THORACIC COMPUTED TOMOGRAPHY IN FELINE PATIENTS WITHOUT USE OF CHEMICAL RESTRAINT
Abstract
Computed tomography (CT) and thoracic radiography were performed in nonsedated, nonanesthetized, cats with thoracic disease. The final diagnosis was obtained with echocardiography, cytology, histopathology, necropsy, or response to therapy. For CT imaging, cats were in a positioning device using a 16 multislice helical CT system. Fifty-four cats had CT imaging of which 50 had thoracic radiography. The most common diagnoses were lung neoplasia, lower airway disease, and cardiomyopathy (nine each). Other disease groups included mediastinal mass (eight), infection (seven), trauma (four), and hernia (three). CT provided additional correct diagnoses in 28% (14/50) and additional information in 74% (37/50) of the cats. Additional correct diagnoses achieved only with CT were most common for cats with lower airway disease. The most common additional findings with CT were lung nodules (n=4), lung masses (n=4), bronchiectasis (n=4), and mediastinal lymphadenopathy (n=3). Survey CT led to a significant different diagnosis or different prognosis in 20 of the 50 cats that were imaged both modalities. Contrast CT was performed in 19 cats, most commonly in cats with lung neoplasia (n=6), a mediastinal mass (n=4) or an infection (n=3), and provided additional correct diagnosis in two cats not achieved with survey CT. Thoracic CT using a positioning device in diseased awake cats is feasible, safe, and clinically useful.
Introduction
General anesthesia is used typically for canine and feline patients undergoing thoracic computed tomography (CT).1–5 General anesthesia causes atelectasis that can interfere with evaluation of the lung and is also contraindicated in many emergency conditions, especially for patients with respiratory distress. The use of CT in normal cats without anesthesia or sedation was described recently. CT images of awake cats were acquired using a low-attenuating clinically acceptable positioning device.* CT imaging was completed in 20 of 22 (91%) cats and image quality in the completed studies was excellent with minimal motion artifact.6 The purposes of the present study were to test the usefulness of the positioning device in feline patients with respiratory disease and to compare the CT findings to radiographic findings in the same patients.
Materials and Methods
Fifty-four cats presenting to the emergency department with a recent history of, or current clinical signs of, respiratory disease were stabilized and underwent CT thoracic imaging in the positioning device* without sedation or general anesthesia using a 16 slice helical system.† The mean age was 9.5 years (range 0.17–19 years) and mean body weight was 4.9 kg (range 2–8.4 kg). There were four males, 35 neutered males, and 15 neutered females. Breeds were domestic short hair (n=32), domestic long hair (n=10), mixed (n=4), Siamese (n=3), and one each domestic medium hair, Himalayan, Maine Coon, Devon Rex, and Burmese.
Evidence of respiratory disease was based on information presented by the owner, physical findings of the referring veterinarian or response to specific therapy. Inclusion based on current clinical signs was a decision made by the primary clinician. Clinical signs included increased respiratory rate or effort, cyanosis, open-mouth breathing, extension of head and neck, anxious behavior, decreased tolerance to handling, cough, auscultation of abnormal breathing sounds, abdominal breathing, or nasal discharge. Cats with at least two of the aforementioned clinical signs, excluding cough and nasal discharge, were characterized as having dyspnea. Forty-one of the 54 cats (76%) were dyspneic and 13 (24.1%) were eupneic.
Cats were typically placed in the positioning device while in the emergency room and transported to the radiology department. During transportation and CT scanning, oxygen was provided to dyspneic cats (41) at a flow of 2 l/min through a tubing in the device at the cranial end of the patient. Images of the entire positioning device were acquired resulting in whole-body scanning in all cats. The CT protocol was: 0.562 pitch, either 80 kV and 130 mA, or 120 kV and 45 mA, collimation of 16 × 0.625 mm, gantry rotation speed of 0.5 s, 25 cm field of view, 1.25 mm slice thickness with 0.63 mm increment and detail algorithm. In a subjective evaluation for motion artifact performed during the scanning, seven cats had the first CT examination repeated one time due to severe motion which resulted in a nondiagnostic study. This nondiagnostic images were not included in the study. Intravenous iodinated‡ (2 ml/kg) contrast medium was administered as clinically indicated.
