, and isoechoic mass in the gallbladder fundal. The tumor surface displayed a heterogeneous, thick, and highly echoic layer. Blood flow was detected in the base of the tumor mass by Doppler color flow mapping. CE-TU examination revealed strong homogeneous enhancement, but tumor surface was not enhanced. This imaging suggested that the lesion was not a primary gallbladder carcinoma or composed of non-neoplastic polyps.
Total laparoscopic cholecystectomy was performed because of an internal hemorrhage in the gallbladder. On histological examination, the mass was found to consist of atypical cells with small nuclei and clear cytoplasm. These findings matched those of RCC that was resected 2 years ago. The final diagnosis was gallbladder metastasis from RCC. Most of the tumor surface was covered with necrotic debris. It was considered that the necrotic debris corresponded to the highly echoic surface layer observed on the preoperative ultrasound images. A heterogeneous thick, highly echoic surface layer that is not enhanced might be useful for differentiating gallbladder metastasis from RCC from primary gallbladder carcinoma.
# P-0256
Impact of emergent ERCP and the efficacy of elective EUS in patients with acute biliary pancreatitis
Sho Hasegawa, Shinsuke Koshita, Kei Ito, Yoshihide Kanno, Takahisa Ogawa, Hiroaki Kusunose, Kaori Masu, Toshitaka Sakai, Touji Murabayashi, Fumisato Kozakai and Yutaka Noda
Department of Gastroenterology, Sendai City Medical Center, Sendai, Japan
Aims: Our aim is to clarify the efficacy of emergent ERCP and appropriate imaging studies to detect common bile duct stones (CBDS) in patients with acute-biliary pancreatitis (ABP). Methods: We included consecutive 154 patients diagnosed with ABP. We retrospectively investigated the following: (i) outcomes of emergent ERCP; (ii) the diagnostic ability of CBDS detection by CT; (iii) the diagnostic ability of CBDS detection by EUS or MRCP in subjects without CBDS depicted by CT; (iv) the rate of spontaneous passed CBDS. Seventy cases of CBDS detected by ERCP were defined as those with definitive CBDS. Results: (i) Emergent ERCP was performed in 41 patients (27%). The presence of CBDS was confirmed in 93%, and cholangitis was improved in all of those patients after ERCP. One patient (2%) developed necrotizing pancreatitis. (ii) All 50 subjects with CBDS detected by CT underwent emergent or elective ERCP. The sensitivity, specificity, and accuracy for detecting CBDS using CT were 61%, 92%, and 75%, respectively. (iii) Of the 104 patients without CBDS detected by CT, 70 underwent MRCP and/or EUS, 31 underwent diagnostic ERCP, and the remaining three underwent follow-up. The sensitivity, specificity, and accuracy for the diagnosis of CBDS were respectively 50%, 88%, and 83%, using MRCP, whereas they were respectively 86%, 96%, and 95% using EUS. (iv) Twelve patients who underwent CT followed by diagnostic ERCP and 62 patients underwent CT and EUS and/or MRCP were negative for CBDS; therefore, 74 were considered to have spontaneously passed stones. Conclusion: Emergent ERCP was effective and safe for therapy of ABP. Because almost half of patients with ABP had spontaneously passed stones, the performance of non-invasive examinations such as EUS and MRCP should be considered to avoid unnecessary ERCP after improvement of pancreatitis. EUS rather than MRCP may contribute to detect CBDS that are not visualized by CT.
# P-0395
Study on protruded lesion in the gallbladder suspicious of cancer
Park Kyunghwa1, Taku Aoki1, Genki Tanaka1, Takayuki Shiraki1, Yuhki Sakuraoka1, Takatsugu Matsumoto1, Takayuki Kosuge1, Shozo Mori1, Masato Kato1, Hidetsugu Yamagisi2 and Keiichi Kubota1
1Second Department of Surgery, Dokkyo Medical University; 2Department of Pathology, Dokkyo Medical University
Background: It is still difficult to make a correct diagnosis preoperatively for benign and malignant protruded tumor of the gallbladder. (Pt-Gb). The advance of ultrasound examination enables to find more Pt-Gb, but it is still difficult for ultrasound to make a qualitative diagnosis of Pt-Gb. Although there are many studies reporting the usefulness of other imaging modalities and EUS for qualitative diagnosis of Pt-Gb, the conclusion has not been made. In this study, we investigated the accuracy of preoperative qualitative diagnosis of Pt-Gb. Methods: Between April 2014 and August 2016, 25 patients with Pt-Gb were operated in our department. In these patients, we retrospectively reviewed preoperative diagnoses and postoperative, histological diagnoses of operative specimens. Results: In 25 patients, 4 patients were preoperatively diagnosed as benign and 21 patients were as malignant. And the discrepancy between preoperative and postoperative diagnoses was found in 17 patients. Preoperatively, all the 17 patients were diagnosed as having malignant lesions, but histological diagnosis revealed benign Pt-Gb. Among the preoperative, imaging modalities, PET was positive in 7 and negative in 10 patients. And the sensitivity and the specificity of CT, MRI, EUS, and PET were 25 and 75%, 30 and 65%, 100 and 60%, and 100 and 68%, respectively. Conclusion: Preoperatively, CT, MRI, EUS, and PET are reliable for diagnosing benign Pt-Gb. But these modalities are not reliable for diagnosing malignant Pt-Gb. It is suggested that, among these modalities, PET demonstrated the highest accuracy and should be performed routinely. On the other hand, accuracy of EUS is dependent on individual examiners, and much effort should be made to improve accuracy of EUS for preoperative diagnosis of Pt-Gb.
