Clinical and patient-centred long-term results of root coverage using the envelope technique in a private practice setting: 10-year results—A case series
Funding information
The study was self-funded by the authors and their institutions.
Abstract
Aim
Evaluation of long-term results after connective tissue graft (CTG) using the envelope technique and the effect on patient-centred outcomes (Oral Health Impact Profile: OHIP) in a private practice setting.
Materials and Methods
Fifteen patients (11 female, mean age: 45.0 ± 8.88 years) underwent root coverage procedure using a CTG involving maxillary Miller class I teeth. Pre-operatively, 3 and 120 ± 12 months after surgery, all patients were examined, completed OHIP questionnaire, and were asked to assess improvement and their satisfaction with the results of surgery. All procedures were performed by the same investigator.
Results
Recession depth at 3 months of 1.19 ± 0.93 mm was reduced to that of 0.63 ± 0.64 mm at 120 ± 12 months after surgery (p = .117). Recession width (−1.23 ± 2.27 mm) decreased as well (p = .117), while relative root coverage increased from 48.46 ± 32.18% at 3 months to 71.22 ± 30.86% at 120 months (p = .011). The number of cases with complete root coverage increased from two (15.4%) to six (40.0%) from 3 to 120 months (p = .046). OHIP score (12.07 ± 10.15) did not change after 10 years (12.13 ± 9.86, p = .889). Ten years after surgery, 12 patients (80%) reported they would make the decision again to undergo CTG transplantation.
Conclusions
Within the limitations of the study design with a high risk of bias in a practice setting, long-term stability of recession reduction, OHIP and patient-perceived satisfaction remained stable over 10 years.
Clinical Relevance
Scientific rationale for the study: The primary aim of plastic periodontal therapy is to achieve long-term stability of root coverage of denuded root surfaces and of patients’ satisfaction. Thus, this study considered the long-term stability of root coverage and patient-centred outcomes after connective tissue grafting using the envelope technique.
Principal findings: Application of the envelope technique achieved long-term stable clinical results and patient-centred outcomes in 15 singular Miller class I defect cases at 10 years after using a connetctive tissue graft (CTG).
Practical implications: Root coverage and patient-centred outcomes may be maintained in a stable fashion at 10 years after therapy with CTG using the envelope technique in a practice setting.
1 INTRODUCTION
The literature provides a long list of available procedures and related modifications to cover singular facial recessions (Cairo, 2017; Tonetti & Jepsen, 2014), including coronal/lateral advanced flaps (Allen & Miller, 1989; Grupe, 1966; Zucchelli, Cesari, Amore, Montebugnoli, & De Sanctis, 2004), connective tissue grafts (CTGs; Raetzke, 1985), free gingival grafts (FGGs; Nabers, 1966) and guided tissue regeneration (GTR; Tinti, Vincenzi, Cortellini, Pini Prato, & Clauser, 1992). One of these options, the so-called envelope technique, was first described by Raetzke in 1985. Its unique feature was the absence of vertical relief incisions in combination with a CTG from the palate (Raetzke, 1985).
Both short-term (Abundo, Corrente, Ambrois, Perelli, & Savio, 2009; Hansmeier & Eickholz, 2010; Ratka-Krüger, Neukranz, & Raetzke, 1999) and long-term (Nickles, Ratka-Krüger, Neukranz, Raetzke, & Eickholz, 2010; Rossberg, Eickholz, Raetzke, & Ratka-Krüger, 2008) results of this surgical approach have already been reported. Ratka-Krüger et al. in 1999 detailed a reduction in the recession depth (RD) by 2.9 mm with a mean relative root coverage (RC) of 74.1% (Ratka-Krüger et al., 1999) after 3 months. Abundo et al. in 2009 found a significant RD reduction of 3.12 mm after 12 months with a mean relative RC of 95.54% (Abundo et al., 2009). In 2008, Rossberg et al. demonstrated a significant RD reduction of 2.7 mm and a mean RC of 89.7% over 10 years on average (Rossberg et al., 2008). These results were only partially confirmed 2 years later, however, with a mean RD reduction of 2.07 mm but a lower mean relative RC of 43.7% (Nickles et al., 2010).