Thoracic radiographs were made in left and right lateral and either dorsoventral or ventrodorsal recumbency. The attending clinician decided whether CT or radiography was performed first. The time from initial presentation in the hospital to initiation of imaging was recorded.
All cats had a final diagnoses based on echocardiography, cytology, histopathology, necropsy, or clinical response to specific therapy. Follow-up was obtained when possible. The cats were separated into eight clinical classifications based on final diagnosis: (1), pulmonary neoplasia (2), lower airway disease, (3) cardiomyopathy (4) mediastinal mass (5) infection, (6) trauma, (7) hernia, and (8) other.
All imaging studies were evaluated on a PACS workstation§ by consensus of two radiologists. Contrast enhanced CT images and multiplanar reconstruction (MPR) images were not compared with radiographs to avoid bias. MPR and contrast-enhanced images were evaluated retrospectively for additional diagnoses and additional CT findings, compared with survey CT.
The CT and radiographic image sets were anonymized and randomized. CT images were evaluated using a standardized questionnaire that addressed 36 specific items related to disease and four related to image quality (Appendix A). Evaluators answered the questions as present, absent, or indeterminate. Specific disease was graded as absent, mild, moderate, or severe on either modality and was based on standard criteria.7–10 Motion artifact was graded subjectively as: (1) absent; (2) mild: hardly noticeable, not causing misrepresentation of any thoracic structures, and present in less than five slices; (3) moderate: easier to notice, not causing misrepresentation of any thoracic structures, and present in more than five and less than 15 slices; (4) severe: easy to notice, causing mild misrepresentation of thoracic structure, and present in more than 15 slices. Evaluators provided the reasons for indeterminate findings and if technique or positioning was judged inadequate.
Commercial software¶,∥ was used for statistical analyses. The Kolmogorov–Smirnov test was used to test for normalcy of the data. A Wilcoxon test for paired samples was used to compare the time from presentation to performing radiographs with the time from presentation to performing CT. For the imaging evaluation, the results of radiographic analysis were compared with the results of CT analysis using interrater agreement test. A comparison of proportions was performed for indeterminate findings and for image quality evaluation for each imaging modality including technique adequate, positioning adequate, motion artifact, and complete study. Results for κ interrater agreement test were assessed according to a reference range.11 A P<0.05 was considered statistically significant for all statistical tests.
Results
Forty-one cats had a final diagnosis based on necropsy (n=14), cytology (n=13), echocardiography (n=7), histopathology (n=5), or surgery (n=2). In the remaining 13 cats a presumed diagnosis was made based on response to therapy and follow-up.
Of the 54 cats undergoing CT imaging, 50 also had radiography performed, of which 46 had complete three-view radiographic studies and CT imaging performed within 24 h of each other. Only these 46 cats were included in the statistical analysis for comparison between the imaging modalities, but all cats were evaluated for additional information and correct diagnosis provided by either imaging modality, image quality of the radiographic and CT studies, and time from presentation in the hospital to performing each study.
Thirty-two of 50 cats had radiography performed before CT and radiography was the initial imaging modality in 26 of the 38 (68.4%) dyspneic cats that had radiography performed. The median time from presentation to the hospital to radiography was 175 min (range 8–2025), and from presentation to CT was 237.5 min (range 26–2057); this difference was statistically significant (P=0.0427).
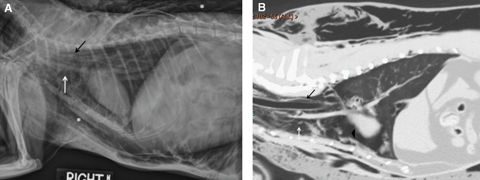
Overall accuracy of the correct final diagnosis was higher for survey CT (42/54; 77.8%) than radiography (29/50; 58%) (Table 1). The group with the largest difference between the correct diagnosis provided by CT vs. radiography was for cats with lower airway disease, where eight of nine (88.9%) of correct diagnoses were made with CT compared with four of eight (50%) for radiography. The group for which CT had the highest accuracy overall was for cats with a cranial mediastinal mass (100%, 8/8). CT provided additional information in comparison with radiographs in 37 of 50 (74%) cats with the most common additional findings being lung nodules (lesions <3 cm) (n=4), lung masses (lesions >3 cm) (n=4), bronchiectasis (n=4), and mediastinal lymphadenopathy (n=3, Fig. 1). The fewest additional findings obtained from CT in comparison with radiographs were in cats with cardiomyopathy (3/8, 37.5%,). Additional CT findings were clinically important in 20 of 50 (40%) cats, leading either to a different diagnosis or adding important information, such as the presence of metastasis.
