Genetic markers for methazolamide-induced Stevens–Johnson syndrome and toxic epidermal necrolysis
Abstract
Linked article: M. Jiang et al. J Eur Acad Dermatol Venereol 2022; 36: 873–880. https://doi.org/10.1111/jdv.17980.
Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are uncommon, life-threatening, severe cutaneous adverse reactions characterized by varying extents of epidermal necrosis and mucosal breakdown.1 The mortality rate associated with SJS/TEN depends on the severity of the disease, with typical mortality rates of between 1% and 5% for SJS and as high as 25%–30% for TEN.1
Methazolamide (MTZ), a sulfonamide derivative, is a potent carbonic anhydrase inhibitor that is commonly used to treat increased intraocular pressure in patients with glaucoma. MTZ-induced SJS/TEN (MTZ-SJS/TEN) has been reported primarily in patients of Japanese, Korean and Han Chinese descent.2, 3 Because glaucoma is a common condition among older adults, and age is a risk factor that predicts mortality in patients with SJS/TEN, identifying risk factors associated with the development of MTZ-SJS/TEN is necessary when treating patients with glaucoma to prevent this adverse event. HLA-B59:01 has previously been associated with MTZ-SJS/TEN development; however, a comprehensive, exome-wide study remains necessary to identify other candidate genes.3
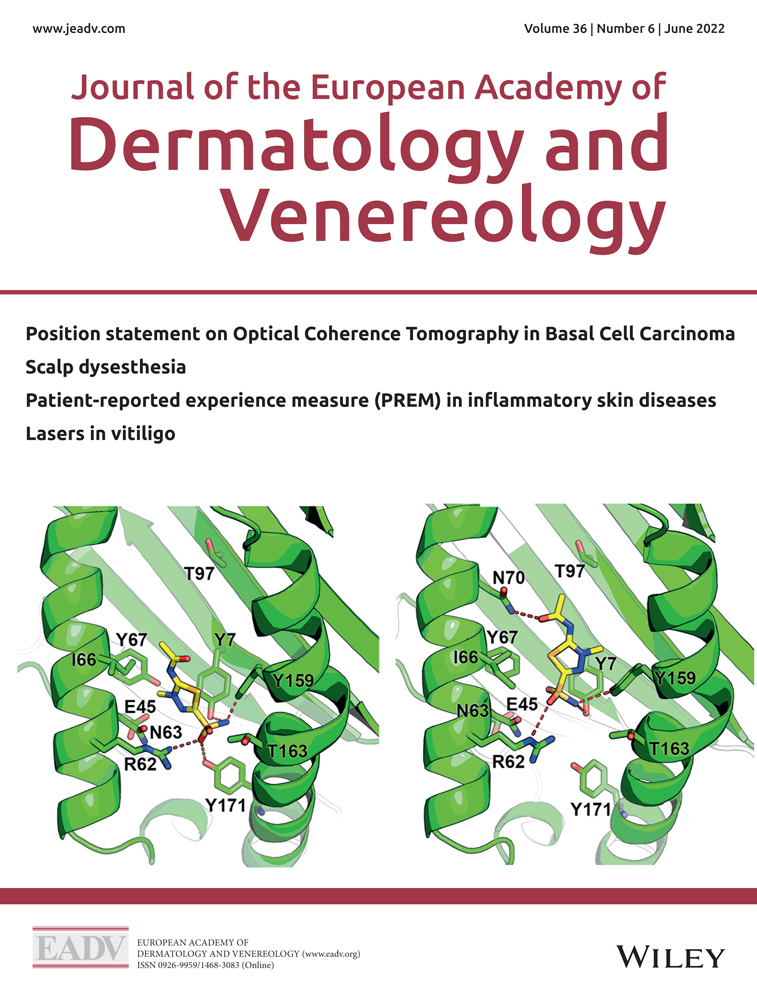
In this issue of JEADV, Jiang et al. conducted both an exome-wide association study and an HLA-based association analysis in patients with MTZ-SJS/TEN.3 They found that HLA-B*59:01 and HLA-B*55:02 are associated with MTZ-SJS/TEN, potentially due to the E45–L116 motif, which is uniquely shared by HLA-B*59:01 and HLA-B*55:02. Molecular docking analysis revealed that MTZ binds stably to the binding pockets of HLA-B*59:01 and HLA-B*55:02 due to hydrogen bonds and low steric hindrance. They also identified the E45-L116 motif, defined by the rs41562914–rs12697944 haplotype, as an outstanding predictor of MTZ-SJS/TEN development, with a sensitivity and specificity of 89% and 96%, respectively.3
However, this study only identified MTZ-SJS/TEN-predictive genetic markers in a Han Chinese population, and these associations may not generalize to other populations, as different ethnic groups may carry different genetic markers for MTZ-SJS/TEN. Previous studies have shown that the genetic screening for HLA-B*1502 prior to prescribing carbamazepine could effectively prevent SJS/TEN development.4, 5 Further studies remain necessary to determine the efficacy of prospective screening for the rs41562914(A)–rs12697944(A) haplotype, combined with the use of alternative drug treatment for carriers of this risk factor, to confirm the decreased incidence of SJS/TEN in Han Chinese patients carrying this genetic marker.
Conflicts of interest
None declared.
Funding source
This work was supported by a grant from the Ministry of Science and Technology of Taiwan (MOST 109-2314-B-002-052-MY3).
Open Research
Data availability statement
None