In addition to long-term clinical data, systematic reviews and meta-analyses are increasingly demanding the collection of patient-centred outcomes (Cairo et al., 2016; Chambrone et al., 2018). The patient's aesthetic perception plays a superior role, since a desire for improved aesthetics is the main indication for plastic periodontal surgery (Cairo, 2017; Mounssif et al., 2018). Both long-term studies mentioned above showed that all treated patients were satisfied with the final resulting RC at 10 years after using the envelope technique (Nickles et al., 2010; Rossberg et al., 2008).
Further, patient-centred parameters were collected using the validated OHIP (Oral Health Impact Profile) questionnaire. This questionnaire was developed to metrically evaluate oral health-related quality of life. The OHIP-49 version, with 49 items, is the most widely used tool in international clinical research (John, Patrick, & Slade, 2002) and has therefore been translated into various languages including German (OHIP-G49). The questionnaire primarily asks about oral problems and symptoms.
Accordingly, the objective of this prospective clinical trial was to generate clinical and patient-centred long-term results following envelope technique application in a private practice setting.
The associated hypothesis was that the mean RC and patient-centred outcomes would remain stable at 10 years after surgical recession coverage of Miller class I defects (Miller, 1985) completed using the envelope technique.
2 MATERIALS AND METHODS
2.1 Patients
This study re-examined 16 patients who had already been reported on at 3 months after root coverage (Hansmeier & Eickholz, 2010). These patients underwent root coverage with the envelope technique between February and May 2008. Two additional patients underwent surgery who were not included in the original report (Hansmeier & Eickholz, 2010) because they were not available for re-examination within the originally established time window for the study. The entire study was conducted in a private practice setting (UH).
- Presence of a maxillary Miller class I or II defect
- Age ≥18 years
- Absence of a periodontal probing depth (PPD) of ≥5 mm at the tooth with the recession and its adjacent teeth
- Oral hygiene instructions and approximal plaque index (API) of less than 35% prior to surgery (Lange, Plagmann, Eenboom, & Promesberger, 1977)
- Presence of written informed consent.
- Pregnancy
- Haemorrhagic disorders
- Anticoagulative therapy.
After 120 ± 12 months, patients were included for follow-up if they agreed to participate again. All patients were informed about the study project and agreed to participate by signing an informed consent form. The study was approved by the Institutional Review Board for Human Studies of the Medical Faculty of the Johann Wolfgang Goethe-University (approval no. 320/07, amendment no. 126/17). For the 10-year re-examination, the study was registered with the German Register of Clinical Trials (Deutsches Register Klinischer Studien; ID no. DRKS00016912; URL: https://www.drks.de). Ten years ago, registration in a clinical trial register was less common than is true today. Thus, a retrospective registration (10 years after baseline) was done.
P.E. and H.P. conceived the ideas; P.R. described the envelope technique for the first time and inspired the study; U.H. performed the surgeries and examinations; U.H. and H.P. collected the data; H.P. and B.D. analysed the data; H.P. and K.N. led the writing; and all authors contributed to the writing.
2.2 Periodontal surgery
The surgical procedure performed herein has already been described in detail (Hansmeier & Eickholz, 2010) and will therefore only be briefly summarized in the following. All surgical procedures and examinations were performed by one operator (UH) and followed the surgical protocol described by Raetzke (Raetzke, 1985).
After local anaesthesia (Ultracain DS forte; Sanofi/Aventis), the root surface was scaled and planed and a 0.5-mm-wide epithelial margin was excised around the recession. This was followed by the preparation of the envelope as an undermining, circumferential and supraperiosteal tunnel preparation around the recession with a scalpel (no. 15c or MB69). At the palatal harvesting site, a paramarginal incision was made at a point approximately 2 mm from the gingival margin of the premolars and molars. A second, parallel incision was made 1–2 mm further palatinally. Both incisions were at least twice the length of the recession width and were made converging and parallel to the underlying bone. Thus, the removal of a tissue wedge was possible. The epithelial margin of the removed graft was excised extraorally, and the CTG was inserted into the prepared envelope. The CTG covered the entire root surface and at least 50% of the CTG was submerged in the envelope. Then, it was fixed with tissue adhesive (Histoacryl; B. Braun Melsungen AG). The recipient site was covered with a wound dressing (COE-Pak; GC America Inc.), and the harvesting site was sutured (Permilene 6/0 DSMP13; B. Braun Melsungen AG).
