The effects of systemic diseases, genetic disorders and lifestyle on keloids
Abstract
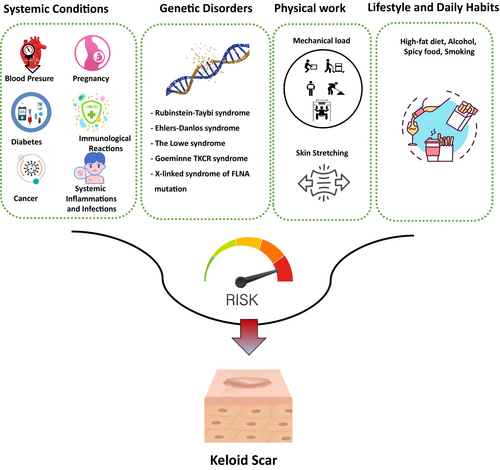
Keloid are a fibroproliferative disorder caused by abnormal healing of skin, specifically reticular dermis, when subjected to pathological or inflammatory scars demonstrating redness, elevation above the skin surface, extension beyond the original wound margins and resulting in an unappealing cosmetic appearance. The severity of keloids and risk of developing keloids scars are subjected to elevation by other contributing factors such as systemic diseases, general health conditions, genetic disorders, lifestyle and natural environment. In particular, recently, daily physical work interpreted into mechanical force as well as the interplay between mechanical factors such as stress, strain and stiffness have been reported to strongly modulate the cellular behaviour of keloid formation, affect their location and shape in keloids. Herein, we review the extensive literature on the effects of these factors on keloids and the contributing predisposing mechanisms. Early understanding of these participating factors and their effects in developing keloids may raise the patient awareness in preventing keloids incidence and controlling its severity. Moreover, further studies into their association with keloids as well as considering strategies to control such factors may help clinicians to prevent keloids and widen the therapeutic options.
1 INTRODUCTION
Keloids are defined as fibroproliferative disorder of the skin,1 caused by abnormal healing of skin subjected to injury or irritation, resulting in pathological or inflammatory scars. These scars demonstrate redness, elevation above the skin surface, extension beyond the original wound margins, and an unappealing cosmetic appearance. Furthermore, keloids are associated with intermittent pain, persistent itching and a sensation of contraction.2
Under normal homeostatic conditions, wound repair is limited in its scope and intensity. Most wounds fully mature within several months to over a year. Fibrosis occurs when key repair processes become deregulated and/or accentuated, leading to excessive ECM accumulation, which can result in the formation of hypertrophic scars or keloids.3 Common causes of skin injury and irritation include trauma, burn, surgery and skin piercing.4 Additionally, keloids can be influenced by systemic diseases, common lifestyle, natural environment and genetic factors in various mechanisms.
Systemic factors hypothesized to contribute to cutaneous pathological scarring include circulating immunological, genetic and endocrinological factors and cells,5 which directly impact the angiogenesis, inflammation, fibrosis and remodelling in pathological scars, thereby shaping their development and behaviour.
Several environmental lifestyle factors more indirectly affect cutaneous pathological scars, namely physical exercise, diet and smoking. The evidence for these contributing factors ranges from strong to highly speculative.
Abnormal keloid wound healing is commonly caused by sustained actions of fibroblasts which are responsible for the majority of collagen and ECM deposition. These actions are mainly driven by various growth factors, such as TGF-β, PDGF, fibroblast growth factor β (FGF-β) and insulin-like growth factor I (IGF-I) and other signalling cascades involved in fibrosis.6
In this article, we aim to review these participating factors and their impact on keloids development (Figure 1).
1.1 Systemic factors and general conditions
1.1.1 Blood pressure
The evidence has established a relationship between high blood pressure and pathological scarring. Studies have indicated that patients with high blood pressure undergoing invasive surgery are more prone to developing keloids postoperatively.7 Furthermore, individuals with multiple keloids or large-sized keloids (>10 cm2) were more likely to clinically present with associated hypertension. Conversely, severe hypertensive patients have been reported to have more tendency to develop multiple and/or large keloids.8 African Americans have also been described with higher incidence rates of keloids than Caucasians, and correspondingly, a similar pattern is observed in hypertension morbidity.9, 10
Anti-hypertensive drugs, particularly angiotensin-converting enzyme inhibitor (ACEI) such as Captopril,11 and calcium-channel blocker such as Verapamil,12 have been shown to be effective in keloids treatments (Figure 2).