| Groups | N | CT Correct Diagnosis | Rad Correct Diagnosis | CT Additional Information | Rad Additional Information |
|---|---|---|---|---|---|
| Lung neoplasia | 9 | 8/9 (88.9%) | 8/9 (88.9%) | 7/9 (77.8%) | 0/9 (0%) |
| Lower airway | 9 | 8/9 (88.9%) | 4/8* (50%) | 8/8* (100%) | 0/8* (0%) |
| Cardiomyopathy | 9 | 8/9 (88.9%) | 6/8* (75%) | 3/8* (37.5%) | 2/8* (25%) |
| Mediastinal mass | 8 | 8/8 (100%) | 6/7* (85.7%) | 6/7* (85.7%) | 1/7* (33.3%) |
| Infection | 7 | 2/7 (28.6%) | 1/7 (14.3%) | 5/7 (71.4%) | 0/7 (0%) |
| Trauma | 4 | 3/4 (75%) | 0/4 (0%) | 4/4 (100%) | 0/4 (0%) |
| Hernia | 3 | 2/3 (66.7%) | 1/2* (50%) | 1/2* (50%) | 0/2* (0%) |
| Miscellaneous | 5 | 3/5 (60%) | 3/5 (60%) | 3/5 (60%) | 0/5 (0%) |
| Total | 54 | 42/54 (77.8%) | 29/50 (58%) | 37/50 (74%) | 3/50 (6%) |
- * One cat did not have radiographs . CT, computed tomography; Rad, radiography.
(A) Left lateral thoracic radiograph of a cat with lymphoma. Note increased soft-tissue opacity dorsal to the sternum (asterisk) obscuring the cranial mediastinum. (B) Transverse survey computed tomographic (CT) image of the cranial thorax of the same cat. Note the enlarged sternal lymph node (arrow) not seen radiographically and pleural effusion (asterisk). Window width=400, window level=40.
There was either fair or poor agreement between CT and radiography for 25 of the 36 (69.4%) specific findings that evaluators assessed (Table 2). Presence and degree of pleural effusion, peritoneal effusion, pneumomediastinum, mediastinal mass, and pneumothorax were the only findings for which there was a substantial agreement between radiography and CT.
| N * | Radiograph | CT | κ | |||
|---|---|---|---|---|---|---|
| Absent | Present | Absent | Present | |||
| Extrathoracic | ||||||
| Fracture | 46 | 46 | 0 | 45 | 1 | 0 |
| Costal arch deformation | 46 | 44 | 2 | 42 | 4 | 0.292 |
| Sternum deformation | 46 | 45 | 1 | 45 | 1 | −0.022 |
| Abdomen | ||||||
| Peritoneal effusion | 46 | 41 | 5 | 42 | 4 | 0.877 |
| Pneumoperitoneum | 46 | 46 | 0 | 45 | 1 | 0 |
| Mass | 46 | 46 | 0 | 45 | 1 | 0 |
| Aerophagia | 46 | 31 | 15 | 32 | 14 | 0.346 |
| Mediastinum | ||||||
| Esophageal dilation | 46 | 40 | 6 | 29 | 17 | 0.084 |
| Pneumomediastinum | 46 | 44 | 2 | 44 | 2 | 1 |
| Mass | 42 | 36 | 6 | 38 | 4 | 0.774 |
| Lymphadenopathy | 40 | 40 | 0 | 37 | 3 | 0 |
| Cardiomegaly | 42 | 37 | 5 | 35 | 7 | 0.419 |
| Microcardia | 46 | 41 | 5 | 44 | 2 | 0.238 |
| Pleural cavity | ||||||
| Effusion | 46 | 30 | 16 | 31 | 15 | 0.951 |
| Pneumothorax | 46 | 43 | 3 | 41 | 5 | 0.728 |
| Diaphragm | ||||||
| Hernia | 40 | 40 | 0 | 40 | 0 | † |
| Flattening | 43 | 37 | 6 | 43 | 0 | 0 |
| Tenting | 44 | 43 | 1 | 44 | 0 | 0 |
| Asymmetry | 46 | 46 | 0 | 46 | 0 | † |
| Upper airway | ||||||
| Tracheal narrowing | 46 | 45 | 1 | 44 | 2 | 0.657 |
| Tracheal deviation | 46 | 42 | 4 | 45 | 1 | −0.036 |
| Main stem bronchi narrowing | 46 | 46 | 0 | 43 | 3 | 0 |
| Lower airway | ||||||
| Bronchial wall thickening | 45 | 36 | 9 | 34 | 11 | 0.359 |