2.3 Post-surgical phase
All patients were instructed to refrain from mechanical plaque control for 1 week at the surgical sites. For chemical plaque control, they rinsed twice daily for 2 min with 0.2% chlorhexidine gluconate solution (Corsodyl; Fink GmbH) over the given period. Ibuprofen 200 mg (which is available as over-the-counter medication in Germany) was recommended to all patients as an on-demand medication. After 1 week, the wound dressing and sutures were removed. Patients were not advised to use a special brushing technique. All participants were given the recommendation to attend regular supportive periodontal therapy (SPT) at least once a year. A risk-adapted determination of the SPT interval was not established.
2.4 Clinical examinations
- Recession depth (RD): RD was measured as the distance from the CEJ to the most apical point of the buccal gingival margin
- Recession width (RW): The periodontal probe was placed horizontally at the most apical point of the buccal CEJ for measurement, and the distance from the gingival margin mesial to a point distal of the recession was measured
- Width of the keratinized gingiva (gingival width, GW): The GW was measured as the most apical point of the buccal gingival margin to the mucogingival border after staining with 3% iodine solution
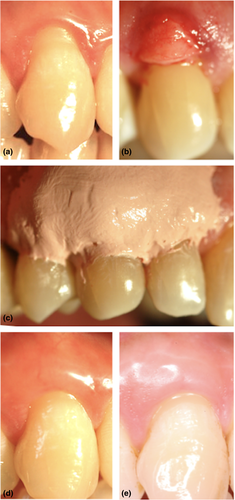
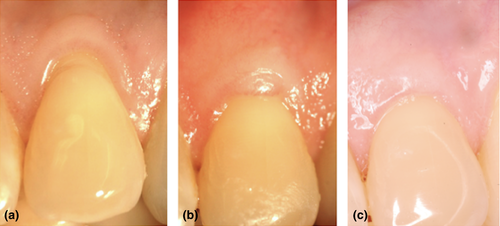
In addition, all study participants were asked about their smoking habits and classified as either non-smokers (never smoked), former smokers (quit smoking) or active smokers (currently smoking). Pre-surgically, after 3 and 120 ± 12 months, photographs of the test teeth were taken (Figures 1 and 2).
2.5 Patient-centred parameters
- Aesthetics
- Hypersensitivity
- Root caries.
- Would you undergo this procedure again (yes/no)?
- How much did your original reason to undergo this procedure improve [grades: A (very good) to F (insufficient)]?
- How satisfied are you with the outcome of the procedure [grades: A (very good) to F (insufficient)]?
2.6 Statistics
The patient was regarded as the statistical unit. Each patient contributed one recession to the statistical evaluation. If more than one recession was treated in one patient, the recession with the highest initial RD was included in all cases.
The primary outcome parameter of this study was the change in relative root coverage (relative RC, %) from 3 to 120 ± 12 months post-operatively. Relative RC was calculated as RD reduction at the corresponding time divided by the baseline RD and multiplied by 100. OHIP score was considered the secondary endpoint. All other clinical (PPD, RD, RW, GW, amount of complete root coverage) and patient-centred parameters were considered as control variables.
After testing for normal distribution using the Kolmogorov–Smirnov test, all quantitative parameters were recorded descriptively as medians, interquartile ranges (IQRs) or ranges.
The reduction of RD was calculated as the difference in millimetres between the pre- and post-surgical RD. The percentage of complete RC (CRC) achieved after 3 and 120 ± 12 months was calculated as the number of completely (100%) covered root surfaces at each re-examination point divided by the total number of defects and multiplied by 100.
The presence of plaque was expressed as the number of such at all three points in time. Comparisons for all parameters at the different follow-up times were made using the Friedman test. Means ± standard deviations were additionally calculated to provide comparability with other studies.