# P-0404
Preoperative endoscopic biliary drainage procedures may affect intrahepatic recurrence of cholangiocarcinoma after surgical resection
Sang-Woo Cha, Shin Ok Jeong, Young Deok Cho, Hyun Jong Choi, Jong Ho Moon and Sang Heum Park
Institute for Digestive Research and Digestive Disease Center, Department of Internal Medicine, Soon Chun Hyang University, College of Medicine, Seoul, South Korea
Background and Aim: Our aim is to determine the impact of preoperative endoscopic nasal biliary drainage (ENBD) and/or endoscopic retrograde biliary drainage (ERBD) procedures on intrahepatic recurrence rate in patients with cholangiocarcinoma after surgical resection. Method: Between January 2005 and January 2017, 143 patients were diagnosed with cholangiocarcinoma and received surgical resection. Among 143 patients, 99 patients were treated with preoperative ENBD and/or ERBD. We retrospectively analyzed prognostic factors (age, gender, preoperative ENBD and/or ERBD, tumor differentiation, pT factor, lymph node metastasis, surgical margin, lymphovascular invasion, preoperative maximal total bilitubin, postoperative chemoradiation/chemotherapy/radiation therapy, and CA19–9) for recurrence after surgical resection. Result: Intrahepatic recurrence after surgical resection was detected in 22/99 (22.2%) patients with preoperative ENBD and/or ERBD and in 5/44 (11.4%) patients without preoperative ENBD and/or ERBD for a median period of 12 months (range 0–48). On univariate analysis, intrahepatic recurrence rate of patients who underwent ENBD and/or ERBD (n = 99) was higher than those of patients who did not (n = 44) (P = 0.090) and those of patients who had T3/T4 factor (n = 74) was higher than those of patients who had T1/T2 factor (n = 69) (P = 0.168). Intrahepatic recurrence rate of patients who had elevated CA19–9 (>200) (n = 49) was higher than those of patients who had not (n = 94) (P = 0.002). In multivariate analyses, preoperative ENBD and/or ERBD and elevated serum CA19–9 level (>200 ng/mL) were prognostic factors for intrahepatic recurrence, with hazard ratios (HR) of 2.154 (95% confidence interval [CI] 0.893–7.626, P = 0.080) and 3.647 (95% CI 1.660–8.011, P = 0.001). Conclusion: Preoperative ENBD and/or ERBD procedures may affect the intrahepatic recurrence of the tumor in patient with cholangiocarcinoma after surgical resection. And serum elevated CA 19–9 level affected the intrahepatic recurrence of the tumor in patients with cholangiocarcinoma after surgical resection.
