E-Poster Presentations - A4) Lower GI
# P-0010
An unusual cause of chronic diarrhea
Wing Yan Mak1, Yee Tak Hui1, Ting Wa Lam1, Wai Hon Li2 and Kam Hung Kwok3
1Department of Medicine; 2Department of Obstetrics and Gynaecology; 3Department of Surgery, Queen Elizabeth Hospital, Hong Kong
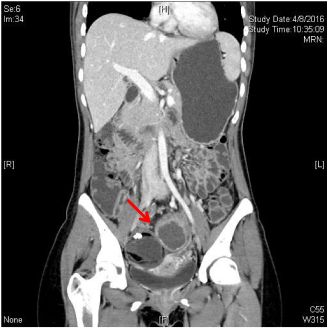
A 24-year-old lady with good past health complained of persistent blood-less diarrhea for 3 months. The frequency was up to 6 times per day, and there was lower abdominal discomfort and significant weight loss. Lower abdomen was soft but distended on examination. Blood tests revealed microcytic, hypochromic anemia and raised inflammatory markers (CRP 40; ESR 71).
Colonoscopy showed mild rectal inflammation only. Terminal ileum and colonic biopsies were unremarkable. Further imaging with CT enteroclysis showed a 6-cm right dermoid and a 9-cm left dermoid with air-fluid level. Fistulation to rectosigmoid junction was suspected. Repeated sigmoidoscopy showed a hair-like protrusion and suspected fistula opening at 10 cm above anal verge. Open right ovarian cystectomy, left salpingo-oophorectomy, and anterior resection of rectum with defunctioning ileostomy was performed. Intraop confirmed central 3-mm fistulation over left dermoid. Pathology was benign mature cystic teratoma. Patient had no more diarrhea. Closure of stoma was arranged.
CT enteroclysis showing left dermoid cyst and 2.2-cm internal fat-containing nodule with fistulation to rectosigmoid junction.
Reference
# P-0016
Combination therapy with 5-aminosalicylic acid and azathioprine compared with 5-aminosalicylic acid monotherapy for intestinal Behçet's disease
Joo Sung Kim1, Jihye Kim1, Jaeyoung Chun1, Youn Su Park1, Jee Hye Kwon1, Jee Hyun Kim1, Jooyoung Lee1, Jong Pil Im1 and Jae Hee Cheon2
1Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea; 2Department of Internal Medicine and Institute of Gastroenterology, Yonsei University College of Medicine, Seoul, Korea
Background/Aims: Treatment of intestinal Behçet's disease (BD) has not been established yet. The aim of this study was to assess the efficacy of combination therapy with 5-aminosalicylic acid (5-ASA) and azathioprine compared with 5-ASA monotherapy for induction treatment in patients with intestinal BD. Methods: We retrospectively reviewed the medical records of all patients who were diagnosed with intestinal BD and treated with 5-ASA for at least 6 months at Seoul National University Hospital and Severance Hospital from March 1986 to December 2014. Among them, patients who were treated with 5-ASA alone (monotherapy group), or concomitant azathioprine which started within 3 months after initiation of 5-ASA (combination group) were included. Primary endpoints were clinical remission (CR) at 6 months and 1 year after initiation of 5-ASA, defined as a disease activity index of intestinal BD (DAIBD) score less than 20. The secondary endpoints were clinical relapse after CR, intestinal BD-related surgical treatment and hospitalization, mortality, and adverse drug events. Results: A total of 98 patients were enrolled in this study. The mean follow-up was 6.2 years. Among them, 35 patients (35.7%) were enrolled in combination group. Mean DAIBD scores at diagnosis of intestinal BD in combination group (65.2) were significantly higher compared with monotherapy group (51.5) (P = 0.029), and all patients in combination group had moderate (67.8%) or severe disease activity (32.1%) of intestinal BD at the diagnosis. CR at 6 months after initiation of 5-ASA were 53.5% and 62.9% in monotherapy and combination group, respectively. CR at 1 year after initiation of 5-ASA in combination group (66.7%) was not significantly different from that in monotherapy group (56.1%). The rate of clinical relapse after CR was 50.0% and 52.9% in monotherapy and combination group, respectively. No patient underwent surgery for intestinal BD-related complications during the follow-up.
Conclusion: Combination therapy with 5-ASA and AZA within 3 months from initiation of 5-ASA may be not superior to 5-ASA monotherapy for induction of CR in patients with intestinal BD.
# P-0028
Relapse prevention in ulcerative colitis through educational hospitalization providing plant-based diet experience
Mitsuro Chiba1, Kunio Nakane1, Tsuyotoshi Tsuji1, Satoko Tsuda1, Hajime Ishii1, Hideo Ohno1, Kenta Watanabe1, Mai Ito1, Masafumi Komatsu1, Koko Yamada2 and Takeshi Sugawara3
1Division of Gastroenterology, Akita City Hospital, 010-0933, Akita, Japan; 2Nutrition Room, Akita City Hospital, 010-0933, Akita, Japan; 3Division of Gastroenterology, Nakadori General Hospital, 010-8577, Akita, Japan
Background: No studies has evaluated the effect of a plant-based diet (PBD) in ulcerative colitis (UC). To determine whether educational hospitalization providing PBD experience prevents relapse in patients with UC. Methods: Patients with mild UC or UC in remission that did not need immediate treatment were included. A PBD and dietary guidance were provided during a 2-week hospitalization. Medication already prescribed by a doctor was maintained during hospitalization; otherwise, no medicatiosn was administered. The primary endpoint was relapse during the follow-up period. Relapse was defined as a flare up that required more aggressive treatment. Kaplan–Meier analysis was used to calculate the cumulative relapse rate. The secondary endpoints were immediate improvement in symptoms or laboratory data during hospitalization and a chronological change in the plant-based diet score (PBDS), which evaluated adherence to the PBD. This research has been approved by an ethical committee. Results: Sixty cases were studied (29 initial episode cases and 31 relapse cases). Median age was 34 years. Proctitis was seen in 31 patients, left-sided colitis in 7, extensive colitis in 22; medication in 37 and non-medication in 23. Median follow-up period was 2 years 6 months. Six cases relapsed during follow-up. There were no differences in cumulative relapse rates between initial episode cases and relapse cases. Cumulative relapse rates (n = 57) at 1, 2, 3, 4, and 5 years of follow-up were 2%, 4%, 7%, 17%, and 17%, respectively. Immediate clinical improvements during hospitalization were observed in 31 of 40 patients (78%) including remission in 11 (28%). The PBDS of 21.7 at a mean follow-up of 14.9 months for 22 cases was higher than their baseline PBDS of 7.7 (P < 0.0001). Conclusion: Relapse rates after educational hospitalization providing a PBD experience are low compared with those reported with medication. Educational hospitalization is effective at inducing habitual dietary changes.
# P-0041
Characteristics of colonoscopic findings and clinical manifestations of lower gastrointestinal bleeding in patients with chronic kidney disease
You Sun Kim, Jin Young Kim, Kyung Jin Lee, Ho Seok Koo, Hyun Mee Lee, Jeong Seop Moon and Haeng Il Koh
Department of Internal Medicine, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea
Introduction: Patients with chronic kidney disease (CKD) are more likely to have lower gastrointestinal bleeding (LGIB) risk. Several factors of CKD patients including platelet dysfunction due to uremia, poor blood supply, and frequent use of anticoagulant agents are suggested to increase the LGIB. This study aims to investigate the colonoscopic findings of LGIB in CKD patients. Methods: A total of 230 hospitalized CKD patients who underwent colonoscopy due to suspected LGIB between January 2003 and August 2016 were reviewed retrospectively. We categorized CKD into 5 stages by estimated glomerular filtration rate (eGFR) (stage 1, ≥ 90; stage 2, 60 ≤ < 90; stage 3, 30 ≤ < 60; stage 4, 15 ≤ < 30; stage 5, < 15 mL/min/1.73 m2) and compared characteristics of colonoscopic findings and clinical manifestations of LGIB. Results: Among 230 CKD patients who suspected having LGIB, a total of 31.7% (73 patients, 103 cases) had been confirmed having actual LGIB by colonoscopy. Actual LGIB patients comprised 35 (47.9%) men, and their mean age was 65.7 ± 12.8 years. Most common causes of LGIB were hemorrhoid bleeding (32 cases, 43.8%), followed by colorectal ulcer bleeding (21 cases, 28.8%), diverticular bleeding (12 cases, 16.4%), colitis bleeding (12 cases, 16.4%), and angiodysplasia (12 cases, 16.4%). As progression of CKD stage, the incidence of LGIB is also increased (P = 0.002). In addition, the proportion of colorectal ulcer (P = 0.049) and colitis (P = 0.025) are increased according to progression of CKD stage. LGIB is more frequently occurred in CKD patients with hemodialysis (P = 0.001) and hypoalbuminemia (P = 0.002). Conclusions: In CKD patients, the risk of LGIB is significantly increased related with decrease of kidney function, hemodialysis, and hypoalbuminemia. The possibility of LGIB due to colorectal ulcer and colitis is increased in advanced CKD stage. Clinicians should pay attention regarding the risk of LGIB in hospitalized CKD patients
# P-0042
Rapid and accurate diagnosis of Clostridium difficile infection by real-time PCR
You Sun Kim1, Pil Hun Song1, Jung Hwa Min1, Yong Moon Woo1, Hyun Mee Lee1, Jeong Seop Moon1 and Dong Hee Whang2
1Departments of Internal Medicine; 2Laboratory Medicine, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea
Background/Aims: The incidence and severity of Clostridium difficile infection (CDI) have increased worldwide, resulting in a need for rapid and accurate diagnostic methods. Methods: A retrospective study was conducted to compare CDI diagnosis methods between January 2014 and December 2014. The stool samples which were obtained in presumptive CDI patients were compared for the diagnostic accuracy and rapidity, including real-time PCR of toxin genes, C. difficile toxin assay, and culture for C. difficile. Results: A total of 207 cases from 116 patients were enrolled in this study and 117 cases (56.5%) were diagnosed as CDI. Among the 117 cases, the sensitivities of real-time PCR, C. difficile toxin assay, and culture for C. difficile were 87.2% (102 cases, 95% CI: 80.7–92.8%), 48.7% (57 cases, CI: 41–59.8%), 65.0% (76 cases, CI: 60.2–78.5%), respectively (P < 0.005). Notably, 34 cases (29.0%) were diagnosed as CDI by real-time PCR only. The time required to obtain results was 2.27 hours (136.62 ± 82.51 minutes) for real-time PCR, 83.67 hours (5020.66 ± 3816.38 minutes) for toxin assay, and 105.79 hours (6347.68 ± 3331.46 minutes) for culture (P < 0.005), respectively. Conclusions: We confirmed that real-time PCR of toxin genes is the most effective diagnostic method for accurate and early diagnosis of CDI. It also helps to diagnose hypervirulent CDI, such as ribotype 027 infection.
# P-0049
The clinical and ultrasound feature of appendicular mucinous adenocarcinoma
Lingxia Tong, Na Qi and Pengyuan Zheng
Department of Utrasound, JiLin Tumor Hospital, China
Aim: The aim is to increase the accuracy rate of diagnosis by analyze the clinical and ultrasound feature of appendicular mucinous adenocarcinoma. Methods: A retrospective analysis was made on the clinical data and ultrasound feature of 8 cases of appendicular mucinous adenocarcinoma which confirmed by surgery pathology in our hospital. Results: In 8 patients, 2 females and 6 males, 8 patients all felt abdominal pain, Clinical manifestations of 4 patients were abdominal pain and diarrhea, 3 cases in clinical were palpable mass. The ultrasonic manifestations were as follows: 8 patients are shown as mixed mass, 5 cases predominantly presented with a cystic mass and 2 cases solid-appearing mass, 1 case presented half of cystic or solid. The form of 5 masses presented irregular, 3 cases were oval or nearly circular. The form of solid part all presented irregular in 8 cases, 5 masses showed unclear boundary and 3 clear. Four masses showed calcified area inside capsule wall. All of the 8 cases were blood flow signal on CDFI. There were 2 cases that showed ascites. Conclusion: Ultrasonography of appendicular mucinous adenocarcinoma is mixed mass, almost of the form was irregular, and the boundary was unclear; the solid part of mass was irregular; calcified was shown inside capsule wall; and spot and linear blood flow signals were present on the solid part of masses from CDFI. We can enhance the rate of ultrasonic diagnose with the clinical feature.
# P-0062
Anxiety and female gender are related to IBS in medical student using new Rome IV criteria
Ardhi Rahman Ahani, Ari Fahrial Syam, Rudi Putranto and Pringgodigdo Nugroho
Department of Internal Medicine, Faculty of Medicine Universitas Indonesia-Cipto Mangunkusumo National Referral Hospital, Jakarta, Indonesia
Background: The irritable bowel syndrome (IBS) needs special attention because of its high morbidity and cost. In general, IBS prevalence in medical student is higher than common population because being in constant stressful condition. The aim of study was to know the related factors causing IBS using new Rome IV criteria. Method: A cross-sectional study of 350 Universitas Indonesia medical students from first grade until fifth grade was done during November–December 2016. This study used stratified randomized sampling. The Rome IV criterion was used for diagnosing IBS. This research has been approved by an ethical committee. Questionnaire-guided interview was applied to all subjects. A bivariate analysis was done to know relationship between IBS and its related factors using chi-square, unpaired t-test, and their alternatives. Multivariate analysis was done using logistic regression test. Results: The IBS proportions were 18.3% (95% CI 15.4–21.2) in the female medical students and 9.7% (95% CI 7.5-11.9) in the male medical students. The highest subtype was diarrhea subtype (53.1%). Both student-life stress inventory score (stressor and response to stressor) were higher in IBS group than in non-IBS group (For stressor (66.4 + 11.4) vs (60.0 + 12.2), P = 0,001) and for response to stressor (64.0 (41–97) vs 55.0 (35–88), P < 0.0001). Anxiety and female gender were related to IBS ((OR 2.89; 95% CI 1.43–5.83) and (OR 2.14; 95% CI 1.12–4.08)). Conclusions: The IBS prevalence in medical student of Universitas Indonesia using new Rome IV criteria was 14%. Meanwhile, the IBS proportions were 18.3% (95% CI 15.4–21.2) in the female medical students and 9.7% (95% CI 7.5–11.9) in the male medical students with predominant diarrhea subtype (53.1%). Anxiety and female gender were significantly related to IBS.
# P-0065
Reduction in the risk of mortality by performing mass screening for colorectal cancer using fecal occult blood testing in combination with flexible sigmoidoscopy
Ryoichi Nozaki, Kazutaka Yamada and Masahiro Takano
Coloproctology Center, Takano Hospital, Kumamoto, Japan
Background: The efficacy of fecal occult blood testing (FOBT) and flexible sigmoidoscopy (FS) for colorectal cancer (CRC) screening have been well documented, but the efficacy of FOBT in combination with FS has not yet been established. The aim of this study was to investigate the efficacy of FOBT in combination with FS to determine whether or not a reduction in the CRC mortality rates could be achieved. Methods: A population-based case–control study was conducted in areas where no previous and no other concomitant CRC screening had been performed. A total of 118 patients diagnosed with CRC, including 49 cases with rectal cancer and 14 cases with sigmoid colon cancer, were included in this study. Controls were residents who were confirmed to be alive at the time the patients were diagnosed with CRC and whose gender, age (±3 years), and addresses were matched. The case control ratio was 1:3. The relative risk of CRC mortality for individuals with a history of FOBT in combination with FS screening was calculated as the odds-ratio (OR). Results: The OR of subjects with a history of FOBT in combination with FS screening and corrected for FOBT single screening was 0.51 (95% confidence interval: 0.24 to 1.05) for colon cancer in general and 0.33 (0.12 to 0.92) for rectal and sigmoid colon cancer. Moreover, the observation period for each kind of cancer was examined. The OR for colon cancer in general (within 7 years) was 0.31 (0.10 to 0.90), and rectal and sigmoid colon cancer (within 7 years) was 0.17 (0.04 to 0.66). However, there was no significant reduction in the OR of proximal colon cancer deeper than the descending colon (0.40; 0.05 to 3.46) even within a year. Conclusion: These findings suggest that FOBT in combination with FS screening may reduce the mortality rate of CRC.
# P-0068
The Asia-Pacific colorectal screening score is useful to stratify risk for colorectal advanced neoplasms in Vietnamese patients with irritable bowel syndrome
Duc Trong Quach1,2, Toru Hiyama3, Thu Anh Nguyen1,4, Hoa Quoc Ly1,5 and Shinji Tanaka6
1Department of Internal Medicine, University of Medicine and Pharmacy, Hochiminh, Vietnam; 2Department of Gastroenterology, Gia-Dinh People's Hospital, Hochiminh, Vietnam; 3Health Service Center, Hiroshima University, Higashihiroshima, Japan; 4Department of Gastroenterology, Trung-Vuong Hospital, Hochiminh, Vietnam; 5Department of Gastroenterology, Can-Tho City General Hospital, Can-Tho, Vietnam; 6Department of Endoscopy, Hiroshima University Hospital, Hiroshima, Japan
Background: The Asia Pacific Colorectal Screening (APCS) score has been validated in several populations but not yet in patients with irritable bowel syndrome (IBS). Aim: To assess the performance of APCS score in stratifying risk of colorectal advanced neoplasms (CAN) in Vietnamese IBS patients. Methods: Consecutive patients who fulfilled IBS diagnosis criteria according to the Rome III were prospectively enrolled and underwent colonoscopy. APCS score for each patient was calculated by summing the points attributed by risk factors. Three tiers of risk were defined: 0–1 “average risk” (AR); 2–3 “moderate risk” (MR); and 4–7 “high risk” (HR). Logistic regression analysis was performed to assess the relative risk of CAN in HR group and MR group compared with AR group. Results: There were 404 patients with excellent bowel preparation and complete colonoscopy. The mean age was 48.8 ± 11.2 years and male : female ratio was 1.2:1. Twenty-eight patients (6.9%) were diagnosed with CAN: 19 (4.7%) advanced adenoma and 9 (2.2%) invasive CRC. Patients in the MR and HR tiers had 5.6-fold (95% CI 1.2 to 24.7, P = 0.012) and 12.1-fold (95% CI 2.6 to 56.2, P < 0.001) increased rates of CAN compared to those in the AR tier, respectively. Three out of 9 patients with invasive CRC had no alarm features but had high sum APCS score (2 in MR tier and 1 in HR tier). Conclusion: The APCS score is useful to identify IBS patients with high risk of CAN for colonoscopy priority.
Key words: Colon cancer, Vietnamese, irritable bowel syndrome
# P-0074
Aging, current smoking, and metabolic factors are independently associated with the prevalence of colorectal neoplasia in Japan
Nagamu Inoue, Rieko Bessho, Toshifumi Yoshida, Kazuhiro Kashiwagi, Yoshinori Sugino and Yasushi Iwao
Center for Preventive Medicine, Keio University School of Medicine, Tokyo, Japan
Background and Aims: For the past decades, the incidence and mortality rate of colorectal cancer (CRC) has been increased in Japan. The association of metabolic syndrome (MetS) and CRC has been reported in several studies; however, individual factors contributing to development of CRC have been obscure, especially in Japan. In the present study, we investigated the risk factors such as metabolic and lifestyle factors for development of colorectal neoplasia (CRN) including adenomatous polyps as precancerous lesions by using comprehensive health checkup data. Methods: Among 7213 subjects who took comprehensive health checkup at our hospital between in August 2012 and July 2015, 1772 subjects who also underwent screening colonoscopy were analyzed. CRN was defined as adenomatous polyp ≥ 5 mm in size and adenocarcinoma. Demographic characteristics, anthropometric measurements, visceral fat area (VFA), hematological metabolic parameters, and current smoking and drinking habits were assessed. Association between variables and CRN was evaluated by univariate analysis and then by multivariate analysis using multiple logistic regression model. A P value < 0.05 was considered statistically significant. Results: Of 1772 subjects analyzed, 195 subjects had CRN (11.0%) and 5 had invasive colorectal cancer (0.3%). Four hundred and forty-six subjects were diagnosed as MetS (25.2%), and presence of MetS was significantly associated with CRN (P < 0.01). Univariate analysis identified significant association of age, body mass index (BMI), VFA, systolic blood pressure (SBP), low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides (TG), fasting plasma glucose, hemoglobin A1c (HbA1c), fatty liver, current smoking habit, and current drinking habit with prevalence of CRN. Logistic regression analysis revealed that age, current smoking, BMI, SBP, LDL and HDL cholesterol, and TG were independent factors associated with CRN prevalence. Conclusion: The present study demonstrated that metabolic factors in addition to aging and current smoking might be risk factors for CRN in Japan.
# P-0082
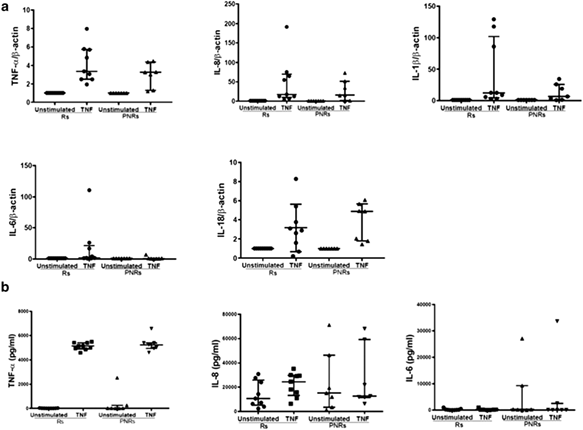
Serum-derived hyaluronan-associated protein (SHAP) is a novel biomarker for inflammatory bowel diseases
Yoshiharu Yamaguchi1, Hisatsugu Noda1, Noriko Okaniwa1, Kazunori Adachi1, Tetsuya Shinmura1, Shoko Nakagawa1, Masahide Ebi1, Naotaka Ogasawara1, Yasushi Funaki1, Lisheng Zhuo2, Koji Kimata2, Makoto Sasaki1 and Kunio Kasugai1
1Department of Gastroenterology, Aichi Medical University School of Medicine, 1-1 Yazakokarimata, Nagakute, Aichi, Japan; 2Research complex for Medicine Frontiers, Aichi Medical University, 1-1 Yazakokarimata, Nagakute, Aichi, Japan
Background/Aims: Serum-derived hyaluronan-associated protein (SHAP) has been shown to relate inflammatory diseases. We evaluated the role of SHAP in inflammatory bowel disease (IBD) pathogenesis and its potential as a novel IBD biomarker. Methods: We compared serum concentrations of SHAP or clinical variables inflammatory markers with normal controls and studied SHAP expression in DSS-treated intestinal mice samples and in human intestinal samples of IBD by histological analysis. Results: In DSS-treated mice, the serum SHAP was significantly elevated compared with the concentration in control mice (8.2 ± 2.3 ng/mL vs 5.1 ± 0.9 ng/mL, P < 0.01). Serum SHAP was positively correlated with the histological damage of the colon (r = 0.566, P < 0.001). In ulcerative colitis patients, serum SHAP was significantly higher in patients with active than remission (9.1 ± 5.6 ng/mL vs 5.0 ± 4.0 ng/mL, P < 0.05), and this value was positively correlated with erythrocyte sedimentation rate, serum levels of tumor necrosis factor (TNF)-α, and Mayo endoscopic grade (r = 0.568, P < 0.001; r = 0.521, P < 0.001; and r = 0.641, P < 0.001, respectively). In Crohn's disease, there was no difference in serum SHAP between patients with active disease and those in remission, but there was a relation with TNF-α levels (r = 0.630, P = 0.002). SHAP staining was observed in the fibroblasts of the colonic epithelium and submucosa. SHAP staining was recognized in the vascular endothelial cells and in the area surrounding blood vessels that were adhered to leucocytes. Conclusion: We propose that SHAP is related to colitis pathogenesis and may play a role in modulating disease activity. This may be a novel biomarker for IBD and a potential therapeutic target molecule.
Key words: serum-derived hyaluronan-associated proteins, hyaluronan, inflammatory bowel diseases, biomarker
# P-0097
Intensive granulocyte–monocyte adsorptive apheresis twice a week for treatment of ulcerative colitis: A Japanese single-center study
Hiroki Tanaka, Kohei Sugiyama, Maki Miyakawa, Masanao Nasuno and Satoshi Motoya
IBD Center, Sapporo Kosei General Hospital, Sapporo, Japan
Background/Aims: Intensive granulocyte–monocyte adsorptive apheresis (GMA) administered twice a week for the treatment of ulcerative colitis (UC) achieves remission more effectively and faster than weekly administration. We investigated the efficacy and related prognostic factors in patients with UC treated by intensive GMA. Methods: We retrospectively analyzed the data of active UC patients who received intensive GMA treatment from April 2010 to March 2016. We excluded patients with a Lichtiger clinical activity index (CAI) score of ≤ 4 and those who received additional medical treatments within 1 week before or after GMA treatment. GMA was performed using the Adacolumn (JIMRO, Takasaki, Japan). Each patient received GMA twice a week for 5 weeks with a maximum of 10 treatments. Remission was defined as a CAI score of ≤ 4 within 10 GMA treatments. We investigated the remission rate and time required for remission. Prognostic factors related to the remission rate were evaluated using univariate analysis. Results: Of the 101 patients included in this study (mean age, 43.3 years), 37 were females. The mean duration of disease was 5.4 years, and the mean CAI score was 9.4 at baseline. Sixty-one patients had pancolitis, 31 had left-sided colitis, and 9 had proctitis-type colitis. There were 43 steroid-naïve, 39 steroid-dependent, and 19 steroid-resistant patients. Remission was achieved in 51% with a mean time to remission of 14.3 days, and significantly in patients with low CAI scores at baseline (average CAI score was 8.8 of the remission group and 10.0 for the nonremission group, P = 0.037). Conclusion: About 50% of UC patients treated by intensive GMA achieved remission within 2 weeks on average. Higher CAI scores at baseline could be a poor predictor of remission.
# P-0098
Long-term outcome and related prognostic factors of infliximab maintenance treatment for Japanese patients with Crohn's disease: A Japanese single-center study
Maki Miyakawa, Hiroki Tanaka, Kohei Sugiyama, Masanao Nasuno and Satoshi Motoya
IBD Center, Sapporo Kosei General Hospital, Sapporo, Japan
Background/Aims: There are few reports about maintenance treatment with infliximab (IFX) for Asian patients with Crohn's disease (CD). We evaluated IFX maintenance treatment for Japanese CD patients based on long-term outcomes and related prognostic factors. Methods: Retrospective data were collected from luminal CD patients who received IFX for ≥ 14 weeks between 2003 and 2015. IFX maintenance treatment was evaluated using rate of sustained clinical benefit—defined as lack of treatment failure—which was estimated using the Kaplan–Meier method. Treatment failure was defined as either discontinuation of IFX, dose escalation, or intestinal resection for CD. Prognostic factors associated with the rate of sustained clinical benefit were evaluated using multivariate Cox regression analysis. Results: Of the 308 patients included in this study (mean age, 30.8 years), 80 were females. The mean duration of the disease was 7.1 years and the mean C-reactive protein (CRP) level at baseline was 2.07 mg/dL. Seventy-three patients had ileitis, 177 had ileocolitis, and 58 had colitis. One hundred sixty-three patients were diagnosed with inflammatory disease, 103 with stricturing disease, and 42 with penetrating disease. Concomitant treatment with immunomodulators (IM) was administered to 219 patients. Before initiating infliximab therapy, 100 patients had undergone at least 1 intestinal resection. The 2-, 4-, 6-, and 8-year sustained clinical benefit rates were 64%, 53%, 45%, and 38%, respectively. In the multivariate Cox regression analysis, stricturing disease and a higher CRP level at baseline were identified as poor predictors of sustained clinical benefit, whereas concomitant treatment with IM was identified as a good predictor. Conclusions: The treatment failure rate in patients with CD receiving IFX maintenance treatment was about 60% but was decreased by combination therapy of IFX with IM. Conversely, stricturing disease and a higher CRP level at baseline were prognostic factors for a poor long-term outcome.
# P-0099
Efficacy of Multi Matrix System mesalazine for the induction of remission in patients with ulcerative colitis who insufficiently respond to other mesalazine formulations: A Japanese single-center study
Kohei Sugiyama, Hiroki Tanaka, Maki Miyakawa, Masanao Nasuno and Satoshi Motoya
IBD Center, Sapporo Kosei General Hospital, Sapporo, Japan
Background/Aims: Multi Matrix System (MMX) mesalazine has been approved in Japan for the treatment of ulcerative colitis (UC). We evaluated the efficacy of MMX mesalazine for the induction of remission in patients with UC who insufficiently respond to pH- or time-dependent mesalazine. Methods: Retrospective data were collected from active UC patients who switched to MMX mesalazine 4.8 g/day because of an insufficient response to 3.6 g/day of pH- or 4.0 g/day of time-dependent mesalazine between December 2016 and February 2017. Patients with a partial Mayo score (pMS) of ≤ 4 and those who received other remission induction therapy at baseline were excluded. The efficacy of switching to MMX mesalazine was evaluated by the decrease in pMS, which was calculated at baseline, 2 weeks, and 4 weeks. Remission was defined as a decrease in pMS to ≤ 2. Prognostic factors related to the remission rate were evaluated using univariate analysis. Results: Of the 21 patients included in this study (mean age, 44.3 years), 14 were female. The mean duration of disease was 7.5 years, and the mean pMS was 4.6 at baseline. Ten patients had pancolitis, 8 had left-sided colitis, and 3 had proctitis-type colitis. Concomitant treatment with immunomodulators and local mesalazine was administered in 3 and 8, respectively. Previous treatment included pH- and time-dependent mesalazine in 15 and 6 patients, respectively. pMS at 2 weeks significantly decreased to 3.0 and at 4 weeks to 2.7. The remission rate at 2 weeks was 48% and at 4 weeks was 57%. No significant prognostic factor related to the remission rate was identified in the univariate analysis. Conclusion: Switching to MMX mesalazine 4.8 g/day in UC patients insufficiently responding to 3.6 g/day of pH- or 4.0 g/day of time-dependent mesalazine is effective and should be considered.
# P-0110
Clinical features of nosocomial diarrhea with and without Clostridium difficile infection: A comparative study
Unchana Sura-Amonrattana1, Pattarachai Kiratisin2 and Monthira Maneerattanaporn1
1Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand; 2Department of Microbiology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
Background/Aims: Nosocomial diarrhea (ND) is common, and routine laboriously investigations were usually applied. It is not uncommon that patients with ND be empirically treated as C. difficile associated diarrhea (CDAD) regardless of the test for CDAD. We aimed to compare manifestations of CDAD to non-CDAD. Methods: We conducted 1:4 cross-sectional study. Patients with ND who had stool test for C. difficile were recruited from December 2014 to October 2016. Demographic data, clinical features, investigations, laboratory findings, management, and outcomes were recorded. Statistical analysis was computed using SPSS version18. Results: A total of 360 ND cases that had stool test for C. difficile were recruited. Seventy seven (21.4%) had CDAD (+ stool for C. difficile). Mean age, gender distribution, and comorbidities between groups were similar. Factors associated with CDAD including hypoalbuminemia < 3.5g/dL, previous hospitalization, receiving corticosteroids, white blood cell, and concurrent C. difficile infection in the same ward were identified (Table 1). Common drugs usage (BLBIs & PPIs) and modes of feeding between groups were not different [(BLBIs; 43.4% non-CDAD vs 24.1% CDAD; P = 0.09), (PPI; 83% non-CDAD vs 80.5% CDAD; P = 0.606)], enteral feeding (67.1% non-CDAD vs 55.8% CDAD; P = 0.132). Empirical treatment of CDAD was prescribed in 46.3% in non-CDAD and 89.6% in CDAD group (P < 0.001). Response rates (diarrhea resolved within 7 days after treatment initiation) were comparable (56.9% non-CDAD vs 55.8%CDAD; P = 0.23). Although severity of disease between groups were comparable, mortality rate in CDAD is significantly higher of 23.4% and 13.4% in non-CDAD; P = 0.033. Discussion and Conclusion: The incidence of CDAD has been increased. Most risk factors of CDAD in our study were consistent with the existing evidence but PPI and BLBIs were indifference. Concurrent CDAD in the same ward, which have not mentioned before, is also predictor of CDAD. The CDAD group had higher mortality although disease severity between groups was similar.
| Risk factor | Non-CDAD (N = 283) | CDAD (N = 77) | OR(95%CI) | P value |
|---|---|---|---|---|
| Previous hospitalization | 146(51.6%) | 58(75.3%) | 2.864(1.623–5.056) | < 0.001 |
| Receiving corticosteroids | 44(15.5%) | 22(28.6%) | 2.173(1.205–3.919) | 0.009 |
| Concurrence of C. difficile infection in the same ward | 6(2.1%) | 5(6.5%) | 4.038(1.019–16.009) | 0.047 |
| Abdominal pain | 15(5.3%) | 7(9.1%) | 1.787(0.701–4.551) | 0.28 |
| White blood cells (WBC) | 9,700(6,280–14,220) | 11,260(9,490–14,720) | — | 0.02 |
| Hypoalbuminemia | 212(74.9%) | 67(87%) | 2.244(1.096-4.595) | 0.024 |
| Severity | 82(29%) | 16(20.8%) | 0.643(0.350-1.180) | 0.152 |
# P-0118
Five-year clinical outcomes of Crohn's disease: A report of 287 multiethnic cases from an international hospital in Thailand
Vibhakorn Permpoon1 and Krit Pongpirul2,3,4
1Digestive Disease Center, Bumrungrad International Hospital, Bangkok, Thailand; 2Department of Preventive and Social Mecicine, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand; 3Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA; 4Bumrungrad Research Center, Bumrungrad International Hospital, Bangkok, Thailand
Background: Crohn's disease (CD) has been relatively rare in Asian region, whereas its clinical outcomes have been dominated by evidence from Caucasians in developed countries. This study was aimed to report clinical characteristics and outcomes of 287 multiethnic patients who visited our institution. Methods: We reviewed medical records of all patients who visited Bumrungrad International Digestive Disease Center (BIDDC) during 2005–2010. Colonoscopy and sigmoidoscopy were performed in compliance with the ASGE guidelines. Results: Of 262,606 individuals, 287 CD patients were followed up for 5.65 years on average. Forty-two percent were Middle Eastern, followed by Caucasian (30%) and Asian (29%). Middle Eastern and Caucasian had higher CD prevalence than Asian (286.71, 278.66, and 43.10 per 100 000 population, respectively). Significant variation in male proportion was observed (P = 0.001), ranging from 39% (Asian) to 68.24% (Caucasian). The overall mean age was 39.46 years with significant variation across ethnic origins (P < 0.001), ranging from 33 (Middle East) to 45 (Caucasian). Middle Eastern had a longer duration of symptoms (26.55 months) than Caucasian (11.98 months) and Asian (12.35 months) (P = 0.0008). The proportions of perianal lesions were statistically different across ethnic origins (P = 0.014): 9.76% (Asian), 24.17% (Middle Eastern), and 12.94% (Caucasian). Fifteen out of 85 Caucasian patients were severely active, compared with Middle Eastern (10.83%), and Asian (6.10%). Disease progression existed in 88 of 254 patients who initially had non-severe pathology, which significantly varied across ethnic groups, ranging from 20% (Middle Eastern) to 51% (Asian) (P < 0.0001). Clinical improvement was observed in 82% of the patients. However, 75 patients required either surgery or hospitalization with significant ethnic variation (37.65% of Caucasian, 28.33% of Middle Eastern, and 10.98% of Asian; P < 0.0001). Conclusions: Crohn's disease prevalence, gender, age, duration of symptoms, perianal lesion, pathological severity, and disease progression varied across ethnic origins.