| Bronchiectasis | 46 | 44 | 2 | 40 | 6 | −0.07 |
| Alveolar pattern | 44 | 22 | 22 | 10 | 34 | 0.364 |
| Lung mass (>3 cm) | 44 | 38 | 6 | 34 | 10 | 0.548 |
| Unstructured interstitial | 45 | 43 | 2 | 32 | 13 | 0.205 |
| Structured interstitial | 45 | 40 | 5 | 36 | 9 | 0.167 |
| Vascular pattern | 46 | 44 | 2 | 44 | 2 | 0.477 |
| Bulla | 44 | 43 | 1 | 41 | 3 | −0.035 |
- * Indeterminate answers resulted in some findings having <46 cats . †Insufficient number to perform test . CT, computed tomography.
The majority of indeterminate answers occurred for radiographic studies (Table 3). The most common indeterminate answers were for mediastinal lymphadenopathy (8/50, 16%), diaphragmatic hernia (8/50, 16%), mediastinal mass (5/50, 10%), and cardiomegaly (5/50, 10%), all in cats with concurrent pleural fluid or a cranial mediastinal mass.
| Outcome | Radiograph | CT |
|---|---|---|
| Mediastinal lymphadenopathy | 16% (8/50) | 0% (0/54) |
| Diaphragmatic hernia | 16% (8/50) | 0% (0/54) |
| Mediastinal mass | 10% (5/50) | 0% (0/54) |
| Cardiomegaly | 10% (5/50) | 0% (0/54) |
| Diaphragmatic flattening | 8% (4/50) | 1.9% (1/54) |
| Lung mass | 6% (3/50) | 0% (0/54) |
| Diaphragmatic tenting | 4% (2/50) | 1.9% (1/54) |
| Alveolar pattern | 4% (2/50) | 0% (0/54) |
| Bulla | 4% (1/50) | 0% (0/54) |
| Esophageal dilation | 2% (1/50) | 0% (0/54) |
| Bronchial wall thickening | 2% (1/50) | 0% (0/54) |
| Unstructured interstitial pattern | 2% (1/50) | 0% (0/54) |
| Structured interstitial pattern | 2% (1/50) | 0% (0/54) |
- CT, computed tomography.
When comparing the proportions of image quality, two of 50 (4%) of the radiographic studies were characterized by inadequate technique and eight of 50 (16%) characterized by inadequate positioning (Table 4). The positioning for all CT studies was considered adequate; mild obliquity was common but this did not affect image quality. Motion artifact, not found in any radiographic study, was present in 27 of 54 (50%) CT studies. Motion artifact was mild in 23 of 27 (85%) CT studies and moderate in four of 27 (16.6%). On retrospective evaluation of the MPR images for artifacts, mild stair-step artifact was seen on 63 studies (from a total of 108 dorsal and sagittal studies). This was more easily seen on a soft-tissue window (window width=400, window level=40) and present almost exclusively at the diaphragm and soft-tissue regions adjacent to the ribs. Motion and stair-step artifact did not affect image quality in any cat.
| Radiography | CT | % Difference | 95% CI | χ2* | Significance | |
|---|---|---|---|---|---|---|
| Technique adequate | 96% | 100% | 4% | −5.4% to 10.6% | 0 | P=1 |
| Positioning adequate | 84% | 100% | 16% | 4.7% to 29.1% | 6.658 | P=0.0099 |
| Motion artifact | 0% | 50% | 50% | 34.4% to 63.9% | 31.215 | P<0.0001 |
| Complete study | 96% | 100% | 4% | −3.9% to 13.7% | 0.510 | P=0.4751 |
- * Degrees of freedom=1 . Outcomes indicate presence; CT, computed tomography.
