The Periodontal Benefits of Alveolar Ridge Augmentation With Xenograft Following Third Molar Extraction: A Randomised Controlled Trial
Funding: This work was supported by Doctor of Clinical Dentistry Student Research Grant from The University of Queensland and The University of Queensland School of Dentistry and Colgate-Palmolive Student Research Grant. Biomaterials (Bio-Oss Collagen) were donated by Geistlich Pharma Australia.
ABSTRACT
Aim
To evaluate the effect of deproteinised bovine bone mineral with collagen (DBBM-C) grafting on periodontal healing at the distal aspect of the second molar (D2M) during adjacent third molar extraction.
Material and Methods
Forty-two sites in 28 patients were randomly allocated into two groups. The test group (18 sites) received DBBM-C grafting during extraction, whereas the control group (24 sites) received extraction alone. The patients were reviewed 6 months postoperatively, and the D2M and extraction sites were evaluated by both linear and volumetric cone beam computed tomography measurements.
Results
Nine patients dropped out (14 sites) and two patients were excluded (4 sites), leaving a total of 17 patients (24 sites) who were reviewed after 6 months. Both groups showed significant healing when examining the linear measurements (except at the disto-lingual aspect of the second molar) and the defined volumes of interest. There were, however, no significant differences between the groups in the linear or volumetric outcome analyses.
Conclusions
Within the limitations of the study, the use of DBBM-C during third molar extraction did not improve periodontal healing at the D2M. This trial was registered in April 2020 in the Australian New Zealand Clinical Trials Registry under code ACTRN12620000497909 (https://anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12620000497909).
1 Introduction
Third molar impaction has a reported worldwide prevalence of 24.4% (Carter and Worthington 2016). Retained third molars rarely remain healthy, with deep periodontal pockets often detected around both the third and adjacent second molars (Vandeplas et al. 2020).
The periodontal condition often improves after the extraction of impacted third molars (Blakey et al. 2009). In some cases, the periodontal defects associated with the distal aspect of the second molar (D2M) were seen to persist even after extraction. Kugelberg (1990) reported that 44.4% of subjects aged 26 years or older had persistent intrabony defects exceeding 4 mm at the 4-year follow-up post extraction. Similarly, Kan et al. (2002) found that 67% of sites exhibited probing depths ≥ 5 mm even 6–36 months after extraction. These findings show that a substantial portion of third molar extraction sites heal with residual periodontal defects.
Risk factors for persistent periodontal defects after third molar extraction have been identified. Kugelberg et al. (1991) identified pre-existing defects at the time of extraction as the strongest predictor of postoperative intrabony defects. Additional risk factors include impaction depth (Montero and Mazzaglia 2011), mesio-angular impaction (Kan et al. 2002) and eruption status (Dodson 2004). These residual deep periodontal pockets may predispose the second molar to periodontal disease progression and tooth loss (Matuliene et al. 2008).
Consequently, different regenerative approaches have been investigated as adjuncts to third molar extraction, to prevent and/or treat the periodontal defects at the D2M associated with third molar impaction (Corinaldesi et al. 2011; Sammartino et al. 2009). In a split-mouth randomised controlled trial, guided tissue regeneration with a polyglycolic acid/polylactic acid membrane resulted in a significant reduction in residual intrabony defects at 12 months (Aimetti et al. 2007). The use of deproteinised bovine bone mineral (DBBM) combined with a resorbable collagen membrane has also been evaluated in a randomised controlled trial, which resulted in statistically significant probing pocket depth (PPD) reduction on the disto-buccal aspect of the second molar (Hassan et al. 2012).
Currently, no particular treatment protocol has been shown to provide superior healing (Camps-Font et al. 2018), and there is limited evidence for additional benefits with the use of xenografts in the management of defects associated with the D2M. A systematic review examining the benefit of xenograft grafting at the time of third molar extraction (Toledano-Serrabona et al. 2021) could identify only three studies, emphasising the need for more well-conducted investigations with larger sample sizes and longer follow-up.
The aim of this study was therefore to evaluate the effect of DBBM-C grafting at the time of third molar extraction on the prevalence of persistent periodontal defects associated with the adjacent second molar, as measured by radiographic bone loss.