# P-0132
Prognostic factors of the clinical outcome for patients with gastroenteropancreatic neuroendocrine tumors
Pao-Yuan Huang1, Ming-Luen Hu1, Chih-Ming Liang1, Wei-Chen Tai1,2, Keng-Liang Wu1,2, Yi-Chun Chiu1,2 and Seng-Kee Chuah1,2
1Division of Hepatogastroenterology, Department of Internal Medicine, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan; 2Chang Gung University, College of Medicine, Kaohsiung, Taiwan
Introduction: There is an increasing trend in the incidence of gastroenteropancreatic neuroendocrine tumors (GEP-NETs) in the world. The aim of this study was to identify the prognostic factors for the survival of patients with GEP-NETs. Materials and Methods: A cross-sectional, retrospective chart review study was conducted on patients with pathologically proven GEP-NETs between the periods of January 2003 to December 2016 at Kaohsiung Chung-Gung memorial hospital. Results: A total 97 patients who met the criteria were studied (male/female = 54/41, age: 57.7 ± 15.4 years). The presentation, clinical characteristics, and disease outcome were reviewed and analyzed. The most frequent primary site of the GEP-NETs was the rectum (48%), followed by pancreas (17%), duodenum (11%), stomach (10%), colon (6%), and appendix (5%), and most of them were hormonally nonfunctional (94.8%). There were 56 tumors classified as NET G1, 9 as NET G2, and 14 as G3. Distant metastasis was found in 13 patients (13%). Curative treatments such as surgery or endoscopic resection were performed in 83.5% of patients (n = 81). The mean overall survival was 107.2 ± 7.8 months. The estimated 3- and 5-year overall survival rates for all patients were 84% and 82%, respectively. Logistic regression analysis showed that metastasis, initial palliative treatment, and higher histopathological grading were associated with poor survival outcome. Conclusions: The prognostic factors affecting the survival of patients with GEP-NETs are the presence of metastases at diagnosis, initial palliative treatment, and high histopathological grade. Keywords: Gastroenteropancreatic neuroendocrine tumors; clinical outcome; prognostic factors
# P-0137
Incidence of breast cancer among patients with colorectal cancer in women: A nationwide cohort study in Korea
Dong Woo Shin1, Yoon Jin Choi1, Dong Ho Lee1,2, Hyun Soo Kim1 and Kyung-Do Han3
1Department of Internal Medicine and Seoul National University Bundang Hospital, Seongnam, Gyeonggi-do, South Korea; 2Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, South Korea; 3Department of Biostatistics, College of Medicine, The Catholic University of Korea, Seoul, South Korea
Background/Aims: As life expectancy is prolonged and the treatment of cancer develops, secondary primary tumors have become a major issue. Colorectal cancer patients are known to be particularly vulnerable to the development of new types of cancer. This study aims to understand incidence rates of breast cancer, which is often found in female patients with colorectal cancer during the follow-up period. Methods: This study used a population-based retrospective cohorts, those registered with colorectal cancer code (ICD-10 code C18, C19, and C20) in the National Health Insurance Corporation between 2007 and 2015. We analysed the hazard ratios of breast cancer on 56 682 patients with colorectal cancer and 288 119 age- and gender- matched controls without colorectal cancer. Patients were followed up until breast cancer was developed and relevant diagnostic code (ICD-10 code C50) was given. Cox proportional models were used to estimate the relative hazard ratios. Results: The mean follow-up period was 4.4 years in the colorectal cancer group and 4.5 years in the general population. Breast cancer was developed in 382 out of 56 682 (0.67%) patients with colon cancer and 1053 out of 288 119 (0.37%) in the general population. The incidence of breast cancer was higher in the colorectal cancer cohort than in the general population (Hazard ratio [HR] 2.02, 95% confidence interval [CI] = 1.58–2.58). After adjusting for sex, age, smoking, drinking, exercise, and comorbidities (diabetes mellitus, hypertension, and hyperlipidemia), patients with colorectal cancer also had an increased risk of breast cancer (HR 1.98, 95% CI = 1.55–2.53) compared with those without colorectal cancer. Conclusion: This study shows that women who have been diagnosed with colorectal cancer have a higher chance of also being diagnosed with breast cancer within five years. For women diagnosed with colorectal cancer, screening tests such as breast ultrasound and mammography should be performed more intensively.
# P-0140
A prospective assessment of bowel habit in patients with non-constipated irritable bowel syndrome
Ji Young Lee, Oh Young Lee, Byung Chul Yoon, Ho Soon Choi, Hang Lak Lee and Kang Nyeong Lee
Departments of Internal Medicine, Hanyang University Hospital
Background and Aims: The prevalence of irritable bowel syndrome (IBS) varies according to geographically based populations, sex, age, and socioeconomic status. Many studies have reported the prevalence of IBS, but the effects of socioeconomic status and quality of life have not been well described. And there is no long-term follow-up study for IBS and alternating IBS in Korea. Therefore, we conducted to determine different characteristics of IBS subtype and factors influencing the IBS subtype. Methods: A prospective study, using a reliable and valid questionnaire based on the fulfillment of the Rome III criteria and EuroQol five dimensions (EQ-5D) questionnaire was performed. The patients with physician-diagnosed IBS symptoms fill out the questionnaire at baseline, 3-, 6-, and 12-month follow-up period. Algorithms to classify subjects into IBS-D, IBS-C, and IBS-U groups used questionnaire information and modified Rome III definitions. Results: Among 39 non-constipated IBS patients, there were no differences between groups except for stool frequency. The proportion of patients in each subgroup remained the same over the year is 20.51%, and most patient changed to either of the other 2 subtypes at least once. There were no differences in age, sex, BMI, and EQ-5D score between groups that stayed the same subtypes and changed the subtypes. Conclusions: In our study, non-constipated IBS patients commonly transition between subtypes, and there were no influencing factor that change subtypes. We questioned the meaning of existing classification of IBS subtypes using Rome III criteria, and further studies will be needed to support our opinion.
# P-0157
Characterization of intestinal epithelial response to endocytosed bacteria: Implication in tumorigenesis
Linda Chia-Hui Yu1, Shu-Chen Wei2 and Yen-Hsuan Ni3
1Graduate Institute of Physiology, National Taiwan University College of Medicine; 2Department of Internal Medicine, National Taiwan University Hospital; 3Department of Pediatrics, National Taiwan University Hospital, Taipei, Taiwan
Colorectal cancer (CRC) is the second leading cause of cancer mortality, of which patients with inflammatory bowel disease showed higher risk. Adherent-invasive Escherichia coli strain LF8[2] is associated with intestinal lesions in Crohn's disease and has been implicated in promoting inflammation and tumorigenesis through macrophage activation. However, it remains unclear whether endocytosed bacteria induce epithelial proliferation and/or death. Aim: To characterize the epithelial response to endocytosed bacteria in mouse CRC models and human epithelial cell lines. Methods: Mice were subjected to CRC induction by three cycles of azoxymethane (AOM)/dextran sodium sulfate (DSS) or to colitis by DSS. In some groups, antibiotics were administered to AOM/DSS mice. Bacterial colonies isolated from colonocytes were quantified and sequenced for 16S rDNA. Human Caco-[2]BBe cells were apically exposed to bacteria to examine intracellular bacterial counts by a gentamycin resistance assay. Epithelial proliferation was measured by cell counting and cell cycle by flow cytometry. Cell death was measured by DNA fragmentation and lactodehydrogenase assay. Results: Antibiotics treatment decreased bacterial endocytosis by colonocytes and reduced tumor burden in AOM/DSS mice, suggesting a role of bacteria in tumorigenesis. Enterobacteriaceae family became the dominant fecal bacteria in antibiotics-treated mice, and its abundance was positively correlated with tumor burden. Increased virulence factors, e.g., fimA/C/H and htrA, were found in fecal bacteria. The endocytosed bacterial strains in colonocytes of AOM/DSS and DSS mice included Escherichia, Enterobacter, Enterococcus, and Staphylococcus. By in vitro co-culturing with Caco-[2] cells, higher levels of bacterial internalization were noted by mouse E. coli and human LF8[2], compared with the other strains. Mouse E. coli and human LF8[2] promoted proliferation and apoptosis in Caco-[2] cells. Conclusions: Antibiotic treatment reduced colon tumorigenesis, which may be partly due to the reduction of bacterial endocytosis. Internalized E. coli in colonocytes may play an important role in promoting cell proliferation during colon cancer development. Keywords: colorectal cancer, intestinal microbiota, antibiotics, bacterial internalization, cell proliferation
# P-0160
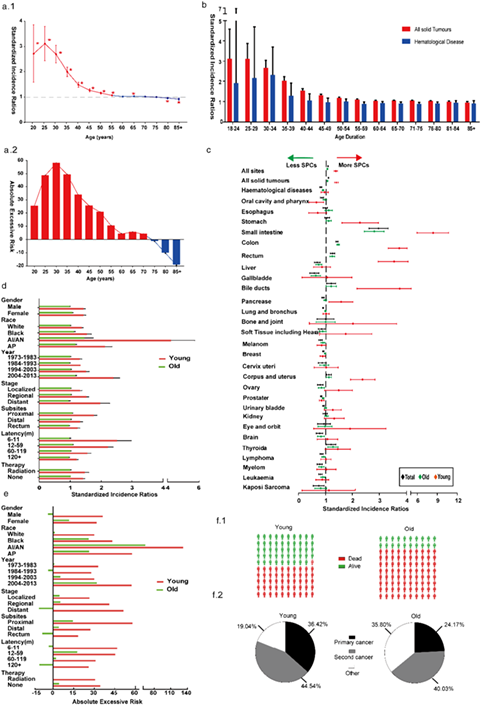
Excess risk of second primary cancers in young-onset colorectal cancer survivors
Xingkang He1, Wenrui Wu2, Yue Ding1, Lei-Min Sun1 and Jianmin Si1
1Department of Gastroenterology, Sir Run Run Shaw Hospital; 2The First Affiliated Hospital, Zhejiang University, Hangzhou, China
# P-0178
Cost-effectiveness of hospital charge for colonic diverticular bleeding depended on management of repeated bleeding and blood transfusion: Analysis with diagnosis procedure combination (DPC) data in Japan
Yoichiro Ito1, Yasuhisa Sakata1, Hisako Yoshida2, Sayuri Nonaka3, Susumu Fujii3, Yuichiro Tanaka1, Shimpei Shirai1, Eri Takeshita1, Takashi Akutagawa1, Hiroharu Kawakubo1, Koji Yamamoto1, Nanae Tsuruoka1, Ryo Shimoda1, Ryuichi Iwakiri1 and Kazuma Fujimoto1
1Department of Internal Medicine and Gastrointestinal Endoscopy; 2Clinical Research Center; 3Medical Information Center, Saga Medical School, Saga, Japan
Background: Bleeding from a colonic diverticulum is sometimes serious for aged patients. The aim of this study was to determine the risk factors for high-cost medical treatment of colonic diverticular bleeding using the diagnosis procedure combination (DPC) data. Methods: From January 2009 to December 2015, 78 inpatients with colonic diverticular bleeding were retrospectively identified by DPC data in Saga Medical School Hospital. All the patients underwent colonic endoscopy within 3 days. The patients were divided into two groups: the low-cost group (DPC cost of < 500 000 yen) and the high-cost group (DPC cost of > 500 000 yen). Results: Univariate analysis revealed that aging, hypertension, rebleeding, a low hemoglobin concentration at admission, and blood transfusion were risk factors for high hospitalization cost. Multivariate analysis revealed that rebleeding (odds ratio, 5.3; 95% confidence interval, 1.3–21.3; P = 0.017) and blood transfusion (odds ratio, 3.8; 95% confidence interval, 1.01–14.2; P = 0.048) were definite risk factors for high hospitalization cost. Conclusion: Rebleeding and blood transfusion were related to high hospitalization cost for colonic diverticular bleeding, suggesting that therapeutic and/or prophylactic treatment with emergency endoscopic hemostasis might be critical for cost-effectiveness.
# P-0185
A comparison of sigmoidoscopy-based screening strategies in their capability to predict proximal neoplasia in asymptomatic Chinese population
Jason Liwen Huang1, Ping Chen2, Xiaoqin Yuan2, Yunlin Wu2, Miaoyin Liang1, Yuan Fang1, Harry Haoxiang Wang3,4 and Martin Chisang Wong1,5,6
1JC School of Public Health and Primary Care, Faculty of Medicine, Chinese University of Hong Kong(CUHK), Hong Kong, SAR, China; 2Ruijin Hospital North, Shanghai Jiaotong University, Shanghai, 201801, China; 3School of Public Health, Sun Yat-Sen University, Guangzhou, 510080, Guangdong, China; 4General Practice and Primary Care, Institute of Health and Wellbeing, University of Glasgow, Glasgow, G12 9LX, UK; 5Institute of Digestive Disease, Faculty of Medicine, CUHK, HKSAR, China; 6State Key Laboratory of Digestive Disease, Faculty of Medicine, CUHK, HKSAR, China
Background/Aims: The criteria for colonoscopy referral represent a key determinant of the efficiency and effectiveness of colorectal cancer screening programs based on flexible sigmoidoscopy (FS). This study aims to compare the performance of four major published scores to detect proximal neoplasia (PN) and advanced proximal neoplasia (APN) in an asymptomatic Chinese cohort. Methods: In 2013–15, asymptomatic individuals aged 50–75 years were recruited in a large hospital-based endoscopy unit in Shanghai, China. The performance of four existing scores in predicting PN and APN was evaluated by simulating colonoscopy, including (1) the UK flexible sigmoidoscopy; (2) Screening for COlon REctum (SCORE); (3) NORwegian Colorectal Cancer Prevention (NORCCAP) trials, and (4) Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial. The sensitivity, specificity, the number of subjects needed to screen (NNS), and the number of subjects needed to refer (NNR) for colonoscopy to detect one APN/PN were assessed. The area under the receiver operating characteristic curve (ROC) was also estimated. Results: Among 5833 eligible cases, 749 had PN (12.8%), including 151 APN (2.6%). The PLCO criteria obtained the highest sensitivity to detect PN (49%) and APN (66%), while the UK criteria achieved the highest specificity (93%) for both PN and APN. The lowest NNS was required by the PLCO criteria for PN (16 vs 19–38) and APN (58 vs 69–86), and the UK criteria required the lowest NNR to detect PN (3.2 vs 4.0–4.8) and APN (7 vs 10–16). The AUROC of all the four criteria was 0.57–0.61 for PN and 0.68–0.70 for APN (Table 1). Conclusions: For PN/APN, the PLCO criteria had the highest sensitivity and lowest NNS, while the UK criteria had the highest specificity and the lowest NNR. The limited performance of all the four existing criteria implies the need for further studies based on Chinese cohorts.
| Category | PLCO criteria | NORCCAP criteria | SCORE criteria | UK criteria | |
|---|---|---|---|---|---|
|
PN n = 749 (12.8%) |
Se(95%CI) | 0.49(0.45,0.53) | 0.40(0.37,0.44) | 0.25(0.22,0.28) | 0.20(0.18,0.23) |
| Sp(95%CI) | 0.73(0.71,0.74) | 0.82(0.81,0.83) | 0.89(0.88,0.90) | 0.93(0.93,0.94) | |
| NNS(95%CI) | 16(14,18) | 19(17,21) | 32(28,36) | 38(33,45) | |
| NNR(95%CI) | 4.8(4.4,5.2) | 4.0(3.6,4.4) | 4.0(3.5,4.5) | 3.2(2.8,3.6) | |
| ROC(95%CI) | 0.61(0.59,0.63) | 0.61(0.59,0.64) | 0.57(0.55,0.59) | 0.57(0.55,0.59) | |
|
APN n = 151 (2.6%) |
Se(95%CI) | 0.66(0.59,0.74) | 0.56(0.48,0.64) | 0.47(0.40,0.56) | 0.45(0.37,0.53) |
| Sp(95%CI) | 0.74(0.73,0.75) | 0.80(0.79,0.81) | 0.88(0.87,0.89) | 0.93(0.92,0.93) | |
| NNS(95%CI) | 58(48,71) | 69(56,85) | 81(64,102) | 86(68,109) | |
| NNR(95%CI) | 16(13,19) | 14(12,18) | 10(8,13) | 7(6,9) | |
| ROC(95%CI) | 0.70(0.66,0.74) | 0.68(0.63,0.73) | 0.68(0.63,0.73) | 0.69(0.64,0.74) |
- APN, advanced proximal neoplasia; CI, confidence interval; NNR, number need to refer; NNS, number need to screen; PN, proximal neoplasia; ROC, area under the receiver operating characteristic curve; Se, sensitivity; Sp, specificity.
# P-0192
Fecal calprotectin versus fecal immunochemical test for the prediction of mucosal healing and endoscopic activity in ulcerative colitis
Hyung Wook Kim, Dae Hwan Kang, Cheol Woong Choi, Su Jin Kim, Hyeong Seok Nam, Dae Gon Ryu, Ji Hwan Go and Il Eok Jo
Department of Internal Medicine, Pusan National University School of Medicine, Pusan National University Yangsan Hospital, Korea
Background: Mucosal healing (MH) has been suggested as a therapeutic goal for ulcerative colitis (UC). Fecal calprotectin (Fcal) and fecal immunochemical test (FIT) are known to be a useful predictor of MH and endoscopic activity in UC. The aim of this study was to compare the superiority of the two tests in the prediction of MH and endoscopic activity in UC. Methods: A total of 57 results, obtained in simultaneous examination with endoscopy and two tests, were retrospectively evaluated for 48 patients with UC. The efficacy of two tests for evaluation of MH and disease activity was compared with endoscopic findings. Endoscopic activity were assessed using the Mayo endoscopic subscore (MES) classification. Negative cut-off valve in two tests was defined as follows: Fcal ≤ 140 ug/g, FIT ≤ 100 ng/mL. Results: Both Fcal and FIT results were significantly correlated with endoscopic activity (r = 0.678 and 0.75). In the prediction of mucosal healing (MES = 0, 1), both tests showed similar usefulness (negative Fcal vs positive Fcal (OR = 23.6, P < 0.001), negative FIT versus positive FIT (OR = 16.0, P < 0.001)). But Fcal showed only usefulness (negative Fcal vs positive Fcal (OR = 11.3 P < 0.001), negative FIT versus positive FIT (OR = 5.8, P = 0.076)) in complete mucosal healing (MES = 0). And the sensitivity, specificity, and predictive values of the combination did not largely surpass those values of Fcal alone. Conclusions: Both Fcal and FIT were well correlated with endoscopic activity in UC. However, Fcal was more effective than FIT in predicting complete MH.
# P-0193
Polyp missing rate and its associated risk factors of referring hospital for endoscopic resection of advanced colorectal neoplasia in Korea
Hyung Wook Kim, Dae Hwan Kang, Cheol Woong Choi, Su Jin Kim, Hyeong Seok Nam, Dae Gon Ryu, Yong Jae Lee and Byung Jin Kwon
Department of Internal Medicine, Pusan National University School of Medicine, Pusan National University Yangsan Hospital, Korea
Background and Aims: Missed polyps are frequently observed in surveillance colonoscopy or during referral resection. We evaluated the polyp missing rate and its associated risk factors in patients who were referred to a tertiary hospital for endoscopic resection of advanced colorectal neoplasia. Methods: A total of 388 patients with advanced neoplasia who underwent colonoscopy in their referring hospital and only endoscopic resection without total-colonoscopy in Pusan National University Yangsan Hospital (PNUYH) from 2009 to 2014 and who underwent surveillance colonoscopy within 6 to 12 months were retrospectively analyzed. Results: The missing rate for polyps, adenomas, and advanced neoplasia were 52.6% (204 cases), 41.5% (161 cases), and 5.7% (22 cases), respectively. The advanced neoplasia in surveillance colonoscopy comprised the following: ≥ 1 cm lesions (11 cases, 50%), high-grade dysplasia (4 cases, 18.2%), villous adenoma (4 cases, 18.2%), and invasive cancer (3 cases, 13.6%). Risk factors for missed adenomas in multivariate analysis were ≥ 60 years (P = 0.004), male sex (P < 0.001), and no usage of the cap in index colonoscopy (P = 0.015). Missed polyps/adenomas were most frequent in the ascending colon (P < 0.001). Conclusions: The missing rate for polyps and adenomas of referring hospital was higher than expected. Especially, patients with old age or male or no usage of the cap on initial colonoscopy were at increased risk of missed adenoma. Careful total colonoscopy during referral resection or early surveillance colonoscopy is mandatory in these patients.
# P-0198
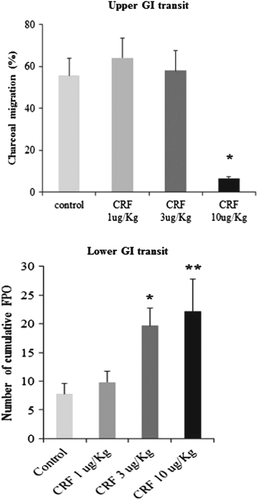
The effect of peripheral CRF peptide and water avoidance stress on colonic and gastric transit in guinea pig
Zahid Hussain, Hae Won Kim, Cheal Wung Huh, Young Ju Lee and Hyojin Park
Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
Background: Functional dyspepsia (FD) and irritable bowel syndrome (IBS) are common gastrointestinal diseases, often patients with one of these diseases commonly overlap. Emerging evidence links the activation of corticotropin releasing factor (CRF) receptors with stress-related alterations of gastric and colonic motor function. Therefore, we investigated the effect of peripheral CRF peptide and water avoidance stress on upper and lower GI transit in guinea pig. Methods: Different doses (1, 3, and 10 μg/kg) of CRF were injected intraperitoneal in fasted guinea pigs 30 minutes prior to the intragastric administration of charcoal mix, and upper GI transit was measured. Colonic transits of non-fasted guinea pigs were indirectly assessed after injection of various doses of CRF. The guinea pigs were subjected to water-avoidance stress, and gastrocolonic transits were recorded in different sets of experiments. Results: CRF (10 μg/kg) significantly inhibited upper GI transit compared to control (Fig. 1). In contrast, colonic transit demonstrated significant acceleration of cumulative fecal pellet output at 3 and10 μg/kg dose of CRF compared with control (Fig. 1). Next, the effect of CRF antagonist (astressin) was tested on this model. Remarkably, astressin pretreated guinea pigs significantly reverses the effect of CRF peptide on gastrocolonic transit. However, water avoidance stress (WAS) accelerated lower GI transit significantly, while gastric transit remains unaffected compared to control. Conclusion: Peripheral CRF significantly suppress gastric transit and accelerate colonic motility, whereas central CRF involved WAS stimulated only colonic transit. Therefore, peripheral CRF could be utilized to establish the animal model of overlap syndrome.
# P-0209
Lipocalin 2 down-regulates cell proliferation and EMT through reprograming of glucose metabolism in colorectal cancer
Sang Wook Kim
Department of Internal Medicine, Chonbuk National University Medical School
Lipocalin 2 (LCN2) is a member of the lipocalin superfamily, and it has an important role in the oncogenesis and cancer progression in various type of cancer. However, the expression pattern and functional role of LCN2 in colorectal cancer (CRC) is still poorly understood. The purpose of this study was to investigate whether LCN2 is associated with proliferation and epithelial-mesenchymal transition (EMT) in CRC and to elucidate the underlying signaling pathway. LCN2 was preferentially expressed in CRC than in normal tissues. However, the expression in CRC from metastatic or advanced-stage group was significantly lower than in CRC from non-metastatic or early-stage group. Knockdown of LCN2 using small interfering RNA (siRNA) in CRC cells expressing high level of LCN2 induced of cell proliferation and morphological switch from epithelial to mesenchymal state. Furthermore, down-regulation of LCN2 in CRC cells increased cell migration and invasion involved in the regulation of EMT markers. Knockdown of LCN2 also induced glucose consumption and lactate production, accompanied by increase in energy metabolism related proteins. Taken together, our findings indicated that LCN2 can negatively modulate the proliferation, EMT, and energy metabolism in CRC cells. Thus, Lcn2 may be a candidate metastasis suppressor and a potential therapeutic target in CRC.
# P-0210
MicroRNA-30a suppresses cell motility and EMT by direct targeting oncogenic TM4SF1 in colorectal cancer
Young Ran Park, Se Lim Kim, Hee Chan Yang, Sung Kyun Yim, Soo Teik Lee and Sang-Wook Kim
Department of Internal Medicine, Chonbuk National University Medical School, Jeonju, Republic of Korea
Colorectal cancer (CRC) is one of the leading causes of cancer death worldwide, with many oncogenes and tumor suppressor genes composed. MicroRNAs (miRNAs) are small non-coding RNA that can negatively regulate gene expression. Previous evidences have revealed that miRNAs regulate the process and development of many cancers. Here, we investigated the role of miR-30a in CRC and its unknown mechanism. Through qRT-PCR, we found that miR-30a was down-regulated in CRC tumor tissues and cell lines and that miR-30a was significantly associated with T stage and lymph node metastasis compared with adjacent normal tissues. We also confirmed that miR-30a decreased migration and invasion in CRC cell lines that transmembrane4-L-six-family protein (TM4SF1) gene was the direct target of miR-30a through luciferase reporter assay. More importantly, miR-30a overexpression regulated was not only a down-regulation of TM4SF1 mRNA and protein expression but also an inhibition of VEGF and enhance of E-cadherin. We also detected that TM4SF1 was up-regulated in CRC tumor specimens and that TM4SF1 was significantly associated with advance stage and lymph node compared with CRC adjacent normal tissues. The miR-30a levels and negatively correlated with the TM4SF1 mRNA level in CRC specimens. Our finding is that miR-30a is an important regulator of TM4SF1, VEGF, and E-cadherin for CRC metastasis, and its pathway was a potentially new approach in the metastasis and therapeutic treatment for CRC. Keywords: miR-30a, colorectal cancer, transmembrane4-L-six-family protein 1, metastasis
# P-0214
Safety and efficacy of cold polypectomy for small colorectal polyps in patients taking antithrombotic therapies
Ken Umemura, Fumiko Shimoda, Yu Tanaka, Keiichiro Hiramoto, Osamu Kimura, Sho Asonuma and Akihiko Satoh
Department of Gastroenterology, South Miyagi Medical Center, Ohgawara, Japan
Background: Cold polypectomy has accepted as a preferred technique for removal of diminutive colorectal polyps by its superior safety with a decreased risk of electrocautery-related complications. However, there are not many studies so far concerning the safety of the procedure in high-risk patients of bleeding. The aim of the present study was to evaluate the safety and efficacy of cold polypectomy for small polyps in patients taking antithrombotic agents. Methods: We conducted a retrospective observational study. Patients who were performed cold polypectomy for colorectal polyps less than 10 mm in size at our hospital between July 2014 and August 2016 were included. Patients' characteristics, antithrombotic agents, adverse events (immediate and/or delayed bleeding and perforation) and length of hospitalization were documented from a hospital database. Delayed bleeding was defined as bleeding that required endoscopic treatment within two weeks after polypectomy. Results: A total of 477 patients (female 122, mean age 66.8 y.o.) having 1094 eligible polyps were enrolled; 84 patients (201 polyps) taking antithrombotic agents (antithrombotic group) and the other without antithrombotic agents (non-antithrombotic group). The antithrombotic therapies included antiplatelet agents in 59 cases, anticoagulants in 22 cases, and the combination of those in 3 cases. The polypectomy specimens were adequate for histopathological assessment in all cases, and the rate of completed resection was 98.5% (1078/1094). Bleeding following the polypectomy was observed in 4 patients (0.8%); 1.2% (1/84) in the antithrombotic group, and 0.8% (3/393) in the non-antithrombotic group (P = 0.70). No perforation related to cold polypectomy occurred. The mean hospitalization was 2.2 days (2–13); 2.8 days (2–13) in the antithrombotic agents group; and 2.1 days (2–11) in the non-antithrombotic group, respectively. Conclusion: These results demonstrate that cold polypectomy is a safe and effective technique for removal of small polyps less than 10 mm even in patients taking antithrombotic therapies. Keywords: antithrombiotic agents, cold polypectomy, colorectal polyps
# P-0216
Utility of serial C-reactive protein measurements in patients treated for suspected abdominal tuberculosis
Vishal Sharma, Harshal S Mandavdhare, Sandeep Lamoria, Amit Kumar, Ravi Sharma and Surinder S Rana
Department of Gastroenterology, Postgraduate Institute Of Medical Education And Research, India
Introduction: Utility of inflammatory markers in follow-up of patients of abdominal tuberculosis is uncertain. Methods: We did a retrospective analysis of collected database of patients who received antitubercular therapy (ATT) for suspected diagnosis of abdominal tuberculosis (peritoneal or intestinal). The patients were labelled to have confirmed (caseating granulomas or acid fast bacilli positivity on smear or culture) or probable tuberculosis (elevated ascitic adenosine deaminase or granuloma without caseation or histological findings consistent with tuberculosis). Patients were followed up clinically for symptomatic improvement and objectively for resolution of ascites and/or ulcer healing. Serum C-reactive protein was measured at diagnosis and at 2 and 6 months of treatment. Results: Of a total of 122 patients, 10 had incomplete records. Of the rest 112 patients (61 males, mean age: 36.34 ± 14.76 years), 25 had confirmed, while 87 had probable tuberculosis. Sixty-six patients received ATT for intestinal, 28 for peritoneal, and 18 for combined involvement. Eleven patients had normal CRP at baseline; 9 improved on follow-up (8 intestinal, one combined), while 2 had alternative diagnosis (Crohn's disease: 1 and NSAID enteropathy: 1). Of the 101 patients with elevated CRP, the CRP declined in 93 patients and all had tuberculosis. Of the eight patients with plateaued or rising levels, 2 had confirmed, and 6 probable TB. Causes of lack of decline were resistant TB (1), inter-current infection (1), alternative diagnosis (lymphoma: 1, peritoneal carcinomatosis: 1, and Crohn's disease: 3). The cause of lack of improvement in CRP was not clear in one patient. Conclusion: Declining CRP levels correlated with mucosal healing or ascites resolution in abdominal tuberculosis. Lack of decline in CRP levels in patients receiving ATT should raise the suspicion of alternative diagnosis or resistant tuberculosis.
# P-0240
The right ingredients for a superior bowel preparation: A retrospective on inpatient bowel preparation in Singapore
Zhen Xi Joel Lee1, Weilin Xie1, Sasha Thrumurthy1, Cai Sheng Joseph Wong2, Kim San Lim2, Jing Zhi Ong2 and Kuo Chao Yew1
1Department of Gastroenterology & Hepatology, Tan Tock Seng Hospital, Singapore; 2Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Background/Aim: Factors contributing to bowel preparation outcome can be divided into patient as well as regimen administration factors. Studies have demonstrated contributing factors such as gender, diabetes, stroke disease, regimen compliance, and the timing of scope following regimen administration. We performed a retrospective analysis on inpatient bowel preparation in our hospital. Case Description (Methods): We included 611 inpatients who underwent colonoscopy in our hospital, from June 2015 to December 2015. Patient demographic, co-morbidity, functional status, bowel preparation regimen, and administration were explored. The Boston Bowel Preparation Scale (BBPS) was used to assess preparation outcome. A score of ≥ 5 for total BBPS and ≥ 2 for each segment of colon were considered adequate bowel preparation. Univariate and multivariate analysis were performed. Case Description (Results): A total of 251 patients were male (41.1%), 360 were female (58.9%), mean age was 68.9 ± 13.9, and BMI was 23.6 ± 4.8. Diabetes was found to be significantly associated with poorer bowel preparation outcome (42% vs 32%, P = 0.014). Male sex is associated with better bowel preparation at transverse and left colonic regions (56.1%, P = 0.03 and 54.7%, P = 0.003 respectively). A poorer bowel preparation outcome was noted in patients requiring regimen administration via nasogastric tube (3.4% vs 0.8%, P = 0.02). Further sub-analysis demonstrated a more morbid baseline such as stroke disease (40% vs 2.5%). Slow bowel preparation beyond 2 days does not seems to result in a better BBPS (19.4% vs 16%, P = 0.323). Amongst patients who consumed the same amount of PEG volume (mean 2 L per day), there is no consistent BBPS outcome, suggesting further confounding factors are present. The same observation was noted with total bowel frequency and duration of fasting. Conclusion: The interaction between patient and administrative factors is consistent with our practical experience where the physician has to weigh up multiple factors before prescribing the bowel preparation regimen. Further exploration into this interaction will be both interesting and important.