Contrast medium was given to 19 cats, two of which had no precontrast CT imaging. Cats that received contrast medium had lung neoplasia (n=6), a mediastinal mass (n=4), infection (n=3), cardiomyopathy (n=2), hernia (n=2), lower airway disease (n=1), or chylothorax (n=1). The same diagnosis was reached in 15 of 17 (88.2%) cats with both survey and contrast CT. However, nine cats had additional information provided from postcontrast images, including sternal and cranial mediastinal lymphadenopathy in eight cats, and cystic regions within a cranial mediastinal mass. Of the eight cats that had thoracic lymphadenopathy detected based on contrast enhanced CT, nine had neoplasia (eight lung carcinoma, one thymoma).
Twenty-one cats had pleural effusion based on at least one imaging modality. The majority were in the cardiomyopathy group (7/21, 33.3%, followed by mediastinal mass and lung neoplasia (5/21 each, 23.8%). Seven of nine (78%) cats with cardiomyopathy, five of eight cats with cranial mediastinal lymphadenopathy (62.5%), and five of nine with lung neoplasia (55.6%) had pleural effusion.
In the nine cats with lung neoplasia, eight had a primary lung tumor and one had metastases from intestinal lymphoma. The most common CT findings were one to multiple lung masses (7/9), one to multiple soft-tissue nodules (4/9), pleural effusion (4/9), and a patchy alveolar pattern (4/9). Additional information obtained with CT compared with radiographs (7/9) included soft-tissue attenuating pulmonary masses (n=4) (Fig. 2) and metastasis (n=4) seen either as lung nodules (n=2) or a patchy alveolar pattern (n=2). Contrast medium was given to six of the cats with lung neoplasia leading to additional CT detection of thoracic lymphadenopathy in five.
(A) and (B) Right lateral and ventrodorsal thoracic radiographies of a cat with a cytologic diagnosis of pulmonary carcinoma. There is an alveolar pattern with a rounded appearance in the left caudal lung lobe on the VD view (white arrow) and increased soft-tissue opacity dorsal to the sternum secondary to pleural effusion (asterisk). (C) Transverse survey computed tomographic image of the same cat. The alveolar pattern in the left caudal lung lobe was confirmed to be a soft-tissue mass (white arrow). Note also the cavitary mass in the right caudal lung lobe (black arrow), pleural effusion (asterisk), and pneumothorax (arrow head) that were not visible radiographically. Window width=1600, window level=−600.
Of the nine cats with lower airway disease, seven were diagnosed based on response to therapy and follow-up, and two based on histopathology. The most common CT findings were diffuse bronchial wall thickening (8/9), a patchy alveolar pattern (5/9) and bronchiectasis (4/9). The wall of the bronchi could be easily measured and was considerably thicker compared with cats with other diseases (Fig. 3). The wall of the principal bronchi ranged from 1.2 to 1.7 mm, and the wall of a bronchi in the periphery (approximately 2 cm from the thoracic wall) ranged from 0.9 to 1.2 mm. In a retrospective evaluation, the wall of the principal bronchi measured in 10 cats with other disease process ranged from 0.8 to 0.9 mm and bronchi could not be seen at the periphery of the pulmonary parenchyma. Additional information from survey CT compared with radiographs was obtained in eight of eight cats and included bronchial wall thickening (n=4), bronchiectasis (n=4), pneumonia (n=3), and main stem bronchial (n=2, Fig. 4) and tracheal (n=1) thickening with luminal stenosis.