2 Materials and Methods
2.1 Experimental Design and Setting
The study was designed as a 6-month randomised controlled trial and was registered, during April 2020, in the Australian New Zealand Clinical Trials Registry (ACTRN12620000497909). Consultation and recruitment were conducted in a private practice setting, and surgery was performed at The Wesley Hospital in Brisbane (Australia). The study took place between June 2020 and July 2023.
2.2 Ethics Statement
Ethical approval was obtained from The University of Queensland Human Research Ethics Committee (2020000215) and the UnitingCare Health Human Research Ethics Committee (2009) and was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013. All participants provided informed consent. This study followed the reporting criteria set out by the CONSORT guidelines.
2.3 Study Population
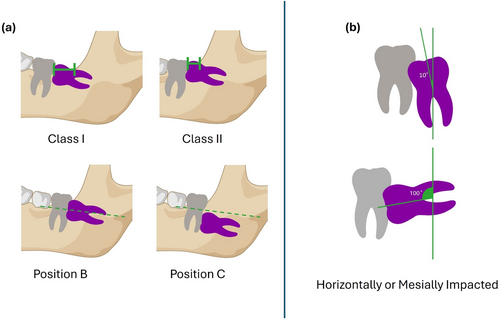
Patients attending the surgical rooms of two experienced specialist oral and maxillofacial surgeons (N.J., J.T.H.) for extraction of impacted mandibular third molars were screened and recruited. Patients were included if they met the following inclusion criteria: (i) one or two unerupted mandibular third molars with a class I or II and position B or C impaction, according to the Pell and Gregory classification (Pell 1933) and with a horizontal or mesio-angular impaction according to Winter's classification (Winter 1926), as illustrated in Figure A1; (ii) radiographic bone loss ≥ 5 mm on the D2M, measured from the cemento-enamel junction (CEJ) to the alveolar crest on preoperative cone beam computed tomography (CBCT); (iii) able to tolerate extraction; (iv) American Society of Anaesthesiologists Class I physical status; and (v) aged between 18 and 45 years.
The exclusion criteria were as follows: (i) disto-angular impaction or extraction that required extensive surgery; (ii) a history of diagnosed periodontal disease (> 2 mm of clinical attachment loss); (iii) pathology that required more than just extraction and primary wound closure; (iv) full-mouth plaque score ≥ 40%; and (v) unwilling to return for review.
2.4 Randomisation and Study Groups
Randomisation used computerised sequence generation. Allocation was concealed from the surgeon until after tooth removal, by using sealed envelopes. In the test group, the alveolar socket was grafted with a 90% deproteinised bovine bone mineral and 10% porcine collagen graft (DBBM-C, Geistlich Pharma, Wolhusen, Switzerland), firmly compacted against the exposed root, cemento-enamel junction (CEJ) and approximately 1 mm above the CEJ. The control group received extraction alone. Both test and control sites were then closed with simple interrupted sutures and primary wound closure.
2.5 Surgical Procedure
Two surgeons (N.J., J.T.H.) performed extractions using a standardised, minimally traumatic approach to preserve the buccal cortex. If necessary, roots were sectioned with a bur and removed separately. Careful curettage of the socket was performed. Subjects were excluded if lingual bone perforation occurred during extraction. Subjects were prescribed postoperative analgesics and advised to rinse with 0.2% chlorhexidine mouthwash twice daily for 2 weeks. Other postoperative instructions included a soft diet for 2 weeks and avoiding any brushing directly on the surgical site for 1 week. Patients were reviewed after 2 weeks and sutures were removed. Any incidence of postoperative complications was recorded.
2.6 Clinical Outcome Variables
A clinical examination was performed at 6 months by an investigator, who was blinded (S.Q.), using a UNC-15 probe (Hu-Friedy, Chicago, IL). Full-mouth Plaque Index (PlI) (Silness and Löe 1964) and Gingival Index (GI) (Loe and Silness 1963) around the adjacent mandibular second molar were recorded. PPD disto-buccal (DB), distal (D) and disto-lingual (DL) of the second molar were also measured.
2.7 Radiographic Outcome Variables
CBCT scans (i-CAT 17-19DX) were carried out at baseline and 6 months postoperatively. DICOM files were analysed using the 3D Slicer 5.2.2 software with the SlicerIGT extension for point registration. A blinded examiner (S.Q.) performed all measurements. The angle and classification of impaction were determined using the baseline CBCT imaging. Technical imaging details appear in Data S1.