# P-0246
Combining fecal calprotectin and fecal Hgb quantification is better than fecal calprotectin for predicting endoscopic disease activity in UC patients
Young Bin Kim, Young Sook Park, Hee Chan Jeong, Dong Shin Kim, Young Kwan Jo and Sang Bong Ahn
Division of Gastroenterology, Department of Internal Medicine, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea
Backgrounds and Aims: Fecal calprotectin, which is an indirect measurement of inflammation with neutrophils in the gut, is known as excellent fecal biomarker that reflects disease activity in UC. But fecal calprotectin level in real-world practice shows variable range in active inflammation state. So we aimed to know that combination of fecal calprotectin and fecal Hgb quantification can predict endoscopic disease activity in UC patients more accurately than single method. Methods: We prospectively enrolled 78 patients with UC who underwent sigmoidoscopy or colonoscopy and calculated FC level and fecal Hgb quantification at Eulji university Eulji hospital from March 2015 to July 2016. Endoscopic disease activity was evaluated by Mayo endosopic scoring (MES). Fecal calprotectin level measured by immunochromatography technique. Fecal Hgb quantification measured by OC-Sensor Diana (EIKEN®), which uses latex agglutination immune-turbidimetry(range 0–1000 ng/mL). Results: Fecal calprotectin levels were increasing with severity of endoscopic inflammation and were well correlated by MES score (R = 0.351, P-value = 0.001). Fecal Hgb quantification also shows correlation with endoscopic disease activity (R = 0.563, P-value = 3.18 × 10−7). Fecal calprotectin shows correlation with fecal Hgb quantification (R = 0.49, P-value = 1.20× 10−5). Combining fecal calprotectin and fecal Hgb quantification shows more accurate predictor for endoscopic disease activity (R2 0.49) than fecal calprotectin (P-value 0.008) or fecal Hgb quantification (P value 0.001). Conclusion: Fecal calprotectin level shows correlation with mucosal inflammatory activity in UC patients. But it shows limitation of wide range in same endoscopic score. This study shows combining fecal calprotetin and fecal Hgb quantification can predict endoscopic disease activity better than fecal calprotectin single measure.
# P-0247
Clinical outcomes of rectal neuroendocrine tumor treated by endoscopic resection
Maiko Takita, Ken Ohata and Nobuyuki Matsuhashi
NTT medical center Tokyo
Background: The therapeutic strategies for the rectal neuroendocrine tumor (NET) have not been still established. We conducted this retrospective study to evaluate the clinical outcomes of rectal NET after endoscopic treatment. Methods: Between January 2001 and March 2017, 195 patients with 197 rectal NET(G1) underwent endoscopic treatment in our hospital. Firstly, we investigated association between clinicopathological characteristics including endoscopic findings and therapeutic outcomes. Curative resection was defined as R0 resection without LVI. Subsequently, we investigated the long-term outcomes of the cases. Results: The average age was 52.9 years, and the majority were male (74%). Most of the lesions were located at Rb (83%), and the average diameter was 5.1 mm. Lesions were resected by EMR-C/ESMR-L/ESD: 9/174/14, respectively. Of the 197 lesions, 190 and 117 achieved complete and curative resection, respectively. Multivariate logistic regression analyses revealed that the diameter (OR: 13.7, 95% CI; 1.68–112, P = 0.015) and depression (OR: 4.69, 95% CI; 1.42–15.5, P = 0.011) are significantly associated with non-curative resection. Fourteen of the 80 lesions with non-curative resection underwent additional surgery, among which 4 cases had histological lymph node metastasis. Of the 150 lesions that can be followed for more than 12 months (80 achieved curative resection, 59 were followed without additional surgery, and 11 underwent additional surgery), no case had recurrence during the follow-up period (average 60.2 months, 65.5 months, and 35.3 months). Conclusions: Current rational guideline for endoscopic resection on treatment of rectal NET including 10 mm or less and lack of depression is considered to be appropriate to provide curative resection. However, given that there was no recurrence without additional surgery in cases regarded as non-curative resection, observation without additional surgery might be allowed. To establish curative criteria and indication for endoscopic treatment, further studies are needed.
# P-0255
The gender differences of colorectal tumor in screening colonoscopy
Dong Shin Kim1, Young Sook Park1, Young Kwan Jo1, Hee Chan Jeong1, Young Bin Kim1, Sang Bong Ahn1, Seong Hwan Kim1, Dong Wook Oh1, Byoung Kwan Son1, Jeong Hwan Kim2 and Ji Hye Han2
1Department of Gastroenterology Internal Medicine; 2Department of Health Screening Center, Nowon Eulji Medical Center, Eulji University, Korea
Background and Aim: Recently, colon cancer incidence is rising in Asian countries. Colonoscopic polypectomy of adenoma can reduce cancer incidence. But there is limited data on gender difference in colon tumor. This study aimed to evaluate the gender difference of colorectal tumor in asymptomatic screening colonoscopy. Methods: A Restrospective cross-sectional study was performed by using data from routine health check-up examinations from January 1, 2013 to December 31, 2013 at the Nowon Eulji Medical Center. A total of 938 consecutive participants aged 24 to 75 years undergoing screening colonoscopy were agreed this study. Results: The total number of observed polyps was 1150. There were no significant differences in age, total cholesterol, and LDL level between men and women. But there were significant differences in BMI, triglycerides, HDL, fasting glucose, hemoglobin, and hematocrits. There were no differences in location of adenoma between men and women. Men have a greater risk of having colon tumor (OR = 2.14, 95% CI: 1.71–2.68, P value < 0.001) and having adenoma (odds ratio [OR] = 1.44, 95% CI: 1.16–1.79, P value < 0.001) than women. Also, male sex (OR = 1.45, 95% CI: 1.24–1.58, P value < 0.001) was independent predictor of advanced histological type such as high-grade dysplasia or cancer. Conclusions: This study shows that men shows has higher incidence of colon adenoma and cancer than female at the same age. Also, male sex has higher risk of more advanced histology type of tumor than female.
# P-0257
Cost-benefit analysis of heparin bridging therapy for colorectal EMR in Japan
Shiro Hayashi, Tsutomu Nishida, Ryo Tomita, Yu Higaki, Hiromi Shimakoshi, Akiyoshi Shimoda, Naoto Osugi, Aya Sugimoto, Kei Takahashi, Dai Nakamatsu, Kaori Mukai, Tokuhiro Matsubara, Masashi Yamamoto, Koji Fukui and Masami Inada
Department of Gastroenterology and Hepatology, Toyonaka Municipal Hospital, Osaka, Japan
Background: The guidelines recommend heparin bridging (HB) for patients at high risk for thrombosis during endoscopic mucosal resection (EMR). HB is supposed to increase the risk of bleeding that consequently results in longer hospital stay or higher healthcare cost while preventing thromboembolism. The aim of the present study was to compare cost-benefit and bleeding events between HB and without HB. Methods: This is a retrospective single center cohort study of consecutive patients that underwent HB with colorectal EMR at our institution between March 2015 and April 2016. A total of 59 patients were enrolled. We studied the rate of post-EMR bleeding, the days of hospital stay, and healthcare cost of hospital stay for EMR under HB based on the database of the diagnosis procedure combination (DPC)-based payment system in Japan. We also studied them according to the type of anticoagulant agents (warfarin and direct oral anticoagulant: DOAC). Results: Among 59 patients underwent HR [64% men; mean age, 71 ± 11 years], 30 patients (51%) were taking warfarin and 29 patients (49%) were taking DOAC. Post-EMR bleeding required endoscopic hemostasis occurred in 6 patients (10%). The mean hospital days were 9.5 (3–34) days. Mean cost was 324 343 ±176 210 yen (2975 ± 1616 dollar); on the other hand, the control cost was 148 746 yen (1365 dollar). According to type of anticoagulants, warfarin and DOAC, post-EMR bleeding was 6.9% and 13% (P = 0.42), the mean hospital days was 13.4 versus 5.3 (P < 0.0001), and mean cost was 445 910 versus 198 301 yen (4091 vs 1819 dollar, P < 0.0001), respectively. Conclusion: Colorectal EMR under HB had 10% of post-EMR bleeding. It costed more than double and took 3 times longer hospital stay comparing standard EMR without HB. Among patients under HB, warfarin tended to lower post-EMR bleeding but higher cost due to longer hospital than DOAC.
# P-0260
Assessment of frequency and severity of constipation and its impact on quality of life in Indian patients with functional constipation and constipation-predominant irritable bowel syndrome
Ramesh Rooprai1, Naresh Bhat2, Rajesh Sainani3, Mayur Mayabhate4 and Rashmi Hegde4
1Rai Specialty Care Centre, Jaipur, India; 2Columbia Asia Hospital, Bengaluru, India; 3Sainani Medicare Clinic, Mumbai, India; 4Abbott India Limited, Mumbai, India
Background: Functional constipation (FC) and irritable bowel syndrome (IBS) are among the most common functional gastrointestinal disorders globally. Though low quality of life (QoL) has been reported in FC and IBS-constipation (IBS-C) patients, irrespective of their culture/nationality, no much data is available on the subgroup comparison in Indian milieu. Hence, the present analysis was conducted to compare frequency and severity of constipation and its impact on QoL in Indian patients with FC and IBS-C. Methods: Patients (≥ 18 years) satisfying Rome-III criteria for FC and IBS-C were enrolled in this prospective, multicentric, clinico-epidemiological study. Their demographics, severity of constipation (constipation scoring system [CSS]), constipation-related symptoms (patient assessment of constipation symptoms [PAC-SYM]), and quality of life (PAC-QoL) were assessed. Results: Out of 925 enrolled patients, 75.6% were diagnosed with FC against 24.4% with IBS-C (P < 0.0001). Mean age of study population was 43.8 ± 16.3 years (men: 65.5%; women: 34.5%). PAC-SYM (FC: 27.1 ± 6; IBS-C: 30.1 ± 4.9; P < 0.0001) and CSS scores (FC: 8.4 ± 3.1; IBS-C: 11.2 ± 3; P < 0.0001) were significantly higher in IBS-C versus FC patients, leading to poor QoL (PAC-QoL score: FC: 38.1 ± 16.8; IBS-C: 42.2 ± 13.6; P = 0.0002). Conclusion: Although this study highlights high prevalence of FC than IBS-C in India, frequency and severity of constipation seems to be higher in IBS-C patients than FC, leading to poor QoL. This emphasizes the need to consider IBS-C as an important clinical entity similar to FC and to be managed in a holistic way.
| Parameters* | FC (n = 699) | IBS-C (n = 226) | P-value |
|---|---|---|---|
| Have you felt bloated to the point of bursting? | 1.4 ± 1.2 | 1.6 ± 1.1 | a0.0021 |
| Have you felt heavy because of your constipation? | 2.0 ± 1.1 | 2.1 ± 1.0 | 0.0519 |
| Have you felt any physical discomfort? | 1.6 ± 1.1 | 1.9 ± 1.0 | a< 0.0001 |
| Have you felt the need to open your bowel but not been able to? | 1.6 ± 1.2 | 1.8 ± 1.1 | a0.0120 |
| Have you been embarrassed to be with other people? | 0.9 ± 1.1 | 1.2 ± 1.0 | a0.0021 |
| Have you been eating less and less because of not being able to have bowel movements? | 1.5 ± 1.2 | 1.7 ± 1.2 | a0.0310 |
| Have you had to be careful about what you eat? | 1.4 ± 1.2 | 1.6 ± 1.2 | 0.1927 |
| Have you had a decreased appetite? | 1.4 ± 1.2 | 1.5 ± 1.3 | 0.6799 |
| Have you been worried about not being able to choose what you eat (for example, at a friend's)? | 1.0 ± 1.1 | 1.2 ± 1.1 | 0.0916 |
| Have you been embarrassed about staying in the toilet for so long when you were away from home? | 1.0 ± 1.0 | 1.1 ± 1.1 | 0.1673 |
| Have you been embarrassed about having to go to the toilet so often when you were away from home? | 1.0 ± 1.0 | 0.9 ± 1.0 | 0.9266 |
| Have you been worried about having to change your daily routine (for example, travelling, being away from home)? | 1.2 ± 1.1 | 1.3 ± 1.1 | 0.1318 |
| Have you felt irritable because of your condition? | 1.6 ± 1.0 | 1.8 ± 0.9 | a0.0068 |
| Have you been upset by your condition? | 1.6 ± 1.1 | 1.8 ± 1.0 | a0.0046 |
| Have you felt obsessed by your condition? | 1.3 ± 1.2 | 1.7 ± 1.1 | a< 0.0001 |
| Have you felt stressed by your condition? | 1.5 ± 1.1 | 1.8 ± 1.0 | a< 0.0001 |
| Have you been less self-confident because of your condition? | 1.1 ± 1.1 | 1.7 ± 1.0 | a< 0.0001 |
| Have you felt in control of your situation? | 1.8 ± 1.2 | 1.7 ± 1.0 | 0.5202 |
| Have you been worried about not knowing when you are going to be able to have a bowel movement? | 1.4 ± 1.0 | 1.5 ± 0.9 | 0.2768 |
| Have you been worried about not being able to open your bowels when you needed to? | 1.4 ± 1.1 | 1.6 ± 1.1 | 0.0982 |
| Have you been more and more bothered by not being able to open your bowels? | 1.4 ± 1.1 | 1.7 ± 1.0 | a0.0010 |
| Have you been afraid that your condition will get worse? | 1.5 ± 1.0 | 1.6 ± 0.9 | 0.1261 |
| Have you been felt that your body was not working properly? | 1.5 ± 1.0 | 1.8 ± 1.0 | a0.0003 |
| Have you had fewer bowel movements than you would like? | 1.9 ± 1.1 | 2.1 ± 1.1 | a0.0108 |
| Have you been satisfied with how often you open your bowels? | 1.0 ± 0.8 | 0.8 ± 0.8 | a0.0042 |
| Have you been satisfied with the regularity with which you open your bowels? | 0.9 ± 0.9 | 0.7 ± 0.8 | a0.0007 |
| Have you been satisfied with your bowel function? | 0.9 ± 0.9 | 0.6 ± 0.8 | a< 0.0001 |
| Have you been satisfied with your treatment? | 1.4 ± 1.0 | 1.5 ± 1.0 | 0.1389 |
| Composite score based on PAC-QOL questionnaire | 38.1 ± 16.8 | 42.2 ± 13.6 | a0.0002 |
- * Data represented as mean ± SD;
- a Significant
# P-0264
The potential biological function of miR-150 in the pathogenesis of IBD
Suna Zhou1, Wenguang Ye2, Mingxin Zhang2 and Jun Liang1
1Department of Radiotherapy, Tangdu Hospital, Fourth Military Medical University, Xi'an, China; 2Department of Gastroenterology, Tangdu Hospital, Fourth Military Medical University, Xi'an, China
Aims: The expression of miR-150 was significantly up-regulated in colonic tissue and peripheral blood of ulcerative colitis (UC) and Crohn's disease (CD) patients. But the biological function of miR-150 in the pathogenesis of IBD remains to be explored. Methods: Target prediction algorithms (miRanda, MiRDB, miRWalk, and Targetscan) were used to identify potential targets for miR-150. RT-PCR and Western blot were applied to determine miR-150 and its predicted targets in colonic tissue of UC patients and healthy volunteers. In addition, the human intestinal epithelial HT29 cells were transfected with pre-control and pre-miR-150 expression plasmids using adhesion-assisted lipofection method and then the expression of genes predicted to be targeted by miR-150 were detected by PDCD4, ADIPOR2, NLK, and IL-7. Cells' proliferation was tested by MTT. Results: Our study found that miR-150 expression was significantly up-regulated in colonic tissue of UC patients compared with the normal colonic tissue. By target prediction algorithms and literature review, 4 candidate target genes, including PDCD4, ADIPOR2, NLK, and IL-7, were chosen for the further research. The down-expression of PDCD4, ADIPOR2, NLK, and IL-7 were found in colonic tissue of UC patients compared with the healthy volunteers. Furthermore, forced expression of miR-150 in HT29 cells strongly elevated miR-150 levels and decreased PDCD4, ADIPOR2, NLK, and IL-7 levels. Besides, the proliferation of HT29 cells was inhibited obviously after transfecting with pre-miR-150 plasmids. Conclusion: The present study presents the first evidence that miR-150 and its targets PDCD4, ADIPOR2, NLK, and IL-7 were likely involved in the pathogenesis of IBD.
# P-0273
Unsedated colonoscopy: Patient characteristics and pain score compare with sedated colonoscopy
Bu Seok Jeon
Department of Internal Medicine, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea
Background/Aim: Colonoscopy has important roles in the prevention of colorectal cancer. In sedated colonoscopy, some problems could be occurred including nursing for monitoring and recovery. Therefore, this study was evaluated for patient's acceptances of unsedated colonoscopy comparing with sedated colonoscopy. Method: In this prospective trial, total patients were underwent colonoscopy by three experienced endoscopists and three trainees. We investigated patient characteristics, the degree of pain, and satisfaction with questionnaire, and other factors with regard to sedated and unsedated colonoscopy. Result: Among 186 patients, 110 (59%) underwent unsedated colonoscopy and 94 (51%) were performed by experienced endoscopists. In total patient's group, longer insertion time, higher pain score, and lower satisfaction were revealed in unsedated group than in those sedative group (unsedated vs sedated: 9.0 min vs 6.5 min; P < 0.01, 3.3 vs 1.0; P < 0.01, 56.4% vs 84.2%; P < 0.01), respectively. In experienced as well as trainee group, the patterns of insertion time, pain score, and satisfaction were similar (unsedated vs sedated: 6.0 vs 4.6; P = 0.03, 2.3 vs 0.3; P < 0.01 and 65.2% vs 91.7%; P < 0.01), respectively. At multivariate analysis, factors associated with pain were experienced/trainees (OR 5.1; 95% CI, 1.8–14.2; P < 0.01), sedative/non-sedative (OR 4.9; 95% CI, 1.6–15.4; P < 0.01), weight circumference (OR 1.3; 95% CI, 1.0–1.5; P = 0.03), and satisfaction (OR 45.4; 95% CI, 14.6–140.8; P < 0.01). However, there was no difference weight circumference, education level, history of colonoscopy and abdominal operation, and patient's willingness to repeat the same procedure between two groups. Conclusion: Sedative colonoscopy is more comfortable and satisfied to patient than unsedated one in experienced and trainee groups.
# P-0274
Differences of quality in colonoscopy between non-expert and expert at the right colon
Bu Seok Jeon
Department of Internal Medicine, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea
Background and Aims: Colonoscopy is regarded as the gold standard for colorectal cancer (CRC). However, because the right colon polyps were frequently missing, interval CRC could be developed. It is related to the experience of the endoscopist and quality of the colonoscopy. We aimed to analyze the differences of quality in colonoscopy between non-expert and expert at the right colon. Methods: A total of 590 patients who underwent screening colonoscopy from March 2016 to August 2016 were enrolled in this study. Data were obtained by retrospectively reviewing the medical records. The expert and non-expert group included were three fellows and one experienced staff, respectively. As a quality indicator, the cecal intubation rate and the mean withdrawal time were also measured. The polyp detection rate (PDR) and adenoma detection rate (ADR) was measured with logistic regression model according to withdrawal time, especially in the right colon. Results: The number of colonoscopy performed by non-expert and expert were 250 and 340, respectively. Cecal intubation success rate was 100% in both groups. Expert had longer mean withdrawal times than non-expert (17.3 ± 4.1 min vs 12.1 ± 3.3 min, P < 0.001). Following logistic regression analysis, the detection rate of small polyp (5–10 mm) and non-adenomatous polyp detection rate in right colon showed higher in the expert group (expert vs non-expert: 23.5% vs 9.2%; OR 2.0; P = 0.01, 32.6% vs 13.6%; OR 2.2; P = 0.03), respectively. There were no significant difference in PDR, ADR, diminutive polyps (< 5 mm) and large polyps (> 10 mm) in right colon. Conclusions: Expert colonoscopy is superior to non-expert in withdrawal time, detection rate of small and non-adenomatous polyp in right colon. Key words: colonoscopy, quality, right colon.
# P-0284
Study of colonoscopic biopsies in cases of chronic non-bloody diarrhea with emphasis on microscopic colitis
Aleena Jain
Department of Gastrointestinal and hepatopancreatobiliary Pathology, Seth GS Medical College & King Edward Memorial Hospital, Mumbai, India
Objectives: The most common cause of chronic non-bloody diarrhea (CNBD) is diarrhea predominant irritable bowel syndrome. Many of these cases mimic microscopic colitis (MC), which differs in treatment, and only few studies have been done in India regarding this. Hence, this study was undertaken to determine prevalence of microscopic colitis and other incidental pathology in patients of CNBD with its clinical correlation, along with an attempt defining histological parameters in normal colonic biopsies in Indian population. Methods: Colonic mapping biopsies were stained with H&E, masson-trichome, and immuno-histochemistry for CD3 wherever necessary, from adult patients of CNBD with normal colonoscopy and controls. Results: A total of 184 colonic mapping biopsies from 38 cases and 7 controls were studied. Most patients had abdominal pain. About 76.3% cases showed normal histology (functional diarrhea), 10.5% colonic intraepithelial lymphocytosis, and 5.3% lymphocytic colitis. Mucosal prolapse syndrome with subtle colonoscopic findings and eosinophilic colitis with 55 eosinophils/hpf accounted for 2.6% each. Majority of controls showed < 5 intra-epithelial lymphocytes per 100 surface enterocytes (IEL), < 6-μm subepithelial collagen layer, and < 30 eosinophils/hpf in colon that was similar when compared with other studies. Conclusions: Most patients of CNBD with normal colonoscopy are the cases of functional diarrhea. The prevalence of MC and mean age at presentation is lower and mean IEL count is higher in Indian population, with lymphocytic colitis being more prevalent than collagenous colitis. Key words: Chronic non-bloody diarrhea, irritable bowel syndrome, microscopic colitis, lymphocytic colitis, intraepithelial lymphocytes
# P-0294
MiR-520a regulates cancer-related inflammation by targeting E2F7, IRF2, and Rab22a in colon cancer
Manli Cui1, Mingxin Zhang1, Lingmin Zhang2, Jingjie Wang1 and Suna Zhou3
1Department of Gastroenterology; 2Department of Radiotherapy, Tangdu Hospital, Fourth Military Medical University, Xi'an, 710038; 3Department of Anesthesiology, First Affiliated Hospital, Xi'an Jiaotong University, Xi'an, 710038
Background: Cancer-related inflammation (CRI) play an important role in the development of colon cancer (CC), and the target gene analysis showed that miR-520a potential target genes closely correlated to CRI important signaling pathways. The present study was to evaluate the regulation inhibition of miR-520a on CRI in CC and its mechanism. Methods: The expression of miR-520a in four CC cell lines and a normal colon epithelium cell line (NCM460) after different inflammatory stimuli was detected by RT-PCR. By regulating the expression of miR-520a, Western blot was applied to analysis expression of CRI key transcription factors and representative cytokines; the regulation of miR-520a on expression of potential target genes (E2F7, IRF2, and Rab22a) was explored by RT-PCR, western blot, and dual luciferase reporter gene analysis. Then, target genes shRNA plasmids were constructed to explore their effect on CRI. Last, in vivo experiment was carried out to test effect of miR-520a on tumor growth and CRI. Results: The expression levels of miR-520a in CC cells were lower than that in NCM460. Inflammatory stimuli at 48 h significantly reduced expression of miR-520a in CC cells but had no effect in NCM460. After up-regulation or down-regulation of miR-520a, it was found that miR-520a reduced of CRI key transcription factors and representative cytokines. Then, over-expression of miR-520a significantly altered potential target genes protein expressions, and reporter gene analysis revealed that miR-520a post-transcriptionally regulated expression of target genes by specific area of 3'-UTR. Transfection by target genes shRNA plasmids together could get the same effects of miR-520a on CRI. Furthermore, miR-520a was able to repress tumor growth of CC cells and CRI in vivo. Conclusion: miR-520a influences inhibits key transcription factors and cytokines by targeting (E2F7, IRF2, and Rab22a, implicating its role in the regulation inhibition of CRI in CC.
# P-0308
Acute abdomen with idiopathic mesenteric phlebosclerosis: Case report
Hidetsugu Nakazato1, Koudai Shinzato1, Kinjyo Shogo1, Takeshi Tomiyama1, Shinji Nagamine1, Takehiko Tomori1, Jun Miyagi1, Seiji Nagayoshi1, Yasushi Omine1, Hideaki Sasaki2 and Tetsuhiro Miyara3
1Department of Surgery; 2Department of Emergency Medicine; 3Department of Radiology, Okinawa Redcross Hospital, Japan
Introduction: Idiopathic mesenteric phlebosclerosis (IMP) is an idiopathic disorder characterized by venous calcification and fibrosis of mesenterium and presents various digestive symptoms such as nausea, vomiting, and ileus. Etiology is not obvious, but long-term intake of the traditional Chinese medicine is suspected as one of the causative drugs. Case: The patient was 68-year-old male who have been taking herbal medicine for 17 years because of child A type liver cirrhosis derived from HBV. He had had right abdominal pain 2 months ago and got better naturally. He gradually worsen abdominal pain again and was transferred to our hospital. Physical examination revealed tenderness and rebound tenderness on whole abdomen. Abdominal X-ray showed that multiple minute calcifications existed along with mesenteric side of cecum and ascending colon and part of small intestine was distended with fluid. Computed tomography (CT) showed thickening colic wall from cecum to transverse colon along with multiple minute calcifications, intra-abdominal free air, and ascites from below the right diaphragm to the pelvis. Emergency operation was performed for gastrointestinal perforation with IMP. Pathological examination revealed that fibrosis of the submucosal tissue and venous calcifications was observed in the ileocecal to sigmoid colon. There was no thrombotic finding. Postoperative diagnosis was perforation that was related to IMP. Discussion: If IMP presents with abdominal pain symptoms, gastrointestinal perforation should be excluded. It is suggested that the necessity of stopping or reducing oral administration of herbal medicine.
# P-0310
Development and validation of predictive model for participation in colorectal cancer screening in Korea
Joo Won Chung
Gastroenterology, National Medical Center, Seoul, Korea
Background: The number of individuals partaking in colorectal cancer (CRC) screening still remains to be low even after the implementation of the Korean Government's National Cancer Screening Program for CRC. The aim of this study is to identify factors associated with partaking in CRC screening and develop and validate a predictive model for CRC screening participation. Methods: The Korean National Health and Nutrition Examination Survey (KNHANES) 2007–2010 datasets were used to develop a CRC screening participation screening score. A total of 10 527 individuals aged ≥ 50 who completed the survey and not previously diagnosed with CRC were selected. Both logistic regression (LR) analysis and artificial neural network (ANN) were used to develop predictive models. Multilayer perception ANN was constructed based on 16 clinical variables. We then validated the models using the KNHANES 2011 and 2012 (n = 5986) datasets and compared them with each other. Results: Out of 10 527 individuals selected, 57.0% (n = 6005) responded unscreened for CRC. Among various demographic and socioeconomic factors, the following 8 parameters including, age, household income, marital status, education level, private health insurance, self-reported depression, self-reported health status, and residence were found to be independently associated with CRC screening participation. LR analysis produced screening score (range 0–10.3), and a cut-off point of ≥ 5.5 defined 49% as unscreened for CRC and yielded area under the curve (AUC) of 0.626. When validated with KNHANES 2011 and 2012 datasets, the AUC of the defined LR model was 0.663; meanwhile, the AUC of ANN-based predictive model was 0.743. Conclusion: The ANN produced better performing model than LR analysis based model in identifying population with low CRC screening participation. Sensible approaches should be implemented to encourage partaking in CRC screening in the identified individuals.
# P-0329
MiR-29a/HSP47 pathway is crucial for ileocolonic anastomosis fibrosis in IL-10-deficient mice that underwent ileocecal resection
Hong– Wei Hou1, Zhen-Ling Ji2, Dong Wang2, Jin-Min Wang2 and Rong Wu2
1Southeast University, Nanjing, China; 2Department of General Surgery, Zhongda Hospital, Southeast University, Nanjing, China
Background: Ileocecal resection (ICR) is most common in Crohn's disease (CD) among many surgery interventions. However, reoperations are often needed owing to the frequent anastomotic recurrences. The purpose of this study is to investigate the effect of miR-29a/HSP47 pathway in the fibrosis of ileocolonic anastomosis. Methods: Eighteen IL-10−/− mice were randomized to three groups in average as control, saline-treated ICR (ST-ICR) and pre-miR-29a ICR (miR-29a-ICR) group. Effects of miR-29a treatment on small intestine (SI) and ileocolonic anastomosis were determined by histopathology, Western blot, and Elisa analysis. Analysis of changes of miR-29a/HSP47 pathway was measured by qRT-PCR and Western blot. Results: Compared with control group, significantly higher inflammation score of SI and anastomosis was observed in ST-ICR group (P < 0.05) but prominently reversed by miR-29a, which is also in accordance with the results of area of CD4+ cells infiltration. With rising of inflammation severity, both the level of IL-6 and TNF-α ascended, while they were significantly decreased after the treatment of pre-miR-29a (P < 0.05). Besides, the fibrosis score and collagen I and III levels in ST-ICR group were significantly decreased by pre-miR-29a 8 weeks after performing ICR (P < 0.05). qRT-PCR showed that the level of HSP47 in anastomosis of ST-ICR group is significantly higher than control group(P < 0.05), although the production of HSP47 was significantly inhibited by pre-miR-29a. The changes of HSP47 were inversely correlate with the trend of miR-29a but positively correlate with the inflammatory and fibrosis severity. Conclusion: Our study demonstrated that miR-29a/HSP47 signaling pathway might be a new therapeutic strategy for CD and is valuable in the prevention of postoperative intestinal anastomotic inflammation and fibrosis for CD patients.
# P-0361
Increased risk of advanced colorectal neoplasia in asymptomatic individuals with family history of colorectal cancer: A systematic review and meta-analysis
Martin Cs Wong1,2,3, Ch Chan1, Jiayan Lin1, Yuan Fang1, Wilson Wl Cheung1, Miaoyin Liang1, Dh Fung1, Cp Yu4 and Jason Lw Huang1
1School of Public Health and Primary Care, Faculty of Medicine, Chinese University of Hong Kong(CUHK), HKSAR, China; 2Institute of Digestive Disease, Faculty of Medicine, CUHK, HKSAR, China; 3State Key Laboratory of Digestive Disease, Faculty of Medicine, CUHK, HKSAR, China; 4Li Ping Medical Library, CUHK, HKSAR, China
Background: Whether screening participants with a known family history of colorectal cancer (CRC) in their first degree relatives (FDRs) has increased risk of advanced neoplasia remains inconclusive. We tested the hypothesis that there is no difference in the risk of advanced neoplasia among asymptomatic individuals with family history of CRC in their FDRs vs. those without. Methods: We searched Ovid Medline, EMBASE, and grey literature from their inception to December 2016 and included all screening studies that investigated the relationship between family history of CRC in FDR and the occurrence of ACN. Data were independently extracted by two reviewers with disagreements resolved by a third reviewer. We pooled absolute risks and odds ratios with a random effects meta-analysis. Subgroup analyses were performed according to the reported number of FDRs with CRC; age of FDR when CRC was diagnosed; study design/setting; assessment method of family history; and the quality of selection studies. Heterogeneity was characterized with the I2 statistics. Results: We pooled 15 studies, including 144 780 asymptomatic subjects. A family history of CRC in an FDR conferred a significantly higher risk of advanced neoplasia (OR = 1.49, 95% CI = 1.38–1.59; P = 0.18, I2 = 10.0%) than those with no family history in an FDR. No publication bias was identified by Begg's (tau = 0.26, P = 0.20) and Egger's test (t = 0.55, P = 0.59). No significantly different risk of advanced neoplasia was observed in subgroup analyses, regardless of the numbers of FDRs; the CRC onset age of FDR; population based or hospital-based study; medical record or self-reported family history; or high and low study quality. Conclusions: Our findings supported that asymptomatic individuals with family history of CRC in FDRs had a significantly higher risk of advanced neoplasia. Screening tests that could primarily detect and remove advanced neoplasia are indicated for these subjects. Key word: colorectal cancer screening; family history; advanced neoplasia; first-degree relatives; meta-analysis
# P-0364
Incidence of prostate cancer in colorectal cancer patients: Nationwide retrospective cohort study
Hyun Soo Kim, Dong Woo Shin and Dong Ho Lee
Department of Internal Medicine and Seoul National University Bundang Hospital, Seongnam, Gyeonggi-do, South Korea
Background: Colorectal cancer is one of the most common cancers diagnosed worldwide, and prostate cancer is also the most common malignancy in men. Both of them also tend to occur more frequently in developed countries. There have been several reports on the association between colorectal cancer and prostate cancer, but the conclusions are inconsistent. Methods: We aim to investigate the incidence of prostate cancer as a second primary malignancy among patients with prior primary colorectal cancer (CRC) using a nationwide population-based dataset. We followed up with patients registered in the Republic of Korea National Health Insurance Corporation who were diagnosed with colon cancer between 2007 and 2014 and investigated the incidence of prostate cancer (one year lag period). The incidence of prostate cancer was also evaluated in age and gender-matched controls using a cohort of patients diagnosed with colorectal cancer during the same period. Follow-up started at the date of CRC diagnosis and continued until the earliest date of prostate cancer diagnosis, death, loss to follow-up, or the 2015 year-end. Multivariable models included the variables of age, sex, body mass index, hypertension, diabetes mellitus, dyslipidemia, and income. Results: We analyzed a total of 85 462 first primary CRC survivors. During the follow-up period of 494 222 person-years, 2005 (2.3%) developed prostate cancer (incidence rate 4.06/1000 person-years). Compared with the general population, CRC patients had a significantly increased risk of secondary prostate cancer (HR = 2.30, 95% CI = 2.182–2.426; P < 0.001). Multivariate analysis showed that age< 55 years (HR = 20.85, 95% CI = 11.88–36.59; P < 0.001) is a significant independent predictor of prostate cancer development. Conclusion: Men who develop colorectal cancer are at an increased risk of prostate cancer, with the greatest risk in men under the age of 55. This data suggests that CRC patients under 55 years old require regular screening for prostate cancer.
# P-0386
Acute mesenteric ischemia during colonoscopy: A case report
Beverly Lou T Mamitag and Virgilio P Banez
Section of Gastroenterology and Digestive Endoscopy, Department of Internal Medicine, Manila Doctors Hospital, Philippines
Introduction: Acute mesenteric ischemia is rare and accounts for 1:1000 to 1: 10 000 acute hospital admissions in USA, Europe, and Japan and is associated with high morbidity and mortality if remain unrecognized. It can happen during colonoscopy, especially in patients with history of cardiac arrhythmia. Case Description: This is a case of a 51-year-old female, known hypertensive with paroxysmal atrial fibrillation, who initially presented with constipation with bloatedness after a spine surgery. Chest findings were normal. Heart rate was normal, and rhythm was regular. Abdominal examination revealed a globular abdomen with hypoactive bowel sounds, tympanitic on percussion, soft on palpation with tenderness in all quadrants. No peritoneal signs. On digital rectal examination, noted with tight sphinteric tone, no mass, no blood with fecal material present on examination finger. The constipation was unresponsive to laxatives, prokinetic, and enemas. Management: Initial impression was Ileus probably secondary to cervical dysautonomia versus Partial Gut Obstruction from Colonic New Growth. On CT scan, there was only noted dilatation of descending and transverse colon with fecal retention without evidence of bowel obstruction. Patient then underwent colonoscopy, and during colonoscopy, had episode of atrial fibrillation and desaturations and suddenly developed gangrenous bowels from previously normal-looking colonic mucosa and underwent emergency exploratory laparotomy. Recommendations: Different therapeutic approaches are proposed for management of superior mesenteric artery embolus, and these include surgical revascularization, intra-arterial perfusion with a thrombolytic agent, intra-arterial perfusion of vasodilators, and simple systemic anticoagulation. But there is a uniform agreement that exploratory laparotomy is mandatory when signs of peritonitis are present.