# P-0411
Diagnostic performance of FDG positron emission tomography/computed tomography for patients with extrahepatic cholangiocarcinoma
Hong Joo Kim
Internal Medicine, Sungkyunkwan University Kangbuk Samsung Hospital, Republic of Korea
Background: This study aimed to evaluate diagnostic values and prognostic relevance of PET-CT in patients with extrahepatic cholangiocarcinoma. Methods: One hundred sixty-three patients with confirmed diagnosis of extrahepatic cholangiocarcinoma who underwent FDG PET-CT at a single tertiary referral center between April 2008 and December 2014 were retrospectively and consecutively recruited and analyzed in the current study. Results: One hundred thirty (79.8%) out of 163 primary tumor lesions were correctly detected by FDG PET-CT, compared with 154 (94.5%) out of 163 primary tumor lesions in MDCT and 75 (97.4%) out of 77 primary tumor lesions in MRI. Thirty (18.4%) and 18 (23.4%) primary tumor lesions were detected in MDCT and MRI, respectively, and not detected in PET-CT (P < 0.01, compared with MDCT and MRI). Regional lymph node metastases were detected in 29 out of 64 (45.3%) patients by FDG PET-CT, in 49 out of 64 (76.6%) patients by MDCT, and in 23 out of 28 (82.1%) patients by MRI. Twenty-five (39.1%) out of 64 patients and 14 (50.0%) out of 28 patients showed false negative findings in regional lymph node metastasis by FDG PET-CT compared with MDCT (P < 0.01) and MRI (P < 0.01), respectively. Distant metastases were detected in 11 out of 13 (84.6%) patients by FDG PET-CT, in 9 out of 13 (69.2%) patients by MDCT, and in 6 out of 6 (100.0%) patients by MRI (P > 0.05). The cumulative overall survival rate was significantly higher in patients' group with common bile duct cancer (compared with hilar cholangiocarcinoma); well-differentiated histology; curative intent resection; lower pT and AJCC staging; N0, M0 staging; tumor size <25 mm; and SUVmax < 5. Conclusions: FDG PET-CT showed less reliable sensitivity in detecting primary tumor mass and regional lymph node involvement that could be detected by MDCT or MRI.
# P-0413
Primary Fistulotomy in patients with bile duct cannulation
Mu Song Jeon, Kahng Dong Hwahn, Geun Am Song, Gwang Ha Kim, Bong Eun Lee, Hye Kyung Jeon, In Sub Han and Moon Won Lee
Department of Gastroenterology, Pusan National University School of Medicine, South Korea
Background/Aims: Needle-knife fistulotomy has commonly been used for overcoming duct cannulation difficult bile duct cannulation. There are little data on primary fistulotomy in patients with bile. We aimed to assess the safety and complications of primary fistulotomy in patients with bile duct cannulation. Methods: We performed a retrospective study and enrolled 554 patients who underwent bile duct cannulation via endoscopic retrograde cholangiopancreatography (ERCP) at Pusan National University Hospital from January 2014 to December 2014. Two hundred seventy-two patients had naïve papilla and no biliary pancreatitis when admission. Patients were classified in three groups according to utilization of cannulation: 81 patients underwent conventional cannulation (group 1), 95 patients failed conventional cannulation and then, underwent P-duct stent insertion or precut fistulotomy (group 2), and 96 patients underwent primary fistulotomy (group 3). Complications after ERCP were defined as bleeding, post-ERCP pancreatitis, and perforation according to Cotton's criteria. Results: Between three groups, there were no significant differences in baseline characteristics. But bulging was more common in group 3. ERCP was successfully performed except for two cases in group 2 and one case in group 3. The post-ERCP pancreatitis rate was not significantly different between three groups (6.2%, 9.5%, 2.1%, pZ0.094). But hyperamylasemia was significantly different between three groups (11.1%, 17.9%, 6.3%, pZ0.043). There are no clinically significant bleeding or perforation in the three groups. Conclusions: Primary fistulotomy is effective and safe in achieving ductal access in patients with bile duct cannulation.
# P-0438
Endoscopic retrograde cholangiopancreatography (ERCP)—A novel risk factor for conversion of laparoscopic cholecystectomy
R G M S Nandasena1, M A C Lakmal1, A A Pathirana2 and B D Gamage2
1Professorial Surgical Unit, Colombo South Teaching Hospital; 2Department of Surgery, Faculty of Medical Sciences, University of Sri Jayawardenepura
Introduction: Laparoscopic cholecystectomy is the standard care for symptomatic gallstone disease. Although open cholecystectomy has a longer convalescence, it is considered a safe approach when difficulties are encountered during laparoscopic surgery. The conversion rate 10 to 25% is documented in the literature. Although studies have shown many risk factors for conversion, the effect of preoperative ERCP is scarce worldwide. Methods: Two hundred and two consecutive laparoscopic (LC) and laparoscopy converted to open (LCOC) cholecystectomies performed on patients attending a tertiary referral center from 2014 to 2016 were analyzed using spss version 20.0. Results: One hundred and thirty-three LC and 69 LCOC were done with a conversion rate of 34.1%. Majority were females (76%). Mean age was 46.35 years (range 16–80). Demographic data and surgical factors are comparable in both groups. Main indications for surgery were biliary colic (n = 81), calculous cholecystitis (n = 38), choledocholithiasis (n = 31), and gallstone pancreatitis (n = 10). All patients with choledocholithiasis underwent ERCP prior to cholecystectomy. Fifty-two percent and 6% had ERCP preoperatively in LCOC and LC groups, respectively (OR—13.9, 95% CI 5.8–32.9). Eighty-one percent of the patients who underwent ERCP had a conversion (P < 0.001). ERCP with common bile duct stenting (11%) had no significant correlation with the conversion. There is no significant association between number of ERCP and conversion (median—2, range 1–5). Mean duration after ERCP to surgery was 20.3 weeks (range 2–48 weeks) in LCOC group. No bile duct injuries were reported in both groups. Conclusion: ERCP is a significant risk factor for conversion according to our data. Longer mean duration after ERCP to surgery reported in our series may have contributed to higher conversion as early surgery has shown to minimize the risk of conversion in the literature. Post-ERCP patients should be informed about the higher risk of conversion, and the surgery should be performed by an experienced surgeon to minimize the risk.