2.7.1 Linear CBCT Measurements
The bone height adjacent to the mandibular second molar (CEJ-C) was examined by measuring the distance between the CEJ and the most coronal part of the alveolar crest (Figure 1). This was performed at the DB, D and DL positions around the second molar, as well as at the slice with the most bone loss at baseline (worst slice).
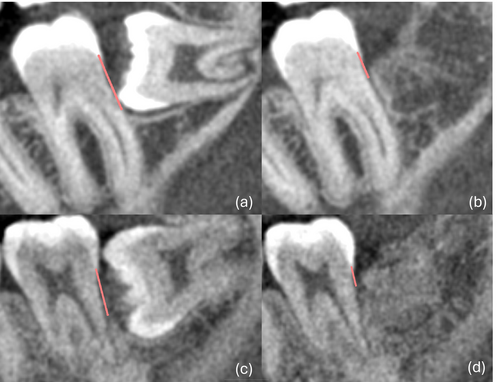
2.7.2 Volumetric CBCT Measurements
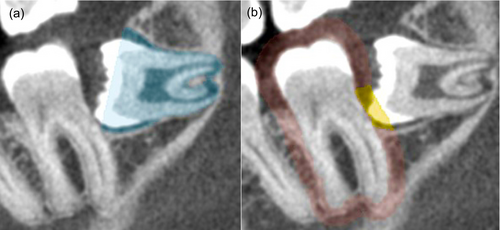
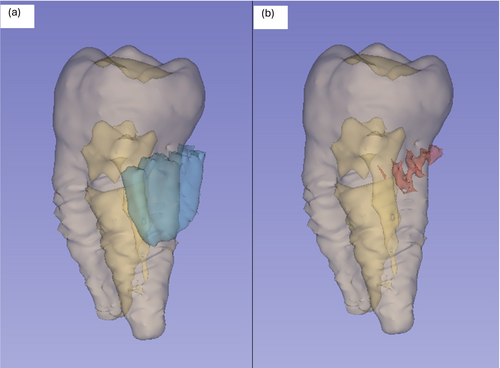
Two volumes of interest were defined, one to represent socket healing (SHV), that is, the components of the impacted third molar which were reasonably assumed would heal with bone infill after third molar removal, and the other to represent periodontal healing (PHV) around the D2M.
As shown in Figure 2, the SHV comprised the volume of the third molar and follicle which was bound coronally by the mesial and distal bone peaks of the socket. PHV was defined as the volume of the third molar tooth and follicle, bound coronally by a plane parallel and 2 mm apical to a line drawn through the mesial and distal CEJ on each slice. The lateral boundaries of the PHV were defined by a 2-mm perimeter around the second molar (Figures 2 and 3). Segmentation of these regions of interest was done slice by slice from the buccal to the lingual extent of the tooth.
The primary outcome measures were CEJ-C, SHV and PHV. The secondary outcome measure was postoperative PPD.
2.8 Data Analysis
Sample size determination was based on linear bone height measurements (Singh et al. 2015), which reported control group values of 2.12 ± 0.666 mm and test group values of 1.00 ± 0.408 mm at 6 months. Using a more conservative standard deviation (0.666) and the observed difference between means (1.12 mm), we calculated an effect size (Cohen's d) of 1.68. With a significance level of 0.05 (two-tailed) and 90% power for an unpaired t-test, we determined a minimum requirement of nine sites per group. To account for potential dropouts and non-normal distribution in this small sample, we set a target of 18 sites per group.
Comparisons between preoperative and postoperative measurements were conducted by reporting results at the site level, with robust standard errors used to adjust for clustering effect due to repeated measures. Intragroup changes were analysed using paired t-tests adjusted for repeated measures, examining changes within each group at 6 months. Between-group differences were examined using linear regression, which was equivalent to an independent t-test but allowed for adjustment of standard errors and clustering at the subject level. Normality was assessed using skewness and kurtosis tests.
Intra- and inter-rater reliability for CEJ-C and PHV measurements was assessed using ICC on seven randomly selected sites. Detailed methodology appears in Data S2.