# P-0391
Emergency department visits for acute lower gastrointestinal bleeding and outdoor temperature changes in Korea
Gukhwan Choi, Jaeyoung Chun, Jue Lie Kim, Sun A Park, Hosim Soh, Han Myung Lee, Yoon Jun Kim, Jong Pil Im, Sang Gyun Kim and Joo Sung Kim
Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea
Background/Aims: Acute gastrointestinal bleeding (GIB) shows seasonal and monthly variations. However, the effect of outdoor temperature changes on the development of acute GIB has not been evaluated yet. The aim of this study was to determine the seasonal and monthly patterns of acute lower GIB and to define the outdoor temperature parameters associated with the seasonal variation in acute lower GIB. Methods: From March 2011 to February 2016, the medical records of all patients who visited the emergency department for the management of acute lower GIB at Seoul National University Hospital in Korea were retrospectively reviewed. Acute lower GIB was defined as melena or hematochezia that occurred within 24 hours before the emergency department visits and was confirmed by endoscopic and/or radiologic evaluation. We evaluated the seasonal and monthly patterns of the emergency department visits for acute lower GIB and analyzed the association between the seasonal variation of acute lower GIB and outdoor temperature parameters including air temperature and changes in intraday temperature. Results: A total of 1264 patients with acute lower GIB were enrolled in this study. The study population comprised 720 males (57.0%), and the mean age was 63.7 years. Emergency department visits for acute lower GIB showed seasonal variation: 360 (28.5%) in spring, 292 (23.1%) in summer, 308 (24.4%) in autumn, and 304 (24.0%) in winter (P = 0.035). The monthly pattern of the emergency department visits for acute lower GIB was also detected (P = 0.002) with the most frequent visits in April and the least in July. Among the outdoor temperature parameters, the intraday temperature change (defined as the difference between daily maximum and minimum temperature) showed the strongest association with the emergency department visits for acute lower GIB (Spearman correlation coefficient r = 0.653, P < 0.001). Conclusions: The emergency department visits for acute lower GIB has a clear seasonal and monthly variation. The seasonal variation in acute GIB might be associated with change in intraday temperature. Keywords: Gastrointestinal bleeding; seasonal variation; monthly variation; temperature change; emergency department
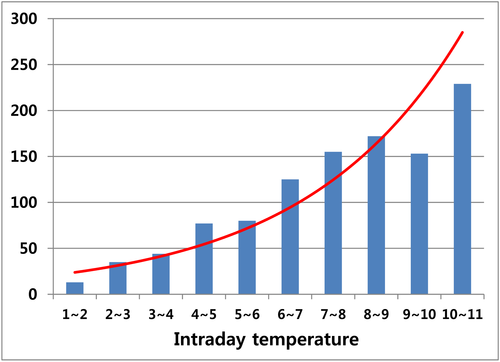
# P-0398
Efficacy of contrast-enhanced computed tomography (CECT) for colonic diverticular bleeding
Masato Kinoshita, Yuta Inoue, Tetsuyuki Abe, Ryoko Futai, Mika Miki, Syohei Abe, Ayaka Sasaki, Katsuhide Tanaka, Tomoo Yoshie, Takayuki Oose and Tsuyoshi Sanuki
Department of Gastroenterology, Kita-harima Medical Center, Ono, Japan
Background: Colonic diverticular bleeding is one of the most common conditions seen in clinical settings. However, detection of the active bleeding site is difficult in some cases. Previous articles have reported the efficacy of contrast-enhanced computed tomography (CECT) for the detection of the bleeding site; thus, we retrospectively evaluated the efficacy of CECT in our institution. Methods: We studied 109 patients having colonic diverticular bleeding between April 2011 and October 2016. We performed CECT as far as possible, except in patients who had contrast media allergy, asthma, and kidney disease. We, at first, sequentially performed an urgent colonoscopy and endoscopic hemostasis for those patients in whom the bleeding site was detected (clipping for active diverticular bleeding). Intravascular treatment (coil embolization) and surgery were performed as needed for cases that were difficult to treat with endoscopic hemostasis. Results: CECT was performed in 59% (64/109) patients, and active extravasation detected in 50% of these (32/64). The detection rate of the active bleeding site was 69% (22/32) in patients showing extravasation and 41% (13/32) in those without extravasation. The detection rate in the extravasation group was significantly high (chi-squared test, P value = 0.024). The endoscopic detection rate of an active bleeding site was 44% (48/109), and rate of successful endoscopic hemostasis was 98% (47/48). Intravascular treatment was performed in 5% (5/109) of the patients and surgery (including elective surgery) in 7% (8/109). There was no mortality case among the studied patients. Conclusion: CECT has good efficacy in the detection of colonic diverticular bleeding sites, and therefore, we recommend that CECT should be performed before an urgent colonoscopy.
# P-0400
Risk of advanced colorectal neoplasm by the combined United States and United Kingdom risk stratification guidelines (Short title: Postpolypectomy surveillance guideline)
Dong Il Park1,2, Soo-kyung Park1,2
1Division of Gastroenterology, Department of Internal Medicine, Kangbuk Samsung Hospital, 2Gastrointestinal Cancer Center, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
Background/Aims: The United Kingdom (UK) differs from the US guidelines in that they only consider the patients with ≥ 5 adenomas and do not consider villous histology or high-grade dysplasia (HGD) when they categorize risk groups. Thus, we aimed to investigate the risk of advanced colorectal neoplasm (CRN) by categorized risk groups, considering both ≥ 5 adenomas and histology (villous or HGD). Methods: A total of 2570 patients with ≥ 1 adenoma at index colonoscopy who underwent follow-up colonoscopy were included. The patients were divided into 6 groups : group 1, 1–2 non-AAs (AA; ≥ 10 mm or HGD or villous adenoma); group 1A, 1–2 adenomas with ≥ 1 AA; group 2, 3–4 non-AAs; group 2A, 3–4 adenomas with ≥ 1 AA; group 3, ≥ 5 non-AAs; and group 3A, ≥ 5 adenomas with ≥ 1 AA. The risk of advanced CRN at 3 years was compared between the 6 groups. Results: Group 3A showed higher risk of advanced CRN (9.6%) than group 3 (4.5%, P = .03) and group 1A (4.6%, P < .001). The risk of advanced CRN in the group 3 (4.5%) showed no difference compared with the group 1A (4.6%, P = .91) or group 2A (6.8%, P = .25). There was no difference between groups 1 and 2 in the risk of advanced CRN (1.7% vs 2.2%, P = .22). The Cox proportional hazard model revealed that ≥ 1 AA at index colonoscopy was an independent risk factor of advanced CRN. Conclusions: More intensive surveillance than the 3-year interval for the patients with ≥ 5 adenomas with ≥ 1 AA and less intensive surveillance than the 3-year and 1-year interval for those with 3–4 non-AAs and ≥ 5 non-AAs, respectively, might be suggested in a Korean population. Keywords: colon polypectomy; adenoma; cancer; surveillance
Abbreviations used in this paper: AA, advanced adenoma; BMI, body mass index; CIs, confidence intervals; CRC, Colorectal cancer; CRN, colorectal neoplasm; HGD, high-grade dysplasia; JRSC, Japanese Research Society Classification; ORs, odds ratios; UK, United Kingdom; US, United States.
# P-0403
The role of TLR2-mediated Treg/Th17 imbalance in the pathogenesis of DSS-induced mice
You Fu Xie1, Jian Yu Hao1, Yan Hua Pang1, Ya Hui Ma2 and Xin Juan Liu1
1Department of Gastroenterology, Bei Jing Chao Yang Hospital, Capital Medical University, China; 2Department of Internal Medicine, Bei Jing Hai Dian Maternal and Child Health Hospital, China
Background: The imbalance of Treg/Th17 cells in the DSS-induced mice is related with the reduction of CD45RA-FoxP3high-activated Treg (FrII) cells, which has the real function of immunosuppression, and with the elevation of CD45RA-FoxP3low Treg(FrIII) cells, which provide FoxP3+IL17a+ trait but lack of immunosuppressive capacity.TLR2 is an important moleculer in the differentiation between Treg and Th17 cells. The aim of our research is evaluating the levels of Th17 cells, Treg, and its subsets by blocking the TLR2 in dextran sulfate sodium (DSS)-induced mice. Methods: Eighteen mice were divided into three groups, including healthy control mice (group A), ulcerative colitis mice (group B), and TLR2mAb-intervened UC mice (group C). DAI (disease activity index) and the pathology of rectum were evaluated. Treg cells with their subsets Th17 cells and CD25+FoxP3+IL-17a+ cells from various tissues of mice were evaluated by flow cytometry. Results: The symptoms, DAIs, and the inflammation of colonic mucosa of group C were alleviated compared with group B. T compared with group B, both of the Treg and Th17 cell levels were declined in PBMC of group C (1.153 ± 0.028 vs 1.275 ± 0.063 and 0.273 ± 0.061 vs 0.488 ± 0.015,P < 0.05, respectively). Increased FrII cells in spleen, PBMC, MLN, and LPC and declined FrIII cells in spleen and PBMC were observed in group C compared with group B (P < 0.05, respectively).The level of CD3+CD8-CD25+FoxP3+IL17a+ cells in spleen,PBMC, MLN, and LPC of group C were lower than group B (P < 0.05, respectively). Conclusion: Blocking TLR2 could improve the level of FrII cells in PBMC, MLN, and LPC but reduce the levels of FrIII and FoxP3+IL17a+ cells in DSS-induced mice. Furthermore, TLR2mAb could alleviate the DAI index as well as the inflammation of colonic mucosa in DSS-induced mice.
# P-0405
Nuclear factor-κB activation correlates with disease phenotype in Crohn's disease
Yoo Min Han1, Jaemoon Koh2, Ji Won Kim3, Ji Min Choi1, Goh Eun Chung1 and Joo Sung Kim1
1Department of Internal Medicine and Healthcare Research Institute, Healthcare System Gangnam Center, Seoul National University Hospital, Seoul, Korea; 2Department of Pathology, Seoul National University College of Medicine, Seoul, Korea; 3Department of Internal Medicine, Seoul National University Boramae Hospital, Seoul National University College of Medicine, Seoul, Korea
Background: Unregulated activation of nuclear factor-κB (NF-κB) plays a critical role in the pathogenesis of Crohn's disease. In this study, we investigated the clinical characteristics and disease outcome of Crohn's disease patients with varying levels of the NF-κB activation. Methods: Crohn's disease patients who underwent surgical bowel resection were divided into two groups, based on the activation status of NF-κB. NF-κB activation was assessed by the immunoreactivity of nuclear NF-κB during immunohistochemical staining of bowel resection specimens. We compared the demographic and clinical characteristics between groups. Furthermore, the occurrence of reoperation, readmission, and medication change due to disease flare-up were investigated according to NF-κB activation status. Results: Among 83 Crohn's disease patients, 47 (56%) showed high NF-κB activity and 36 (44%) showed low NF-κB activity. Patients with high NF-κB activity had higher frequency of ileocolonic involvement (P = 0.028) and lower frequency of perianal involvement (P = 0.042) relative to patients with low NF-κB activity. Total histologic scores were significantly higher in patients with high NF-κB activity than those with low NF-κB activity (P = 0.044). There was no significant difference in the frequency of reoperation, readmission, and medication change in relation to NF-κB activation status. Conclusions: Crohn's disease patients with high NF-κB activation showed specific clinical manifestations of higher frequency of ileocolonic involvement and lower frequency of perianal involvement relative to patients with low NF-κB activation. High NF-κB activity was associated with more severe histologic scores. However, the NF-κB activity did not affect the outcome and disease course after surgery.
# P-0424
Risk factors and outcomes of emergency room visits in intestinal Behçet's disease
Jihye Park1, Jae Hee Cheon1,2, Hyun Jung Lee1,2, Soo Jung Park1,2, Tae Il Kim1,2 and Won Ho Kim1,2
1Department of Internal Medicine, Yonsei University College of Medicine, 50-[1] Yonsei-ro, Seodaemun-gu, Seoul, 037[2][2], Korea; 2Institute of Gastroenterology, Yonsei University College of Medicine, 50-[1] Yonsei-ro, Seodaemun-gu, Seoul, 037[2][2], Korea
Background/Aims: Intestinal Behçet's disease (BD) is a chronic recurring intestinal vasculitic disorder that can lead many patients to visit the emergency room (ER). We aimed to identify the utilization patterns of ER by intestinal BD patients and to investigate the independent risk factors associated with intestinal BD-related ER visits. Methods: Between March 2005 and January 2017, a total of 606 intestinal BD patients were registered at the Inflammatory Bowel Disease (IBD) Clinic of Severance Hospital, Seoul, Korea. We retrospectively reviewed the medical records of intestinal BD-related ER visits. Multivariate analyses were conducted to identify the independent risk factors of intestinal BD-related ER visits. Results: Of the 606 persons with intestinal BD, 186 (30.5%) visited the ER at least once, and the total number of ER visits was 510. The causes of ER visits of intestinal BD patents were abdominal pain (60.6%), gastrointestinal bleeding (22.0%), fever (19.8%), vomiting (12.2%), and diarrhea (10.0%) in decreasing order. The hospitalization rates from ER was 77.1%, and surgical rate from ER was 6.2%. In the Cox proportional hazard model, lower social economic status (hazard ratio [HR]: 1.884, 95% confidence interval [CI]: 1.282–2.768, P = 0.001), higher comorbidity index (HR: 1.548, 95% CI: 1.056–2.271, P = 0.025), use of corticosteroids (HR: 1.459, 95% CI: 1.189–1.790, P < 0.001), higher C-reactive protein (CRP) level (HR: 1.375, 95% CI: 1.052–1.797, P = 0.020), and higher disease activity index for intestinal Behçet's disease (DAIBD) score (HR: 1.013, 95% CI: 1.011–1.015, P < 0.001) were independent risk factors associated with intestinal BD-related ER visits. While older age (HR: 0.982, 95% CI: 0.974–0.990, P < 0.001), disease duration (HR: 0.850, 95% CI: 0.829–0.872, P < 0.001), use of opioids (HR: 0.528, 95% CI: 0.341–0.819, P = 0.004), higher hemoglobin level (HR: 0.944, 95% CI: 0.898–0.993, P = 0.025) were significantly associated with decreased ER visits. Conclusions: The presences of low income, comorbidity, high DAIBD score, use of corticosteroid, and high CRP level were associated with intestinal BD-associated ER visits. Key words: Behçet's disease; emergency room; risk factor; outcome
| Variables | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | *P value | HR | 95% CI | *P value | |
| Age (years) | 0.975 | 0.968–0.982 | < 0.001 | 0.982 | 0.974–0.990 | < 0.001 |
| Males | 0.793 | 0.665–0.947 | 0.010 | 1.146 | 0.924–1.421 | 0.215 |
| Disease duration (years) | 0.885 | 0.868–0.902 | < 0.001 | 0.850 | 0.829–0.872 | < 0.001 |
| Medical aid (vs National health insurance) | 1.822 | 1.322–2.510 | < 0.001 | 1.884 | 1.282–2.768 | 0.001 |
| Charlson comorbidity index | ||||||
| 0 | 1.000 | reference | < 0.001 | 1.000 | reference | 0.026 |
| 1 | 1.305 | 0.962–1.772 | 0.087 | 1.548 | 1.056–2.271 | 0.025 |
| ≥ 2 | 1.839 | 1.495–2.263 | < 0.001 | 1.266 | 0.964–1.663 | 0.090 |
| DAIBD score | 1.014 | 1.012–1.015 | < 0.001 | 1.013 | 1.011–1.015 | < 0.001 |
| Deep ulcer (vs. aphthous, shallow ulcer) | 1.808 | 1.519–2.152 | < 0.001 | 1.191 | 0.920–1.541 | 0.184 |
| Volcano shape ulcer (vs. oval, geographic ulcer) | 1.716 | 1.412–2.085 | < 0.001 | 0.885 | 0.651–1.204 | 0.437 |
| Previous intestinal resection | 1.384 | 1.159–1.652 | < 0.001 | 1.400 | 1.111–1.764 | 0.004 |
| Mesalamine or sulfasalazine | 1.025 | 0.425–2.475 | 0.956 | |||
| Corticosteroid | 1.972 | 1.657–2.348 | < 0.001 | 1.459 | 1.189–1.790 | < 0.001 |
| Azathioprine | 1.971 | 1.643–2.364 | < 0.001 | 1.073 | 0.859–1.339 | 0.536 |
| Methotrexate/6-mercaptopurine | 1.483 | 0.871–2.525 | 0.146 | |||
| Anti-TNFα | 1.711 | 1.169–2.506 | 0.006 | 0.750 | 0.479–1.172 | 0.207 |
| Metronidazole/ciprofloxacin | 2.268 | 1.867–2.755 | < 0.001 | 1.165 | 0.919–1.477 | 0.206 |
| Opioid | 1.513 | 1.066–2.147 | 0.021 | 0.528 | 0.341–0.819 | 0.004 |
| Anxiety drug | 1.577 | 1.141–2.180 | 0.006 | 1.395 | 0.940–2.069 | 0.098 |
| NSAID | 1.296 | 1.078–1.558 | 0.006 | 1.204 | 0.958–1.513 | 0.112 |
| CRP (mg/L) | 2.339 | 1.941–2.817 | < 0.001 | 1.375 | 1.052–1.797 | 0.020 |
| ESR (mm/hr) | 1.012 | 1.009–1.014 | < 0.001 | 1.002 | 0.999–1.006 | 0.233 |
| Hemoglobin (g/dL) | 0.843 | 0.810–0.877 | < 0.001 | 0.944 | 0.898–0.993 | 0.025 |
# P-0450
Post-marketing safety experience of vedolizumab in patients with pre-existing viral hepatitis
Deng-Chyang Wu1, Ida Normiha Hilmi2, Shashi Adsul3, Aimee Blake4 and Fatima Bhayat4
1Kaohsiung Medical University Chung-Ho Memorial Hospital, Kaohsiung, Taiwan; 2University Malaya Medical Centre, Kuala Lumpur, Malaysia; 3Takeda Pharmaceuticals (Asia Pacific) Pte. Ltd., Singapore; 4Takeda Development Centre Europe Ltd, London, UK
Background: Systemic immunosuppressive treatment can reactivate the latent hepatitis virus.1 The gut selectivity of vedolizumab (VDZ) may be associated with a lower risk of hepatitis virus reactivation than anti-tumor necrosis factor-alpha (TNFα) agents. As VDZ clinical trials excluded patients with chronic viral hepatitis B or C, there are no clinical trial data available in this population. Here, we describe the VDZ safety experience in patients with pre-existing hepatitis B or C in the post-marketing setting. Methods: Adverse events (AEs) were identified from the VDZ Global Safety Database (data-cut May 20, 2014 to Nov 19, 2016) and included if patients' medical history or concurrent conditions included a Medical Dictionary for Regulatory Activities (MedDRA) preferred term of hepatitis B or C infection. Results: In the context of ~77 382 patient-years of VDZ post-marketing exposure (30 470 AEs), 15 patients (n = 6 ulcerative colitis; n = 7 Crohn's disease; n = 2 indication not reported [NR]) with hepatitis B (n = 5, including 2 chronic) or C (n = 10) infection were identified. Eight patients received prior/concomitant anti-TNFα therapy; NR n = 2. 51 AEs (n = 13 serious [non-fatal]; n = 38 non-serious) were reported, reflecting the general VDZ safety profile. Liver-related events occurred in two patients with hepatitis C (one event each): hepatic neoplasm and hepatic mass. Both resulted in VDZ discontinuation. Of events with a reported outcome, 22/26 (84.6%) were resolved/resolving and 4/26 (15.4%) were unresolved at the time of reporting; NR n = 25. VDZ was continued in 10/14 (71.4%) patients; NR n = 1. Discussion and Conclusion: There was no evidence of increased risk of viral reactivation in patients with hepatitis B or C receiving VDZ. Limitations associated with post-marketing safety reporting and currently limited VDZ availability in regions with endemic hepatitis B and C should be considered when interpreting these results.
Reference:
# P-0463
Fructo-oligosaccharide exacerbates stress-induced visceral hyperalgesia and gut inflammation in a murine model
Binrui Chen1, Lijun Du1, Huiqin He1, John J Kim1,2 and Ning Dai1
1Department of Gastroenterology, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Zhejiang, China; 2Division of Gastroenterology, Loma Linda University Medical Center, Loma Linda, USA
Background and Aim: Low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) diet can reduce symptoms of irritable bowel syndrome (IBS), but mechanisms were poorly understood. We aim to explore the role of FODMAPs in triggering IBS symptoms by investigating visceral sensitivity, intestinal inflammation, and short chain fatty acid (SCFA) in stress-induced IBS mice model. Methods: Mice were subjected to water avoidance stress (WAS condition; 1 h/day for 10 days) or sham stress (basal condition; 1 h/day for 10 days) with a gavage of saline or saline solution containing FOS (8 g/kg) for 2 weeks. Then visceral sensitivity was measured by abdominal withdrawal reflex, and mucosal inflammation was measure by histological analyses. Immunohistochemistry, reverse transcription, and gas chromatography were used to estimate mucosal mast cell, gut cytokines expression, and SCFA, respectively. Results: Stress induced a mice model with visceral hyperalgesia and low-grade inflammation. In WAS condition, increased visceral sensitivity and mucosal mast cell (12.3 ± 2.61 vs 8.33 ± 3.55, P < 0.01), IL-23 mRNA expression (3.17 ± 2.11-fold, P < 0.05) in ileum and IL-1β mRNA expression (2.45 ± 1.55-fold, P < 0.05) in colon were observed in FOS-administered mice compared with saline-administered mice. In addition, concentrations of acetic (2.48 ± 0.62 vs 1.04 ± 0.10, P < 0.01) and butyric (0.27 ± 0.09 vs 0.19 ± 0.003, P < 0.05) of colon feces increased in FOS-administered mice compared with saline-administered mice in WAS condition. In basal condition, no difference of visceral sensitivity, intestinal inflammation, and SCFA were observed between mice treated with FOS or saline. Discussion and Conclusion: FOS leads to an increase in visceral sensitivity and intestinal inflammation in stress-induced IBS mice, and these may be explained by the increased production of SCFA. These findings support the hypothesis that visceral hyperalgesia and gut inflammation aggravated by certain FODMAPs may be responsible for IBS symptoms generation and indicate an alternative mechanism of the efficacy of low-FODMAP diet for IBS patients.
# P-0476
Optimization of sacral nerve stimulation for colonic inflammation in TNBS-induced colitis in rats
Nina Zhang1,2, Xuhang Li2, Han Zhang2, Liuqin Jiang2, Shengai Zhang2, Jieyun Yin2, Pankaj P Pasricha2, Xiaoping Zou1 and Jiande D Z Chen2
1Division of Gastroenterology, Nanjing Drum Tower Hospital, Nanjing, China; 2Division of Gastroenterology and Hepatology, Johns Hopkins University, Baltimore, Maryland, USA
Background/Aims: The aim of our study was to explore feasibility of sacral nerve stimulation (SNS) that would have less side effects for colonic inflammation, optimization of SNS methodologies and mechanisms. Methods: Intestinal inflammation was induced by intrarectal administration of TNBS (2,4,6-trinitrobenzenesulfonic acid) in rats. Five days later, the rats were treated with SNS of different methodologies for 10 days. Three major efforts were made in optimizing SNS: 1) to determine the best stimulation duration; 2) to determine the best stimulation location; and 3) to determine the best stimulation parameters. Inflammatory responses were assessed by disease activity index (DAI), histological sections, and myeloperoxidase (MPO) activity. Levels of inflammatory cytokines, plasma norepinephrine (NE), and pancreatic polypeptide (PP) in both plasma and tissues were assessed. Results: 1) Stimulation duration: both SNS-1h and SNS-3h significantly decreased the DAI scores, microscopic scores, MPO activity, and pro-inflammatory cytokines (IL-2/EGF/IL-13/IL-1a/IL-12p70 in serum and IL-1a/IL-6/IL-17A/TNF-α in tissue) and increased anti-inflammatory cytokines (IL-4 in serum and IL-10 in tissue), compared with sham-SNS (all P value < 0.05); SNS-1h was superior to SNS-3h. SNS-1h remarkably decreased plasma NE (2.80 ± 0.54 vs 8.67 ± 3.98, P = 0.04) and increased plasma PP (4.34 ± 0.35 vs 2.96 ± 0.13, P = 0.003) compared with sham-SNS. 2) Stimulation location: bipolar not bilateral or unipolar stimulation significantly decreased the DAI scores, microscopic scores, MPO activity, pro-inflammatory cytokines (IL-5/IL-12p70 in serum and TNF-α in tissue), and plasma NE and increased anti-inflammatory cytokines (IL-10 in tissue) and plasma PP (all P value < 0.05). 3) Stimulation parameters: SNS with 5Hz intermittent stimulation but not the 14Hz continuous SNS decreased the DAI scores, microscopic scores, MPO activity, and pro-inflammatory cytokines (IL-5/IL-13 in serum and TNF-α/LIX in tissue) and increased anti-inflammatory cytokines (IL-4 in serum and IL-10 in tissue) and plasma PP (all P value < 0.05). Conclusion: Bipolar stimulation for 1 hour daily using intermittent 5 Hz parameters is most effective in improving colonic inflammation in rats.
# P-0487
The usefulness of enteral nutrition therapy followed by endoscopic monitoring in patients with Crohn's disease after intestinal resection
Satoshi Hiyama1, Hideki Iijima2, Tsunekazu Mizushima3 and Tetsuo Takehara2
1Department of Gastroenterology, JCHO Osaka Hospital; 2Department of Gastroenterology and Hepatology; 3Department of Therapeutics for Inflammatory Bowel Diseases, Osaka University Graduate School of Medicine
Background: To prevent the recurrence of post-operative Crohn's disease (CD) patients is important. Our treatment strategy in post-operative CD patients is to start enteral nutrition (EN) therapy combined with continuation of pre-operative medication followed by adjustment of medication including anti-TNF antibody according to the endoscopic anastomosis findings within one year after the operation. We evaluated the efficacy of this strategy. Methods: This is a retrospective study of 35 CD patients who underwent intestinal resection between January 2008 and March 2015 at Osaka University Hospital. Rutgeerts score ≧ i2 at the time of endoscopy was defined as endoscopic recurrence (ER), and clinical course within 2 years from the operation was compared with non-ER group. Results: Clinical backgrounds including past history of intestinal resection did not differ between ER (n = 10) and non-ER group (n = 25). The proportion of the patients who continued EN ≥ 900 kcal/day was significantly lower in ER group compared with non-ER group (P < 0.05), but no difference was observed in the proportion of other medications including anti-TNF therapy. Eight patients (80%) in ER group adjusted their medication including starting, dose-escalating, or switching anti-TNF antibody after the endoscopy. Although serological remission (CRP < 0.2 mg/dL) rate was significantly lower in ER group compared with non-ER group at the time of endoscopy [30% (3/10) vs 88% (22/25); P < 0.001)], both clinical remission (CDAI < 150) and serological remission rate at 2 years after the operation did not differ between two groups. Conclusions: EN therapy with therapeutic adjustment according to the endoscopic anastomosis findings may improve clinical course of CD patients after intestinal resection.
# P-0490
The outcomes and risk factors of early readmission in patients with intestinal Behçet's disease
Yong Eun Park1, Jae Hee Cheon1,2, Yehyun Park1,2, Soo Jung Park1,2, Tae Il Kim1,2 and Won Ho Kim
1Department of Internal Medicine; 2Institute of Gastroenterology, Yonsei University College of Medicine, Seoul, Korea
Background and Aim: Hospital readmission rate is an integral quality of care measurement for hospitalized patients that is unknown for intestinal Behçet's disease cases. The purpose of this study was to investigate risk factors and outcomes for patients readmitted with intestinal Behçet's disease. Methods: We retrospectively reviewed patients with intestinal Behçet's disease who were readmitted to our hospital between 2005 and 2016. We analyzed the risk factors and outcomes for early readmission within 3 months. Results: Of the 204 patients with intestinal Behçet's disease readmitted between 2005 and 2016, 103 patients (50.5%) were readmitted within 3 months and 101 patients (49.5%) were never readmitted or readmitted after 3 months. Factors including abdominal pain, diarrhea, fever at first admission, bowel resection surgery, volcano type ulcer, high disease activity index for intestinal Behçet's disease score, high erythrocyte sedimentation rate, high C-reactive protein levels, ulcer location, and use of 5-aminosalicylic acids, steroids, antibiotics, or opioids were significantly associated with early readmission in the univariate analysis (all P < 0.05). After multivariate analysis, a short hospital stay at first admission (P = 0.004), a high disease activity index for intestinal Behçet's disease score (P < 0.001), steroid use (P = 0.028), and opioid use (P = 0.041) were independent factors for early readmission. Conclusion: Factors including a short hospital stay at first admission, a high disease activity index for intestinal Behçet's disease score, and steroid or opioid use were the independent prognostic factors for readmission within 3 months, which might help guide appropriate management strategies for hospitalized patients with intestinal Behçet's disease.
Key words: Intestinal Behçet's disease, readmission, prognostic factor
# P-0491
Adenoma recurrence rate after left- versus right-sided colectomy for colon cancer: Is there really a difference between the two operative methods?
Gee Young Yun, Hee Seok Moon, Ju Seok Kim, Sun Hyung Kang, Jae Kyu Sung and Hyun Yong Jeong
Department of Internal Medicine, Department of Gastroenterology, Chungnam National University School of Medicine, Korea
Background: Patients with a history of colonic resection for cancer have an increased risk for the development of metachronous malignant and premalignant lesions. Data on detection rates of premalignant lesions during colonoscopy surveillance in this setting are scarce; the most recent study was published in 2015. Fuccio et al. reported that patients who have undergone left-sided colectomy (LCR) are at higher risk for developing adenomas than those who have undergone right-sided colectomy (RCR). We tried to confirm the results of the previous study, assessing the risk for developing metachronous precancerous lesions in patients with previous colonic surgery for cancer according to the resection type. Methods: We retrospectively screened all consecutive patients who had undergone colonic surgery at Chungnam National University Hospital (CNUH) between September 2011 and April 2016. We enrolled 218 patients who had undergone LCR or RCR. Polyp, adenoma, and advanced adenoma detection rates (PDR, ADR, and AADR) were the main outcome measurements between the two groups. Results: A total of 218 patients were enrolled in the LCR and RCR groups (52 and 166 patients, respectively). In first surveillance colonoscopy, the PDR, ADR, and AADR in the LCR and RCR groups were 36.5%, 26.9%, and 5.8% and 31.3%, 26.5%, and 3.6%, respectively. In second surveillance colonoscopy, the PDR, ADR, and AADR in the LCR and RCR groups were 47.4%, 15.8%, and 5.2% and 36.6%, 31.7%, and 12.2%, respectively. In third surveillance colonoscopy, the ADR in the LCR and RCR groups was 20.0% and 27.8%, respectively. There was no significant difference between the two groups, for all of the above results. Conclusions: Based on our results, there was no significant difference in adenoma recurrence rate after LCR or RCR. Large prospective studies and surveillance programs should be performed according to the type of the colonic resection, with longer intervals for patients with previous RCR compared with those with previous LCR.
# P-0509
Trends in emergency department visits and hospitalization rates for inflammatory bowel disease: Results from a single-center in 2004, 2009, and 2014
Gunn Huh1, Hyuk Yoon2, Yoon Jin Choi2, Young Soo Park2, Nayoung Kim1,2 and Dong Ho Lee1,2
1Department of Internal Medicine, Seoul National University College of Medicine, Korea; 2Department of Internal Medicine, Seoul National University Bundang Hospital, Korea
Background: The use of biologics in inflammatory bowel disease (IBD) has increased recently. The aim of this study was to investigate the trends in IBD-related ED visits and hospitalization rates. Methods: Medical records of IBD-related visits in ambulatory department and ED at Seoul National University Bundang Hospital in 2004, 2009, and 2014 were reviewed. Demographics and clinical characteristics were compared. Multiple-variable regression analysis was used to identify significant risk factors for hospitalization. Results: The proportion of IBD patients who visited ED was 6.67% in 2004, 6.37% in 2009, and 6.24% in 2014. The mean age of them was 34.5 ± 14.0 years, and 70.7% of them were men. The most common chief complaints were abdominal pain (67.6%) in Crohn's disease (CD) patients and hematochezia (42.1%) in ulcerative colitis (UC) patients. The hospitalization rate from ED was 48.5% in CD patients and 50% in UC patients. Multiple-variable regression analysis showed that significant risk factors associated with hospitalization were disease duration less than 6 years (RR = 2.930, P = 0.039), leukocytosis (WBC > 10.0 × 103/μL) (RR = 2.710, P = 0.026) and elevated C-reactive protein (CRP > 1.0 mg/dL) (RR = 2.975, P = 0.014). Conclusion: The absolute number of IBD-related ED visits increased from 2004 to 2014, but there was no significant change in proportion of ED visits and hospitalization rates. Disease duration less than 6 years, leukocytosis, and elevated CRP were associated with hospitalization among IBD patients who visited ED.