Transverse survey computed tomographic image of mid thorax of a cat with lower airway disease. Note the severe diffuse bronchial wall thickening (white arrows) WW=1600, WL=−600.
Transverse computed tomographic image of the cranial thorax of a cat with lower airway disease. Note the bilateral principal bronchi stenosis (arrows); diameter=1.7 mm (compared with 4.9 mm caudally, right principal, and 4.2 mm caudally, left principal). Window width=1600, window level=−600.
Diagnoses in the nine cats with cardiomyopathy were restrictive cardiomyopathy (n=4), hypertrophic cardiomyopathy (n=3), arrythmogenic cardiomyopathy (n=1), and unclassified cardiomyopathy (n=1). Final diagnosis was based on echocardiography (n=7) or necropsy (n=2). The most common CT findings were cardiomegaly (7/9) (Fig. 5A and B), pleural effusion (7/9), and a patchy alveolar pattern (6/9). Additional information was obtained from CT compared with radiographs in three of eight cats and included cardiomegaly (n=2 cats, both with pleural effusion), pleural effusion (n=1), and a consolidated alveolar pattern (n=1). Eight of nine (88.9%) cats had CT findings consistent with congestive heart failure, including pulmonary edema and pleural (n=7) or peritoneal (n=2) fluid. The interventricular septum and left ventricular free wall (average 45–68 HU) were hyperattenuating compared with blood (average 20–40 HU) in survey CT images in four cats (Fig. 5A and B). Wall-chamber characterization was indistinct in three cats and could not be assessed in two cats.

(A) and (B) Left lateral and VD thoracic radiographies of a cat with restrictive cardiomyopathy and congestive heart failure. The cardiac silhouette is not well visualized on the lateral view due to pleural effusion (asterisks). Note the alveolar pattern in the right middle and caudal part of left cranial lobe on the VD view (arrows). (C) Dorsal multiplanar reconstruction computed tomographic image of the same cat. Note the enlarged left atrium (arrow) and pleural effusion (asterisk). WW=400, WL=40.
In the eight cats with a mediastinal mass, the diagnoses were thymoma (n=4), lymphoma (n=3), and carcinoma (n=1). The most common CT findings were a soft-tissue mass in the cranial mediastinum (7/8) that was homogeneous (3), cystic (3) or mixed soft tissue and mineralized (1), pleural effusion (5/8), and atelectasis (4/8). Additional information from survey CT compared with radiographs was obtained in six of seven cats and included atelectasis (n=3), and one cat each with pulmonary metastasis, sternal and cranial mediastinal lymphadenopathy, a neck mass and a lung mass. Contrast CT was performed in four cats. Additional findings in contrast-enhanced CT images were cystic portions of a thymoma (n=1) and sternal and cranial mediastinal lymphadenopathy (n=1).
Of the seven cats with infection, the diagnoses were aspiration pneumonia (n=1), suppurative tracheitis with suppurative bronchitis (n=1), suppurative tracheitis and bronchopneumonia (n=1), lung abscess with pleuritis (n=1), suppurative bronchopneumonia secondary to Bordetella bronchiseptica (n=1), pyogranulomatous pneumonia with fibrosis (n=1), and suppurative inflammation (n=1). The most common CT findings in this group were a patchy alveolar pattern (4/7), one to multiple lung masses (3/7), a mixed patchy and consolidated alveolar pattern (2/7) and sternal, and cranial mediastinal lymphadenopathy (2/7). Additional information was obtained with CT compared with radiographs in five of seven cats and included sternal and cranial mediastinal lymphadenopathy (n=2), and one cat each with tracheal and main stem bronchial wall thickening with stenosis and collapse, lung mass, and lung nodule. Correct diagnosis obtained with survey CT and not with radiography included pneumonia with tracheitis and tracheal and bronchial collapse and stenosis (n=1) and bronchitis with pneumonia (n=1).
Of the four cats with trauma, the diagnoses were one cat each with human abuse causing liver rupture and pulmonary contusion, tracheal rupture associated with endotracheal intubation (Fig. 6), trapped inside a tumble clothes dryer, and hit by a car. Correct diagnosis obtained with survey CT and not with radiography were trauma (n=2) and tracheal rupture (n=1). Additional information obtained with CT (4/4) were bulla (n=1), pulmonary contusion (n=1), lung atelectasis (n=1), rib fracture (n=1), discontinuity of tracheal wall (n=1), pneumopericardium (n=1), and lung nodules (n=1).