Due to the additional recruitment of two patients who did not participate in the follow-up examination for the first 3 months, the value determinations after 3 months are based on 13 patients and those after 120 ± 12 months are based on 15 patients. In order to identify possible risk factors for the change in mean relative RC between 3 and 120 ± 12 months, a linear regression analysis with the factors RD, RW, GW and PPD at baseline and after 3 months was performed.
Changes in OHIP-49 over time were analysed by using the Wilcoxon signed-rank test. The patient-centred outcomes for improvement and satisfaction were compared with the decision to undergo surgery again using the chi-square test.
p Values were not adjusted for multiple testing. A significance level of .05 was assumed. All statistical analyses were performed with computer software (IBM® SPSS® Statistics 24 software package; IBM Corp.).
3 RESULTS
3.1 Patients
Originally, 18 patients were recruited for this study and underwent surgery. Three months after surgery, 16 were available for re-examination within the designated time window of the original study. Two additional patients underwent RC surgery but were not available for the 3-month re-examination within the designated time window and were not reported in the 3-month analysis (Hansmeier & Eickholz, 2010). These two additional patients could be recruited for the 10-year follow-up, however. In total, after 120 ± 12 months (9.50 ± 0.11 years), 15 patients (11 females) with an average age of 45.0 ± 8.88 years contributing 15 maxillary Miller class I recessions participated in the study. Three of the 16 patients who reported after 3 months were not available at 10 years after surgery (Hansmeier & Eickholz, 2010): one lost the treated tooth due to progressive PPD and two other patients refused to participate after 10 years. All follow-up examinations took place between September and November 2017. Most patients opted for the procedure for aesthetic reasons (9) or for hypersensitivity (10); only one patient pursued such for the management of root caries. Five patients made double statements, in which both aesthetics and hypersensitivity were reported. Three (20%) of the patients examined were former smokers at the time of surgery, and all others (80%) were reported to be non-smokers. One of the original non-smokers stated at 120 ± 12 months to be a former smoker. Five patients (33.33%) complied with regular SPT (≥1 SPT per year; Table 1).
| Patient | Age at surgery | Tooth | Regular recalls | Number of recalls | Smoking status (at surgery) |
|---|---|---|---|---|---|
| 1 | 40 | 23 | − | 2 | Never |
| 2 | 57 | 23 | − | 8 | Former |
| 3 | 71 | 23 | + | 15 | Never |
| 4 | 46 | 24 | + | 12 | Never |
| 5 | 50 | 22 | + | 10 | Never |
| 6 | 44 | 13 | − | 8 | Never |
| 7 | 40 | 13 | − | 7 | Never |
| 8 | 39 | 23 | − | 8 | Never |
| 9 | 46 | 13 | − | 6 | Never |
| 10 | 41 | 14 | + | 16 | Former |
| 11 | 45 | 13 | + | 11 | Former |
| 12 | 33 | 16 | − | 4 | Never |
| 13 | 43 | 14 | − | 6 | Never |
| 14 | 39 | 13 | − | 9 | Never |
| 15 | 38 | 16 | − | 2 | Never |
|
BL (n = 15) |
3 months (n = 13) |
Change BL-3 months |
p |
120 months (n = 15) |
Change BL-120 months |
p |
Change 3–120 months |
p | |
|---|---|---|---|---|---|---|---|---|---|
| OHIP-G49 | 17.07 ± 12.49 | 12.07 ± 10.15 | −5.00 ± 7.86 | .027 | 12.13 ± 9.86 | −4.93 ± 11.81 | .128 | 0.31 ± 7.79 | .889 |
| 15.0 (7.0–24.0, 2.0–45.0) | 10.0 (4.0–19.0, 1.0–35.0) | 3.0 (0–11.5, −10.0–18–0) | 8.0 (5.0–20.0, 2.0–34.0) | 2.0 (−2.0–16.0, −15.0–30.0) | 2.0 (−4.0–6.0, −18.0–12.0) |
Note
- −, irregular recall; +, regular recall.
- Abbreviation: BL, baseline.