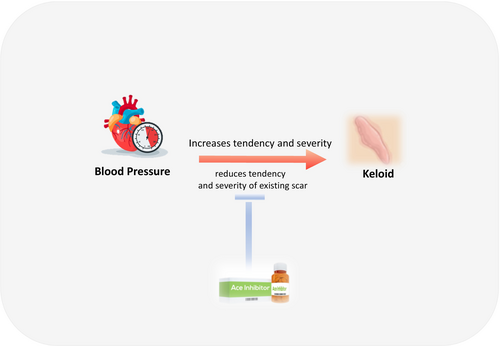
Because keloids prevalence in hypertensive adults remains low,13 we consider it as an aggravating factor for local severity of keloids rather than a common cause. Some possible mechanisms are thought to play a role in affecting the wound healing progression and the cellular proliferation as follows:
The mechanisms underlying the keloidogenesis and the aggravating effects of systemic hypertension remain unelucidated; however, we speculate that it acts by aggravating the endothelial dysfunction in cutaneous pathological scars by change in permeability of blood vessels and increased blood flow,14 along with the occurring vascular tone changes, coagulation can become activated, and vasomodulation becomes imbalanced, thereby promoting the profibrotic activities of fibroblasts and driving local inflammation.15
1.1.2 Pregnancy and hormonal effects
Pregnancy and hormonal effects during puberty have been suggested as risk factors for exacerbating pre-existing keloid and hypertrophic scars.16, 17
During pregnancy, a variety of hormonal changes and functional skin changes occur.18 Skin changes involve modifications in the dermis and its vascular network, leading to an increase in the total volume of circulating blood and promoting skin inflammation. These alterations in the wound healing process result in a disturbed mechanical status of the skin, stimulating the development of keloids with unusual characteristics and in uncommon body sites.19, 20
Pregnancy is believed to worsen pre-existing keloids or hypertrophic scars and may even trigger a previous scar to evolve into a keloid scar.21 (Figure 3).
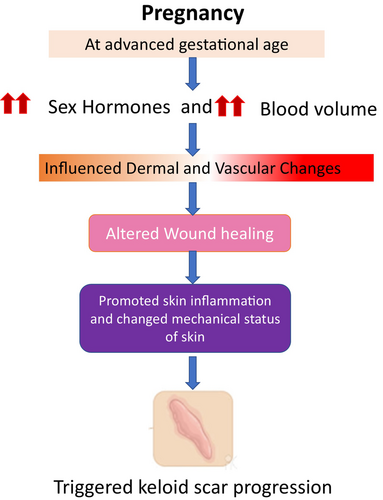
Keloids are more often witnessed in females between the age of 10 and 30 years and tend to resolve during menopause.22 Thus, pregnancy is considered as an exacerbating factor of keloids and correspondingly,23 sex hormones, particularly increased oestrogen is thought to act as a physiological risk factor for keloidogenesis.24 This hormonal contribution has been also indicated by the effect of tamoxifen treatment, which suppressed oestrogen-induced growth of keloids.25
Management of pathological scars during pregnancy remains an ambiguous area lacking strong evidence and guidance. The safety of various treatments, such as steroids and surgical excision during pregnancy with the ongoing impact of hormones, remains questionable. Therefore, further investigations are needed to understand the impact of sex hormones on keloids.
1.1.3 Diabetes
Recent study showed that keloids develop in type 2 diabetes patients and does not exhibit the classic ‘dumbbell’ shape.26, 27 Clinically, diabetes often causes an unhealing wound and chronic ulcer.28 The underlying mechanism is complex and involves hyperglycaemia, chronic inflammation and circulatory dysfunction.29
Moreover, patients with diabetes who are prone to chronic wounds (chronic inflammations), occurring at predilection body sites of keloids, predispose to high risk of keloids occurrence.30
In line with this, a nationwide retrospective cohort study using the National Database of Health Insurance Claims of Japan revealed that dipeptidyl peptidase-4 inhibitors (DPP4i), which is used in the treatment of diabetes, may be indirectly effective for keloids and hypertrophic scars as observed in diabetic patients treated by DPP4i who have shown lower risks of developing keloids after surgery by promoting insulin secretion.31
Similar to pathological scars, chronic diabetic wounds are characterized by chronic inflammation in which wounds express higher levels of NLRP3, caspase-1, and IL-1β mRNA and protein than non-diabetic wounds,32 which suggests that inflammasomes may participate in the poor healing of diabetic wounds.