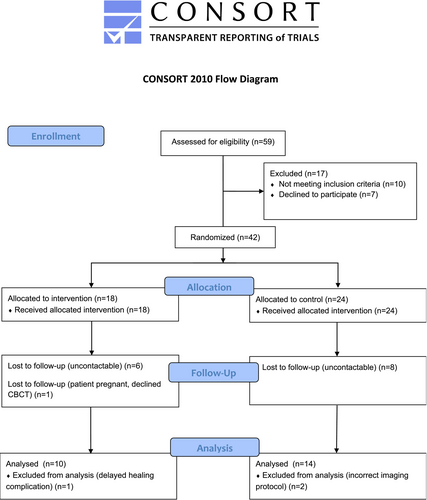
3 Results
As shown in Figure 4, 28 patients (n = 42 sites) were randomised into two groups (n = 18 test and n = 24 control), all of whom received their assigned treatment. Nine patients (n = 6 test and n = 8 control) were lost at the follow-up appointment, as they were uncontactable. Additionally, one patient (n = 1 test) was excluded, as the patient declined further radiographic imaging. During the analysis, one patient (n = 2 control) was excluded because of the use of an incorrect imaging protocol, which significantly varied from the initial protocol. One site in the test group was excluded because of a delayed healing complication; however, the other site in this patient (n = 1 control) was included in the analyses. Therefore, 17 patients (n = 10 test and n = 14 control) in total were included for the data analyses.
The mean age of the participants was 24.9 years. Most teeth had a Class II (83.3%), Position B (95.83%) Pell and Gregory classification of impaction. All the teeth were either mesio-angularly or horizontally impacted with a mean impaction angle of 63.4° ± 17.79° in the control group and 57.54° ± 21.59° in the test group (Table 1). The mean time between surgery and the review was 6.79 ± 0.73 months.
| Variable | Total | Control (n = 14 sites) | Test (n = 10 sites) |
|---|---|---|---|
| Patient characteristics | |||
| Gender | |||
| Male | 7 patients (12 sites) | 6 sites (50%) | 6 sites (50%) |
| Female | 10 patients (12 sites) | 8 sites (66.67%) | 4 sites (33.33%) |
| Age, years | |||
| Mean ± SD | 24.9 ± 6.0 | 24.6 ± 5.9 | 25.4 ± 6.5 |
| Site characteristics | |||
| Pell and Gregory class (I, II or III) | |||
| I | 0 | 0 | 0 |
| II | 20 | 12 | 8 |
| III | 4 | 2 | 2 |
| Pell and Gregory position (A, B or C) | |||
| A | 0 | 0 | 0 |
| B | 23 | 14 | 9 |
| C | 1 | 0 | 1 |
| Angle of impaction (degrees, Mean ± SD) | 63.4 ± 17.79 | 57.54 ± 21.59 | |
| CEJ-C—worst slice (mm, mean ± SD) | 6.78 ± 1.59 | 7.22 ± 2.23 | |
| CEJ-C—DB position (mm, mean ± SD) | 5.51 ± 2.30 | 6.13 ± 2.47 | |
| CEJ-C—D position (mm, mean ± SD) | 4.91 ± 1.51 | 5.91 ± 2.32 | |
| CEJ-C—DL position (mm, mean ± SD) | 2.20 ± 1.13 | 2.13 ± 1.24 | |
| SHV (mm3, mean ± SD) | 503 ± 247 | 657 ± 294 | |
| PHV (mm3, mean ± SD) | 49.4 ± 14.4 | 61.5 ± 25.6 | |
- Note: n = number of sites, CEJ-C expressed in mm; SHV, PHV expressed in mm3, mean age calculated and reported at the site level.
- Abbreviations: CEJ-C, linear measurement from the cemento-enamel junction to the bone crest; D, distal; DB, disto-buccal; DL disto-lingual; PHV, periodontal healing volume of interest; SD, standard deviation; SHV, socket healing volume of interest.
3.1 Linear Outcome Measures
At baseline, the CEJ-C measurements DB of the D2M had the most bone loss when compared to the D and DL sites, 5.51 ± 2.30 and 6.13 ± 2.47 mm for the control and test groups, respectively (Table 1). Improvement in CEJ-C-measured DL of the D2M was not statistically significant at the 6-month review in either the control (p = 0.60) or the test (p = 0.62) groups. However, the bone loss DL at baseline was minimal, as shown by CEJ-C measurements of 2.20 ± 1.13 in the control group and 2.13 ± 1.24 in the test group. All other measurements, in both groups, showed significant reduction in CEJ-C at the 6-month review (Table 2). There were no significant differences in terms of CEJ-C between test and control groups.
