Silver nanoparticle dressing: The knowledge of advantages and limits improves the indications in clinical practice
Valentina Budini is a first author.
Abstract
Silver nanoparticle dressings have gained popularity recently as a way to treat challenging wounds. Notwithstanding the properties of Ag-NPS (silver nanoparticles) described by several articles, there is a lack of clinical studies that guide healthcare professionals to specific and conscious use. In this case series, Ag-NPS dressing was tested on a randomized group of 10 patients with complex wounds requiring conservative treatment. Each case was analysed, recording the patient's history, the peculiar characteristics and the progressive changes in the wound. The wound bed and the quality of the peri-wound skin improved and a decrease in signs of infection was observed. The application of the dressing was simple and comfortable for the patient and it was appreciated for its sealing ability. A few capacity restrictions showed up: those should be read as elements to improve the indications for this peculiar dressing. The thin tissue matrix of the Ag-NPS dressing does not allow for massive absorption and also performs poorly in reducing little exudate. The reduction in wound width is also limited: reconstructive surgery was required in half of the enrolled patients to achieve wound healing.
1 INTRODUCTION
Over the years, many dressings and various devices have been developed to deal with complex wounds, to allow the best and fastest evolution of the lesion and to improve the appearance of the scar.1
One of the most innovative and promising technologies is based on silver nanoparticles (Ag-NPS), which can be incorporated into common wound dressing materials such as chitosan, PVA, cellulose and polycaprolactone with various structures, including nanofibers, hydrogels and mats.2
Applications of nanoparticles for wound healing have been widely explored, but they are still far from common clinical practice and commercialization. Many authors believe that the determining factor to increase the popularity and correct use of this type of dressing is the enhancement of clinical evidence.3
It is also necessary that health workers, especially in territorial centres, acquire a greater awareness of the indications and rationale for the use of a silver-based dressing.4
2 MATERIALS AND METHODS
The research is centred on clinical experience in order to aid in knowledge acquisition and the more conscientious application of silver nanoparticles.
The Ag-NPS tested is a gelling non-woven dressing, made up of poly-absorbent polyacrylic fibres which have demonstrated a debridement and cleansing action, and a TLC-Ag colloidal lipid matrix which has antimicrobial action.5 The TLC-Ag matrix (lipid-colloidal technology with silver ions) has been shown to reduce the bacterial load of the wound within the biofilm6 even in the case of colonization by MRSA and P. aeruginosa.7, 8 The poly-absorbent fibres of the dressing absorb and trap slough and exudate through an electrostatic mechanism.9
From September 2022 to November 2023, a case series, treated with Ag-NPS dressings, was analysed.
The hospital ethics committee approved Ag-NPS use before beginning patient treatment. The exclusion criteria were: poor compliance and non-adherence to treatment, inability to perform dressings with the application of Ag-NPS dressing at the treating physician or nursing district, drug addiction, allergy or hypersensitivity to Silver or other metals, septicaemia or bacteraemia, highly injured exudates, under 18 years of age, pregnant and lactating women.
The research describes the treatment of 10 patients with complex wounds, both male and female. The choice of patients to include in the study was random, through a random number generation, which selected patients seen at our clinic who met the inclusion criteria previously determined.
- High compliance and willingness to continue follow-up at our clinics.
- Absence of systemic infections (documented by normal WBC, CRP and procalcitonin infection indices and absence of bacteraemia at study entry).
- Assessment by a vascular surgeon, who attests to the absence of peripheral or venous artery obstructions. Measurements using Doppler flowmetry reveal an acceptable blood flow.
- By signing a written consent, all enrolled patients have agreed to the processing of their data and photographs for scientific purposes by signing a written consent. The purpose and methods of the study were explained to them before signing.
The patient's medical history, a description of the primary features of the lesion, and all study results were gathered during the initial outpatient appointment and entered into the patient's medical record (Figure 1).
- Age and sex of the patient, current pathologies, pharmacotherapy.