(A) Right lateral thoracic radiograph of a cat with confirmed tracheal rupture. A region of tracheal wall discontinuity was suspected on the dorsal aspect of the thoracic trachea (black arrow). Note also severe subcutaneous emphysema (asterisks) and pneumomediastinum (white arrow). (B) Sagittal multiplanar reconstruction computed tomographic image of the same cat. Note the tracheal discontinuity (black arrow), pneumomediastinum (white arrow), and pneumopericardium (arrow head). On surgery a 1 cm long tear was present at the right-dorsal aspect of the tracheal wall. WW=1600, WL=−600.
Of the three cats with a hernia, the diagnoses included one cat each with hiatal hernia, diaphragmatic hernia (Fig. 7), and peritoneal pericardial diaphragmatic hernia. Correct diagnosis obtained with survey CT and not with radiography was diaphragmatic hernia, radiographically diagnosed as severe pleural effusion of unknown cause. Additional information obtained with CT (1/2) included liver, spleen and fat in the thoracic cavity, and disruption of diaphragm.

Transverse survey computed tomographic image of caudal thorax of a cat with diaphragmatic hernia. Note the large amount of fat attenuating material (−128 HU) in the ventral aspect of the thorax (asterisk). The spleen (black arrow) and a liver lobe (white arrow) are visible in the thorax. The heart is displaced dorsally and to the right (black arrow head). Atelectasis is also present (white arrow head). WW=400, WL=40.
Of the five cats in the miscellaneous group were cats with lidocaine toxicity, chylothorax and fibrosing pleuritis, smoke inhalation, pulmonary edema secondary to fluid overload, and normal (n=1 each). The most common CT findings were a patchy alveolar pattern (n=2), bronchial wall thickening (n=2), and one finding each of pneumothorax, pleural effusion, and bronchiectasis. Additional information obtained with CT (3/5) included: bronchial wall thickening (n=2), lung atelectasis (n=1), patchy alveolar pattern (n=1), and bronchiectasis (n=1).
Discussion
Cats in this study had CT imaging without sedation or anesthesia and there were no complications. The positioning device provided a suitable environment for imaging without general anesthesia or sedation and allowed constant oxygen to dyspneic cats and fluid administration throughout the procedure. CT led to a correct diagnosis in 42 of 54 (77.8%) cats while with radiography a correct diagnosis was reached in 29 of 50 (58%) cats. This is consistent with previous studies of thoracic CT in humans and anesthetized dogs and cats.1,3–5,12,13
Our technique was particularly useful in dyspneic cats that can be stressed when restrained for radiographic examination.14 In this study, four cats were not adequately stable for thoracic radiography study but could be imaged with CT.
None of the eight cats with primary lung neoplasia were thought to have regional lymphadenopathy based on either radiography or survey CT, however lymphadenopathy was detected in five of these cats following contrast medium administration.
CT had a higher accuracy for lower airway disease (88.9%) compared with radiography (50%), which was expected because feline lower airway disease may appear normal radiographically in as many as 23% of cats.14–21
Bronchiectasis was detected with CT in four cats but was not detected radiographically in any cat. In humans, bronchial dilation occurs in up to 80% of patients with asthma and high-resolution CT is superior to bronchography for the evaluation of patients with both bronchiectasis and small-airway disease.22,23 Our results suggest that the incidence of bronchiectasis may be underestimated in cats with lower airway disease.
CT had high accuracy for the diagnosis of cardiomegaly and congestive heart failure. Pleural effusion, seen in seven cats in the cardiomyopathy group, was not a limiting factor with CT regarding the evaluation of the size and shape of the cardiac silhouette. Also, it was often possible to identify specific cardiac chambers even without contrast medium administration and cardiomegaly could be assessed readily on transverse CT images in eight of the nine cats in this group. Additionally, although not evaluated herein, it should be possible to differentiate fat and pericardial fluid, which can make the evaluation of heart size in obese cats and cats with pericardial effusion more accurate than with radiography.