| Baseline–6 months | Mean | SD | Mean diff. (Control – test) | p | 95% CI |
|---|---|---|---|---|---|
| Linear CBCT measurements | |||||
| CEJ-C—worst slice (mm) | |||||
| Control | −2.59* | 1.01 | 1.49 | 0.08 | (−3.18 to 0.20) |
| Test | −4.08** | 2.49 | |||
| CEJ-C—DB position (mm) | |||||
| Control | −1.63* | 1.24 | 1.63 | 0.10 | (−3.60 to 0.33) |
| Test | −3.26** | 2.84 | |||
| CEJ-C—D position (mm) | |||||
| Control | −1.75* | 1.03 | 1.01 | 0.29 | (−2.94 to 0.92) |
| Test | −2.76** | 2.40 | |||
| CEJ-C—DL position (mm) | |||||
| Control | −0.08 | 0.58 | 0.14 | 0.78 | (−1.16 to 0.89) |
| Test | −0.22 | 1.39 | |||
| Volumetric CBCT measurements | |||||
| SHV (%) | |||||
| Control | 86.21* | 12.57 | −2.61 | 0.27 | (−2.26 to 7.48) |
| Test | 88.82** | 7.11 | |||
| PHV (%) | |||||
| Control | 73.60* | 20.95 | −1.47 | 0.80 | (−10.69 to 13.64) |
| Test | 75.07** | 13.93 | |||
- Note: CEJ-C expressed in mm, SHV, PHV expressed as percentage. The comparison of measurements between baseline and 6 months was done with paired t-tests and between groups with linear regression, adjusted for repeated measures using robust standard errors.
- Abbreviations: CEJ-C, linear measurement from the cemento-enamel junction to the bone crest; CI, confidence interval; D, distal; DB, disto-buccal; DL, disto-lingual; PHV, periodontal healing volume of interest; SD, standard deviation; SHV, socket healing volume of interest.
- * p < 0.001 for intra-group comparison with baseline for control group.
- ** p < 0.001 for intra-group comparison with baseline for test group.
3.2 Volumetric Outcome Measures
There was statistically significant radiographic healing at 6 months for the SHV, with 86.21% ± 12.57% and 88.82% ± 7.11% bone infill for the control and test groups, respectively (Table 2). PHV also improved significantly in both the control and test groups, with 73.60% ± 20.95% bone infill in the control group and 75.07% ± 13.93% in the test group. There were no significant differences in volumetric outcome variables between the groups.
3.3 Clinical Outcome Variables
PlI, GI and PPD were not recorded at baseline. At 6 months, the mean full-mouth PlI was 1.03 ± 0.59 and 1.20 ± 0.63, and the mean GI was 1.04 ± 0.66 and 1 ± 0.54 in the control and test groups, respectively. When comparing PPD at 6 months between the control and test groups at the DB, D, DL and the mean of all three measurements, there were no significant differences (Table 3).
| Mean | SD | Mean diff. | p | 95% CI | |
|---|---|---|---|---|---|
| PPD—DB position (mm) | |||||
| Control | 3.43 | 1.34 | −0.97 | 0.31 | (−1.00 to 2.94) |
| Test | 4.4 | 2.63 | |||
| PPD—D position (mm) | |||||
| Control | 3.64 | 0.93 | −0.16 | 0.71 | (−0.73 to 1.04) |
| Test | 3.8 | 1.32 | |||
| PPD—DL position (mm) | |||||
| Control | 2.86 | 1.03 | −0.24 | 0.59 | (−0.70 to 1.19) |
| Test | 3.1 | 0.88 | |||
| Mean PPD (mm) | |||||
| Control | 3.31 | 0.65 | −0.46 | 0.27 | (−0.39 to 1.30) |
| Test | 3.77 | 1.20 | |||
- Note: PPD expressed as mm. The comparison of PPD measurements taken at the 6-month review was done with linear regression, adjusted for repeated measures using robust standard errors.
- Abbreviations: CI, confidence interval; D, distal; DB, disto-buccal; DL, disto-lingual; PPD, probing pocket depth; SD, standard deviation.