- Aetiology of the lesion, and adjuvant factors that led to skin ulceration.
- Age of the lesion (weeks), size and depth of the lesion (cm) and localization.
- Peculiarities of the ulcer base: percentage quantity of necrosis, granulation tissue, fibrin slough and re-epithelialized tissue.
- Clinical signs of local infection: foul-smelling, peri-wound erythema, pain between dressing changes, local oedema and heat, friable granulation tissue.
- Appearance of peri-wound skin (healthy, hyperemic, macerated, dry and flaking).
- Level of exudate (none, mild, moderate, high and very high).
- Pain perceived by the patient using a visual analogue scale (VAS) ranging from 0 (no pain) to 10 (worst pain ever).
During the first visit, photographs of the lesion were taken.
After inspecting the lesion, skin disinfection with antiseptic (0.05% sodium hypochlorite isotonic solution), cleansing with a physiological solution and drying were performed. The same health worker applied the dressing, which was first moulded to fit the lesion's dimensions before the region was wrapped with sterile gauze. Patients were followed up at our clinic with outpatient medications until the lesion healed, the result stabilized, or surgery required. During each control, the lesion's features were evaluated and photographs were collected. The lesion's final characteristics and the operator's assessments of the dressing's efficacy were recorded at the last control. The following aspects were considered: reduction of the wound surface, reduction of clinical signs of local infection, appearance of the peri-wound skin, absorption capacity, holding capacity, ease of application, conformability, patient comfort during dressing removal, ease of removal.
Data analysis was carried out through descriptive analysis when quantitative data were established and the numerical descriptive indices were calculated: mean, standard deviation, minimum and maximum.
Contingency tables and graphs have been created for the main qualitative variables.
3 RESULTS
We analysed 10 cases, 8 women and 2 men, with an average age of 67 (median 72.5 and SD 19.5). Eight patients suffered from a vascular disorder (arterial or venous) that contributed to the onsets and maintenance of the lesion. Two patients had DM II and three of them were following corticosteroid therapy.
As regards the aetiology of the lesion, four patients had suffered a traumatic accident in the area and one patient had undergone surface surgery; half of the patients described a ‘spontaneous’ onset of the lesion.
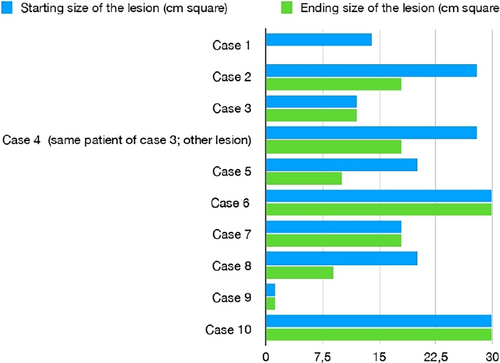
The time elapsed from the onset of the lesion to the first visit to our clinic range from 3 to 40 weeks (mean 13.6). The size of the lesion varied between 1 and 30 square cm, with an average of 20 (median 20; SD 9.3). The depth of the lesion was between 0.2 and 0.5 cm (mean 2.6; median 2; SD 1). In 9 out of 10 cases, the lesion developed in the lower limbs (five on the feet, four on the legs).
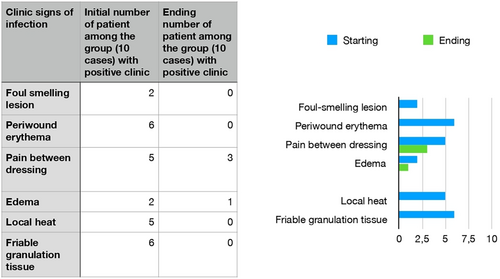
About the clinical signs of infection present at the beginning of the treatment: two patients showed foul-smelling lesions, six patients had friable granulation tissue, six patients had peri-wound erythema, two patients had oedema and five patients had local heat. Five patients felt pain during the medication change.