# P-0532
Case series of colonic muco-submucosal elongated polyps in a single center in Taiwan: A comparison of clinical characteristics with previous reports
Yoen Young Chuah1,2, Ping I Hsu1, Wen Chi Chen1, Tzung Jiun Tsai1, Feng Woei Tsay1, Kung Hung Lin1, Sung Shuo Kao1, Yun Da Li1, Yeong Yeh Lee3 and Wei Chih Sun1
1Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan; 2Ping Tung Christian Hospital, Ping Tung, Taiwan; 3School of Medical Sciences, Universiti Sains Malaysia, Kota Bharu, Malaysia
Background/Aims: Colonic muco-submucosal elongated polyp (CMSEP) was first reported by Matake et al. in 1998. It is a distinctive non-neoplastic colorectal polyp characterized by pedunculated elongated shape mainly composed of normal mucosa and dense submucosa showing dilated blood and lymphatic vessels. Our study aimed to survey the clinical manifestations of CMSEPs in Taiwan and to compare our data with published reports of other Western and Eastern countries. Methods: From October 1980 to December 2016, patients with CMSEPs confirmed with histopathology from Kaohsiung Veterans General Hospital were retrospectively reviewed. Clinical characteristics of patients and distribution of CMSEPs and concomitant diseases were further analyzed. In addition, previously published case reports were derived from PUBMED/MEDLINE. Clinical characteristics of our patients with CMSEPs were compared with that of published reports. Results: A total of 27 patients (age range 39–82 years old, males 62.9%) were reviewed and their characteristics are shown in Table 1. Of these CMSEPs, sigmoid colon (52%) was the most common location. They were often asymptomatic and found incidentally during screening colonoscopy (40.7%). More than half of patients (51.9%) had no concomitant colonic diseases, but in those who had concomitant lesions, these were frequently adenoma (29.6%) There were 11 case reports/series from the East (largest series by Matake et al. in 1998) and 4 case reports/series from the West (largest series by Rola et al. in 2016) with a total of 58 cases. Comparatively, our results were closer to the Western data. Comparing East vs West, CMSEPs are predominant in males (60.3% vs 70.4%), more frequent in the sigmoid colon (34.5% vs 51.9%) and mostly found during screening exam (29.3% vs 51.9%). Conclusion: CMSEPs have distinctive but shared clinical characteristics in Taiwan and elsewhere in the world. The data in Taiwan are closer to the Western data probably because of introduction of screening colonoscopy.
| Case | Age (yr) | Sex | Symptoms | Polyp location | Polyp number | Polyp Size(mm) | Management | Concomitant colonic disease |
|---|---|---|---|---|---|---|---|---|
| 1 | 64 | M | Screening | Sigmoid | Multiple | 2–10 | Polypectomy | No |
| 2 | 57 | M | Screening | Sigmoid | Single | 13 | Polypectomy | No |
| 3 | 46 | M | Screening | Sigmoid | Single | 5 | Polypectomy | Adenoma |
| 4 | 60 | M | FOBT (+) | Sigmoid | Single | 9 | Polypectomy |
Adenoma Diverticulum |
| 5 | 58 | F | Diarrhea | Ascending | Single | 12 | Polypectomy | No |
| 6 | 63 | M | FOBT (+) | Sigmoid | Single | 12 | Polypectomy | Adenoma |
| 7 | 53 | F | FOBT (+) | Sigmoid | Multiple | 3–15 | Polypectomy | No |
| 8 | 68 | M | FOBT (+) | Descending | Single | 5 | Polypectomy | No |
| 9 | 64 | F | FOBT (+) | Sigmoid | Multiple | 6–7 | Polypectomy | No |
| 10 | 78 | M | Diarrhea | Sigmoid | Single | 8 | Polypectomy | No |
| 11 | 52 | M | Diarrhea | Sigmoid | Single | 9 | Polypectomy | Adenoma |
| 12 | 62 | M | Screening | Transverse | Single | 13 | Polypectomy | Diverticulum |
| 13 | 50 | F | Screening | Transverse | Single | 8 | Polypectomy | No |
| 14 | 39 | M | Screening | Sigmoid | Single | 6 | Polypectomy | No |
| 15 | 82 | F | AP | Sigmoid | Single | 20 | Polypectomy | No |
| 16 | 70 | M | FOBT (+) | Transverse | Single | 5 | Polypectomy | Adenoma |
| 17 | 71 | F | Screening | Sigmoid | Single | 10 | Polypectomy | Diverticulum- |
| 18 | 65 | M | FOBT (+) | Sigmoid | Single | 4 | Polypectomy | Adenoma |
| 19 | 76 | M | Bloody stool | Sigmoid | Single | 12 | Polypectomy | Adenocarcinoma |
| 20 | 69 | M | Screening | Cecum/ascending | Multiple | 4/8 | Polypectomy | No |
| 21 | 67 | F | Screening | Transverse | Single | 10 | Polypectomy | Adenoma |
| 22 | 52 | M | Tarry stool | Descending | Single | 15 | Polypectomy | No |
| 23 | 54 | M | Tarry stool | Cecum | Multiple | 13/15 | Polypectomy | No |
| 24 | 72 | F | Screening | Ascending | Single | 6 | Polypectomy | Diverticulum |
| 25 | 66 | M | Tarry stool | Transverse | Single | 12 | Polypectomy | Adenoma |
| 26 | 73 | F | Screening | Rectum | Single | 7 | Polypectomy | No |
| 27 | 59 | F | Abdominal pain | Transverse | Single | 11 | Polypectomy | Diverticulum |
- M, male; F, female; FOBT, fecal occult blood test.
# P-0552
Awareness survey of inflammatory bowel disease for Korean high school students
Byung Ik Jang, Che Eun Lim, Dah Gun Lee, Jeoung Hye Lee, Yu Na Lee, Jeoung Eun Lim and Crohn's and Colitis Association In Daegu-Gyeongbuk (Ccaid)
Hyehwa Girl's High school, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
Purpose: To investigate the knowledge and awareness level of inflammatory bowel disease (IBD) and changing awareness of the disease among high school students. Methods: We explained the purpose of the study to 310 female high school students and presented them with a 20-item questionnaire on the awareness level of IBD. The questionnaire-response data were reorganized based on individual questions to determine the current trends in the awareness of Crohn's disease (CD) and ulcerative colitis (UC). Results: Among the included students, only 23% of participants were aware of IBD (UC: 25% and CD: 20%). Awareness of the disease or knowledge of the disease name was via the internet and newspaper (UC: 14% and CD: 12%) and TV (UC: 11% and CD: 10%). Awareness of IBD was absent in most of the participants (UC: 63% and CD: 69%). The rate at which participants could explain UC and CD was 8% and 7%, respectively. Only 18% of participants could differentiate between IBD and IBS, whereas the remaining 72% were confused between the disease and illness. Participants were aware that the incidence of IBD was increasing due to excessive stress (31%) and westernized eating habits (20%). Conclusions: Results of the questionnaire-survey on high school students in Korea indicated a low knowledge and awareness level of IBD such as UC and CD. Public education and strategies to improve awareness of IBD are necessary. In addition, more effort is needed to improve IBD awareness based on efficient methods of promotion and education.
# P-0576
Cancer surveillance in inflammatory bowel disease: A single-center experience
Hang Hoi Michael Wong and Ying Ki Shirley Tze
Department of Medicine and Geriatrics, United Christian Hospital, Hong Kong
Background: Surveillance colonoscopy program aims to reduce morbidity and mortality due to CRC. The overall incidence of inflammatory bowel disease (IBD)-associated CRC has been diminishing in recent decades in western countries; in contrast, the incidence in Asia is still rising. Therefore, we aim to perform an observational study to raise awareness of the importance of cancer surveillance in IBD. Methods: We conducted a retrospective observational study on all our patients (total numbers: 242) suffering from IBD to determine whether they are being risk stratified and receiving their screening colonoscopy and ongoing surveillance. The extent of their disease, the year of diagnosis, screening colonoscopy, subsequent surveillance, and their risks of developing colonic neoplasm were reviewed. Results: Among the total 140 (59%) UC patients and 102 (41%) CD patients, 112 had the diagnosis of IBD made after year 2008; that is, they do not require screening colonoscopy yet. In the remaining 130 patients, 84 (65%) received screening colonoscopy and 46 (35%) did not receive screening colonoscopy. Comparing the two groups, 1 patient died from non-IBD-related cause in the screening group, whereas 8 patients died in the non-screening group. Among these 8 patients, one died from colorectal cancer and 2 died from other IBD-related causes. Risks stratification was inadequately performed in our hospital. Despite all high-risk cases that offered cancer surveillances, the moderate and low risk groups were not clearly identified. Conclusions: The CRC risk is considered to be high among patients with IBD. And as the incidence of CRC is rising among this group in Asia, gastroenterologists are obligated to stratify their risks in developing colorectal cancer and perform surveillances accordingly.
# P-0596
Colonic MALToma, clinical data and result of treatment in single center
Dong Hwahn Kahng, Moo Song Jeon, Sang Gyu Park, Young Joo Park, Dong Hoon Baek and Geun Am Song
Department of Internal Medicine and Gastroenterology Division, Pusan National University School Of Medicine, Korea
Background: Colonic mucosa-associated lymphoid tissue lymphomas (MALToma) are rare, and the treatment has not been established definitively. Colonic MALToma is a slow growing malignancy with rare recurrence following treatment, so the prognosis is known to generally good. This report investigated the clinical results following treatment in patients who diagnosed with colonic MALToma in a single center. Methods: From January 2003 to June 2014, colonoscopy were performed in 6 consecutive patients with diagnosed colonic MALToma in a single medical center and mean follow-up period was 73.6 months (range; 33–142 months). All patients were histologically diagnosed, including biopsy, endoscopic mucosal resection (EMR), or endoscopic mucosal dissection (ESD), and treated by chemotherapy alone or radiotherapy alone. Results: Of 6 patients, 1 patient was Ann Arbor stage IE, and IIE and IV are 3 and 2 patients, respectively. Colonic MALTomas were located in cecum (1), IC valve (1), ascending colon (1), transverse colon (2), and rectum (1). Two patients had double lesions, such as small bowel and ascending colon and stomach and transverse colon, respectively. Treatments were chemotherapy (5) and radiotherapy (1). Among 5 patients who received chemotherapy, 2 patients were recurred so they had to receive additional chemotherapy. Conclusion: Colonic MALToma should be evaluated properly because the prognosis depends on a set of severe factors, including stage of tumor, age, tumor size, involvement of vital organs, or surgical resectability , although many MALToma patients have long survival and most lesions are located in single area.
# P-598
Family History of Gastric Cancer is Associated with the Risk of Colorectal Neoplasia
Yoon Suk Jung
Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Korea
Background and Aim: Family history of colorectal cancer (CRC) is an important risk factor for colorectal neoplasia (CRN). However, family history of cancer at other sites may also be associated with CRN risk. We aimed to investigate CRN risk according to family history of cancers at 12 different sites, including stomach, esophagus, liver, biliary system, lung, thyroid, prostate, breast, ovary, endometrium, and uterine cervix, as well as colorectum. Methods: A cross-sectional study was performed on 139,497 asymptomatic examinees who underwent colonoscopy as part of a health check-up. Results: The mean age of the study population was 41.6 and the prevalence of CRN was 16.3%. Multivariate analyses revealed that family histories of CRC (adjusted odds ratio [AOR] 1.26; 95% confidence interval [CI] 1.17-1.35) and gastric cancer (AOR 1.07; 95% CI 1.01-1.13) were independent risk factors for CRN. Notably, the risk of CRN increased even more for participants with family histories of both CRC and gastric cancer (AOR 1.38; 95% CI 1.12-1.70). Family history of CRC was associated with risk of CRN in participants aged both <50 and ≥50, whereas family history of gastric cancer was associated with risk of CRN in participants aged <50 (AOR 1.22; 95% CI 1.14-1.30), but not in participants aged ≥50 (AOR 1.08; 95% CI 0.99-1.18). Conclusions: Family history of gastric cancer was an independent risk factor for CRN, especially in those aged <50. Persons with family histories of gastric cancer and CRC, especially those with family histories of both, may need to begin colonoscopy earlier.
# P-0622
Histological remission with probiotics alone in ulcerative colitis
Huiyu Lin and Wee Chian Lim
Tan Tock Seng Hospital, Singapore
Introduction: Intestinal microflora imbalances are thought to play a role in the inflammatory process of ulcerative colitis (UC), and there is increasing interest in modulating gut bacterial composition with treat UC. Probiotics have been reported as effective adjunctive therapy in mild-moderately active UC. However, data are lacking on the role of probiotics alone in the induction and maintenance of remission in UC. We report 2 cases of UC patients who achieved and maintained clinical, endoscopic, and histological remission on probiotics without concomitant standard therapy. Methods: Electronic records of 125 (56% Chinese, 23% Indian, 12% Malay, and 9% others) UC patients followed up at our center from 2002–April 2017 were retrospectively reviewed. Most patients were on standard therapy (aminosalicylates, thiopurines, and biologics). Two swapped from conventional treatment to probiotics alone. Results: Case 1: A 34-year-old Chinese male with left-sided UC (diagnosed 2012) was clinically stable on sulfasalazine (SSZ) 1–1.5 g/d only. Medication non-compliance resulted in a mild flare (July 2014). Colonoscopy demonstrated active proctosigmoiditis despite restarting medications. He responded well to intensified therapy: SSZ 2 g/d, mesalamine suppository (0.5 g/d) and VSL#3 (112 billion/d) but subsequently discontinued all medications (April 2016) and suffered another flare (September 2016: stool-calprotectin 380). He commenced Progut 1 cap tds (combination Lactobacillus, Bifidobacterium, and Streptococcus) with good response (stool-calprotectin < 30). Colonoscopy (April 2017) showed normal colonic mucosa (Mayo score 0); histology was consistent with quiescent UC. Case 2: A 66-year-old Chinese female diagnosed with mild extensive UC (February 2016) was started on prednisolone but was unable to tolerate SSZ (drug-induced rash) nor azathioprine (gastrointestinal side effects). Progut 1 cap bd was initiated, and she achieved and maintained steroid-free remission. Colonoscopy (December 2016) demonstrated normal mucosa throughout the colon; histology showed quiescent chronic colitis. Conclusion: Probiotic monotherapy may be effective in inducing and maintaining clinical, endoscopic, and histological remission in UC patients with mild disease. This observation should be confirmed with larger studies.
# P-0623
Intestinal amebiasis mimicking ulcerative colitis in a 33-year-old Filipino female: A case report
Dan Karlo Esquera1, Vanessa Mahrie Madayag2 and Danilo Valencia3
1Main Author, Senior Resident/Third Year Resident/Hospitalist, Department of Internal Medicine, Iloilo Mission Hospital, Iloilo City, Philippines; 2First Year Training Resident, Department of Internal Medicine, Iloilo Mission Hospital, Iloilo City, Philippines; 3Internist-Gastroenterologist, Department of Internal Medicine, Iloilo Mission Hospital, Iloilo City, Philippines
Background/Introduction: Amebiasis is a ubiquitous parasitic infection affecting 10% of the world's population causing more deaths every year (100 000 deaths). Most individuals are asymptomatic. Symptoms may last for years and may mimic ulcerative colitis. Methods: Fecalysis, colonoscopy with Biopsy. Results/Case Description: We present the case of a 33-year-old Filipino female with the history of bloody stool and was managed as case of amebiasis 8 months prior to admission (PTA). However, patient had recurrence of bloody stool on 2 weeks PTA. Digital rectal exam on admission revealed blood and mucoid on examining finger without mass or hemorrhoid. Work ups revealed Entamoeba histolytica and coli cyst on fecalysis. Colonoscopy with biopsy showed severe inflammation with cobblestone formation and chronic severe non-specific colitis on Biopsy. She was managed with metronidazole, ciprofloxacin, and 5-amino salicylic acid. Patient's recovery was uneventful and was discharge improved. Discussion: Amebiasis can exacerbate symptoms of ulcerative colitis. Inadequate mucosal immune response on the intraluminal antigenic components is essential in UC pathogenesis. UC is an immune-mediated chronic intestinal condition that usually involving the rectum and extending to colon. Incidence estimates 0.1–6.3 per 100 000, while prevalence rate 4.9–168.5 per 100 000 in Asia. Stool exam and culture methods are often unrewarding for diagnostics. Colonoscopy can be performed either to diagnose amebiasis or to exclude other causes. The pathological diagnosis of UC is often difficult because biopsy material may not contain pathognomic features. The best way for reliant diagnosis is multidisciplinary approach including clinical history, colonoscopic findings with biopsy, radiology, and relevant serology. Conclusion: This case report is presented since we believe that this could raise awareness among medical practitioners of amebiasis that could precipitate ulcerative colitis. It is very important to consider UC to regions with prevalence of amebiasis.
# P-0641
Abiotrophia defectiva: A rare gut pathogen resulting endocarditis in inflammatory bowel disease
Yu Jun Wong1, Bee Xian Tan2 and Brian John Schwender1
1Department of Gastroenterology and Hepatology, Singapore General Hospital, Singapore; 2Department of Pathology, Singapore General Hospital, Singapore
Clinical History: A 44-year-old man has ulcerative colitis (UC) for the last 3 years on maintenance twice daily oral mesalazine 2 g. Five months ago, investigation showed that his UC was in deep remission (clinical, endoscopic, and histological). A month prior to admission, his C-reactive protein (CRP) start to rise (39.8 MH/L from baseline of 1.8 MG/L). Computer tomography of abdomen and pelvis excluded intraabdominal collections, abscesses, or colitis. Incidental finding include a subcentimeter hypoattenuation area at left kidney. One month later, he was admitted for rectal bleeding with non-specific abdominal discomfort. He had no risk factors for endocarditis including prior valvular heart disease, central catheter insertion, or intravenous drug abuse. Investigation: Raise CRP (87.3 MG/L) and leucocytosis (16 × 109/L) was noted. Blood and stool cultures as well as Clostridium difficile PCR were negative. He was treated as mild UC flare. Differential Diagnosis: Mild UC flare and endocarditis. Progression: His stool calprotectin was 73 ug/g on arrival. At the same time, a new ejection systolic murmur was detected on admission. Transesophageal echocardiography showed multiple mitral valve vegetations. Repeated blood cultures grew Abiotrophia defectiva after 53 hours of incubation. Dental review excluded oral pathology. Following diagnosis of A. defectiva endocarditis, he completed 4 weeks of intravenous benzylpenicillin and gentamicin. No further embolic or cardiac complications after 3 months of follow up. Learning Point of This Case: A. defectiva, a gut pathogen, can cause subacute endocarditis in UC. Adequate blood sample and incubation period is required to detect this fastidious organism. It is associated with high morbidity and relapse despite appropriate treatment. Conclusion: A. defectiva, a rare gut pathogen, can result in subacute endocarditis, mimicking UC flare. More data on incidence of endocarditis among UC is required to guide the role of prophylactic antibiotic among UC patients undergoing endoscopy.
# P-0646
Sera with anti-enteric neuronal antibodies from irritable bowel syndrome patients promote neuronal apoptosis
Wenjuan Fan1, Guijun Fei1, Yongzhe Li2, Chaojun Hu2, Xiaoqing Li1, Haiwei Xin1, Zhu Liming1 and Xiucai Fang1
1Department of Gastroenterology; 2Department of Rheumatology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, 100730, China
Background and Aim: Previous studies found that the positive rate of anti-enteric neuronal antibodies (AENA) in sera of irritable bowel syndrome (IBS) patients was higher than that in healthy subjects (HS). The aim of this study is to demonstrate whether AENA positive sera from IBS patients promote apoptosis of enteric neurons and human neuroblastoma cells (SH-Sy5Y). Methods: Sera AENA were detected with indirect immunofluorescence (IR) for IBS patients who met Rome III criteria. Myenteric neurons from guinea pigs and SH-Sy5Y cells were cultured for 4 days and incubated with fetal bovine serum (FBS), sera from HS or IBS patients with AENA negative, mild positive, positive, and intensive positive. The apoptosis was detected by IR with anti-PGP9.5/TUNEL/DAPI, anti-PGP9.5/anti-cleaved caspase3/DAPI for myenteric neurons, Western blot to examine the expression of cleaved caspase3, bax and bcl-2, and flow cytometry (annexin V-FITC/propidium iodide staining) for SH-Sy5Y cells. Results: After incubation with AENA positive, intensive positive sera of IBS patients and the percentage of TUNEL positive staining were significantly higher than FBS and HS groups (6.2% ± 2.0% and 10.2% ± 4.6% vs 0.5% ± 0.5% and 1.3% ± 1.9%, n = 6 in each group, all P < 0.05); the percentage of cleaved caspase3 positive staining in AENA positive and intensive positive groups were 20.0% ± 7.3% and 35.0% ± 13.3%, which were higher than AENA negative, FBS, and HS groups (4.9% ± 2.1%, 0.9% ± 0.4%, and 4.3% ± 1.5%, all P < 0.05). In AENA positive and intensive positive groups, the expressions of cleaved caspase3, bax were higher and bcl-2 was lower than other groups (P < 0.05). Flow cytometry showed the percentage of apoptotic cells were higher in AENA positive and intensive groups than other groups (all P < 0.05). Conclusions: Sera with AENA positive and intensive positive from IBS patients promote enteric neurons and SH-Sy5Y cells apoptosis in vitro, which indicate sera AENA might target enteric neurons and induce neuronal apoptosis.
Key words: irritable bowel syndrome, anti-enteric neuronal antibody, apoptosis [Support by grant 2014DFA31850]
# P-0667
RhoA: The key signaling pathway of microRNA-126 in suppressing the epithelial–mesenchymal transition, proliferation, migration, and invasion of colorectal cancer cells
Ming-Yu Huang1,2, Wei Yuan1,2, Shuai Wu1,2, Zhao-Hua Shen1,2, Zhen-Yu Yang1,2, Yong-Sheng Quan1,2, Chang-Xin Zhu1,2, Kai Tang1,2 and Xiao-Yan Wang1,2
1Department of Gastroenterology, The Third Xiangya Hospital of Central South University, Changsha, Hunan, China; 2Hunan Key Laboratory of Nonresolving Inflammation and Cancer, Changsha, Hunan, China
Background: Previously, we found that microRNA-126 (miR-126) was significantly down-regulated in human colorectal cancer (CRC) tissues and negatively related with patient's prognosis. MiR-126 was also low-expressed in high metastatic CRC cell lines and inhibited proliferation, invasion, and metastasis of CRC in vitro. Additionally, miR-126 down-regulated Ras homologue A (RhoA) activity in CRC cells. However, whether miR-126 regulates the process of epithelial–mesenchymal transition (EMT) in CRC and whether RhoA activity and RhoA signaling pathway play an important role in the functions of miR-126 in CRC remain unclear. Therefore, we aimed to identify RhoA signaling pathway associated with the functions of miR-126 in EMT, proliferation, migration, and invasion of CRC cells. Methods: Constructed CRC cell lines of miR-126 over-expression or knockdown. Performed MTT, colony formation, wound healing, migration, invasion assays and RT PCR, Western blot analysis to study the functions of miR-126 in EMT, proliferation, migration, invasion, and expression RhoA signaling pathway of CRC cells. Constructed pDsRed2-V14RhoA (constitutively active RhoA, V14RhoA) and pDsRed2-N19RhoA (domain-negative, N19RhoA) mutants then transfected them into the CRC cell lines of miR-126 over-expression or knockdown to restore RhoA activity. Pull-down assay detected RhoA activity after transfected and then repeated the experiments above to investigate the biological behavior changes of CRC cells. Results; MiR-126 promoted the expression of E-cadherin and suppressed the expression of SLUG, Snail, Vimentin, and Fibronectin of CRC cells. MiR-126 also inhibited proliferation, migration, and invasion of CRC cells and negatively regulated RhoA signaling pathway. V14RhoA effectively increased RhoA activity and reversed the role of miR-126 by promoting EMT, proliferation, migration, and invasion in miR-126 over-expressing HCT116 cells. Conversely, N19RhoA effectively decreased RhoA activity and suppressed EMT, proliferation, migration, and invasion in miR-126-silenced SW480 cells. Conclusion: RhoA signaling pathway was the key signaling pathway of miR-126 in suppressing the EMT, proliferation, migration, and invasion of CRC cells.
# P-0677
Negative effects of Bifidobacterium bifidus on the rat with colonic visceral hypersensitivity induced by acetic acid perfusion
Xin Wang, Weifang Zhang, Kun Wang, Lu Zhang, Qinghua Sun and Liping Duan
Department of Gastroenterology, Peking University Third Hospital, Department of Pharmacology, Peking University Health Center
Backgrounds: Bifidobacterium with appropriate doses has been suggested to reduce the visceral hypersensitivity in IBS. But different treatment effects have been reported. Aims: To study the effects of gavage administration with Bifidobacterium bifidus for two weeks on the visceral hypersensitivity of rats. Methods: colonic visceral hypersensitivity (CVH) was induced by colonic injection of 0.5% acetic acid (AA) in 10-day-old rats, while control (NS) induced with 0.9% NaCL. The (AWR), induced by colorectal distention (CRD), were used to quantify the level of colonic sensitivity in adult rats. The CVH rats in 42-day-old were treated by gavage administration with Bifidobacterium bifidus (1*109 CFU/day) for two weeks (CVH-Bifi). Other CVH rats were treated with 0.9% NaCL (CVH-NS). A group of control with normal sensitivity was treated with sham gavage (Con-sham). In day 56th, another AWR was assessed, and the hippocampus and prefrontal cortex (PFC) were separated and used to analyze the c-fos, NMDAR 2A, and NMDAR2B with Western-blot. Results: After two-week gavage, the CVH-Bifi presented lower volume than that of CVH-NS in CRD, though without statistical difference (2.35 ± 0.28 vs 2.40 ± 0.64, P = 0.11). No significant difference was found between CVH-Bifi and Con-sham as well. In hippocampus, c-fos of CVH-Bifi was higher than that of Con-sham (0.77 ± 0.23 vs 0.31 ±0.08, P = 0.032) and CVH-NS (0.77 ± 0.23 vs 0.48 ± 010, P = 0.171). The NMDAR2A of CVH-Bifi was higher than that of Con-sham (1.04 ± 0.22 vs 0.51 ± 0.16, P = 0.055). In PFC, the NMDAR2A in CVH-Bifi was significantly higher than that of CVH-NS (0.63 ± 0.14 vs 0.21 ± 0.05, P = 0.004) and Con-sham (0.63 ± 0.14 vs 0.20 ± 0.07, P = 0.011). Conclusions: We reported a negative effect of Bifidobacterium bifidus gavage, which induced higher activation of c-fos and higher expression of NMDAR 2A in hippocampus and PFC. The roles of Bifidobacterium bifidus and its metabolites on visceral sensitivity need further study for clarifications.
# P-0681
Evaluation of the blood-based Nu.QTM Colorectal Cancer Screening Triage Test to identify individuals at low risk of CRC in an independent Taiwanese cohort of 383 average risk subjects
M Herzog1, D Pamart1, Han-Mo Chiu2, Li-Chun Chang2, M Eccleston1, B Cuvelier1, E Josseau1, J Micallef1 and J Terrell1
1Belgian Volition SPRL, Isnes, Belgium; 2Department of Internal Medicine, National Taiwan University Hospital, Taiwan
Background: The success of stool-based screening for CRC adopted across Europe has placed significant strain on colonoscopy capacity. Immunohistochemistry studies show genome-wide epigenetic changes in the chromatin of cancer tissue and have identified histo-oncoproteins–histone modifications and other epigenetic changes linked to cancer. Nucleosome bound DNA fragments contain mutations found in cancer tissue suggesting a tumor chromatin origin for, at least some, circulating nucleosomes. Profiling global levels of epigenetic alterations in circulating nucleosomes can provide disease specific diagnostic information. The aim of the study was an evaluation of a CE marked (European Conformity) IVD (Invitro Diagnostic), the Nu.QTM CRC Screening Triage Test in an independent cohort of 383 average risk subjects in Taiwan. Methods: Blinded serum samples taken from FIT positive individuals who participated in the population CRC screening in Taiwan were analyzed (10 μL in duplicate) for circulating nucleosomes containing methylated DNA (normalized to global level of circulating nucleosomes) using the Nu.QTM CRC Screening Triage Test. Results: The Nu.Q CRC Triage test was designed to save at least 20% of colonoscopies with a minimal cancer sensitivity of 90%. Evaluation of these data in the Taiwanese population will be presented. Please note: Evaluation of the product in a further independent study of 4000 FIT+ve individuals will be presented at the DDW meeting in Chicago, May 2017. Conclusions: Stool screening for CRC is widely adopted across European and other countries with proven reduction in mortality but can place significant strain on limited colonoscopy capacity. Combining a single, age adjusted Nu.QTM blood score with FIT score could reduce unnecessary colonoscopies in FIT+ve individuals with minimal reduction in sensitivity. Screening throughput and overall detection of CRC and high-risk adenomas could therefore be increased where colonoscopy capacity is a limiting factor. This approach could provide an affordable, accessible approach to improve stool-based screening capacity ultimately detecting more early-stage cancers and saving lives.
# P-0689
Pulmonary complications of ulcerative colitis successfully treated with salazosulfapyridine without steroids
Shogo Magome, Takahito Takezawa, Masahiro Okada, Hisashi Fukuda, Haruo Takahashi, Yuji Ino, Hirotsugu Sakamoto, Yoshimasa Miura, Yoshikazu Hayashi, Tomonori Yano, Keijiro Sunada, Alan Kawarai Lefor and Hironori Yamamoto
Department of Medicine, Division of Gastroenterology, Jichi Medical University, Japan
Introduction: Lung parenchymal lesions are rare complications of inflammatory bowel disease (IBD) and generally respond well to steroid therapy. We treated a patient with ulcerative colitis (UC)-related lung parenchymal lesions that resolved using salazosulfapyridine without steroids. Case: An 18-year-old man was diagnosed with UC one year prior to presentation and was treated with mesalazine 3.6 g/day and azathioprine 75 mg/day. He went to a local hospital with chest pain and fever. Chest X-ray and computed tomography (CT) showed multiple bilateral lung nodules. They were thought to be infectious in origin because they partially resolved with antibiotic therapy. Two months later, he developed a cough for two weeks. CT scan showed multiple bilateral lung nodules with cavitation. In addition, the serum proteinase-3 anti-neutrophil cytoplasmic antibody (PR3-ANCA) level was elevated. Since empiric treatment with broad-spectrum antibiotics did not resolve the symptoms, granulomatosis with polyangitis (GPA) was suspected, and he was transferred for further evaluation. Further studies did not suggest GPA, but colonoscopy revealed active UC, and pulmonary complications of UC suspected. The patient was treated with 8.0 g/day of salazosulfapyridine switching from mesalazine combined with the same dose of azathioprine because he refused steroid therapy. After six days, one of the nodules partially resolved on X-ray, and the activity of UC gradually resolved. All nodules disappeared five months after starting salazosulfapyridine. UC-related lung parenchymal lesions are rare and poorly understood. This patient illustrates that resolution of UC can lead to improvement in UC-related lung parenchymal lesions.
# P-0697
Utility of azathioprine metabolites measurement in management of inflammatory bowel diseases: A real-life and single-center experience in Malaysia
Nik Nuratiqah Nik Abeed1, Rafiz Abdul Rani2, Thevaraajan Jayaraman2, Zhiqin Wong1, Ngiu Chai Soon1, Norfilza Mohd Mokhtar3 and Raja Affendi Raja Ali1
1Gastroenterology Unit, UKM Medical Centre, Kuala Lumpur, Malaysia; 2Gastroenterology Unit, Faculty of Medicine, Universiti Teknologi MARA, Selangor, Malaysia; 3Department of Physiology, UKM Medical Centre, Kuala Lumpur, Malaysia
Background: Inflammatory bowel disease (IBD) either ulcerative colitis (UC) or Crohn's disease (CD) is increasing in Malaysia. Azathiopurine (AZA) remains the mainstay therapy, and measuring its metabolites, 6-thioguanine nucleotide (6-TGN) and 6-methyl mercaptopurine (6-MMP), is thought to be useful in guiding therapy for IBD patients. We aimed to determine correlation between AZA metabolites with disease activity and guide us to optimally treat patients. Methods: A cross-sectional study of IBD patients and its metabolites-directed algorithm was used to guide the treatment strategy. Harvey Bradshaw index (HBI) score was used to assess pre- and post-treatment. Results: 40 IBD patients [16 UC, 24 CD; 25 males, 15 females) with median of 13 (11.25–24.00) months on stable AZA dose of 1.70 mg/kg/day (1.31–2.07) were recruited. The median 6-TGN and 6-MMP levels were 250.5 (228.5–419.5) and 1127 (922.2–1459.0) pmol/8 × 108 RBC respectively with HBI score of 5.5 (4–8). The 6-TGN level showed negative correlation with HBI score (r = −0.5, P = 0.001) and high 6-TGN levels at 301.56 (IQR; 246–847 pmol/8 × 108 RBC; P = 0.012) kept the disease in remission. Based on metabolites-directed algorithm, 20 patients were in appropriate dose (16 maintain dose and 4 switch to biologics); 12 patients under-dose (7 increase dose, 4 maintain dose, and 1 switch to biologic); 8 patients were thiopurine refractory or overdose (3 reduce dose, 4 maintain dose, and 1 switch to biologic), and none was thiopurine resistant or non-compliant. Post-treatment strategies of HBI score showed statistically significant (P = 0.009). Conclusions: Utilizing the azathioprine metabolites, particularly 6-TGN, is useful in guiding treatment strategies in the management of IBD patients.
# P-0704
Knowledge, attitude, practice, and awareness towards colorectal cancer screening among primary care physicians at the major public teaching hospitals in Malaysia
Mohd Fairul Limun1, Rafiz Abdul Rani2, Wong Zhiqin1, Ngiu Chai Soon1 and Raja Affendi Raja Ali1
1Gastroenterology Unit, Department of Medicine, UKM Medical Centre; 2Gastroenterology Unit, Department of Medicine, Universiti Teknologi Mara (UiTM)
Background: In Malaysia, colorectal cancer (CRC) is commonest cancer for men and second commonest cancer for women. Despite that, CRC screening uptake among Malaysians is still very poor. Primary care physicians (PCPs) are believed to be fundamentally important to influence patients to undergo screening test. So far, little is known about the knowledge, attitude, practice, and awareness towards CRC screening among PCPs in Malaysia. Therefore, we aim to explore these issues in relation to CRC screening among PCPs in major public teaching hospitals in Malaysia. Methods: We conducted a cross-sectional study from October 2016 to December 2016 at 5 major public teaching hospitals (UKM, UM, USM, UiTM, and UPM) in Malaysia. Validated questionnaires were adopted from research program, National Cancer Institute, USA, and given to PCPs to assess their knowledge, attitude, practice, and awareness towards CRC screening. Results: A total of 70 PCPs were participated in this study. Out of 70 PCPs, 68 (97.1%) have good awareness, 51 (72.9%) have positive attitude, and only 39(56%) have average knowledge towards CRC screening. A total of 39 (55.7%) of PCPs were admitted to follow CRC screening guidelines and recommendations in their daily clinical practice. However, only 40 (58.6%) of PCPs were admitted to practice the various modalities of CRC screening tests. The absence of national CRC screening test policy along with the shortage of endoscopic provider were the significant factors that limit the practice of CRC screening among PCPs (x2 = 16.963, P < 0.001 and x2 = 4.062, P = 0.044). Conclusions: Primary care physicians in major public teaching hospitals in Malaysia have average knowledge, positive attitude, and practice as well as good awareness towards CRC screening.