3.4 Intra- and Inter-Rater Reliability
For the intra-rater reliability analysis, ICC was 0.95 (95% CI: 0.90–0.98) for CEJ-C measurements, demonstrating excellent agreement. PHV measurements also demonstrated excellent intra-rater agreement, with ICC = 0.94 (95% CI: 0.79–0.99). For the inter-rater reliability analysis, ICC was 0.88 (95% CI: 0.73–0.95) for CEJ-C measurements, demonstrating good agreement and ICC was 0.97 (95% CI: 0.87–1.00) for PHV measurements, demonstrating excellent agreement.
4 Discussion
Periodontal defects may persist even after extraction in some patients. Kugelberg (1990) demonstrated that PPD ≥ 7 mm and intrabony defects ≥ 4 mm associated with D2M were present even 4 years after third molar removal, with a higher prevalence in those over 26 years of age. While various grafting materials have been investigated to address these defects (Hassan et al. 2012; Sammartino et al. 2009), findings are conflicting and the benefits of alveolar ridge augmentation with DBBM following third molar extractions have been scarcely reported. Sammartino et al. (2009) found significant benefits with DBBM grafting when examining PPD reduction, which were maintained after 6 years of follow-up. Conversely, a study by de Melo et al. (2015) found little benefit in grafting beyond extraction alone in terms of PPD. The latter study was limited by the short follow-up of 60 days. To our knowledge, this is the first study investigating the periodontal benefits of DBBM-C grafting. DBBM-C grafting may provide advantages in terms of handling (Llanos et al. 2019; Wu et al. 2022), which may be of particular importance when dealing with the limited access associated with lower third molar extraction sites.
In this investigation, we found that DBBM-C grafting following extraction of impacted mandibular third molars, in a high-risk population, does not result in improved periodontal healing in terms of radiographic outcome measures. We found no significant difference in CEJ-C between DBBM-C grafting and extraction alone. Even when analysing the slice with the most severe baseline bone loss, to account for variations in impaction patterns and ridge dimensional changes, no significant differences were detected between the groups. These results align with a systematic review by Camps-Font et al. (2018), which found that osseous grafting alone did not result in benefits in terms of alveolar bone gain. Improvements in CEJ-C in the control group are consistent with previous reports (Inocêncio Faria et al. 2013).
The strength of the current trial lies in the inclusion of only deep pre-existing intrabony defects > 4 mm, which represents a risk factor for poor periodontal healing after extraction (Kugelberg et al. 1991). Our inclusion of mesio-angular or horizontal impaction patterns further focused on high-risk cases (Kan et al. 2002). These criteria created a homogeneous population where treatment effects would be most detectable, thereby enhancing statistical power despite a modest sample size. Our study addresses several shortcomings associated with PPD measurements, 2D imaging and previous CBCT studies.
Specific to the context of impacted lower third molars, PPD measurement is the most widely used clinical parameter but has shown poor reliability and reproducibility due to the presence of the impacted third molar crown, which often impeded the periodontal probe's ability to reach the base of the pocket (Karapataki, Hugoson, Falk, et al. 2000). The current study consequently did not report PPD measurements at baseline and did not find significant differences in PPD measurements 6 months postoperatively.
Measurements utilising 2D imaging have been shown to suffer from distortion, resulting in reduced reproducibility (Hausmann and Allen 1997) and underestimation of the prevalence and extent of periodontal defects (Dias et al. 2020). Linear measurements on CBCT imaging have been shown to be more accurate and reliable than 2D imaging (Sherrard et al. 2010) and the accuracy of volumetric measurements on CBCT imaging is comparable to measurements made using micro-computed tomography (Wang et al. 2011). To date, however, studies reporting linear CBCT measurements in the context of D2M periodontal healing have not reported adequately on their methodologies and/or the reliability of their measurements (Kim et al. 2023; Minya et al. 2021). We examined the reliability of CEJ-C measurements, which showed excellent intra- and inter-rater reliability.
Previous studies using volumetric CBCT measures of periodontal healing had short follow-up periods (2–3 months), employed side-by-side analysis or lacked details on image registration (Ritto et al. 2019; Tadic et al. 2023). For the SHV, the mesial and distal bone peaks of the socket were chosen as the superior border. This had been previously shown to dictate the level to which the bone crest heals after extraction (Schropp et al. 2003). The described PHV used is a modification of those described by Yan et al. (2020). When deciding on the parameters defining the PHV, 2 mm apical to the CEJ was used as the superior border, as this has previously been shown to be the physiological upper limit of the CEJ-C measurement (Hausmann et al. 1991). The use of a 2-mm perimeter around the second molar was used by Yan et al. (2020), who demonstrated that a volume bound by a 2-mm perimeter has a strong correlation with linear radiographic measurements and PPD. In the current study, PHV measurements were consistent with the results obtained from linear measurements and showed good intra- and excellent inter-rater reliability. Further validation of the proposed volume of interest is required to examine the association with periodontal health clinically.