Because radiography allowed a correct diagnosis of cranial mediastinal mass in all but one cat, the major advantage of CT imaging in these cats was in providing additional information such as lung atelectasis, pulmonary metastasis, sternal and cranial mediastinal lymphadenopathy, among others.
Cats with pulmonary infection had the lowest number of correct diagnosis achieved with CT (3/7 cats), which could be explained by the common finding of one or multiple lung masses in this group that were misdiagnosed commonly by CT as being a primary lung tumor. The differentiation between an inflammatory from a neoplastic lung mass using CT has not been studied extensively in veterinary medicine. In humans, diagnosis of pneumonia requires a combination of clinical assessment, radiological imaging, and appropriate microbiologic testing. CT is a valuable adjunct when thoracic radiographs are negative or nondiagnostic, in unresolved pneumonias and when complications are suspected such as when dealing with immunocompetent children, neutropenic patients, and patients with human immunodeficiency virus.24–26
The high accuracy of CT in cats with trauma in the present study indicates that CT can be an important modality for assessing the trauma patient.
Evaluating underlying disease radiographically in patients with pleural or peritoneal effusion is inaccurate. In this study pleural effusion was the most common reason for indeterminate findings, including mediastinal lymphadenopathy or masses, cardiomegaly and diaphragmatic rupture.
Positioning was adequate in all CT studies. With a multislice helical CT scanner it is possible to reconstruct images in any plane with resolution similar to that of the acquisition plane and mild obliquity can be corrected during the reconstruction process. Patient motion can cause significant artifacts, such as stair-step artifacts that appear as shading or streaking in the reconstructed image.27 In the present study, mild stair-step artifact was seen in 58% of the MPR images, however this artifact did not affect image quality or interpretation and was not noted in the lung region. The temperament of cats in general also contributes to CT being feasible in this species without sedation or anesthesia. Cats in the positioning device tended to remain in sternal recumbency with minimal movement. Minimal breathing motion artifact was noted commonly but it was detected only in a small number of CT slices in affected image sets and did not impair evaluation in any cat.
In conclusion, CT was highly accurate (77.8%) for the evaluation of cats with respiratory distress. CT provided additional information in 74% of the cats allowing a correct diagnosis not achieved with radiographs in 28% of cats. CT imaging of cats using the positioning device without general anesthesia or sedation, is safe and provides more accurate diagnostic information than radiography.
Footnotes
ACKNOWLEDGMENT
We would like to thank Jodi Matheson, DVM, Dipl. ACVR, for her help evaluating the CT and radiographic images.
Appendix
Appendix A
| Image Quality | Bone Window | Soft-Tissue Window | Soft-Tissue Window | Lung Window | Lung Window |
|---|---|---|---|---|---|
| Technique adequate | Extrathoracic | Abdomen | Mediastinum | Mediastinum/pleura | Lower Airway |
| Positioning adequate | Fracture | Peritoneal effusion | Mass | Esophageal dilation | Bronchial wall thickening |
| Motion artifact | Costal arch deformation | Pneumoperitoneum | Lymphadenopathy | Pneumomediastinum | Bronchiectasis |
| Complete study | Sternum deformation | Abdominal mass | Cardiomegaly | Pneumothorax | Alveolar pattern |
| Aerophagia | Microcardia | Lung mass (<3 cm) | |||
| Unstructured interstitial pattern | |||||
| Pleural cavity | Upper airway | Structured interstitial pattern | |||
| Effusion | Tracheal narrowing | Vascular pattern | |||
| Tracheal deviation | Bulla | ||||
| Diaphragm | Mainstem bronchi collapse | ||||
| Hernia | |||||
| Flattening | |||||
| Tenting | |||||
| Assymetry | |||||
| Degree of bronchial wall thickening | |||||
| Degree of pneumomediastinum | |||||
| Degree of pneumothorax | |||||
| Degree of pleural effusion | |||||
| Degree of esophageal dilation | |||||
| Alveolar pattern distribution | |||||
| Tentative diagnosis | |||||