3.2 Clinical parameters
Table 2 provides clinical parameters. Focused on the long-term stability of the results achieved after 120 months, plaque control deteriorated (median: 0, IQR: 0–.0, range: 0–1.0; p = .014). PPD at 3 months (range: 1.0–2.0 mm) increased significantly to 120 ± 12 months by 0.50 mm (IQR: −1.0 to 0, range: −2.0 to 0; p = .004). In contrast, mean RD at 3 months (range: 0–3.0 mm) decreased by 0.5 mm (IQR: 0–1.25, range: −1.5 to 2.5; p < .117). RW as well as GW at 3 and 120 ± 12 months remained stable between both re-examinations [RW: 1.0 mm (IQR: 0–2.75, range: −4.0–5.0; p = .117), GW: 0.5 mm (IQR: −0.25 to 1.0, range: −1.5 to 1.5; p = .468)]. The average relative RC increased significantly to 75.0% (IQR: 50.0–100, range: 0–100) after 120 ± 12 months as compared with 40.0% (IQR: 22.5–75.0, range: 0–100) after 3 months over the follow-up period (p = .011). The number of cases of CRC rose from two (15.38%) to six (40.0%; p = .097; Table 2).
|
BL (n = 15) |
3 months (n = 13) |
Change BL-3 months (n = 13) |
p |
120 months (n = 15) |
Change BL-120 months (n = 15) |
p |
Change 3-120 months (n = 13) |
p | |
|---|---|---|---|---|---|---|---|---|---|
| Plaque index | 0.0 ± 0.0 | 0.31 ± 0.48 | 0.31 ± 0.48 | .014 | 0.0 ± 0.0 | 0.0 ± 0.0 | 1.000 | 0.31 ± 0.48 | .014 |
| 0 (0–0, 0–0) | 0 (0–1.0, 0–1.0) | 0 (0–1.0, 0–1.0) | 0 (0–0, 0–0) | 0 (0–0, 0–0) | 0 (0–1.0, 0–1.0) | ||||
| Pocket probing depth [mm] | 1.50 ± 0.51 | 1.38 ± 0.51 | −0.12 ± 0.58 | .922 | 2.00 ± 0.71 | 0.50 ± 0.42 | .006 | 0.62 ± 0.72 | .004 |
| 1.5 (1.0–1.5, 1.0–3.0) | 1.0 (1.0–2.0, 1.0–2.0) | 0 (−0.25–0.5, −1.0–1.0) | 2.0 (1.5–2.0, 1.0–4.0) | −0.5 (−1.0- −0.5, −1.0–0.5) | −0.5 (−1.0–0, −2.0–0) | ||||
| Recession depth [mm] | 2.20 ± 0.53 | 1.19 ± 0.93 | −1.04 ± 0.66 | .006 | 0.63 ± 0.64 | −1.57 ± 0.75 | <.001 | −0.58 ± 1.00 | .117 |
| 2.0 (2–2.5, 1.5–3.0) | 1.5 (0.5–1.75, 0–3.0) | 1.0 (0.5–1.5, 0–2.0) | 0.5 (0–1.0, 0–2.0) | 1.5 (1.0–2.0, 0–3.0) | 0.5 (0–1.25, −1.5–2.5) | ||||
| Width [mm] | 4.47 ± 0.92 | 3.08 ± 2.09 | −1.42 ± 1.38 | .014 | 1.80 ± 1.90 | −2.60 ± 1.57 | <.001 | −1.23 ± 2.27 | .117 |
| 4.5 (4.0–5.0, 3.5–7.0) | 3.0 (1.25–4.25, 0–7.0) | 1.0 (0.25–2.5, 0–4.0) | 2.0 (0–4.0, 0–5.0) | 3.0 (1.5–4.0, 0–5.0) | 1.0 (0–2.75, −4.0–5.0) | ||||
| Gingival width [mm] | 4.10 ± 1.11 | 4.96 ± 0.99 | 0.81 ± 0.97 | .011 | 4.80 ± 1.44 | 0.70 ± 1.31 | .057 | −0.19 ± 0.93 | .468 |
| 4.0 (3.0–5.0, 2.5–6.0) | 5.5 (4.25–5.75, 3.0–6.0) | 1.0 (−0.25–1.0, −1.0–2.0) | 5.0 (3.5–6.0, 2.5–7.0) | 1.0 (0–1.5, −2.0–3.0) | 0.5 (−0.25–1.0, −1.5–1.5) | ||||
| RC 3 months | RC 120 months | Change 3–120 months | |||||||
| Relative root coverage [%] | 48.46 ± 32.18 | 71.22 ± 30.86 | 24.10 ± 41.51 | .011 | |||||
| 40.0 (22.5–75.0, 0–100) | 75.0 (50.0–100, 0–100) | 20.0 (0–57.5, −75.0–83.33) | |||||||
| Amount of complete root coverage [n/%] | 2 (15.38) | 6 (40.0) | .046 | ||||||
- Abbreviations: BL, baseline; RC, root coverage.