Although studies have shown benefit with membrane use at the time of extraction, consistent with the principles of guided tissue regeneration (Aimetti and Romano 2007), studies have also reported that its use is technically difficult (Karapataki, Hugoson, and Kugelberg 2000). Consequently, this study explored the benefit of DBBM-C alone, which may be more practical clinically. DBBM-C has shown the ability to result in periodontal regeneration in preclinical studies (Nevins et al. 2003). Future studies examining the benefits of DBBM-C used in combination with other biologics such as enamel matrix proteins may be of interest. However, a recent systematic review found that the use of biologics as adjuncts in alveolar ridge preservation did not result in superior clinical or radiographic outcomes (Suárez-López Del Amo and Monje 2022).
Of interest, qualitative examination of the 6-month CBCT scans revealed more frequent distinct lamina dura in control sites compared to test sites. Since radiographic crestal lamina dura is positively associated with periodontal stability (Rams et al. 1994), this may suggest differences in periodontal healing patterns between groups. However, as this observation was not part of our original assessment protocol, and because of the lack of baseline PPD, its significance remains uncertain and requires further investigation.
The findings of this study have important clinical implications. While DBBM-C grafting alone did not enhance periodontal healing in high-risk cases, this information can help clinicians to avoid unnecessary procedures and associated costs. However, the persistent periodontal defects observed in both groups underscore the need for alternative regenerative approaches in this challenging clinical scenario.
4.1 Limitations
The current study was limited by high dropout rates and a small sample size. Recruitment and retention of patients in the study were hindered by the coronavirus pandemic and associated quarantines. The short follow-up of 6 months may not have been adequate, as radiographic healing of extraction sockets continues between 6 and 12 months (Hassan et al. 2012) and is delayed by advanced radiographic bone loss at the time of extraction (Bertl et al. 2018).
The absence of preoperative PPD measurements represents a methodological limitation, which restricts interpretation of the postoperative periodontal status. While our radiographic analysis provided objective assessment of hard-tissue healing, baseline and follow-up PPD data would have offered additional information on the soft-tissue component of periodontal health. Future investigations using both measurement types could provide a more complete picture of periodontal healing, despite the known difficulties in obtaining reliable PPD readings adjacent to impacted third molars.
Although a standardised protocol for extraction was implemented, primary closure was not always possible; in such instances, this likely impeded the regenerative outcome of the intervention (Wang and Boyapati 2006). Morphological characteristics of the extraction socket, such as the number of residual walls, may also have affected wound stability and consequently the capacity for regeneration (Melcher 1976). These covariates were not recorded and may have confounded the results. Furthermore, scaling and root planing of the D2M, which is recommended prior to and at the time of regeneration (Sanz et al. 2020), was not performed and likely hampered regenerative outcomes.
Partial tooth/root volumetric analysis is also reliant on CEJ identification and has been shown to have decreased accuracy and reproducibility compared to whole-tooth measurements (Forst et al. 2014). Artefacts resulting from radio-dense restorative materials, movement and partial volume effect may also introduce further variability (Schulze et al. 2011).
5 Conclusion
Within the limitations of the study, the use of DBBM-C during third molar extraction did not improve periodontal healing at the D2M. Further research is needed to explore alternative regenerative approaches and to provide effective and predictable management options for periodontal defects associated with third molar extraction.
Author Contributions
All authors contributed to concept and design of the study as well as technical or material support. N.J., S.S.Q. and R.D. contributed to acquisition, analysis or interpretation of data. S.S.Q. drafted the manuscript. All authors contributed to critical revision of the manuscript for important intellectual content. R.S.B.L. and S.I. supervised the study.
Acknowledgements
Open access publishing facilitated by The University of Queensland, as part of the Wiley - The University of Queensland agreement via the Council of Australian University Librarians.
Ethics Statement
The study protocol was reviewed and approved by The University of Queensland Human Research Ethics Committee (2020000215) and UnitingCare Health Human Research Ethics Committee (2009), and was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.