# P-0713
Clinical characteristics and long-term prognosis of elderly-onset Crohn's disease
Eun Mi Song1, Sun-Ho Lee1, Kiju Chang1, Ho-Su Lee2, Sangyoung Yi1, Sun Jin Lee3, Soo Jung Kim4, Euiyoun Kang4, Sung Wook Hwang1,4, Sang Hyoung Park1,4, Dong-Hoon Yang1, Jeong-Sik Byeon1, Seung-Jae Myung1, Suk-Kyun Yang1,4 and Byong Duk Ye1,4
1Department of Gastroenterology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea; 2Department of Biochemistry and Molecular Biology, University of Ulsan College of Medicine, Seoul, Korea; 3Department of Nursing, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea; 4Inflammatory Bowel Disease Center, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea
Background and Aims: Clinical characteristics and long-term prognosis of elderly-onset Crohn's disease (EOCD) in Asians are still unclear. Methods: We identified 29 EOCD patients (diagnosed with CD in age older than 60 years) out of 2989 CD patients (0.97%) from the IBD registry of Asan Medical Center. After excluding two patients with unclear data on the interval between symptom onset to CD diagnosis, 27 EOCD patients were matched with 108 non-elderly-onset CD (NEOCD) patients diagnosed in age between 15 and 25 years (1:4) for interval from symptom onset to diagnosis (± 3 years) and follow-up duration (± 3 years). Results: Median age at diagnosis of CD in EOCD and NEOCD group was 64.7 years (range, 60.0–74.8) and 20.4 years (range, 15.0–25.0), respectively. Female sex was predominant in EOCD group compared to NEOCD group (59.3% vs 29.6%, P = 0.008). The most common Montreal disease location at CD diagnosis in EOCD group was L1, whereas L3 was most common in NEOCD group (L1, L2, and L3; 63.0%, 3.7%, and 33.3% in EOCD group and 17.8%, 2.8%, and 79.4% in NEOCD group, respectively, P < 0.001). Patients with active and/or past perianal fistula at CD diagnosis were less common in EOCD group (14.8% vs 49.1%, P = 0.003). Thiopurines were less often used in EOCD group (hazard ratio [HR] 0.323; 95% confidence interval [CI] 0.177–0.587; P < 0.001). During follow-up (median 5.86 years), risk of behavioral progression and intestinal resection of EOCD group was comparable with those of NEOCD group (HR, 0.378; 95% CI, 0.099–1.452; P = 0.157 and HR, 1.471; 95% CI, 0.723–2.994; P = 0.287, respectively). In multivariate analysis, the disease behavior and the presence of perianal fistula at diagnosis were significant associated factors with intestinal resection, but not the EOCD. Conclusions: EOCD group showed a female predominance and a higher proportion of isolated ileal involvement as well as less frequent perianal fistula at diagnosis. Clinical course appears to be similar between EOCD and NEOCD groups.
Keywords: Crohn's disease, aged, geriatrics, prognosis
# P-0734
Management of irritable bowel syndrome: A clinical challenge
Sudheendra A Deshpande1 and S Vasudha2
1Medical Director, Divya Jyothi Clinic, Ananta Research Foundation; 2Associate, Divya Jyothi Clinic, Ananta Research Foundation
Introduction: Irritable bowel syndrome has been a big challenge in the clinical practice of present times. By the sheer vagaries involved in its presentation, the management of the same involves multipronged strategy. The typical irritative symptoms such as bouts of stomach cramps, bloating, diarrhea, constipation subsequent to certain foods or anxiety/stress lead to discomfort, which seldom subside on its own. Around twice as many women are affected as men. The prevalence estimates usually range from 12–30%2, 3 and may vary significantly between countries and depend on the diagnostic criteria used.4, 5 The prevalence of IBS varies across the world, ranging from as high as 10–20% in the West,6, 7 to as low as 4.2% in India.8Across Asia, it has been noted that the prevalence of IBS is higher in the younger age group.9, 10 Methodology: The selection of patient has been in the age group of 20–60 yrs. The co-morbids suffered in the patients varied from neuro-related, obesity, thyroid dysfunction, renal dysfunction, and so on, verified with periodical investigations. Results and Discussion: Although the symptoms of IBS ease after going to the wash room and opening your bowels, it is typical in its recurrence after subsequent intake of food. This disorder is very much capable of being a direct or indirect causative factor for many chronic disorders. The quality of life (QOL) is badly affected in the patients suffering with IBS having an impact on their productivity at the work place.11 This complex clinical situation needs a more comprehensive management strategy, which is safe and long lasting. There have been appreciable results with the adoption of an integrative approach in the management of IBS. The adoption of Ayurveda with its oral effective herbal formulation as a conventional therapy has yielded encouraging results. A total of 30 patients screened, of which 19 (63.33%) were females and 11 (36.67%) were males were subjected for the Ayurveda Conventional Therapy (ACT). The patients belong to different categories with IBS as a primary complaint and also IBS as a precursor (remained untreated/improperly or incompletely treated) or secondary to many of the chronic disorders such as osteoarthritis, proteinuria, diabetes mellitus, hypertension, and thyroid dysfunction. The ACT included the medicine, diet, and lifestyle change (MDLC), providing a long lasting relief in most of the patients. Among the patients with IBS as the primary complaint in 63.16% females (12 out of 19) and in 62.64% males (7 out of 11), they were subjected to ACT for 12 weeks, and there was clinical improvement in the symptoms up to 98%. In the patients with IBS as secondary complaint, in 36.84% females (7 out of 19) and in 36.36% males (4 out of 11), they were subjected to ACT for 12 weeks, which showed clinical improvement in the symptoms up to 97%. There was an improvement in the quality of life in the patients, bringing about marked improvement at work place with increased energy, reduced anxiety, and stress levels. Conclusion: To conclude, it is an ongoing research module to derive an effective management of IBS and improvement in the QOL with above regimen.
Key words: irritable bowel syndrome, Ayurveda, quality of life
References:
# P-0735
IgG response to class I epitope peptides is a quantitative predictive biomarker in early course of treatment in colorectal cancer treated by therapeutic peptides with oxaliplatin-based chemotherapy
Shinsuke Kanekiyo1, Shoichi Hazama1,2, Hiroko Takenouchi2, Masao Nakajima1, Yoshitaro Shindo1, Hiroto Matsui1, Yukio Tokumitsu1, Shinobu Tomochika1, Yoshihiro Tokuhisa1, Michihisa Iida1, Kazuhiko Sakamoto1, Nobuaki Suzuki1, Shigeru Takeda1, Shigeru Yamamoto1, Tomio Ueno1, Shigefumi Yoshino3, Fumiaki Sugiura4, Kiyotaka Okuno5, Keiko Udaka6, Tomonobu Fujita7, Yutaka Kawakami7, Tomoko Mtsueda6, Kyogo Ito6 and Hiroaki Nagano1
1Department of Gastroenterological, Breast and Endocrine Surgery, Yamaguchi University Graduate School of Medicine; 2Department of Translational Research and Developmental Therapeutics against Cancer; 3Oncology Center, Yamaguchi University Hospital; 4Department of Surgery, Kinki University Faculty of Medicine; 5Department of Immunology, School of Medicine, Kochi University; 6Division of Cellular Signaling, Institute for Advanced Medical Research, Keio University School of Medicine; 7Department of Immunology and Immunotherapy, Kurume University school of Medicine
Objective: Cancer vaccines have emerged as a promising therapeutic approach, but their clinical responses have been limited. To overcome this problem, it is necessary to explore biomarkers for predicting the clinical responses for successful immunotherapy. We previously conducted a phase II trial for advanced colorectal cancer (CRC) using five HLA-A*2402-restricted peptides (KOC1, TOMM34, RNF43, VEGFR1, and VEGFR2). In this study, correlations between overall survival and biomarkers, including cytotoxic T lymphocyte (CTL) and immunoglobulin G (IgG) responses to five peptides, were investigated. Patients and Methods: In 89 patients allowed to analyze the blood antibody titer, the plasma was collected before and after 3 months from vaccine administration. Antigen-specific T-cell response was estimated by enzyme-linked ImmunoSpot assays. The levels of immunoglobulins reactive to each of five peptides were measured by multiplex bead suspension array using the Luminex system. Result: The values of TOMM34 IgG (P < 0.001 ), RNF43 IgG (P < 0.001), and VEGFR2 IgG (P < 0.001) were significantly increased after vaccination and increased VEGFR2 IgG response well correlated with OS in HLA-matched group (P = 0.034 ). CTL response of VEGFR1 and VEGFR2 was also significantly increased in HLA-matched group (P = 0.049 and P < 0.001, respectively). However increased CTL response was not correlated with OS. Multivariate analysis of the Cox regression model indicated that IgG response to VEGFR2 was the most significant predictor for OS in the HLA-A*2402-matched group (P = 0.04). Conclusion: The study's findings suggest that VEGFR2 IgG response may be an immunological biomarker in patients with colorectal cancer treated by therapeutic epitope peptides.
# P-0738
Irritable bowel syndrome may be a condition that is associated with elevated liver enzymes and metabolic syndrome
Seung-Hwa Lee1, Eun-Seong Seo1 and Dong-Ryul Lee2
1Center for Endoscopy, Seo-Hae Hospital; 2Center for Health Promotion, Wonkwang University School of Medicine, South Korea
Background/Aims: Recent studies have revealed a close relationship between hepatic injury, metabolic pathways, and gut microbiota. These microorganisms in the intestine also cause irritable bowel syndrome (IBS). The aim of this study was to examine whether IBS is associated with elevated hepatic enzymes and metabolic syndrome (MS). Methods: This was a retrospective, cross-sectional, case–control study. We examined the levels of hepatic enzymes and metabolic parameters and the prevalence of elevated liver enzymes and MS in IBS patients in comparison with a control group. Of the 343 enrolled subjects, 83 had IBS according to the Rome III criteria. The control group consisted of 260 age- and sex-matched subjects without IBS. Anthropometric, metabolic, and hepatic biochemical parameters were compared between the two groups. Results: As compared with control subjects, patients with IBS showed significantly higher values of anthropometric parameter (body mass index and waist circumference), liver enzymes, and lipid levels. The prevalence of elevated alanine aminotransferase (ALT) and gamma-glutamyl transferase levels was significantly higher in patients with IBS than in control subjects. A statistically significant difference was observed in the prevalence of MS between controls and IBS patients. The relationship between an elevated ALT level, MS, and IBS remained statistically significant after controlling for potential confounding factors. Discussion and Conclusion: These results suggest that IBS may be a condition that is associated with elevated liver enzymes and MS. On the basis of our study, IBS might be an important condition in some patients with elevated liver enzymes and MS.
| A. OR of elevated AST* | ||||||
|---|---|---|---|---|---|---|
| Variable | B | SE | OR | P | 95% CI | |
| IBS | 0.438 | 0.487 | 1.549 | 0.369 | 0.596–4.025 | |
| B. OR of elevated ALT* | ||||||
| Variable | B | SE | OR | P | 95% CI | |
| IBS | 1.340 | 0.373 | 3.818 | < 0.001 | 1.838–7.929 | |
| C. OR of elevated γ-GT* | ||||||
| Variable | B | SE | OR | P | 95% CI | |
| IBS | 0.291 | 0.324 | 1.338 | 0.369 | 0.709–2.528 | |
| D. OR of MS** | ||||||
| Variable | B | SE | OR | P | 95% CI | |
| IBS | 1.237 | 0.284 | 3.446 | < 0.001 | 1.977–6.007 | |
- * Adjustment for obesity, diabetes mellitus, alcohol consumption, LDL cholesterol, total cholesterol, and triglyceride.
- ** Adjustment for alcohol consumption, LDL cholesterol, and total cholesterol.
- ALT, alanine aminotransferase; AST, aspartate aminotransferase; CI, confidence interval; γ-GT, gamma-glutamyl transferase; IBS, irritable bowel syndrome; LDL, low density lipoprotein; MS, metabolic syndrome; OR, odds ratio.
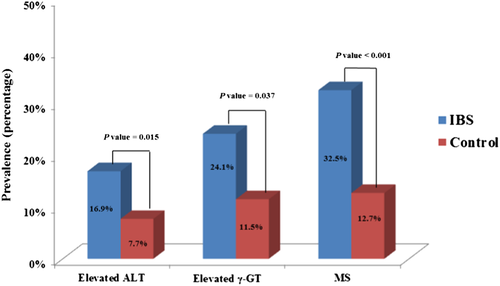
Elevated alanine aminotransferase (ALT) and gamma-glutamyl transferase (γ-GT) were defined as > 41 IU/L for males and > 31 IU/L for females for ALT, and > 66 IU/L for males and > 39 IU/L for females for γ-GT. Metabolic syndrome (MS) was defined as the presence of three or more of the guideline of American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI) Scientific Statement published in 2005. A significant difference was observed between the two groups with regard to ALT (16.9% vs 7.7%; P = 0.015), γ-GT (24.1% vs 11.5%; P = 0.037), and MS (32.5% vs 12.7%; P < 0.001). ALT, alanine aminotransferase; IBS, irritable bowel syndrome; γ-GT, gamma-glutamyl transferase.
# P-0740
Study on the anti-inflammatory mechanisms of Roseburia intestinalis mediated by inducing the differentiation of the Treg cells via TLR5 of the intestinal epithelial cells in inflammatory bowel disease
Zhaohua Shen1,2, Xiaoyan Wang (dum@my)*1,2, Changxin Zhu1,2, Yongsheng Quan1,2, Wei Yuan1,2, Zhenyu Yang1,2, Shuai Wu1,2, Weiwei Luo1,2, Bei Tan1,2 and Mingyu Huang1,2
1Department of Gastroenterology, Third Xiangya Hospital, Central South University, Changsha, Hunan, China; 2Hunan key laboratory of Non-resolving Inflammation and Cancer, Changsha, Hunan, China
Background: R. intestinalis belong to the family of Clostridium XIVa group. Our previous study provided the first evidence that R. intestinalis was significantly reduced in the intestinal tract of the patients with Crohn's disease (CD) in China. This article aims to elucidate the anti-inflammatory effect and mechanism of R. intestinalis in IBD. Methods: We propose to investigate the effects of R. intestinalis on Disease Activity Index (DAI) score, intestinal pathology, the expressions of TLR5, TSLP, and TGF-β, and the differentiation of Treg cells by using murine TNBS colitis models. At the cellular level, we use the human colon epithelial cell line Caco-2, overexpressing and silencing of TLR5 in HEK293 and Caco-2 cells, respectively, to co-culture with different concentrations of R. intestinalis and detect changes of TSLP and TGF-β. Results: R. intestinalis significantly decreased DAI scores (Fig. 1B). R. intestinalis reduced the degree of shortening of the colon and played the anti- inflammatory role by up-regulating the levels of TLR5, TSLP, and TGF-β (Fig. 1C,1E,1F) and increasing the proportion of Treg cells (Fig. 1D). In vitro, the co-culture of R. intestinalis and Caco-2 significantly increased secretion of TSLP and TGF-β levels of the cells (P < 0.05) and the silencing of TLR5 cells did not change theses cytokines. Conclusion: R. intestinalis might promote the secretion of TSLP and TGF-β from intestinal epithelial cells via TLR5, thus inducing the differentiation of the Treg cells.
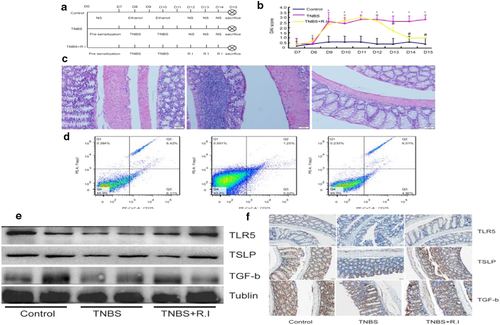
# P-0750
Primary monocytes derived from ulcerative colitis show no difference in the TNF-α-induced immune response among responders and primary non-responders to infliximab
Yuan Li1, Kim Bak Jensen2, Jakob Seidelin1 and Ole Haagen Nielsen1
1Department of Gastroenterology D112, Herlev Hospital, University of Copenhagen, Copenhagen, Denmark; 2Biotech Research and Innovation Centre, University of Copenhagen, Copenhagen, Denmark
# P-0768
Incidence and prevalence of inflammatory bowel disease (IBD) in Hospital Sultanah Aminah Johor Bahru (HSAJB)
Philip Boon Cheong Pang, Yong Siang Ng, Jeevinesh Naidu, Jasminder Sidhu and Maylene Kok
Department of Medicine, Hospital Sultanah Aminah Johor Bahru, Malaysia
Background: IBD is considered an uncommon disease among Asians, including Malaysians. However, experts have recognized that its incidence has been increasing in Asia. Data regarding its incidence and prevalence are limited in Malaysia. Therefore, more studies are needed to reflect the true burden of the disease. Methods: We conducted a hospital-based retrospective review of all IBD cases managed in HSAJB in 2016. The incidence and prevalence of IBD were calculated using the population of state of Johor as the denominator. The incidence and prevalence rates for the major ethnicity in Johor were also calculated using its population as the denominator. Results: Twenty-five new cases of IBD were diagnosed in 2016. The crude incidence of IBD, ulcerative colitis (UC), Crohn's disease (CD), and IBD unclassified (IBDU) were 0.68, 0.36, 0.27, and 0.05 per 100 000 population, respectively. Indians have the highest incidence at 4.21 followed by Malays and Chinese at 0.56 and 0.18 per 100 000 population, respectively (Figure 1). A total of 156 IBD cases were captured; hence, the prevalence of IBD, UC, CD, and IBDU were 4.27, 2.33, 1.86, and 0.08 per 100 000 population, respectively. Similarly, Indians have high prevalence at 16.84, followed by Chinese at 4.06 and Malays at 3.44 per 100 000 population (Figure 1). Conclusion: The incidence of IBD in our study is comparable with current published data. However, the prevalence of IBD in our study is lower than that of the published ones.
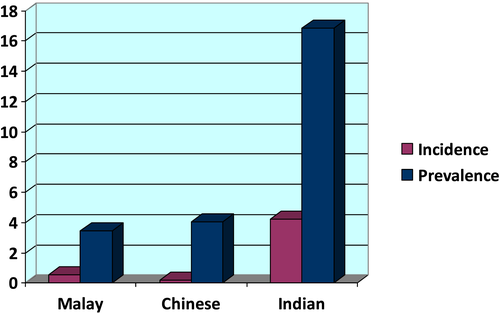
# P-0776
Polyp burden in first-degree relatives of chinese patients with familial colorectal cancer type X syndrome
K L Ko, S Y Leung, Y F Lam, L Y Mak, W P To, Teresa Tong, W L Law and W K Leung
Department of Medicine, Queen Mary Hospital, Hongkong
Background: Familial colorectal cancer type X (FCCTX) syndrome is a heterogenous group of colorectal carcinomas (CRC) characterized by Amsterdam Criteria or Bethesda Criteria but without mutations in the mismatch-repaired (MMR) gene. Individual family member with FCCTX suffers increased risk of CRC, but data on prevalence and characteristic of colonic polyps in this group of subjects are scarce. Method: Eligible cases with their families were identified from the Hereditary Gastrointestinal Cancer Genetic Diagnosis Laboratory at the University of Hong Kong, which is a territory-wide registry for genetic diagnosis of suspected hereditary CRC. Those fulfilling the Amsterdam or Bethesda criteria but tested negative for MMR gene were recruited. First-degree relatives were offered counselling and colonoscopy. The findings on their screening and surveillance colonoscopy were presented. Results: Seventy-one first-degree relatives (31 men) from 29 FCCTX families were identified. The mean age at screening was 52 (SD ± 7.0); 9 (12.7%) subjects have metabolic diseases (diabetes mellitus, cardiovascular, or cerebrovascular disease). At screening, 36 (50.7%) were found to have colonic polyps, with mean number of 2.2 polyps and 1.4 adenoma per patient. Eleven (15.5%) patients had multiple polyps (3 or more), and 6 (8.5%) had advanced adenoma. Of the 37 subjects who had surveillance colonoscopy, the mean interval is 3.6 (± 1.7) years and 19 (51.4%) were found to have polyps, including 14 (37.8%) adenoma and 2 (5.4%) advanced adenoma. Considering both colonoscopies together, 45 (63.3%) had polyps, 30 (42.3%) had adenoma, and 7 (9.9%) had advanced adenoma. Although there was no CRC detected, there were 4 cases of extra-intestinal malignancy. Female gender was found to be associated with a lower risk of polyps (OR = 0.15, 95%CI 0.04–0.52) and adenoma detected (OR = 0.3, 95% CI 0.12–0.95). There was however no association between age, presence of metabolic diseases, or use of aspirin and polyp or adenoma detection. Conclusion: First-degree relatives of Chinese FCCTX family have a high prevalence of adenoma on both screening and surveillance colonoscopy. Strategy on screening and surveillance need to be tailored to this group of at risk individuals.
# P-0796
Colorectal cancer and female patients are major risk factors associated with thrombosis of central venous port in chemotherapy
Akira Doi, Motowo Mizuno, Yuichi Shimodate, Naoyuki Nishimura, Hirokazu Mouri, Kazuhiro Matsueda and Hiroshi Yamamoto
Department of Gastroenterology and Hepatology, Kurashiki Central Hospital, Kurashiki, Japan
Background: Implantable central venous port (CVP) is widely used for chemotherapy, but CVP thrombosis is often observed. In this study, we aimed to identify risk factors associated with CVP thrombosis in patients with digestive organ cancers. Methods: From January 2011 to December 2016, CVP was implanted for chemotherapy in 191 patients with digestive organ cancers at our hospital. Among them, we excluded 11 patients who died or underwent removal surgery of CVP because of infection or wound dehiscence within two months after the implantation, and 180 patients in total were studied. We retrospectively analyzed risk factors for CVP thrombosis and usefulness of Khorana score for prediction of venous thromboembolism in cancer patients. Results: CVP thrombosis was found in 30 (16.7%). The incidence of CVP thrombosis was significantly higher in patients with colorectal cancer (26.0%, 20/77 patients) than with other cancers (gastric cancer 18.2%, 2/11; pancreatic cancer 9.1%, 2/22; esophageal cancer 8.5%, 5/59; and others 7.7%, 1/11). Eight patients (26.7%) complained of symptoms before diagnosis. Multivariate logistic regression analysis identified the followings as independent and significant factors associated with CVP thrombosis: colorectal cancer (odds ratio, 4.0, 95% confidence interval 1.01–15.9, P = 0.049), sex (female, 5.30, 1.87–15.0, P = 0.002), BMI (1.18, 1.02–1.38, P = 0.029), higher level of hemoglobin (1.4, 1.06–1.86, P = 0.011), and higher level of platelet (1.07, 1.01–1.13, P = 0.02), but use of bevacizumab was not associated with CVP thrombosis (P = 0.57, multivariate analysis). Khorana score was not useful to predict CVP thrombosis; score 0, 18.4% (16/87 patients); score1, 16.3% (7/43); score 2, 17.6% (6/34); and score ≧ 3, 6.3% (1/16) (correlation ratio η = 0.067). Conclusions: Colorectal cancer and female patients were major independent and significant risk factors for CVP thrombosis, regardless of use of bevacizumab. We should be aware of CVP thrombosis for effective chemotherapy especially in female and patients with colorectal cancer regardless of Khorana score.
# P-0800
Capability of CT colonography for detecting lesions over time
Masashi Hattori
Department of Gastroenterology, Yamashita Hospital, Japan
Aims: The majority of reports that have examined the capability of CT colonography (CTC) in detecting colorectal cancer and polyps have utilized colonoscopy (CS) as the gold standard to determine the detection rate. However, CS is known to carry a false-negative rate of 3–6%. The present study examined the capability of CTC in detecting lesions over time to investigate its usefulness. Methods: Among 3527 patients who underwent CTC between January 2012 and August 2014 due to a positive fecal occult blood test, this study investigated 103 patients who underwent a second CTC due to a positive fecal occult blood test at least 1 year after the initial CTC up until August 2015. Results: Fifty-eight patients did not present abnormal findings at either CTC. Six patients exhibited polyps at the initial CTC and underwent EMR but did not show abnormal findings during subsequent follow-up. Thirty lesions from 12 patients were detected at the initial CTC but did not show changes during follow-up. False positives were revealed in twelve lesions from eight patients where polyps were detected at the initial CTC but not at the second CTC at the same site. False negatives were revealed in eight lesions from five patients where polyps were not detected at initial CTC but were discovered at the second CTC and also confirmed on retrospective review of the initial CTC. Sixteen lesions from thirteen patients were not detected on initial CTC, were observed at the second CTC, but were not evident on retrospective review of the initial CTC. These were thus considered to be new lesions, polyp size ranged between 2 and 5 mm. In one patient, an 18-mm-sized lipoma appeared during a 36-month follow-up. All false positives among lesions with inconsistent results were ≤ 5 mm in size. The false-negative rate for ≥ 6-mm lesions among all 67 lesions was 4.5% with a detection rate of 95.5%, indicating positive effectiveness. Conclusion: CTC is extremely effective for detecting changes over time.
# P-0837
Epidemiology and clinical course of inflammatory bowel disease in the Central Province of Sri Lanka: A hospital-based study
Udaya Kalubowila1, Tharanga Liyanaarachchi1, K B Galketiya2, Palitha Rathnayaka3, Sampath Tennakoon4, K M P Perera1, S D M U Pathirana1, D B Wettewa1, W R A N M P Ratnayake1, R M Raayiz1 and D M I U Dissanayaka1
1Gastroenterology and Hepatology Unit, Teaching Hospital Kandy, Kandy, Sri Lanka; 2Department of Surgery, Faculty of Medicine, University of Peradeniya, Kandy, Sri Lanka; 3Department of Pathology, Teaching Hospital Kandy, Kandy, Sri Lanka; 4Department of Community Medicine, Faculty of Medicine, University of Peradeniya, Kandy, Sri Lanka
Background: There is increasing prevalence of inflammatory bowel disease (IBD) in Asia, but Sri Lankan data on the state of epidemiology and clinical course of IBD are scarce. Method: A hospital-based study was done recruiting IBD patients who permanently reside in the Central Province of Sri Lanka. Cases were confirmed by standard criteria, and data were collected from health records and patient interviews at clinic visits and hospital admissions. Results: There were 207 cases of IBD: ulcerative colitis (UC)—140, Crohn's disease (CD)—60, and microscopic colitis—7.The crude prevalence rate of UC was 5.44/100 000 (95% CI 5.41–5.47/100 000), and CD was 2.33/100 000 (95% CI 2.31—2.35/100 000). Male to female ratio was 0.8 for UC but 1.5 for CD. Mean age at diagnosis was 42 and 31.9 years for UC and CD, respectively. One UC and one CD patient had a positive family history of IBD. Among UC patients, 60.7%, 24.3%, and 15% had distal, left-sided, and extensive disease, respectively. At presentation, 62.1% of UC patients have had moderately severe disease. About 60% of CD patients had only large bowel involvement, and 80% had non-stricturing and non-penetrating disease. Extra intestinal manifestations were present in 45.7% and 60% of UC and CD patients, respectively, in which peripheral arthritis and arthralgia being the commonest; 6.4% of UC and 23.3% of CD patients (total of 23) required infliximab for induction of remission. Conclusion: The prevalence of UC in this population was similar to other Asian and previous Sri Lankan studies; however, higher prevalence of CD was found. Presentation of UC was a moderately severe distal disease, and UC patients were more likely to be older than CD patients. CD was commonly a male predominant non-stricturing and non-penetrating disease involving only large bowel consistent with Asian studies. CD needed induction with infliximab more than UC.
# P-0849
Effects of acute changes in fermentable fiber intake on regional colonic fermentation and transit in patients with quiescent ulcerative colitis
Chu K Yao, Rebecca E Burgell, Kristin M Taylor, Mark G Ward, Jacqueline S Barrett, Jane G Muir and Peter R Gibson
Department of Gastroenterology, Monash University & Alfred Hospital, Melbourne, Australia
Background/Aims: Defective colonic fermentation was recently described in patients with quiescent ulcerative colitis (UC). Such defects may differ across colonic regions along with varying dietary fiber intake. These aspects require further study. The study aimed to define regional colonic fermentation in patients with quiescent UC by direct intestinal pH-transit profiling. Methods: In a randomized, double-blind study, patients with quiescent UC (Partial Mayo Score ≤ 1; fecal calprotectin < 150 μg/g) and healthy controls were recruited. After a 7-day run-in, subjects received two study meals high (13 g oligosaccharides and resistant starch) or low (< 1 g) in fermentable fiber before ingesting a pH-motility capsule. Subjects then crossed over to the other diet 3 days after passage of the capsule. Endpoints were diet-associated differences in overall, cecal and distal colonic pH, and colonic transit times (CTT). Results: Fifteen UC patients (aged 24–72 y; 9 males) and 9 controls (aged 22–69 years, 4 males) were studied. A high-fiber diet significantly lowered overall and distal colonic pH in healthy controls (Table 1). Conversely, only cecal pH was lowered on the high-fiber diet in UC patients. No diet-associated effects on CTT were seen in either cohort. However, subgroup analysis of UC patients showed highly heterogeneous responses (64% with slower CTT vs 36% with unchanged/faster CTT) to a high-fiber diet. Conclusions: Distinct patterns of fermentation and transit occurred in UC patients after a high fermentable fiber intake compared with controls. These findings suggest that colonic motility and regional microbiota function are abnormal in UC despite quiescent disease. Conflicts of interests: Research support was received from Ferring Pharmaceuticals.
| Overall mean pH (95% CI) | Mean cecal pH (95% CI) | Mean distal colonic pH (95% CI) | Median [IQR] CTT (h) | ||
|---|---|---|---|---|---|
| UC n = 15 | Low fiber | 6.4 (6.2–6.8) | 5.6 (5.3–5.7) | 7.9 (7.6–8.2) | 17 [9–23] |
| High fiber | 6.3 (6.0–6.5) | 5.2 (5.0–5.4) | 8.1 (7.6–8.4) | 21 [16–39] | |
| P-value | 0.20 | 0.001 | 0.09 | 0.13 | |
| Healthy n = 9 | Low fiber | 6.9 (6.5–7.2) | 5.5 (5.2–5.8) | 8.2 (8.0–8.5) | 16 [15–37] |
| High fiber | 6.3 (6.0–6.5) | 5.2 (4.9–5.5) | 7.7 (7.4–8.0) | 18 [15–32] | |
| P-value1 | 0.02 | 0.15 | 0.04 | 0.582 |
- 1 Paired t-test or
- 2 Mann–Whitney test
# P-0862
Efficacy of ultrasonography for evaluation of disease activity in ulcerative colitis
Manabu Shiraki
Department of Gastroenterology, Tohoku Rosai Hospital, Japan
Background: Endoscopic examination carries a risk of perforation of the colon because of mucosal vulnerability in patients with ulcerative colitis relapsing. We report here the efficacy of ultrasonography for ulcerative colitis during active period. Methods: The patients with relapsing ulcerative colitis between September 2014 and March 2016 were included in this study. All patients had undergone sigmoidoscopy, CT, and ultrasonography. The colon ultrasound image was divided into six segments: rectum, sigmoid colon, descending colon, transverse colon, ascending colon, and cecum. Then we evaluated twall thickness, decrease in echogenicity of the submucosal layer, irregularity, or discontinuity of the mucosal layer, assigning an ultrasonographic (US) score to each segment. The colon CT image was also divided into six segments, evaluated wall thickening, and mesenteric vascular engorgement, assigning a CT score to each segment. Lymph node swelling was also evaluated. Further, we calculate a total US score and a total CT score by the sum of the scores of 6 segments. To assess endoscopic severity, Mayo endoscopic subscore was used. We investigated the correlation between those US scores and those CT scores, Mayo endoscopic subscores. Results: Twenty three cases of ulcerative colitis were included in this study. We observed a strong degree of correlation between total CT score and total US score (ρ = 0.70, P = 0.0056) although the sum of the US score of the rectum and sigmoid colon was not related to that of the CT score of the same segment (ρ = 0.42, P = 0.23). We observed a moderate degree of correlation between total US score and partial Mayo score (ρ = 0.45, P = 0.040). Conclusion: This study suggested that ultrasonography could provide useful information to assess the disease activity of ulcerative colitis without unnecessary radiation and invasiveness.
# P-0865
A low-grade appendiceal mucinous neoplasm presented with ileocolic intussusception in cerebral palsy patient: A case report
Kunishige Okamuara1, Masanori Ohara1, Tsukasa Kaneko1, Aki Fujiwara1, Takumi Yamabuki1, Ryo Takahashi1, Kazuteru Komuro1, Nozomu Iwashiro1, Kimitoshi Kubo2, Katsuhiro Mabe2, Mototsugu Kato2 and Noriko Kimura3
1Department of Surgery; 2Department of Gastroenterological Medicine; 3Department of Pathology, National Hospital Organization Hakodate Hospital, Hakodate, Japan
Introduction: Low-grade appendiceal mucinous neoplasm (LANM) is extremely rare. In Japan, it was newly classified based on the WHO classification in 2013. Ileocolic intussusception associated with LAMN is rarely a trigger for discovery. The aim of this study is to report a rare case of low-grade appendiceal mucinous neoplasm presented with ileocolic intussusception. Case description: A 42-year old woman with a history of cerebral palsy and generalized epilepsy admitted in a near-by hospital. She presented with frequent vomiting and abdominal tightness and was transferred to our hospital because of ileus. Abdominal X-ray examination showed small intestinal gas. A nasal ileus tube was inserted under transnasal endoscopy. Abdominal computed tomography revealed transverse colonic intussusception, but no finding of a tumor. Colonoscopy showed smooth surface ridge lesion advanced to the transverse colon. After reduction of the intussusception, submucosal tumor in the cecum was diagnosed and laparoscopic ileocecal resection was performed. Intraoperative findings revealed the moving cecum and ileocolic intussusception recurrence. Histopathological diagnosis indicated a low-grade appendiceal mucinous neoplasm. The patient's postoperative curse was unremarkable, and she could discharge on postoperative day 17. No recurrence has been identified for 10 months after surgery. Discussion: LAMN is one of appendiceal tumors. The prognosis of LAMN is good by curative resection, though LAMN presented with ileocolic intussusception is difficult to have qualitative diagnosis before surgery. Recently, laparoscopic surgery has been selected frequently and can be performed safely. Conclusion: LAMN presented with ileocolic intussusception should be promptly investigated for diagnosis, and appropriate treatment should be selected.