# P-0439
Endoscopic papillary large balloon dilation for large or multiple common bile duct stones: Efficacy, safety, and stone recurrence
Takahiro Inoue, Yohei Taniguchi and Tetsuro Inokuma
Department of Gastroenterology, Kobe City Medical Center General Hospital, Japan
Background: Endoscopic papillary large balloon dilation (EPLBD) has been proposed as an alternative modality for endoscopic extraction of large or multiple common bile duct stones (CBDS). Although EPLBD was found to have a high success rate and an acceptable complication rate, there have been no reports on the recurrence of CBDS after EPLBD. This study evaluated the efficacy, safety, and stone recurrence rate in patients who underwent EPLBD for CBDS. Methods: Seventy-eight patients who underwent EPLBD at Kobe City Medical Center General Hospital from February 2013 to March 2017 were analyzed retrospectively. Parameters were compared in patients with and without stone recurrence, and the efficacy and safety of EPLBD and the stone recurrence rate were investigated. Results: The mean number of stones per patient was 4.3. The overall complete stone removal rate was 93.5%. The mean number of treatments was 1.07, with 92.3% of stones removed during the first session. Mean stone diameter was 14.2 mm, and mean balloon diameter was 13.5 mm. Complications occurred in five patients (6.4%), with three experiencing bleeding and one each experiencing pancreatitis and acute cholecystitis. CBDS recurred after bile duct clearance in 16 patients (20.5%). The mean interval between stone removal and stone recurrence was 5.9 months. None of the possible risk factors associated with recurrence differed significantly in groups of patients with and without recurrence. Conclusion: EPLBD is safe and effective in patients with large or multiple CBDS. Risk factors for CBDS after EPLBD were identified.
# P-0446
The safety of continuation antithrombotic agents undergoing percutaneous transhepatic biliary drainage
Tsubasa Yoshida, Shunsuke Watanabe, Masao Toki, Takeshi Nosaka, Oki Kikuchi, Tomoyuki Goto, Yuri Fukasawa, Hirotaka Ota, Kazushige Otiai, Koichi Gondo, Isamu Kurata, Tomohiko Hasue, Kenji Nakamura, Yasuharu Yamaguchi, Hideaki Mori, Shinichi Takahashi and Tadakazu Hisamatsu
Kyorin University School of Medicine, Japan
Background: The risk of percutaneous transhepatic biliary drainage (PTBD) in patients taking antithrombotic agents remains unknown. We investigated clinical course including the complication of hemorrhagic accident, retrospectively. Methods: We conducted a retrospective study of 101 patients who underwent PTBD between April 2016 and March 2017 at Kyorin University Hospital, Japan. Patients who continued taking antithorombotic agents were categorized as group I, and patients who discontinued for adequate duration or who did not take any antithorombotic agents were categorized as group II. We analyzed patients' backgrounds, the rate of bleeding complications in association with PTBD, success rate of procedure, and hospitalization period after treatment. Bleeding complication was defined as continuation of bleeding from the drainage tube during more than 3 days or requirement for transfusion within 3 days. Results: Patient number of group I/II was 16/85, respectively. There was no difference of the patient characteristics and underlying disease between the two groups. There was no difference between the types of antithrombotic agents and the types of PTBD. Number of patients who had bleeding in associated with procedure was occurred 0 in group I and 3 in group II, respectively, which meant that only group II had patients with bleeding in associated with procedure. Of the three patients who had bleeding, two patients recovered naturally without any therapeutic interventions, and one patient required several times of transfusion. Success rate of procedure was 100%. There was no difference between the two groups in the hospitalization period after the procedure (28 ± 15 days in group I, 24 ± 16 days in group II). Conclusion: In this retrospective study, there was no significant risk of bleeding in associated procedures in patients underwent PTBD with taking antithrombotic agents. It may suggest that it is possible to undergo PTBD safely in the patients who must continue taking antithrombotic agents.