Linear regression analysis showed a significant positive association between RD (p = .035) and GW (p = .037) after 3 months based on the change of relative RC from 3 to 120 ± 12 months after surgery (Table 3).
| Parameter | Regression coefficient | SD | p |
|---|---|---|---|
| Baseline | |||
| Constant | −107.32 | 29.0 | .257 |
| Recession depth | 14.85 | 29.0 | .622 |
| Recession width | 13.48 | 19.19 | .502 |
| Gingival width | 11.30 | 11.74 | .364 |
| Pocket probing depth | −5.51 | 29.14 | .855 |
| 3 months | |||
| Constant | −154.46 | 49.12 | .014 |
| Recession depth | 33.24 | 5.90 | .035 |
| Recession width | −0.33 | 5.90 | .957 |
| Gingival width | 20.11 | 8.05 | .037 |
| Pocket probing depth | 28.09 | 17.88 | .155 |
- Abbreviation: SD, standard deviation.
3.3 Patient-centred outcomes
Table 1 provides data on patient-centred parameters (OHIP) for all follow-up points. Ten years after using a CTG, 12 (80%) out of 15 patients said they would decide to undergo this procedure again. With regard to both patient satisfaction (Table 4a) and improvement in the final result perceived by the patients (Table 4b), 14 patients (93.33%) awarded school grades A through C. The one patient who scored with lower school grades (E for satisfaction, D for improvement) is one of the two cases with recession coverage on a first molar (tooth no. 16). Neither for satisfaction (p = .140) nor for improvement (p = .913) were the patients’ scores significantly different regarding the final result after 10 years as compared with the scores at 3 months after surgery. A correlation between school grade and the decision to undergo surgery again after 10 years could not be demonstrated (satisfaction: p = .153/improvement: p = .172/R2: 0.375).
| (a) | ||||
|---|---|---|---|---|
| School grades for satisfaction | Patient would undergo surgery again (3 months, n = 13) | Patient would undergo surgery again (120 months, n = 15) | ||
| No | Yes | No | Yes | |
| A (very good) | 0 | 4 | 0 | 4 |
| B | 2 | 4 | 2 | 7 |
| C | 0 | 1 | 0 | 1 |
| D | 2 | 0 | 0 | 0 |
| E | 0 | 0 | 1 | 0 |
| F (insufficient) | 0 | 0 | 0 | 0 |
| (b) | ||||
|---|---|---|---|---|
| School grades for improvement | No | Yes | No | Yes |
| A (very good) | 0 | 1 | 0 | 3 |
| B | 2 | 7 | 2 | 8 |
| C | 0 | 1 | 0 | 1 |
| D | 2 | 0 | 1 | 0 |
| E | 0 | 0 | 0 | 0 |
| F (insufficient) | 0 | 0 | 0 | 0 |
4 DISCUSSION
Facilitating comparability to other studies, this discussion focuses on mean values rather than on medians. Short-term observations after surgery according to the envelope technique suggested significant improvements of the mean RD of 2.50–3.21 mm after 3–12 months (Abundo et al., 2009; Hansmeier & Eickholz, 2010; Ratka-Krüger et al., 1999). Comparing the clinical results of this study with similar long-term observations on the envelope technique (Nickles et al., 2010; Rossberg et al., 2008), agreeable results can be observed for mean RD. Both Rossberg et al. (−2.7 ± 1.2 mm; p < .001) and Nickles et al. (−2.07 ± 1.89 mm; p = .042) reported a statistically significant reduction in mean RD after 10 years as compared with that at baseline. This significant reduction was also confirmed by the present study (−1.57 ± 0.75 mm; p < .001). When comparing the mean relative RC of the three studies, however, it is noticeable that Rossberg et al. with a relative RC of 89.7 ± 25.1% came significantly closer to the results achieved in this study (71.22 ± 30.86%) than did Nickles et al. with an outcome of 43.7 ± 41.7%. With a result of 