# P-0880
Impacted ring causing colonic obstruction : A case report
Tae-Kim, Seong Taeg Kim, Seong Joo Ko, Hoe-Soo Jang, Seung Uk Jeong, Soo-Young Na, Hyun Joo Song, Eun Kwang Choi, Heung Up Kim, Byung-Cheol Song and Sun-Jin Boo
Department of Internal Medicine, Jeju National University School of Medicine, South Korea
Introduction: We report on a case of an impacted ring causing colonic obstruction in an old female patient. Case: A 86-year-old woman presented with recurrent abdominal pain (LLQ area), vomiting. She had accidentally swallowed three rings two years ago. She had a history of cerebral infarction, diabetes mellitus, and atrial fibrillation. Abdominal X-ray showed a ring in left pelvic cavity. Abdominal CT revealed a ring-shaped metallic artifact in left pelvic cavity. Sigmoidoscopy showed focal luminal narrowing in the sigmoid colon, and the endoscopy could not pass through the stenotic area. Colon study revealed the stenotic colon encircled by a metallic ring. Laparoscopic sigmoidectomy was performed. A 2-cm sized metallic ring was embedded in the mucosal and submucosal layer. Pathologic findings were chronic foreign body impaction with chronic colitis, ulceration, and submucosal fibrosis. The patient had no abdominal pain during 9 months of follow-up. Conclusion: We report on an old female patient with recurrent abdominal pain vomiting due to a impacted ring causing colonic obstruction.
# P-0890
Combined arterial and venous thrombosis in a patient with ulcerative colitis: A rare occurrence
Thevaraajan Jayaraman1, Rafiz Abdul Rani1, Zhiqin Wong2, Chai Soon Ngiu2 and Raja Affendi Raja Ali2
1Gastroenterology Unit, Faculty of Medicine, University Teknologi MARA, Sungai Buloh Campus, Selangor, Malaysia; 2Gastroenterology Unit, Department of Internal Medicine, University Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia
Introduction: Inflammatory bowel disease (IBD) is a chronic inflammatory disease of the gastrointestinal tract and results from a combination of genetic susceptibility, environmental exposure, and dysregulated responses to intestinal microbiota. Patients with IBD are vulnerable to vascular complications, and the risk of venous thromboembolic disease in IBD is well described; IBD confers a 2-fold increased risk of developing deep vein thrombosis and pulmonary embolism. On the other hand, the risk of arterial thromboembolism in IBD is not well characterized, and there are limited studies to underpin this association. Combined arterial and venous thrombosis in IBD is certainly very rare with only a few cases reported to date. Case Description: We report a case of a 24-year-old male with a two-year history of ulcerative colitis who presents with progressively worsening left distal lower limb pain for one week. He is diagnosed as having critical limb ischaemia secondary to thrombosis in the distal left superficial femoral artery. Incidentally, he also has thrombosis of the left superficial femoral vein. He had to undergo a trans-metatarsal amputation of his distal left lower limb after failure of medical therapy to achieve reperfusion. After making an uneventful recovery from the surgery, he presents six months later with a flare of ulcerative colitis and had to be commenced on biological therapy to achieve clinical remission. Combined arterial and venous thrombosis preceding a flare is a very rare occurrence in ulcerative colitis and serves to underline the high pro-thrombotic potential conferred by IBD.
# P-0908
A randomized controlled trial comparing water infusion and air insufflation as scope insertion technique in the training of primary care physicians for screening flexible sigmoidoscopy
Raymond S Y Tang1, Moe H Kyaw2, Kelvin L Y Lam1, Thomas Y T Lam1, Andrew M Y Ho1, Martin C S Wong2, James Y W Lau3 and Justin C Y Wu1
1Institute of Digestive Disease, The Chinese University of Hong Kong, Hong Kong, China; 2School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong, China; 3Department of Surgery, The Chinese University of Hong Kong, Hong Kong, China
Background: Recently, the use of water infusion (WI) or water exchange techniques has been shown to reduce patient discomfort during colonoscope insertion and to increase the success rate of unsedated colonoscopy, but data on the use of WI in flexible sigmoidoscopy (FS) remain scarce. This study aims to evaluate the impact of WI as scope insertion technique in the training of primary care physicians (PCP) for screening FS. Methods: Eight PCPs without prior endoscopy experience received training for screening FS under supervision by gastroenterologists from 2015 to 2017. FS trainees were randomized to use either WI or air insufflation (AI) during scope insertion. Trainees were mandated to complete ≥ 50 FS per person before competency assessment. The mean percentage of unassisted FS insertion within 10 minutes using WI or AI in the initial 40 FS, patient discomfort, and scope insertion time to descending colon were analyzed. Results: A total of 408 FS were performed by 8 trainees (201 in WI group and 207 in AI group). The baseline characteristics of patients in WI and AI groups were similar. The mean percentage of unassisted FS insertion within 10 minutes using WI or AI were 68.8% versus 79.4%, P = 0.041 in the initial 40 FS, and 70.6% versus 79.2%, P = 0.052 in the overall FS training, respectively. The mean percentage of unassisted FS insertion from the 41st FS and beyond were similar (78.0% vs 78.7%, P = 1). The mean intra-endoscopy pain score (4.0/10 vs 4.0/10, P = 0.977) and the mean scope insertion time (8.3 vs 7.8 mins, P = 0.207) were similar. Conclusion: In this study, the use of AI by PCP in the initial 40 FS training resulted in a higher rate of unassisted FS insertion. The mean percentage of unassisted FS insertion from the 41st FS and beyond and patient discomfort were similar using either WI or AI.
# P-0920
The change of bone mineral density in patients with inflammatory bowel disease
Joonho Jeong, Won Moon, Seunja Park, Jaehyun Kim, Mooin Park, Sungen Kim and Kyungwon Jung
Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea
Background/Aims: There are limited data regarding the impact of treatment for IBD on the BMD status. Therefore, this study aimed to identify the change of BMD in the patients with IBD after treatment. Methods: The cases were retrieved from 442 patients who were diagnosed with IBD in a single university hospital. Of those, 119 patients (CD 84, UC 35) had the follow-up BMD with at least 1-year interval. The associations between BMD, BMI, and disease activity parameters including CDAI, Mayo-score, hemoglobin (Hb), c-reactive protein (CRP), and serum albumin were evaluated as Pearson correlation analysis and partial correlation; BMD was measured as Z-score, and low BMD was defined as less than −1. Results: In enrolled 84 patients with inactive CD, the baseline mean of BMD Z-score at the L-spine and femur neck were −0.44 ± 1.36, −0.13 ± 1.28; the follow-up mean of BMD Z-score at the L-spine and femur neck, corrected by period, were −0.47 ± 1.21 (P = 0.512), −0.18 ± 1.17 (P = 0.304). In enrolled 35 patients with inactive UC, the baseline mean of BMD Z score were −0.20 ± 1.04, −0.11 ± 1.06; the follow-up mean of BMD Z-score at the L-spine and femur neck, corrected by period, were −0.26 ± 1.05 (P = 0.145), −0.08 ± 1.06 (P = 0.633). Low BMD group patients of CD and UC at the baseline were 30 (35.7%) and 11 (30.6%); the number of low BMD patients with CD and UC at the disease-controlled status were 31 (36.9%, P = 0.873), 9 (25%, P = 0.599), respectively. Only in the low BMD group of CD the BMD of femur neck was correlated with BMI, Hb, CRP, and albumin. (0.517: P = 0.003, 0.423: P = 0.02, −0.394: P = 0.031, 0.378: P = 0.039). However, there was no correlation with disease activity parameter and BMD status in partial correlation, using BMI as control variable. Conclusions: There is no correlation with improvement of disease and BMD status after treatment in patients with IBD. However, in low BMD group of CD, treatment itself could improve the status of BMD of femur neck.
# P-0927
The retrospective study on stage IV colorectal cancer at our hospital
Tomoki Nakai
Department of gastroenterology and hepatology, Japanese Red Cross Wakayama Medical Center, Japan
Purpose: Regarding the treatment method for stage IV colon cancer, surgically resectable cases and symptomatic cases with primary tumor is preferred to go through surgical treatment. In unresectable cases, there are variety of treatment options, for example, primary tumor resection, chemotherapy, inserting a self-expandable metallic stent, and combining them. The priority of treatments is still controversial, so we examined the current situation and results at our hospital. Methods: Between January 2012 to December 2015, 189 cases with colon cancer stage IV were diagnosed at our hospital. We retrospectively analyzed 60 asymptomatic patients who did not need to prioritize surgery. We retrospectively analyzed 8 cases with severe stenosis that an endoscopy cannot pass through but underwent first line chemotherapy for other reasons. Results: There were 11 cases with BSC or went to another hospital. Twenty-eight cases underwent preemptive chemotherapy. Twenty-one cases underwent preemptive surgery, and 15 cases were followed by chemotherapy. Out of the 28 cases who underwent preemptive chemotherapy, 2 cases were able to undergo conversion surgery. Out of the 21 cases who underwent resection, 2 cases were able to go through surgery of the metastatic lesion after chemotherapy. The median survival of the preemptive chemotherapy group was 429 days, preemptive surgery group was 755 days. In the preemptive chemotherapy group, there was one case with colorectal obstruction and one case with perforation. Out of the 8 cases with severe stenosis who underwent preemptive therapy, occlusion was seen in 4 cases and perforation in 1 case. Endoscopic stenting was performed in all the cases with occlusion. Conclusions: In cases of the preemptive chemotherapy group with severe stenosis, complete occlusion tented to occur later on. However in such cases, surgery was able to be avoided by endoscopic stenting. We reported the current situation in our hospital.
# P-0929
Comparison of infusion reactions to infliximab and vedolizumab: A retrospective analysis
Webber Chan1,2, Glen Collins1, Esther Lee3, Azeez Mahmoud3 and Rupert Leong1,3
1Concord Repatriation General Hospital, NSW, Australia; 2Singapore General Hospital, Singapore; 3Macquarie University Hospital, NSW, Australia
Background: Infliximab (IFX) and vedolizumab (VDZ) are monoclonal antibodies targeting tumor necrosis factor-α and α4 β7 integrin, respectively, and indicated in the treatment of inflammatory bowel diseases (IBD). Both are administered by intravenous infusion and may be associated with different types of infusion reactions. Aim: To compare the incidence of infusion reactions in adult IBD patients on IFX and VDZ treatment and identify when these infusion reactions happened. Methods: We performed a retrospective review of all IFX and VDZ infusions performed at Concord Repatriation General Hospital and Macquarie University Hospital, Sydney, from January 2012 through March 2017. Fisher's exact test and receiver operating characteristics (ROC) curve analysis were used. Results: A total of 157 consecutive patients who received 1921 infliximab infusions and 61 patients who received 509 vedolizumab infusions were evaluated. All patients received intravenous hydrocortisone prior to IFX and VDZ infusion. Most patients were on concurrent immunomodulators (azathioprine or methotrexate). The overall incidence of infusion reactions to IFX was 1.3% (25 of 1921 of infusions), affecting 14.6% (23 of 157) of patients; and that to VDZ was 0.2% (1 of 509), affecting 1.6% (1 of 61). Mild to moderate and severe acute reactions occurred in 1.2 % (23 of 1921) and 0.1% (2 of 1921) of infliximab infusions, respectively. One case of mild-moderate reaction happened in VDZ infusion, but no severe reactions were observed. Compared with VDZ, IFX was associated with more mild-to-moderate infusion reactions (such as rash, arthralgia, tachycardia, diaphoresis) (P = 0.0425 per infusion, Table 1), whereas the difference for severe reaction (such as significant hypotension and severe dyspnea) was not statistically significant. Based on ROC curve analysis (Figure 1), the optimal number of IFX infusions after which infusion reactions were less likely to happen was 8 (P < 0.01) and that for VDZ was not statistically significant. Conclusion: Infliximab is associated with more mild-moderate infusion reactions compared with vedolizumab, suggesting that IFX is associated with more immunogenicity.
| Mild-mod reactions | None | P value | |
|---|---|---|---|
| IFX | 23 | 1898 | 0.0425 |
| VDZ | 1 | 508 | |
| Fisher's exact test for severe reactions (per infusion) | |||
| Severe reactions | None | P value | |
| IFX | 2 | 1919 | Not significant |
| VDZ | 0 | 509 | |
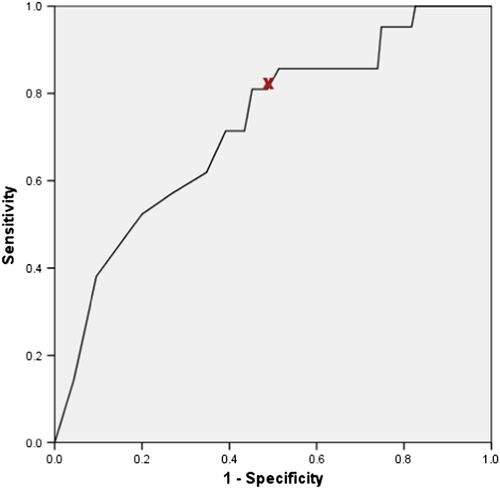
# P-0930
Evaluation of the diagnostic performance of colon capsule endoscopy for colon polyps in Hyogo college of Medicine
Tomoaki Kono, Yoshio Ohda and Hiroto Miwa
Department of Internal Medicine, Hyogo College of Medicine, Japan
Background and Aim: Colon capsule endoscopy (CCE) is a new procedure to investigate colonic lesions. CCE has been endorsed by Japanese Health Insurance since January 2014 and been introduced to our hospital since April 2015. We evaluated its clinical performance from our experience on this device. Methods: Twelve patients who had previously failed colonoscopy underwent CCE in our hospital between April 2015 and December 2016. Colon polyps were detected in all the patients, which were then treated by double-balloon endoscopy (DBE). We assessed the CCE excretion rate, colon transit time, colon cleansing, total water intake, patient's tolerance, complications, and evaluated the per-polyp sensitivity of colorectal polyp detection compared with DBE as the gold standard. Results: The CCE excretion rate was 66.7%. The mean colon transit time was 232 minutes (range: 35–491). The colon cleansing was good in 3 and poor in 9 patients. The total water intake was 4000 mL (range: 3500–4100). The tolerance CCE was rated in 3 grades, and 4 were rated well, 6 were rated moderate, and 2 were poor. No complication was observed. CCE demonstrated a per-polyp sensitivity of 73.1% for all polyps and 93.2% for polyps measuring ≥ 6 mm but had only 53.8% sensitivity for polyps measuring ≤ 5 mm. The combination of polyp size ≤ 5mm and poor colonic cleansing was associated with a particularly low sensitivity of 25.0%. About 91.6% of patients preferred to take DBE for the next procedure to investigate colonic lesions. Conclusion: Most patients preferred DBE to CCE which might come from the burden of colon preparation according to the Questionnaire survey. However, as CCE demonstrated a high diagnostic performance for polyps measuring ≥ 6 mm, it should be accepted as a screening tool for patients with failed colonoscopy, although further improvements may be required for preparation regimens for better colon cleansing.
# P-0934
Postoperative mid-term prognosis in patients with pediatric onset Crohn's disease
Yeoun Joo Lee, Sangwook Mun and Jaehong Park
Department of Pediatrics, Pusan National University Chidren's Hospital, Korea
Background: Patients with Crohn's disease (CD) may require surgical treatment, depending on their medical condition or disease progression. However, limited data are available on the postoperative progression and prognosis of pediatric CD in Korea. This study was conducted to assess the preoperative and postoperative progression and prognosis of pediatric onset CD. Methods: We reviewed medical records of patients diagnosed with pediatric CD who underwent surgery between February 2011 and April 2017 at Pusan National University Children's Hospital. The surgery was divided into luminal surgery and perianal surgery. Patients who underwent surgery were examined for changes in ESR, height, weight, the duration of hospitalization, and number of hospitalizations before surgery, and at 6 months, 1 year, and 2 years after surgery. Results: A total of 158 patients were examined, and 24 (15.2%) patients who underwent surgery were included. Of them, 12 patients (50%) underwent surgery for luminal CD, 9 (37.5%) for perianal CD, and 3 (12.5%) underwent both operations. In 15 patients who underwent luminal surgery, weight gain (P = 0.01) and change of ESR (P = 0.00) were statistically significant. However, increase in height was not statistically significant. The comparison of the two groups according time showed no significance (P = 0.281). The average number of hospitalizations was decreased from 7.3 ± 11.4 times before surgery to 0.4 ± 0.4 times after surgery in all patients (P = 0.007). The annual hospital stay was also significantly reduced from 131.7 ± 165.2 days to 4.1 ± 7.0 days (P = 0.001). Conclusion: This study showed that in operated with pediatric onset CD, weight increases, ESR significantly decreases, and the number of re-admissions and days of hospitalization tends to decrease significantly. Although medical treatment is very important for this disease, quality of life can be improved by timely surgical treatment.
# P-0936
Abdominal catastrophe? A case of pneumatosis intestinalis
Michael Christopher Alianza, Alexandra Laya and Matilde Cheng
We would like to present a case of LDL, 82-year-old male, diagnosed case of COPD, HASCVD, in persistent AF in controlled ventricular response, HFpEF, T2DM, insulin requiring, S/p multiple CVD infarct, former pipe fitter in nuclear power plant then worked as server in the US that came in for diarrhea and hematochizea of 3 days duration. Patient was initially admitted and hydrated. A whole abdominal CT scan was done and shown to have pneumatosis intestinalis with portal gas and pneumoperitoneum. There was also an incidental finding of a mass on the right pleura. He then underwent diagnostic laparoscopy, and intraoperatively, there was no signs of mesenteric ischemia or necrosis. Patient then underwent prophylactic diversion into ileostomy. Patient was then started on antibiotics and was later observed for fever or deterioration of the status. He was then noted to have recovered with no recurrence of the hematochizea. With the said CT scan findings and presentation of hematochizea, it was necessary to undergo a surgical survey of the abdomen; however, in this case, patient's intraoperative finding was completely benign and there was no evidence of ischemia or necrosis. This is one of the few rare instances of a benign pneumatosis intestinalis though the cause could not be completely established due to confounding features of this case. Case Report: Pneumatosis intestinalis, along with pneumoperitoneum and portal gas, is known as signs of catastrophic abdominal findings in CT scan.1,4 On literature, it is often paired with mesenteric ischemia2,4; however, there were reports of a benign abdomen and noted to be intraoperatively benign or need not to be operated upon.3 We are presented with a case of LDL, an 82-year-old male, diagnosed case of COPD, HASCVD, persistent AF in controlled ventricular response, HFpEF, T2DM, insulin requiring, S/p multiple CVD infarct, former pipe fitter in a nuclear power plant then worked as server in the US that came in for diarrhea and hematochizea of 3 days duration. Patient was apparently well and was just recently admitted for pneumonia in the last 3 months. Patient then had sudden onset of loose watery stools, non-mucoid but bloody and on admission patient was noted to have soft abdomen with slight tenderness on the left lower quadrant with normoactive bowel sounds. On chemical exams, patient was noted to have slight leukocytosis. However, on abdominal CT scan, there was note of pneumatosis intestinalis, with portal vein gas and pneumoperitoneum (refer to Figure 1). Other pertinent findings seen on CT were a circumferential mass on the right pleura and bowel wall thickening in the rectum. Patient was then referred to the infectious disease service and surgery service. He was then started on antibiotics and antifungals. Procalcitonin and lactate was done, but results was equivocal. He was then placed on bowel rest and later underwent diagnostic lapascopy. Intraoperatively, the said pneumatosis was seen; however, there was no signs of bowel ischemia nor necrosis. The surgeon then explored and did diverting ileostomy. Post-operatively, the patient was comfortable, and there was no untoward events noted. Antibiotics were completed, and patient was then discharged.
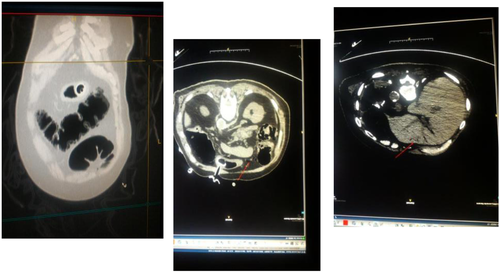
Pneumatosis intestinalis is one of the radiologic findings which could benign or catastrophic. On literature, pneumatosis with portal gas and pneumoperitoneum is often linked with bowel ischemia,4 and for our patient, who is a known case of atrial fibrillation, this scenario likely.2 Often, they would present with bloody diarrhea especially if the segments involved are the large colon.1 There has been case reports however that some of this cases could be managed conservatively with antibiotics3, 5 and observation. However, on our patient, diagnostic laprascopy might be necessary due to the presence of signs of ischemia and or perforation that might necessitate colonic resection. Another confounding factor for this patient would be the presence of COPD that could actually produce the said radiologic finding but otherwise a benign abdomen. Lastly, the presence of infection,1 could actually produce the findings but would not necessitate surgery. He was then managed accordingly, and he is for planned follow up with a CT scan and possible take down ileostomy. With this case, the findings of pneumatosis intestinalis with portal gas require immediate attention; however, management should always be patient-directed and the need for surgery versus conservative and medical management should always be in favor of the patient. It is also imperative to determine if pneumatosis intestinalis is a benign finding based on the clinical aside from the radiologic findings on CT scan. We need to re-evaluate patients for cause and likely outcomes for this patient.
References:
# P-0943
Treatment of irritable bowel syndrome with fecal microbiota transplantation by colonoscopy: A case series of ten patients
Ji Taek Hong, Byoung Wook Bang, Yong Woon Shin, Hyung Gil Kim and Kye Sook Kwon
Division of Gastroenterology, Department of Internal Medicine, Inha University School of Medicine, Incheon, South Korea, 400-711
Background: The pathogenesis of irritable bowel syndrome (IBS) cannot be explained by a simple mechanism, but alterations in the intestinal microbiome are increasingly a focus of interest. Conventional treatments have had only limited success, underscoring the need for additional therapeutic options. We hypothesized that fecal microbiota transplantation (FMT) may be beneficial in managing IBS by restoring the intestinal homeostasis. The purpose of this study is to prospectively examine the symptomatic response of FMT in patients with moderate to severe IBS. Methods: Patients with IBS who were not responsive to conventional treatment were enrolled prospectively in this study. Diagnosis of IBS was based on Rome III criteria and nonresponsive IBS was defined as failure to achieve symptomatic relief with conventional therapeutic modalities. The healthy donors were screened and tested for infectious diseases before stool donation. Patients were questioned with IBS severity score before and 1 month and 3 months after FMT. IBS severity score consist of 5 questions. Total score is 500. Study outcomes included the length of symptom-free intervals, abdominal pain, bloating, flatus, dyspepsia, frequency of bowel movements, and overall well-being before and after FMT. Results: A total of ten patients (mean age of 55 years; 60% male) were enrolled and completed the study questionnaire. Average disease duration from initial diagnosis of IBS to FMT was 3.6 years. In our study, 80% of the patients experienced resolution or improvement of symptoms after FMT. There were no FMT-related adverse events in all patients. IBS severity scores were significantly improved one month after FMT (132 ± 100) comparing to baseline (252 ± 121.7) (P = 0.027). However, their symptoms tended to return to their pre-FMT state at 3 months after FMT (231 ± 110). Conclusions: This study showed that FMT via colonscopy may be helpful for more than one month. However, their effect seemed to decrease over time. FMT can be a viable therapeutic option for IBS when the conventional treatment failed.
Key words: fecal microbiota transplantation; irritable bowel syndrome; colonoscopy
# P-0944
Intraluminal cystic lympangioma in sigmoid colon presenting as acute gastrointestinal bleed: A case report
A R Nitin Rao1 and S K Ravikiran2
1Department of Surgical gastroenterology; 2Medical Gastroenterology, MS Ramaiah Medical College, MSR Nagar, Bengaluru, India
Lympangioma are a common entity; however, intra-abdominal lypmhangioma are rare and constitute less than 5% of all lympangiomas. Cystic lympangioma presenting inside the lumen of the bowel and also presenting as gastrointestinal (GI) bleed is very uncommon. Herewith, we present such a case.
A 56-year-old male was referred to us for massive GI bleed with a hemoglobin of 4 gm% requiring blood transfusion to correct the same. Upper GI endoscopy was normal, and colonoscopy showed a large floppy polyp in the sigmoid colon. As the polyp appeared big and floppy, a decision to not do a polypectomy was made. CT scan abdomen confirmed the polyp with nil else significant in the abdomen. A sigmoid colectomy was performed with end to end stapled anastomosis, with the polyp being cystic in nature. Histopathology confirmed the polyp to be a cystic lympangioma. Patient was discharged on fourth postoperative day and has been followed up for 3 months with full recovery and no recurrence of GI bleed.
# P-0951
Comparison of colonoscopic quality indicators for predicting adenoma miss rate
Dong-Won Lee, Ja Seol Koo, Jung Wan Choe, Seung Young Kim, Jong Jin Hyun, Young Kul Jung, Sung Woo Jung, Hyung Joon Yim and Sang Woo Lee
Department of Internal Medicine, Korea University Ansan Hospital, Ansan-si, Korea
Background: Adenoma detection rate (ADR) is most widely used as an indicator of quality of colonoscopist's skill. However, high ADR alone do not guarantee complete removal of polyps due to limitation of definition of ADR. Therefore, other optimal indicator is needed to better reflect the quality of colonoscopist. In present study, we analyzed the association of several quality indicators such as the total adenoma detected per colonoscopy (APC), adenoma per positive participants (APP), and ADR plus with adenoma missed rate (AMR). Method: Patients who underwent more than two total colonoscopy for screening, surveillance within 36 months in Korea University Ansan Hospital between January 2011 and February 2016 were included. AMR and adenoma more than 5-mm miss rate (AMR > 5mm) were calculated from 5 endoscopists who performed total colonoscopy more than 40 times as a first colonoscopist. ADR, APC, APP, and ADR plus were calculated from 100 colonoscopic results that were randomly selected from total colonoscopy performed by each colonoscopist. Results: A total of 238 patients aged ≥ 40 years were analyzed retrospectively. Mean age was 59.6 years, and male was 63.4%. And mean time interval between colonscopic exams was 18.4 months. There were no significant differences in age, sex, bowel preparation quality, and mean time interval between colonoscopic exams among five endoscopists. AMR was 0.31, 0.44, 0.48, 0.35, and 0.27. AMR > 5 mm was 0.24, 0.23, 0.22, 0.39, and 0.17, respectively. AMR was not significantly correlated with all quality indicators. Whereas APC exhibited a strong inverse correlation with AMR > 5 mm (r = −0.900, P = 0.037), the other indicators were not significantly correlated with AMR > 5 mm (r for ADR = −0.700, P = 0.188; r for ADR plus = −0.800, P = 0.104, r for APP = −0.300, P = 0.624). Conclusion: APC had significant negative association with AMR > 5 mm. APC might be a better quality indicator for a meticulous colonoscopist.
# P-0960
Validation of the ColonFlag CRC performance in the detection of colorectal cancer in the Hong Kong (HK) population: A retrospective case–control study
Simon Ng1, Thomas Lam1, Ran Goshen2, Eran Choman2, Efrat Muller2, Tal Sagiv2, Martin Wong1 and Joseph Sung1
1Institute of Digestive Disease, The Chinese University of Hong Kong, Hong Kong; 2Medial EarlySign Ltd., Israel
Background: Colorectal cancer (CRC) is the third most common cancer and the second leading cause of cancer deaths. The incidence of CRC is rising at an alarming pace in Asian urban societies such as Hong Kong, involving about 5000 new incidences per year. The goals of CRC screening include early detection and removal of precancerous growths. Screening reduces mortality both by decreasing incidence and by detecting cancers at curable stages. Still, the vast majority of CRC cases are not being diagnosed through screening programs, mainly due to failure of individuals to adhere to screening guidelines. Therefore, risk scores for CRC screening have been developed to expedite participation in screening programs. Unfortunately, many of those failed to present a discriminatory power and commonly relate to lifetime risk, rather than current actual risk. ColonFlag uses available complete blood count (CBC) data, age, and sex to provide a score, thus flagging patients to be referred for expedited assessment. Methods: A retrospective observational study (2006–2014) of 500 individuals above 40 y of age diagnosed with CRC and additional 2500 controls with no record of cancer. Cases and controls had at least one CBC available prior to diagnosis. Results: Sensitivity was calculated to be 35.6% at a false positive rate of 5% (success criterion was pre-defined to be ≥ 35%) representing a relative risk of 12.5. The model's AUC (ages 50–75) for CBC test results available up to 6 months prior to the cancer detection, and 6–12 months prior to detection was similar to 2 other previously studied populations (UK and Israel (IL)) (0.78-HK, 0.79-UK, 0.82-IL, and 0.76-HK, 0.75-UK, 0.77-IL, accordingly). Good performance of model was documented for curable CRC stages. Conclusion: These results demonstrate the robustness of the ColonFlag model in flagging individuals at an increased risk to be expedited for CRC screening.
# P-0972
Abdominal tuberculosis: A case series
Ian Homer Y Cua and Roxanne Mae C Butal
Institute of Digestive and Liver Diseases, Saint Luke's Medical Center, E. Rodriguez Sr. Blvd, Quezon City, Philippines
Background: Tuberculosis (TB) remains a major global health problem with extrapulmonary tuberculosis (EPTB) accounting for 1 in 5 registered TB cases. Abdominal TB is the 6th most prevalent presentation of EPTB. It often mimics many other gastrointestinal diseases and confers significant morbidity and mortality; thus, a high index of suspicion is important. Clinical Presentation: First case is a 21/F initially presenting as acute appendicitis who was re-admitted after 2 weeks for small intestinal obstruction. Second case is a 31/M admitted for epigastric pain who subsequently developed massive hematochezia on his 6th hospital day. The 3rd case is a 19/M with 4-month history of undocumented fever, afternoon sweats, and progressive abdominal distention. Management: All 3 cases were diagnosed via histopathology findings. MTB PCR was also taken for the 2nd and 3rd cases. Standard anti-TB regimen of isoniazid, rifampicin, pyrazinamide, and ethambutol were given to all three cases. The first case, however, underwent exploratory laparotomy, right hemicolectomy with ileostomy, and creation of mucus fistula. Conclusion and Recommendations: Abdominal tuberculosis presents with protean manifestations. Neither clinical signs alone nor radiologic, endoscopic, bacteriologic, or histopathologic findings provide a gold standard by themselves in the diagnosis. Thus, it is recommended that knowledge of the different manifestations and investigative findings be coupled with high index of suspicion to avoid missed diagnoses and prevent avoidable morbidity and mortality.
# P-0980
Pembrolizumab, the future of therapy for mismatch repair deficient metastatic colorectal adenocarcinoma: A case report
Katherine Ruth S Oracion
Department of Internal Medicine, St. Lukes Medical Center, Bonifacio Global City, Taguig City, Philippines
Introduction: Pembrolizumab, an anti-programmed death 1 (PD-1) inhibitor is now the focus of cancer research for its favorable clinical response to microsatellite instability (MSI)-high metastatic colorectal cancer. The phase 2 trial by Le et al. showed that on MSI-high colorectal tumors, 40% had objective response (partial or complete response) and 78% showed progression free survival rate after administration of pembrolizumab. Case Description: A 37-year-old male was diagnosed with colon adenocarcinoma with synchronous liver metastasis. He subsequently underwent right hemicolectomy with left hepatectomy. Initial chemotherapy of cetuximab plus 5-FU, folic acid, and oxaliplatin was given that showed complete response on PET CT scan. After three months, surveillance MRI and PET CT scan showed new hypermetabolic lesions at segments IV and V of the liver. Hepatic metastectomy was done, and tumors were analyzed for mismatch repair mutation that revealed MSI-high. Patient underwent subsequent chemotherapy of irinotecan and 5-FU that showed no tumor recurrence on surveillance MRI. Whole body PET CT scan done after 6 months showed hypermetabolic lymphadenopathies at right supraclavicular, right cardiophrenic, and right paracardiac areas with hypermetabolic liver disease at segments V and VIII; hence, 200 mg of pembrolizumab was introduced. After pembrolizumab infusion, surveillance whole body PET CT scan revealed a remarkable metabolic resolution of the previous lymphadenopathies and liver disease at segments V and VIII. Currently, the patient is still on pembrolizumab every 21 days, and no tumor recurrence was noted on surveillance PET CT scan. Conclusion: Although not the primary therapy for colorectal cancer, pembrolizumab showed good response with MSI-high colorectal tumors. Testing of colorectal tumors for MSI may be necessary upon diagnosis, which may predict good response to pembrolizumab. Early introduction of pembrolizumab to advanced colorectal tumors should be considered.
# P-0982
Clinical relevance of HER2 status in patients with residual rectal cancer after preoperative chemoradiotherapy
An Na Seo1, Ghilsuk Yoon1, Vireak Chhun1, Hye Jin Kim2, Jong Min Park3 and Jun Seok Park2
1Department of Pathology, Kyungpook National University Medical Center, Kyungpook National University School of Medicine, Daegu, Korea; 2Colorectal Cancer Center, Kyungpook National University Medical Center, Kyungpook National University School of Medicine, Daegu, Korea; 3Department of Radiology, Central Physical Examination Office, Daegu, Korea
Background: The specific role of human epidermal growth factor receptor-2 (HER2) status in rectal cancers remains unclear. This study therefore aimed to explore clinicopathologic and molecular characteristics and prognostic value of HER2-positivity in residual mid- and/or low-rectal cancers after preoperative chemoradiotherapy (CRT). Methods: Surgical specimens from 145 patients with residual rectal cancer after preoperative CRT between January 2006 and January 2011 at the Kyungpook National University Hospital were used to evaluate HER2 status. HER2 protein expression and gene amplification were determined using immunohistochemistry (IHC) and silver in situ hybridization (SISH) on whole tissue sections, respectively. Polymerase chain reaction was used to analyze molecular characteristics, including microsatellite instability (MSI) and mutations in KRAS exon 2 (codons 12 and 13) and BRAF V600E mutation. Results: Of 139 eligible patients, 8 (5.8%) had HER2 overexpression that was not associated with clinicopathologic characteristics and patient survival, except positive circumferential resection margin (CRM) (P = 0.012). SISH was performed on 24 patient samples with IHC status of 1, 2, or 3. HER2 amplification was identified in 3 patients (2.2%); however, this was also associated with positive CRM (P = 0.009) but not survival (all P > 0.05). Moreover, HER2 overexpression and amplification had no relationship with KRAS or BRAF mutations, and MSI status (all P > 0.05). Conclusion: HER2 positivity was found in a minority of rectal cancer patients and was no significant associations with clinicopathologic and molecular characteristics. Our findings can be helpful in understanding the clinicopathologic bases of HER2 status in rectal cancers.