# P-0457
Validation of Rome IV criteria for sphincter of Oddi disorder and therapeutic effect of endoscopic sphincterotomy by using new method of sphincter of Oddi manometry
Arata Sakai, Seiji Fujigaki, Atsuhiro Masuda, Ryota Nakano, Takashi Nakagawa, Takashi Kobayashi and Hideyuki Shiomi
Division Of Gastroenterology, Department Of Internal Medicine, Kobe University
Background/Aim: Sphincter of Oddi manometry (SOM) is not commonly performed because of its technical difficulty and the high incidence of post-procedural pancreatitis. To reduce post-procedural pancreatitis, we developed a new method of SOM with a guide-wire-type manometer. We had reported the usefulness of this new method. The Rome criteria for the functional gastrointestinal disorders was revised to fourth edition (Rome IV) in 2016. In this study, we validated the Rome IV criteria to examine the result of SOM with a guide-wire-type manometer and the efficacy of endoscopic sphincterotomy (EST) following SOM in patients with SOD diagnosed by the Rome III criteria retrospectively. Methods: A total of 47 procedures were performed in 15 patients with SOD and 14 patients with other diseases. SOD was diagnosed by the Rome III criteria. We performed SOM using the guide-wire-type manometer and measured amplitude, duration, and frequency of SO contractions. All SOD patients were performed EST following SOM. The symptomatic outcome (abdominal pain) after EST was evaluated on a four-level scale: no symptoms, improved, unchanged, and worse. Two of 15 patients could not follow up after EST. Results: In 40 of 47 evaluations (85%), amplitude, frequency, and duration could be analyzed. Severe pancreatitis was observed in one patient, and mild pancreatitis was observed in two patients after SOM. Among the parameters of SO pressure, amplitude (P = 0.0266) and frequency (P = 0.0014) in SOD patients was significantly greater than in non-SOD patients. EST was effective in 11 of 13 SOD patients (84.6%). Two cases for which EST were not effective were both biliary type 3 SOD. Conclusion: SO pressure in SOD patients showed abnormality. EST might be an effective treatment for SOD patients, except for biliary type 3. The Rome IV criteria for SOD is thought to be proper.
# P-0486
Clinical interpretation of elevated CA 19-9 levels in obstructive jaundice following benign and malignant pancreatobiliary disease
Min Seong Kim1, Tae Joo Jeon2, Ji Young Park2, Jeongmin Choi2, Won Chang Shin2, Seong Eun Park2, Ji-Young Seo2 and Young Moon Kim2
1Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, South Korea; 2Division of Gastroenterology, Department of Internal Medicine, Inje University Sanggye Paik Hospital, Inje University College of Medicine, Seoul, South Korea
Background/Aims: Elevated CA 19–9 level may be unable to differentiate between benign and malignant pancreatobiliary disease with obstructive jaundice. The study aims to determine the clinical interpretation and the diagnostic value of CA19–9 level in pancreatobiliary diseases with coexistent obstructive jaundice. Methods: We retrospectively reviewed the data of 981 patients who underwent biliary drainage because of obstructive jaundice following pancreatobiliary disease at Sanggye Paik Hospital for 5 years. One hundred fourteen patients with serial follow-up data for CA 19–9 level were included in this study (80 patients with malignancy and 34 patients with benign diseases). We compared the levels of CA 19–9 levels and the biochemical value before and after biliary drainage. Results: The rate of CA19–9 elevation (>37 U/mL) was significantly different between benign group and malignant group (59% vs 90%, P = 0.001). Despite the decrease in serum bilirubin after biliary drainage, CA 19–9 levels remained elevated in 12% of patients in the benign group and in 63% of patients in the malignant group (P < 0.001). Finally, 12% of patients in the benign group turned out to have malignant disease. An ROC analysis provided a cut-off value of 38 U/mL for differentiating benign disease from malignant disease after biliary drainage (area under curve, 0.787; 95% confidence interval, 0.703 to 0.871; sensitivity, 62%; specificity, 88%). Conclusions: This study suggested that we should consider the possibility of malignant causes if the CA 19–9 levels remain high or are more than 38 U/mL after resolution of biliary obstruction. Key Words: benign; CA 19–9 antigen; drainage; malignant; obstructive jaundice.