71.22%, this study is in the range (64.7%–94.58%) that Roccuzzo et al. found with the sole use of CTGs in a structured review (Roccuzzo, Bunino, Needleman, & Sanz, 2002). Other studies use the term “creeping attachment,” that is, a further increase in RC over a longer follow-up period after an initial partial RC has been attained. This phenomenon was confirmed by the present investigation. Matter showed similar results after 5 years of using FGGs for root coverage with a relative RC of 70% as was found here after 10 years (Matter, 1980). Another study over a shorter follow-up period using CTGs in combination with double pedicle grafts revealed a mean creeping attachment of 0.8 mm over 5 months, which was 0.3 mm more than this study showed after 10 years (Harris, 1997). The data of this study indicate that a larger part of the creeping attachment phenomenon takes place in the first 3 months as compared with that later on (Table 2).
When considering CRC, the studies mentioned in the beginning [82% (Rossberg et al., 2008); 14.3% (Nickles et al., 2010)] differ significantly from this one (CRC: 40.0%). The differences are difficult to explain, as none of the three studies could ensure regular supportive care of most of the study participants over the follow-up period.
The increase of GW is also different between the studies with findings of 4.7 ± 2.3 mm in Rossberg et al. (2008), 3.43 ± 2.84 mm in Nickles et al. (2010) and 0.70 ± 1.31 mm in this study.
The increase of keratinized tissue is assumed to be a result of the exposed portion of the graft. However, due to the lack of data on the exposure of the graft, this was not examined in more detail in the present study. Also, this study included only Miller class I recessions, while Rossberg et al. and Nickles et al. also included Miller class II recessions. In Miller class II, there is no more keratinized tissue, so the average growth of it can be greater.
In comparing the long-term stability of the post-surgical results between 3 and 120 ± 12 months with each other, it is noticeable that the mean RD of Nickles et al. increased significantly by 1.0 ± 0.78 mm (p = .042), whereas in this study, it decreases by 0.58 ± 1.00 mm (p = .117). The situation is similar for the mean GW, which increases by 0.43 ± 3.0 mm in the study by Nickles et al. (Nickles et al., 2010) but decreases by 0.19 ± 0.93 mm in the present study. Both studies re-examined the patients after 3 and 120 ± 12 months, respectively. Rossberg et al. reported no immediate post-operative results (Rossberg et al., 2008).
In general, all three studies have in common that they used the same surgical approach [envelope technique (Raetzke, 1985)]. They differed in their study design, which was prospective for this study and retrospective for the other two (Nickles et al., 2010; Rossberg et al., 2008). They also differed in the number of patients examined [n = 20 (Rossberg et al., 2008); n = 7 (Nickles et al., 2010); n = 13 (after 3 months) and n = 15 (after 120 ± 12 months) in this study]. Furthermore, the primary objective of the study of Nickles et al.—that is the long-term comparison of two surgical procedures (CTG vs. GTR; Nickles et al., 2010)—was different from that of this study. However, the biggest difference between the studies was the choice of setting. While Rossberg et al. and Nickles et al. studied cohorts treated and examined in a university setting (Nickles et al., 2010; Rossberg et al., 2008), this study refers to a private practice setting.