Acknowledgements: This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (grant number: NRF-2015R1C1A1A02037597).
# P-0985
The inflammation and cancer development of the residual rectal mucosa in the patients of ulcerative colitis after colectomy preserving the rectal mucosa
Hajime Mizukami1, Masashi Matsushima1, Fumio Nakahara1, Jun Nakamura1, Tetsushi Uchida1, Jun Koike1, Muneki Igarashi1, Takayoshi Suzuki1, Soutarou Sadahiro2 and Tetsuya Mine1
1Department of Internal Medicine (Gastroenterology); 2Department of Surgery, Tokai University School of Medicine, Isehara, Japan
Background: Ulcerative colitis (UC) causes inflammation and ulceration mainly in the mucosa and submucosa of colon and rectum. Medical treatment for UC has improved considerably over the years; however, there are still patients who require surgery. Surgery for UC usually involves colectomy and removal of rectal mucosa, but the latter is sometimes skipped because of patients' condition, hope, little inflammation of the rectum, and so on. In such patients, the rectal mucosa remains and inflammation and cancer development may occur. Here, we tried to evaluate the residual rectum in such patients after the surgery. Methods: Using the medical records in the hospital, 17 UC patients who received colectomy preserving the rectal mucosa were elucidated. Fourteen of the 17 patients were followed up with endoscopy and used for the study. Inflammation was evaluated endoscopically by the Mayo scoring system on mucosal findings. Cancer development in the residual mucosa, re-operation, and the treatments were also obtained from the medical records. Results: The median ages of onset and surgery were 41.5 and 47.2 years old, respectively. The reasons of surgery were as follows; 2 for cancer, 2 for stricture suspicious of cancer, 4 for reflactory, 3 for perforation, 1 for toxic megacolon, 1 for extensive bleeding, 1 for unknown. Median follow-up time by endoscopy was 90.4 months. Unfortunately, 92.9% of the patients had an active inflammation in the residual mucosa, most of whom did not received the topical therapy on the remaining rectum. There was no patient of cancer development in the remaining rectum or re-operation. Discussion and Conclusion: Rectal cancer after colectomy without rectal mucosectomy seemed to be rather rare. So if ileal-rectal anastomosis after colectomy was performed on the patients due to old age, or little inflammation of the rectum, and other reasons, periodical endoscopy with proper topical therapies should be necessary.
# P-1002
Long-term outcomes of adalimumab treatment in Korean patients with ulcerative colitis: A hospital-based cohort study
Eun Hye Oh1, Eun Mi Song1, Sun-Ho Lee1, Kiju Chang1, Sung Wook Hwang1,2, Sang Hyoung Park1,2, Dong-Hoon Yang1, Jeong-Sik Byeon1, Seung-Jae Myung1, Suk-Kyun Yang1,2 and Byong Duk Ye1,2
1Department of Gastroenterology; 2Inflammatory Bowel Disease Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
Background: Studies regarding the long-term efficacy of adalimumab treatment in non-Caucasian patients with ulcerative colitis (UC) are still lacking. Methods: We analyzed the long-term clinical outcomes of Korean UC patients on scheduled adalimumab treatment at Asan Medical Center, Seoul, Korea. Primary outcome was adalimumab discontinuation due to non-response to adalimumab and/or colectomy. Probabilities of dose intensification of adalimumab and need for corticosteroid rescue therapy during adalimumab maintenance therapy were also evaluated. Results: Between July 2013 and February 2017, adalimumab treatment was commenced on a total of 69 patients; 47 males (68.1%), median age at initiation of adalimumab, 46 years (interquartile range [IQR], 32–56), and median disease duration, 38.0 months (IQR, 21.5–83.5). Median duration of adalimumab treatment was 9.0 months (IQR, 2.00–24.5). Thirty six (52.2%) were anti-TNF-experienced patients (infliximab 31 [44.9%] and golimumab 5 [7.3%]). Fifteen out of 69 patients (21.7%) were primary non-responders, and 7 out of those (46.7%) finally received colectomy. Out of 54 patients who received scheduled adalimumab maintenance therapy, 10 (18.5%) and 2 (3.7%) stopped adalimumab due to loss of response and adverse events, respectively. Dose intensification of adalimumab was needed for 37.0% (20/54), and corticosteroid rescue therapy was needed for 29.6% (16/54) during scheduled adalimumab maintenance therapy, respectively. Among adalimumab maintenance users, the cumulative survival without adalimumab discontinuation was 79.0% at 1 year and 73.3% at 3 years. Conclusion: The long-term efficacy of adalimumab treatment in a real-life cohort of Korean UC patients appears to be comparable with that in previously published Western studies.
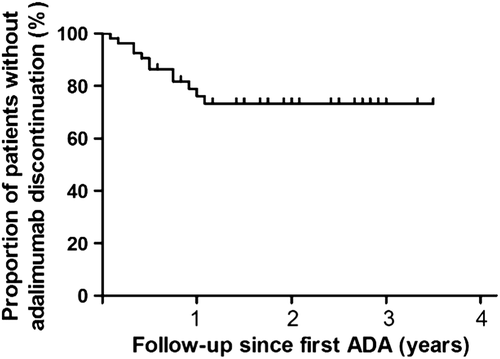
# P-1012
Endoscopic resection of a colonic lipoma presenting with hematochezia
Sung Min Kong, Ji Eun Oh, Sang Goon Shim, Dong Gyu Lee and Ki Hoon Kim
Department of Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
Background: Colonic lipomas are uncommon, benign, fatty tumors that are usually silent clinical course, so they are often found incidentally at colonoscopy, surgery, or autopsy. But lipomas larger than 2 cm can cause symptoms such as abdominal pain, changes in bowel habits, rectal bleeding, obstruction, intussusception, or perforation. We herein report on a case of large lipoma as presented with hematochezia. Case Report: A 31-year-old woman visited our hospital presenting hematochezia and lower abdominal pain. Abdominal computed tomography shows intussusception of sigmoid colon with 3-cm-size intramural lipoma. Sigmoidoscopy was done for an observation and reduction and shows a huge polypoid tumor obstructing the lumen with bleeding and surrounding an edematous mucosa. Follow-up sigmoidoscopy was done and showed a 3-cm-size smooth and pedunculated polyp. We used a standard technique of polypectomy, preceded by submucosal injection with indigo-carmine and epinephrine solution, and fully resected large lipoma. No bleeding or perforation was noted. Pathology examination showed submucosal lipoma with mucosal ulceration. Discussion: In the past, endoscopic resection of colonic lipoma was thought to be higher risk of perforation and bleeding. But several case reports shows colonic lipoma larger than 2 cm can be safely removed using a standard polypectomy technique. Our case shows fully resected lipoma, using safe and effective standard polypectomy technique.
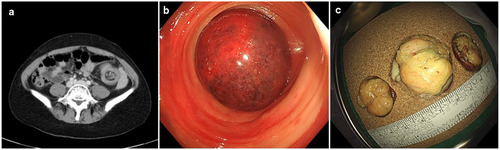
# P-1014
Terrible three's: Recurrent desmoid tumor and colonic polyposis (Gardner's syndrome) in a 32-year-old papillary thyroid cancer survivor
Abegail Latawan-Danasen1, Marie Ellaine Velasquez1 and Joey Lucas2
1Department of Internal Medicine; 2Department of Surgery, Baguio General Hospital and Medical Center, Baguio City, Philippines
Gardner's syndrome (familial adenomatous polyposis FAP + desmoid tumor) related to papillary thyroid carcinoma has been described in some foreign reports, but there is paucity of literature in the Philippines. Desmoid tumors are rare, and papillary thyroid carcinoma has been reported to affect 1–2% of patients with FAP. A 32-year-old Filipina with a history of papillary thyroid carcinoma 14 year prior, and underwent resection of a large (12 × 12 × 10 cm) abdominal desmoid tumor of the rectus abdominis 3 years ago, had a desmoid tumor recurrence that presented as a 2 × 2 cm firm, nodular, slightly tender mass in the anterior abdominal wall. The patient has no lower gastrointestinal symptoms, but due to high suspicion of possible Gardner's syndrome, a pre-operative flexible sigmoidoscopy was done, which confirmed colonic polyposis. Polypectomy revealed a histopathology of tubular adenoma with high-grade dysplasia. Patient underwent surgical resection of a solid nodule, fixed from peritoneum to the fascia, completely excised with safety margin. The histological report confirmed a desmoid tumor composed of fibromatosis. Almost 30% of the thyroid carcinomas associated with FAP have been diagnosed 4–12 years before polyposis was identified. Patients presenting with thyroid carcinoma should be questioned regarding bowel function and family history of gastrointestinal disease. Periodic testing for fecal occult blood and colorectal screening should be recommended. Management of desmoid tumor in FAP is challenging because of no accepted standard treatment and a high incidence of recurrence. Good surgical technique should always be the goal of surgical resection.
# P-1020
A case report of diverticular bleeding that was handled with using over-the-scope-clip (OTSC)
Eisuke Akamine
Department of Gastroenterology, Tane General Hospital, Japan
Over-the-scope clip (OTSC) has been reported to be effective against perforation and bleeding that cannot be handled with the conventional endoscope clip. A 56-year-old male was transported to the emergency department of our hospital with the chief complaint of bowel discharge of fresh blood in March 2017 .At the time of arrival, a blood test showed anemia and simple abdominal CT showed many diverticulums in ascending colon. Diverticular bleeding was suspected, and he was admitted. After admission, his vital signs were stable; therefore, conservative treatment was given. On the second day of admission, massive bleeding occurred and he presented a shock vital. An emergency contrast abdominal CT showed that contrast agent leaked into the ascending colon, and we judged that there was active bleeding; thus, we performed an emergency colonoscopy. The colonoscopy showed arterial bleeding from an exposed vessel of diverticulum in ascending colon, and we stopped bleeding with three clips. After this procedure, bowel discharge was not recognized on the third day of admission. However, he showed intermittent bowel discharge and progressing anemia from the forth day of admission, and we performed colonoscopy again on fifth day of admission. During the colonoscopy, we removed the three clips at the site where we had performed hemostasis and we performed hemostasis again with an OTSC. Then arterial bleeding occurred from the exposed vessel located at the top of the mucosa that was gatherd by OTSC, and we performed additional hemostasis by electrocoagulation. After that, he took good course and was discharged from our hospital on the eighth day of admission. He has gone through without recurrence of bowel discharge until May 2017. The hemostasis with using OTSC for diverticular bleeding is rarely reported. We are going to discuss about this topic with a few literatures and essays.
# P-1022
Evidence-based case report (diagnosis): Effectiveness of colonoscopy capsules compared with conventional colonoscopy in colorectal polyp screening
Azizah Fajar Priarti1, Anindya Larasati1, Fitria Ayu Sutanti Soedjono1, Hans Christian1, Ihsan Hamdani1 and Dian Kusumadewi2
1Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia; 2Department of Community Medicine Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia
Background: Colorectal cancer has incidence rate as much as 15.6 for women and 19.1 for men in 100 000 populations and is the third most cancer in Indonesia. From epidemiological studies, it is known that as many as 30% of colorectal cancer patients in Indonesia are 40 years or younger. The colorectal cancer most often arises from polyps, especially adenomatous polyps. This is shown from the genetic changes that occur in colorectal cancer that can also be found in adenomatous polyps. Adenomatous polyps are common in adults (30%) and in elderly people (50%). Most patients with colorectal polyps have no symptoms, so special tests are required to diagnose them. Colonoscopy is the gold standard to identified this condition. Unfortunately, the test by using conventional colonoscopy is invasive, so that capsule colonoscopy has been developed to identify colorectal cancer. We aimed to find out the effectivity of capsule colonsocopy compared with conventional colonoscopy in colorectal polyp screening. Methods: Literature search using Pubmed, Cochrane, Proquest, Ebsco, and Science Direct databases. The selection of literature is based on determined inclusion and exclusion criteria. The chosen literatures were critically appraised by analyzing the validity, importance, and applicability. Results: Capsule colonoscopy has sensitivity 78–81,25%, specificity 53–94%, positive predictive value 63–92,85%, negative predictive value 56–93%, pre-test probability 28–69/65%, and post-test probability 61–92%. Conclusion: Capsule colonoscopy can be used for colorectal polyp screening because it has high value of sensitivity, not invasive procedure, and more comfortable for patient.
Keywords: capsule colonoscopy, conventional colonoscopy, colorectal polyp screening
# P-1025
Predictive model of biofeedback therapy responsiveness based on three-dimensional integrated pressurized volume in female patients with dyssynergic defecation using high-resolution anorectal manometry
Myeongsook Seo1, Segyeong Joo2, Jungbok Lee3, Hyo Jeong Lee4, Sung Wook Hwang4, Sang Hyoung Park4, Dong-Hoon Yang4, Byong Duk Ye4, Jeong-Sik Byeon4, Suk-Kyun Yang4, Kee Wook Jung4 and Seung-Jae Myung4
1Division of Gastroenterology, Department of Internal Medicine, College of Medicine, Incheon St. Mary's Hospital, the Catholic University of Korea, Incheon, Korea; 2Department of Biomedical Engineering; 3Department of Clinical Epidemiology and Biostatistics; 4Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
Background/Aims: Biofeedback therapy (BFT) is effective treatment of dyssynergic defecation (DD). However, no study has examined the factors that can predict the responsiveness of BFT based on high-resolution manometry (HRAM). We previously suggested the concept of integrated pressurized volume (IPV). Thus, we aimed to construct a predictive model for BFT responders by applying IPV parameter. Methods: Seventy-one female (age: 48–68 years) with DD were enrolled at Asan Medical Center from 2011 to 2015. All subjects underwent initial HRAM and subsequently received BFT. A responder was defined as a subject with at least a three-point improvement on the global bowel satisfaction (GBS) scale after BFT or a two-point increase if the baseline GBS was more than six points. Partial least square regression (PLSR) was conducted to develop a predictive model for BFT responders using IPV parameters, and the PLSR model was assessed using leave-one-out cross validation (LOOCV). Results: Among 71 subjects, 55 (77.5%) showed responsiveness to BFT. There was no significant difference in conventional manometric parameters between responders and non-responders to BFT. Receiver operating characteristic curve analysis demonstrated that the IPV of the upper 1 cm of the anal canal was the best predictor of BFT response (area under the curve [AUC]: 0.74, 95% confidence interval [CI]: 0.63−0.80, P < 0.01). The PLSR model using a linear combination of eight IPV parameters provides an AUC of 0.84 (95% CI: 0.76–0.95, P < 0.01), with a sensitivity of 85.5% and specificity of 62.1%. After LOOCV, the PLSR model was able to correctly discriminate BFT responders, with a sensitivity of 78.9% and specificity of 69.8%. Conclusions: A combination of IPV parameters is superior to conventional parameters in the prediction of responsiveness to BFT. Therefore, IPV parameters can explain the physiology of the anorectal canal more effectively than the conventional parameters.
# P-1043
Efficacy and safety of fecal microbiota therapy in ulcerative colitis: Early experience
Vandana Midha, Arshdeep Singh, Charanpreet S Grewal, Ramit Mahajan, Varun Mehta and Ajit Sood
Background: Gut microbiota is an important player in pathogenesis of ulcerative colitis (UC), and fecal microbiota therapy (FMT) is a promising technique to modulate the gut microbiota. Methods: A single-center prospective study was conducted at Dayanand Medical College and Hospital Ludhiana, India. Patients with moderate to severe steroid dependent active UC (Mayo Clinic score ≥ 4) and those in clinical remission (SCCAI ≤ 2) were planned for multi session FMTs via colonoscope and fecal slurry was delivered close to cecum. FMT sessions were scheduled at baseline, week 2, and then every 4 weeks for six months (total seven sessions) in steroid dependent UC and once every two months (total three sessions) for patients in clinical remission. Primary end point was steroid free clinical remission and maintenance of remission at 24 weeks in the two groups, respectively. Results: Fifty-five patients (40 steroid dependent UC; 15 UC in clinical remission; 29 males; mean age 39.19 ± 9.52 years) were enrolled. The mean duration of disease was 6.37 ± 4.86 years. In the steroid-dependent group, nineteen (47.50%) patients had severe disease (Mayo Clinic score > 10). Twenty-six (65%) patients completed the 24-week follow up, and all (100%) were able to taper and withdraw corticosteroids completely. Eleven (73.33%) patients maintained clinical remission at 52 weeks, whereas ten patients (66.66%) achieved complete mucosal healing. Pain abdomen was the most common adverse event noted followed by transient fever. Conclusion: FMT is an effective therapeutic alternative for steroid dependent active UC and for maintenance of remission. Steroid withdrawal and mucosal healing is demonstrated.
| Steroid Dependent UC | UC in Clinical Remission | |||
|---|---|---|---|---|
| Baseline | Week 24 | Baseline | Week 24 | |
| Number of patients | 40 | 26 | 15 | 15 |
| Mean Age (years) | 36.28 ± 8.23 | — | 42.10 ± 11.82 | — |
| Mean Disease Duration (years) | 7.37±6.89 | — | 5.36 ± 3.78 | — |
| Mean Mayo Score | 10.62 ± 1.51 | 4.98 ± 2.72 | 3.98 ± 1.37 | 1.82 ± 1.16 |
| Mean SCCAI | 8 ± 2.69 | 2.68 ± 1.36 | 1.28 ± 0.72 | 1.05 ± 0.11 |
| Corticosteroids tapered and withdrawn (n)(%) | — | 26 (100) | — | — |
| Mucosal healing (n)(%) | — | 31(77.50) | — | — |
| Clinical Remission (n)(%) | — | 13(32.50%) | — | — |
| Clinical Response (n)(%) | — | 26(100%) | — | — |
| Maintenance of clinical remission (n) (%) | — | — | — | 11 (73.33) |
| Mucosal Healing (n)(%) | — | — | — | 10 (66.66) |
| Total number of FMT sessions (n) | — | 182 | — | 45 |
| Total number of adverse events (n) | ||||
| Pain Abdomen | — | 26 | — | 8 |
| Abdominal Distension | — | 10 | — | 2 |
| Fever | — | 5 | — | 12 |
| Worsening of diarrhea | — | 2 | — | — |
| Flatulence | — | 1 | — | — |
| Borborygmi | — | 1 | — | 2 |
| Fatigue | — | 2 | — | 1 |
# P-1044
Cardiovascular accident risks in 2143 patients with inflammatory bowel diseases: Results from a territory-wide study in Hong Kong
Ting Ting Chan1, Louis Lau1, Whitney Tang1, Francis K L Chan1, Wai K Leung2, Michael K K Li3, Chi M Leung4, Wai Cheung Lao4, Carmen K M Ng5, Fu H Lo6, Alex S F Sze7, Yee T Hui7, Steven W C Tsang8, Edwin H S Shan9, Ching K Loo10, Kam H Chan11, Aric J Hui12, Wai H Chow13, Justin C Y Wu1, Joseph J Y Sung1 and Siew C Ng1
1Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Prince of Wales Hospital; 2Department of Medicine, University of Hong Kong, Queen Mary Hospital; 3Tuen Mun Hospital; 4Pamela Youde Nethersole Eastern Hospital; 5Princess Margaret Hospital; 6United Christian Hospital; 7Queen Elizabeth Hospital; 8Tseung Kwan O Hospital; 9Caritas Medical Centre; 10Kwong Wah Hospital; 11North District Hospital; 12Alice Ho Miu Ling Nethersole Hospital; 13Yan Chai Hospital, Hong Kong
Background: Inflammatory bowel diseases (IBD) composed of Crohn's disease (CD) and ulcerative colitis (UC) are associated with chronic inflammation and induced hypercoagulability. Whether IBD patients have an increased risk of arterial thromboembolism, notably cardiovascular accident (CVA) and coronary heart diseases, is not clear. Objective: This study aimed to assess the CVA incidence, phenotype, and associated risk factors in IBD patients in Hong Kong. Methods: Patients diagnosed with IBD from 1 January 2000 to 31 July 2016 were recruited from the Hong Kong IBD Registry. Relevant medical comorbidities were extracted from the Clinical Data Analysis Reporting Systems (CDARS) of the Hong Kong Hospital Authority covering > 95% of all Hong Kong hospitals. Patients who had a CVA before their diagnosis of IBD were excluded. The principal diagnosis was determined by ICD-9-CM code. Chi-square and independent t-tests were used to compare the demographics between groups, followed by logistic regression models to determine clinically significant risk factors. Results: Amongst 2143 patients (1273 UC; 870 CD; mean age 47.7; 60.1% male) with 17312 person-years follow-up, 24 (1.12%) had developed CVA after the diagnosis of IBD (6 CD; 18 UC). The mean time from diagnosis of IBD to CVA was 73.8 months (IQR, 15.7–127.4 months). IBD subjects who had CVA were older (65 vs 48 years P < 0.01) had more hypertension (29.2% vs 6.9%, P < 0.01), hyperlipidemia (45.8% vs 6.4%, P < 0.01) and atrial fibrillation (8.3% vs 1%, P = 0.002). In univariate analysis, age (OR 1.07, P < 0.01), hypertension (OR 5.52, P < 0.01), hyperlipidemia (OR 7.30, P < 0.01) and atrial fibrillation (OR 8.67, P = 0.005) were significant risk factors. UC patients also had higher CVA risk (odds ratio [OR] 2.07, P = 0.126) compared with CD. In multivariate analysis, age and hyperlipidemia but not UC (adjusted OR 1.05; P = 0.918) remained independently associated with a risk of CVA. Conclusions: In a large population-based Chinese cohort, the risk of CVA in IBD was around 1%, in which UC patients had a higher risk than CD patients. Hypertension, hyperlipidemia, and atrial fibrillation were strong independent risk factors for CVA in IBD, which should be managed and monitored closely.
# P-1047
A case of abdominal Castleman's disease mimicking metastatic lymph node of colon cancer
Dong Hwi Kim, Tae Ho Kim, Chang Whan Kim, Jae Hyuck Chang and Sok Won Han
Gastroenterology Department of Internal Medicine, Bucheon St. Mary's Hospital The Catholic University of Korea
Background: Castleman's disease is a rare lymphoproliferative disorder of unknown etiology. Standard treatment for this lymphoproliferative disorder involving a single node is a complete “en bloc” surgical resection that has proven to be a curative approach. We report a case of abdominal Castleman's disease mimicking metastatic lymph node of colon cancer. Case Presentation: A 57-year-old male was admitted for colon polyp. He underwent colonic endoscopic submucosal dissection (ESD), and biopsy showed adequate adenocarcinoma. Abdominal CT was taken to confirm the presence of distal metastasis of colon cancer. CT showed a single solitary mass in the retroperitoneum [Figure 1]. Laparoscopic excision for a single abdominal mass was performed to differentiate between metastatic LN and other diseases. The tissue was eligible for Castleman's disease. Conclusion: In the case of cancer patients, a single solitary abdominal mass should be distinguished from metastatic lymph node and other lymphoproliferative diseases, such as Castleman's disease.
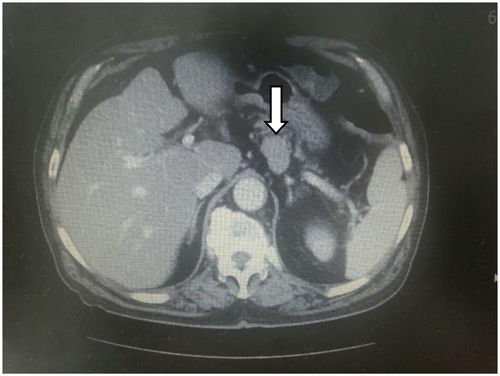
# P-1066
Psychiatric morbidity in patients with inflammatory bowel disease
Rasika Bhamre, Sangeet Sawrav, Shilpa Adarkar, Rishika Sakaria and Shobna J Bhatia
Department of Gastroenterology and Psychiatry, Seth GS Medical College and KEM Hospital, Mumbai, India
Background and Aims: Psychiatric comorbidities are associated with inflammatory bowel disease (IBD). Psychological factors also contribute to worsening of IBD symptoms. The lifetime prevalence of anxiety in patients with IBD ranges from 25–30% in Western population. We conducted an observational study to evaluate the prevalence of depression and anxiety in IBD cases. Methods: Seventy consecutive consenting patients with IBD (62 ulcerative colitis, 8 Crohn's disease [CD]; mean age 36.2 [11.3] years, 40 men) and 100 healthy volunteers (age 31.22 [10.5] years; 44 men) were used as controls. All participants were directed to take self-assessment tests, Patient Health Questionnaire 9 (PHQ9), and Symptom Checklist Anxiety scale (SCL-A20). Participants having a score ≥ 10 on PHQ9, or ≥ 29 on SCL-A20 were administered Depression (HAM-D) or Hamilton Anxiety (HAM-A) scales, respectively. Severity of depression was graded as no depression (HAM-D 0–7), mild (8–16), moderate (17–23), or severe depression (≥ 24). Severity of anxiety was graded as no anxiety (HAM-A 0–5), mild (6–14), moderate (15–27), or severe anxiety (≥ 29). The protocol was approved by the Ethics Committee. Results: The prevalence of depression (34.3% vs 5%, P < 0.0001, OR 9.7) and anxiety (18.6% vs 2%, P = 0.0002, OR 11.17) was higher in patients with IBD as compared with controls. The severity of depression was higher in patients (mean rank 17 vs 7, P = 0.04). The prevalence of depression and anxiety was similar in men and women. The prevalence of depression was not different between UC and CD, and all IBD patients with anxiety had UC. The mean duration of disease and history of corticosteroid treatment or surgery for IBD were not associated with presence of depression or anxiety. Patients with severe CD (CDAI > 450) had more severe depression. Severity of UC did not correlate with severity of anxiety or depression in UC.
Conclusions: Anxiety and depression are more prevalent in IBD patients as compared with healthy individuals.
# P-1068
Interobserver and intraobserver variability in classification of defecatory disorders on high-resolution anorectal manometry
Abhishek Sadalage
Department of Gastroenterology, Seth GS Medical College and K E M Hospital, India
Objective: Defecatory disorders (DD) on anorectal manometry (ARM) are classified into four types based on paradoxical anal contraction, poor anal relaxation, inadequate rectal efforts, or rectal hyposensitivity. There are limited data in intra and interobserver agreement in diagnosis of DD. We assessed intra and interobserver variability in classification of defecatory disorder of manometry data. Methods: ARM tracings of seventy consecutive patients (48 men; mean age 37[15] y), with DD seen over a period of 2 years, were re-analyzed by five observers, blinded to the diagnosis. All observers had minimum 5-year experiences in reporting ARM. One observer re-analyzed the tracings after at least 6 months of initial analysis to assess intraobserver variability. Trace 1.2 software was used for anorectal manometry analysis. K value and Pearson's correlation coefficients were used to assess intra and interobserver variability. Results: The mean duration of symptoms was 3.96 years at presentation, and average stool frequency was 2/day with mean basal pressure 70 (21) mmHg, mean squeeze pressure 138 (63) mmHg, and mean defecation index was 0.64 (0.26). At baseline analysis, 42 patients had type 1 DD, 6 had type 2, 18 had type 3, and 4 had type 4. Intraobserver (experts 1A and 1B) and interobserver variability in classification are shown in the table.
| Inter item correlation matrix ‘k' value/agreement | ||||||
|---|---|---|---|---|---|---|
| Expert 1A | Expert 1B | Expert 2 | Expert 3 | Expert 4 | Expert 5 | |
| Expert 1A | 1.000 | 0.862 | 0.675 | 0.738 | 0.650 | 0.625 |
| Expert 1B | 0.862 | 1.000 | 0.619 | 0.712 | 0.725 | 0.778 |
| Expert 2 | 0.675 | 0.619 | 1.000 | 0.718 | 0.525 | 0.655 |
| Expert 3 | 0.738 | 0.712 | 0.718 | 1.000 | 0.571 | 0.638 |
| Expert 4 | 0.650 | 0.725 | 0.525 | 0.571 | 1.000 | 0.734 |
| Expert 5 | 0.625 | 0.778 | 0.655 | 0.638 | 0.734 | 1.000 |
Conclusion: HRM has good intraobserver agreement and moderate interobserver agreement for classification of defecatory disorders.
# P-1070
Interobserver variability is moderate in classification of defecatory disorders on high-resolution anorectal manometry
Abhishek Sadalage1, Akash Shukla1, Dhiraj Agrawal1, Deepak Gupta1, Philip Abraham2, Megha Meshram1 and Shobna Bhatia1
1Department of Gastroenterology, Seth G S Medical College and K E M Hospital, Mumbai; 2Division of Gastroenterology, PD Hinduja Hospital, Mumbai, India
Objective: Defecatory disorders (DD) on anorectal manometry (ARM) are classified into four types based on paradoxical anal contraction, poor anal relaxation, inadequate rectal efforts, or rectal hyposensitivity. There are limited data in intra and interobserver agreement in diagnosis of DD. We assessed intra and interobserver variability in classification of defecatory disorder of manometry data. Methods: ARM tracings of seventy consecutive patients (48 men; mean age 37[15] y), with DD seen over a period of 2 years, were re-analyzed by five observers, blinded to the diagnosis. All observers had minimum 5-year experiences in reporting ARM. One observer re-analyzed the tracings after at least 6 months of initial analysis to assess intraobserver variability. Trace 1.2 software was used for anorectal manometry analysis. K value and Pearson's correlation coefficients were used to assess intra and interobserver variability. Results: The mean duration of symptoms was 3.96 years, and average stool frequency was 2/day; mean basal pressure 70 (21) mmHg, mean squeeze pressure 138 (63) mmHg, and mean defecation index was 0.64 (0.26). At baseline analysis, 42 patients had type 1 DD, 6 had type 2, 18 had type 3, and 4 had type 4. Intraobserver (expert 1A and 1B) and interobserver variability in classification are shown in the table.
| Table: Inter item correlation matrix ‘k' value/agreement | ||||||
|---|---|---|---|---|---|---|
| Expert 1A | Expert 1B | Expert 2 | Expert 3 | Expert 4 | Expert 5 | |
| Expert 1A | 1.000 | 0.862 | 0.675 | 0.738 | 0.650 | 0.625 |
| Expert 1B | 0.862 | 1.000 | 0.619 | 0.712 | 0.725 | 0.778 |
| Expert 2 | 0.675 | 0.619 | 1.000 | 0.718 | 0.525 | 0.655 |
| Expert 3 | 0.738 | 0.712 | 0.718 | 1.000 | 0.571 | 0.638 |
| Expert 4 | 0.650 | 0.725 | 0.525 | 0.571 | 1.000 | 0.734 |
| Expert 5 | 0.625 | 0.778 | 0.655 | 0.638 | 0.734 | 1.000 |
Conclusion: HRM has good intraobserver agreement and moderate interobserver agreement for classification of defecatory disorders.
# P-1072
Long-term gastrointestinal consequences are frequent following sporadic acute infectious diarrhea in a tropical country: A prospective cohort study
M Masudur Rahman1, Uday Chand Ghoshal2, Shamima Sultana3, M D Golam Kibria1, Nigar Sultana1, Zeenat Arefin Khan3, Faruque Ahmed1, Mahmud Hasan4, Tahmeed Ahmed3 and Shafiqul Alam Sarker3
1Department of Gastroenterology, Dhaka Medical College and Hospital, Dhaka, Bangladesh; 2Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India; 3Nutrition and Clinical Service Division, International Center for Diarrheal Disease Research, Bangladesh; 4Gastroliver Foundation, Dhaka, Bangladesh
Background: Post-infection irritable bowel syndrome (PI-IBS) and functional dyspepsia (PI-FD) have been reported mostly from temperate countries. No report on PI-IBS excluded post-infection malabsorption (PI-MAS). Hence, we studied (i) the frequency of continuing bowel dysfunction after acute gastroenteritis (AGE), (ii) predictors of its occurrence, and (iii) frequency of PI-MAS among patients with PI-IBS. Methods: A total of 345 consecutive subjects each with AGE and age- and gender-matched healthy controls presenting to Dhaka Hospital, ICDDR,B Bangladesh were followed up 3 times monthly for 12 months using a translated-validated Rome III questionnaire and diagnosed using Rome III criteria. Fecal microbiological studies were performed among patients not receiving antibiotic recently. Patients developing PI-IBS were diagnosed as PI-MAS if 2/3 of the following tests were abnormal (i) D-xylose hydrogen breath test, (ii) fecal fat microscopy (Sudan III stain), and (iii) histopathology of endoscopic duodenal biopsy. Results: Patients were comparable with controls in age and gender (female 41% in each group). During follow-up, 57 (16.5%) and 25 (7.4%) patients; 9 (2.6%) and 2 (0.6%) controls developed IBS and FD, [relative risk 6.4 (95% CI 3.2–12.7) and 12.5 (95% CI 3.0–52.4)], respectively (P = 0.000). On univariate analysis, weight loss and presence of FD were the risk factors for PI-IBS. Stool samples were cultured and subjected to PCR for pathogens in 245/345 patients. The frequency of PI-IBS following Vibrio cholera, E. coli and other bacterial infection (i.e., Salmonella, Shigella, Campylobactor, and Aeromonas) was 20%, 16.3%, and 23.5%, respectively, and was comparable between Vibrio cholerae or other types of bacterial or mixed infection. Of 23/57 (40%) patients with PI-IBS undergoing tests for malabsorption, 2 (9%) had PI-MAS. Conclusion: Bowel dysfunction is common after AGE. PI-FD and weight loss are the risk factors for development of PI-IBS. Vibrio cholerae infection is a risk factor for PI-IBS. About 10% patients fulfilling PI-IBS criteria have PI-MAS.