About the composition of the wound bed (average composition of all the ulcers): necrosis was 7%, granulation tissue was 26%, fibrin slough 50% and re-epithelialized tissue was 16%. We followed the patients for an average of 9.6 weeks, a minimum of 2 weeks and a maximum of 20 weeks; hospital check-ups were biweekly. Between hospital check-ups, each patient received Ag-NPS dressing every 3–5 days at the general practitioner, nursing district, or hospice.
Table 1 shows an example of the format compiled with complete judgements of intermediate dressings, correlated by the photographic record (Figure 2).
| Case 1 | |||||||
|---|---|---|---|---|---|---|---|
| Case 1: intermediate dressing | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Date | 21/10/2020 | 28/10/2020 | 11/11/2020 | 25/11/2020 | 9/12/2020 | 13/01/2021 | 25/02/2021 |
| Photograph | NO | YES | NO | NO | YES | NO | YES |
| Visual analogue scale for pain | 7 | 7 | 8 | 6 | 6 | 1 | 0 |
| Size (cm square) | 14 | 12 | 9, 75 | 5, 5 | 5 | 5 | 0 |
| Deep (mm) | 2 | 2 | 2 | 2 | 2 | 1 | 0 |
| Re-hospitalization n (%) | 10 | 15 | 20 | 20 | 30 | 30 | 95 |
| Granulation tissue (%) | 40 | 40 | 35 | 35 | 35 | 35 | 0 |
| Slough/fibrin | 50 | 45 | 45 | 45 | 35 | 35 | 5 |
Perilesional Eritema |
YES | NO | YES | NO | NO | NO | NO |
| Oedema | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Pain between change dressing | 1 | 1 | 1 | 0 | 0 | 0 | 0 |
| Local heat | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Perilesional skin: sane | 0 | 0 | 0 | 1 | 1 | 1 | 1 |
| Perilesional skin: hyperaemia | 1 | 1 | 1 | 0 | 0 | 0 | 0 |
| Perilesional skin: dry & desquamate | 1 | 1 | 1 | 1 | 1 | 1 | 0 |
| Exudate (0–4) | 1 | 1 | 0 | 0 | 0 | 0 | 0 |

- Lesion size ranging from 0 to 30 cm square (mean: 11.3; median 12; SD 8.4), with a reduction in the size ranging from 14 cm square (complete healing) to 0 cm square (mean: 6.5; median: 10; SD 6.1).
- Lesion depth ranging from 0 to 0.2 cm (mean and median: 0,1; SD 0.4) with a mean reduction in depth ranging from 0.3 to 0 cm (mean and median 0.1; SD 0.3).
- About signs of infection: three patients continued to feel pain during the last medication change, and one patient had peri-wound erythema. No patients showed foul-smelling lesions, friable granulation tissue, oedema, or local heat.
- Considering the average composition of all the wound beds analysed, the final results were: re-epithelization 39%; granulation tissue: 40%; slough/fibrin 22%. No percentage of wound bed necrosis.
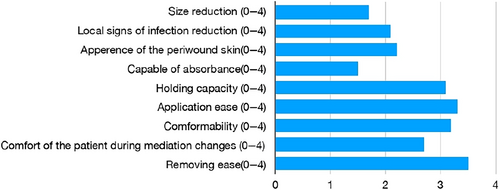
The operator's evaluation of the properties of the dressings is the sum of the judgement given from the beginning of the treatment to the final evaluation. It was rated very good in these aspects: ease of removal, conformability, ease of application, and holding capacity. It was rated good in reducing the clinical signs of local infection and improving the openness of the peri-wound skin, and patient comfort during dressing removal was also good. The reduction capacity of the lesion surface and absorption capacity were evaluated as ‘discrete’.
4 DISCUSSION
The study outcomes are coherent with the results anticipated from Ag-NPS in vitro research.
In particular, the marked improvement of the wound bed, shown by the disappearance of necrotic tissue in all cases, the significant reduction in the percentage of slough and fibrin, and the increase in granulation tissue and re-epithelialized tissue (Figure 3).