Comparing CTG according to the envelope technique in this study with the gold standard therapy, a CTG + coronal advanced flap (CAF) of a current randomized controlled trial (Rasperini et al., 2018) that examined 25 Miller class I and II recessions over 9 years, similar results were found. The mean RD of Rasperini et al. was 0.5 ± 0.5 mm at 9 years after surgery, while the mean GW was 4.80 ± 0.70 mm and the CRC was 66.7%. The corresponding values of this study are 0.63 ± 0.64 mm (RD), 4.80 ± 1.44 mm (GW) and 40.0% (CRC).
Risk factors such as nicotine consumption and irregular SPT are well known and proven (Chambrone et al., 2018; Rasperini et al., 2018; Yadav et al., 2018) but could not be used for further calculations in this study due to the low number of cases included (Table 1). In the case of the present study, a more regular participation in SPT and, thus, a possibly better control of the underlying aetiological factors would probably have led to even better results (Tatakis et al., 2015). Linear regression analyses (Table 3) confirmed that RD and GW achieved after 3 months correlated with RC stability (Pini Prato, Franceschi, Cortellini, & Chambrone, 2018; Rasperini et al., 2018).
In particular, because a large number of the study participants opted to undergo the procedure for aesthetic reasons, this investigation shows additional patient-centred outcomes as recently repeatedly called for (Cairo, 2017; Cairo et al., 2016; Chambrone et al., 2018; Mounssif et al., 2018). The lack of professional evaluation of aesthetic outcomes is more and more being taken into account in current studies (Santamaria et al., 2017; Stefanini et al., 2016) and should be of high importance in the future. The OHIP was already used in the 3-month follow-up (Hansmeier & Eickholz, 2010). Over a period of 120 ± 12 months, the results obtained after 3 months remained stable (p = .889). Other studies also note the use of OHIP in periodontal plastic surgery, but only up to a maximum follow-up period of 6 months (Douglas de Oliveira, Marques, Aguiar-Cantuaria, Flecha, & Goncalves, 2013; Oliveira & Nadanovsky, 2005; Rocha Dos Santos et al., 2017). All three studies used a short version of the OHIP questionnaire (OHIP-14), did not examine the envelope technique and did not deal with changes in the OHIP score over the follow-up time (Douglas de Oliveira et al., 2013; Oliveira & Nadanovsky, 2005; Rocha Dos Santos et al., 2017).
Patient-centred results of the self-assessment of satisfaction (Table 4a) and improvement of the original problem (Table 4b) indicate that patients are at least satisfied (Table 4a) with 14 of the total of 15 recession defects (93.33%) and satisfied (Table 4b) with the improvement (school grades A-C). Nickles et al. and Rossberg et al. reported higher satisfaction with 100% reporting between school grades A and C for the same procedure (Nickles et al., 2010; Rossberg et al., 2008). In this case, the difference between the two studies and the present study is probably due to the fact that two first molars were included in the present study, whereas Nickles et al. and Rossberg et al. did not include any molars. The fact that patients are more satisfied with the outcomes than the clinical parameters might possibly suggest (Petsos, Trimpou, Eickholz, Lauer, & Weigl, 2017) also seems to apply in this study (CRC: 71.22% vs. 93.33% for minimum satisfied patients). Nevertheless, it can be concluded for both studies that the patients were satisfied with the final results after 10 years. This is also expressed in this study by the fact that 12 out of 15 patients (80%) said they would undergo the same procedure again after 10 years (Table 4a/b). Rossberg et al. again exceeded this result with 19 out of 20 patients saying the same (95%; Rossberg et al., 2008).
Limitations of this investigation are certainly the small number of cases and the missing control group on the one hand and the unblinded treatment/examination performed by the same person on the other hand. Nevertheless, to the best of our knowledge, this is the only prospective long-term observation of the envelope technique over 10 years that took place in a private practice setting, which is why it is highly relevant for practitioners.
5 CONCLUSIONS
- Root coverage with CTG using the envelope technique leads to a clinically stable result over 10 years in a private practice setting.
- The envelope technique also leads to the stabilization of the initially improved OHIP values over a follow-up period of 10 years.
- Overall, patients (93.33%) were satisfied with the final result after 10 years.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interests related to this study.