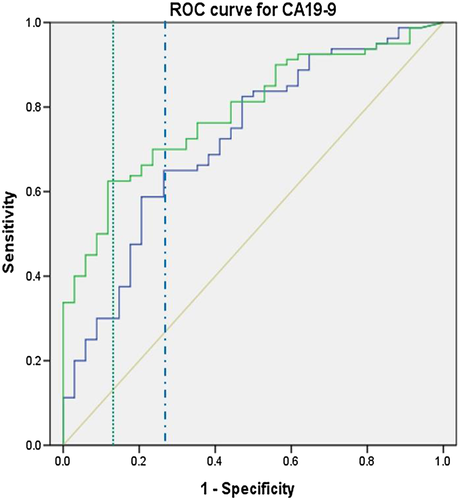
 , CA19–9 (before BD);
, CA19–9 (before BD);  , CA19–9 (after BD);
, CA19–9 (after BD);  , reference line.
, reference line.| — | Malignant (n = 80) | Benign (n = 34) | P value |
| Median CA 19–9 (range, U/mL) | 91.2 (0.6 ~ 10 000) | 14.1 (0.6 ~ 258.5) | — |
| Positive CA 19–9 (>37 U/mL) | 50 (63%) | 4 (12%) | <0.001 |
| Total bilirubin (mg/dL) | 1.5 ± 2.7 | 1.6 ± 2.5 | 0.969 |
| Alkaline phosphatase (U/L) | 193 ± 171 | 136 ± 105 | 0.117 |
| r-Glutamyl transpeptidase (U) | 145 ± 150 | 103 ± 102 | 0.197 |
- Values are presented as mean ± SD, range or number (%).
# P-0732
The efficacy of endoscopic transpapillary intraductal ultrasonography
Takahiro Nakazawa, Takashi Watanabe, Konomu Uno, Takanori Suzuki, Takeo Kanda, Hiromichi Araki, Tadashi Toyohara, Yuka Suzuki, Kazuhiro Nagao, Yusuke Mizuno, Atsunori Kusakabe, Hiroshi Kanie, Syuya Shimizu, Tomonori Yamada and Katsumi Hayashi
Department of Gastroenterology, Japanese Red Cross Nagoya Daini Hospital, Nagoya, Japan
Background and Aims: It is important to differentiate IgG4-SC from primary sclerosing cholangitis (PSC) or cholangiocarcinoma (CC) because the therapeutic strategy is different. We aimed to clarify the efficacy of endoscopic transpapillary intraductal ultrasonography (IDUS) in the differential diagnosis of IgG4-SC. Methods: We studied IDUS findings between IgG4-SC: (n = 92), PSC: (n = 42), CC: (n = 66). (i) IDUS findings at stricture site (IgG4-SC vs PSC): origin (wall thickness, extrinsic compression), symmetry (circular-symmetric, circular-asymmetric), inner margin (smooth, irregular), outer margin (clear, unclear), internal echo (homogeneous, heterogeneous), internal foci (present, absent), diverticulum-like outpouching (present, absent), three layers structure (preservation, disappear), the bile duct wall thickness. (ii) Frequency of diverticulum-like outpouching on ERC and IDUS (PSC). (iii) Wall thickness at non-stricture site (IgG4-SC vs CC). (iv) Symmetry and three layers preservation at non-stricture site (CC). Results: (i) Symmetric wall thickness, smooth inner margin, clear outer margin, and preserved three layers are significantly more frequently observed for IgG4-SC (P < 0.001). Irregular inner margin, diverticulum-like outpouching, and disappearance of three layers are significantly more frequently observed for PSC (P < 0.001). (ii) IDUS is more useful than ERC in the detection of diverticulum-like outpouching for PSC (68.8% vs 37.5% P = 0.077). (iii) 0.8 mm (sensitivity 95.5%, specificity 89.5%) and 1.0 mm (sensitivity 88.6%, specificity 97.4%) of wall thickness at non-stricture site are useful cutoff value for IgG4-SC. (iv) Symmetric wall thickness are detected in 20% at stricture site and 15% at non-stricture site. However, three layers are not preserved (disappearance 86%, partially preserved 14%) in CC. Conclusions: IDUS is useful in the differential diagnosis between IgG4SC, PSC, and CC.