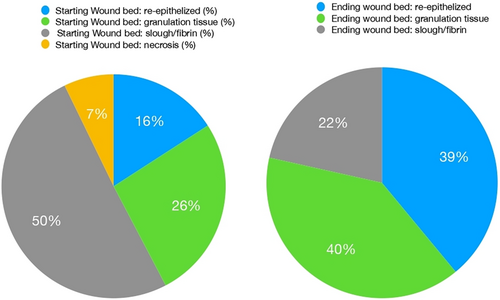
Figure 4 shows a significant reduction in wound surface area for every patient: there was no increase in wound size, albeit in half the cases there is no reduction in size despite the clinical improvement of the wound bed. Furthermore, the high SD value indicates that each case size reduction is significantly different from the others.
Clinical signs of infection show a clear improvement: peri-wound erythema, friable granulation tissue and local heat, signs present in at least half of the lesions analysed, are absent at the end. Oedema and pain between dressing changes were reduced by half of the cases compared with the initial situation (Figure 5).
The peri-wound skin improves together with the signs of infection. At the end of the control, in 9 out of 10 cases, hyperaemia, dryness and desquamation were absent. Discreet management of exudate by the Ag-NPS dressing was also observable (although, as we have already stated initially, the candidate wounds for treatment were not very exudate). At the end of the course of dressings, one patient underwent direct wound suturing surgery and four of the patients underwent a thin dermo-epidermal graft to cover the loss of substance. The Ag-NPS dressing performed a bridge to surgery to prepare the wound bed, demonstrating successful graft survival at one-month postoperative follow-up (Figures 6 and 7).


In one case, a TPN device was applied before Ag-NPS dressing to reduce the size of the wound. An additional instance involved the administration of a topical treatment to reduce eschar in between Ag-NPS dressings, with no adverse effects.
Figure 8 shows the average of the health operator's judgement (among the 10 cases) for each aspect of the dressing considered.
Although the outcomes of these case series are promising, it is necessary to point out some limitations of the study: the small number of patients did not allow a complex statistical analysis and the lack of case controls does not provide an effective comparison. The peculiarity of each complex wound and the uniqueness and clinical complexity of frail patients, can also be considered an intrinsic limitation that makes generalization of the result difficult.
5 CONCLUSIONS
Silver has been known since ancient times for its antimicrobial properties, confirmed by numerous current scientific studies. Silver nanoparticles are one of the most promising ‘new’ medications in the vast field of wound care. Adding silver to simple-to-use dressings would make them ideal for specific and conscious use. However, Ag-NPS dressings face difficulties finding their place in daily clinical practice. This issue is mainly due to the need for practical clinical trials understandable by healthcare professionals and a clear indication of their use. The present study, despite the limitation of a small number of cases and the lack of controls, aims to address this gap through some concrete examples.
Ag-NPS dressing is a promising way of promoting the development of a fertile wound bed and healing moderate-length chronic wounds. Silver nanoparticles lead to progressive cleaning of the ulcer, reduction of signs of local infection and improvement of the perilesional skin. The wound bed progressively evolves from necrotic-fibrinous tissue to granulation and re-epithelialization tissue. The ease of application and patient comfort have made it possible to carry out the dressings even in a non-specialized centre.
The restrictions of use found should be read as elements of refinement of the indications rather than as a negative opinion. Excessively exuding wounds should not be treated with Ag-NPS dressing, as the thin tissue matrix does not allow massive absorption.
Furthermore, Ag-NPS can have an adjuvant role in the reconstructive surgical treatment of the large ulcer.
ACKNOWLEDGMENTS
Non-profit relationship with ‘UgoMedical’. No support for the manuscript, no funding to declare.
CONFLICT OF INTEREST STATEMENT
None of the authors has a financial interest in any of the products, devices or drugs mentioned in this manuscript.
ETHICS STATEMENT
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Written informed consent was obtained from the patient before their inclusion in this study. Additional informed consent was obtained from all patients for which identifying information is included in this article.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.