# P-0824
Hepatobiliary tuberculosis with sclerosing cholangitis
Chiun Yann Ng, Lai Teck Gew, Raman Muthukaruppan, Jayaram Menon and Phei Onn Tan
Department of Medicine, Hospital Queen Elizabeth, Sabah, Malaysia
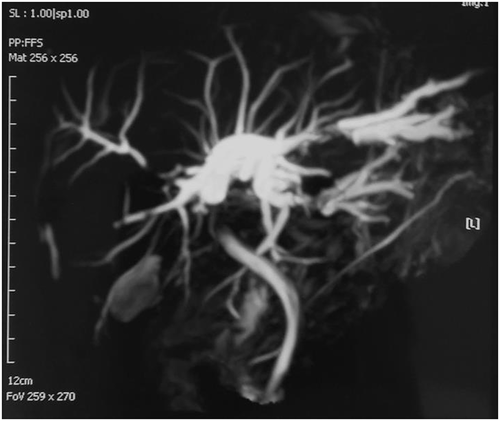
Introduction: Tuberculosis is a common disease in developing and underdeveloped countries. However, hepatobiliary tuberculosis is rare, and the manifestation can be atypical. Thus, high index of suspicion is needed to make a correct diagnosis to avoid delay in the management. We report a case of sclerosing cholangitis in a young man diagnosed with hepatobiliary tuberculosis and the challenges we faced in managing this patient. Case description: A 24-year-old man presented with obstructive jaundice and significant weight loss. Ultrasound of hepatobiliary system and computed tomography (CT) liver showed dilated intrahepatic ducts (IHD) with compression of common hepatic duct (CHD) by calcified granuloma. Endoscopic ultrasound (EUS)-guided fine needle aspiration of the necrotic mass at portal hepatitis showed chronic caseating granulomatous inflammation suggestive of tuberculosis infection. Multiple strictures were seen at IHD and CHD during endoscopic retrograde cholangiopancreatography (ERCP). Mycobacterium tuberculosis (MTB) was detected in the bile by polymerase chain reaction (PCR) and gene expert. Stenting was attempted but failed. Magnetic resonance cholangiopancreatography (MRCP) revealed 1.3 cm stricture in CHD, multiple strictures with dilatation of the IHD (Fig. 1). Ultrasound-guided percutaneous transhepatic biliary drainage (PTDB) was subsequently done, and it was followed by stent implantation through rendezvous technique of PTBD and ERCP. The obstructive jaundice improved tremendously after the procedure, and he was then started on anti-tuberculosis drugs.
# P-0894
Spontaneous cholecystocutaneous fistula—A harbinger of carcinoma of the gallbladder
Shraddha Shetty1 and Ramya Yethadka2
1Centre for Hepatopancreaticobiliary Sciences and Liver Transplantation, Fortis Hospital, Bangalore, India; 2Department of Surgical Oncology, Manipal Hospital, Bangalore, India
Introduction: Cholecystocutaneous fistulas are caused most often by neglected gallstone disease, surgical intervention in the biliary system, and trauma. They can be subclassified into spontaneous or iatrogenic. The number of spontaneous cholecystocutaneous fistulas in recent literature adds up to less than 30. The rarity of the entity in the modern era can be attributed to early diagnosis and treatment of biliary disease. Cholecystocutaneous fistula heralding a diagnosis of carcinoma of the gallbladder has only been reported four times before in literature, and here, we attempt to elucidate the fifth of such case. Case description: A 65-year-old lady presented to the OPD with complaints of a small exuberant mass in the epigastric region of the anterior abdominal wall associated with serosanguinous discharge since 6 months. She had previously undergone excision of this mass with recurrence in the ensuing 2 months. On examination, the presence of a sinus/fistula tract in the epigastric region was seen with friable granulation tissue at the mouth. Biopsy of the tissue yielded an inconclusive result; however, brush cytology of the fistula wall showed malignant cells. Further investigation with an ultrasound and contrast-enhanced computed tomography (CT) of the abdomen revealed an intraluminal lesion within the gallbladder abutting into the second part of the duodenum and extending into the skin of the anterior abdominal wall, which was further confirmed with a CT fistulogram. With a diagnosis of stage IV B gallbladder malignancy, the patient was given palliative chemotherapy with gemcitabine and succumbed to disease 6 months later.
# P-0969
Early post-ERCP cholecystitis—Severity, incidence and risk factors
S K Ravi Kiran1, A R Nitin Rao2, B Avinash1 and B S Satyaprakash1
1Department of Gastroenterology; 2Department of Surgical Gastroenterology, Ramaiah Medical College, MSR Nagar, Bangalore, India
Background: Post-ERCP complications like pancreatitis and cholangitis are a known entity and have been reported regularly. However, there is little published literature on the true incidence of post-ERCP cholecystitis (PEC) and the reasons for it to occur. The published literature cites an incidence of post-ERCP cholecystitis of 0.2% to 0.5%. We retrospectively investigated the incidence of PEC, its varying severity, interval of time between ERCP and development of cholecystitis, and risk factors for PEC. Methods: We studied all the patients who underwent ERCP at our institution between January 2016 and April 2017 and included all the patients who subsequently developed acute cholecystitis, empyema gallbladder, and gangrenous cholecystitis. All the diagnosis were made by need of interventional radiology or surgery. The variables studied include patient factors (age, gender, comorbidities, reasons for ERCP, and biliary anatomy), technical aspects of ERCP (number of passes, quantity of contrast used, and completion of desired therapeutic/diagnostic ERCP goal). Results: A total of 650 ERCPs were performed during the study period. Forty patients (6.1%) subsequent to ERCP developed acute cholecystitis/empyema gallbladder/gangrenous cholecystitis requiring either radiological intervention or laparoscopic/open surgical management. Presently we as we are analyzing the data, a complete analysis would be presented at conference. Conclusion: The world literature reports a low incidence of post-ERCP gallbladder pathology. However, our study shows it to be a much more common entity than generally reported and believed.
# P-1034
Percutaneous cholecystostomy for decompression of biliary obstruction
Jin Myung Park, Chang Don Kang and Sung Joon Lee
Department of Internal Medicine, Kangwon National University Hospital, South Korea
Background: Endoscopic cholangiopancreatography (ERCP) or percutaneous transhepatic biliary drainage (PTBD) is usually performed for biliary decompression in patients with biliary obstruction. Percutaneous cholecystostomy (PC) can be performed as a bridge therapy when ERCP and PTBD are impossible or failed. This study aimed to assess the effectiveness and safety of PC for biliary obstruction in cholangitis or pancreatitis. Methods: We analyzed our database of PC between March 2015 and March 2017. The patients who underwent PC for biliary decompression were reviewed retrospectively. Successful biliary decompression was defined as a decrease in serum bilirubin levels in patients with hyperbilirubinemia. In patients without hyperbilirubinemia, it was defined as improvement in fever and abdominal pain. Adverse events and pain after PC were compared with those of the patients who underwent PC for acute cholecystitis during the same period. Results: A total of 102 patients underwent PC, and it was done for biliary decompression in 14 patients (13 cholangitis and 1 pancreatitis). Successful biliary decompression was achieved in all patients. Adverse events occurred in 2 patients, and 13 patients had pain after PC. PC was performed for 88 patients with cholecystitis. Adverse events occurred in 6 patients, and 54 patients complained pain after PC. There was no statistical difference in incidence of adverse events between cholangitis/pancreatitis and cholecystitis group (14.3% vs 6.8%, P = 0.30). Pain after PC occurred more frequently in cholangitis/pancreatitis than cholecystitis group (92.9% vs 61.4%, P = 0.03). Conclusion: PC could be performed effectively and safely for decompression of biliary obstruction when ERCP and PTBD are impossible or failed. However, attention should be paid to management of pain.
# P-1042
Efficacy and safety of endoscopic gallbladder stenting
Tomoo Miyake1, Yoshihiro Nakashima2, Hirozumi Aoki1, Syunzou Tokioka1, Reiji Nishimon1, Atsushi Kitagawa1, Koji Yoshida2 and Keisuke Hino1
1Div. Hepatology and Pancreatology; 2Div. Interventional Bilio-Pancreatology, Kawasaki Medical School Hospital
Endoscopic gallbladder stenting (EGBS) is an alternative treatment option for high-risk surgical patients with acute cholecystitis. We investigated the cholecystitis recurrence rate in high-risk surgical patients in whom EGBS was performed and evaluate proper stent shape and length. Methods: Fifty-six consecutive high-risk surgical patients who treated by permanent EGBS for acute cholecystitis were enrolled between January 2012 and June 2016. Their median age was 83.3 years. Results: EGBS was successfully performed in 51 patients (91.1%). The median technical time was 35 min (range: 8–70). The average follow-up period was 243 days (range: 57–1120 days). The cholecystitis recurrence rates were 3.6% in the EGBS. In six patients, complications were observed. Post-ERCP pancreatitis, duodenum perforation or cholecystitis caused by stent dislocation. Distal site straight-shaped stent (7Fr) caused the perforation after gallbladder decompression. Conclusion: EGBS is useful for cholecystitis in high-risk surgical patients with calculous cholecystitis. However, stent-related adverse events may occur, and modifications are necessary to reduce these. Distal site pigtail-shaped stent is better to avoid intestinal perforation.