Several lines of evidence then suggest that in particular, inflammasomes in pro-inflammatory M1 macrophages may play a vital role in diabetic wounds, as macrophages isolated from human and murine diabetic wounds exhibit high inflammasome activity.33
1.1.4 Immunological reactions
Vaccine-related keloids have been reported with Bacilli Calmette-Guerin (BCG) vaccine,34 smallpox vaccine35 and occasionally with some hepatitis B vaccine.36
The BCG vaccine is made from attenuated Mycobacterium bovis. The method used to administer the BCG vaccination in Japan is a percutaneous injection using an apparatus with multiple needles that is pressed into two locations on the upper arm. BCG is given once at the age of 5 months (between 5 and 7 months) in Japan. During this age, the skin is characterized by low tension and limited movements.37
Thus, the risk of developing keloids is relatively low compared with vaccine administration at older ages or receiving booster doses.38 Incidentally, over 90% of childhood BCG vaccine-induced keloids in Japan occur in women and are mainly developed as a result of the second injection and not the first.39
These keloids are believed to arise mainly due to dermal injury and as a response to disruptions in the integrity of the skin in high skin tension areas. However, studies have hypothesized the contribution of cellular immunological responses related to vaccines.40
Such responses involve disturbed regulation of collagen equilibrium, genetic immune dysfunction, immune reaction to sebum, as well as plasminogen activator inhibition, and finally, decreased apoptosis and hypoxia41 (Figure 4).
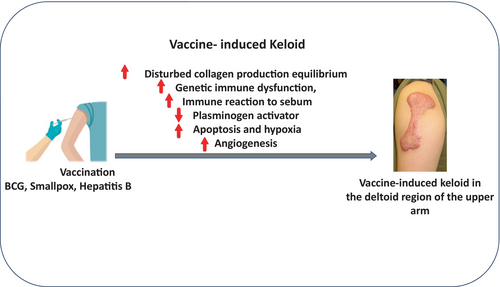
While tattoo-related keloids maybe mainly stimulated by the used painting materials and additives,42 resulting in immune response and accumulation of inflammatory cells in the injected areas.43
Moreover, Tranilast (N-(3,4-dimethoxycinnamoyl) anthranilic acid), an anti-allergic drug, has been approved in Japan and Korea as a treatment for hypertrophic scarring by inhibiting the release of histamine and prostaglandins from mast cells as well as suppressing collagen synthesis by down-regulating TGF-β1.44 It also inhibits the production of various pro-inflammatory cytokines (e.g., IL-8).45
1.1.5 Cancer
Keloids display many cancer-like characteristics such as progressive uncontrolled growth, lack of regression spontaneously and the high rates of recurrence.46 However, keloids show no malignant proliferative potential and never metastasize.
A recent retrospective study using the Taiwan National Health Insurance Research Database (NHIRD) performed the first matched study in an Asian population by analysing 17 401 patients with keloids and 69 604 controls, which indicates that patients with keloids have a higher risk than normal for several cancer types, especially skin cancers in both genders and pancreatic cancer particularly in females.47
The underlying mechanism has not yet been determined; however, previous studies indicate that keloids and human cancers may share similar pathophysiological processes.48 For instance, prolonged inflammation with elevated pro-inflammatory cytokines in injured tissues contributes to keloidogenesis.49 Similarly, chronic inflammation is also known to promote tumour development and progression of some cancers such as skin cancers.50
In case of inflammation associated with wound healing, the pro-inflammatory cytokine TNF-α controls inflammatory cell populations and mediates many of the other aspects of the inflammatory process.51
Therefore, we assume that chronic inflammation is likely to result in fibrosis that may mediate the development of both keloids and cancers.52, 53 Moreover, subsequent studies have shown a contributing role of TGF-β/Smad signalling in keloids development. In parallel, TGF-β/Smad signalling has been also reported in the development of skin cancers.54 Therefore, TGF-β/Smad signalling maybe linked to the pathogenesis of both keloids and cancers.
Moreover, commonalities between keloids and keloidal dermatofibromas suggest a link between genetics, provocative events that induce myofibroblast differentiation and keloidal collagen production.55
1.1.6 Systemic inflammation and infections
The development and severity of pathological scars are additionally aggravated by inflammations predisposed by lymphatic disorders, bacterial and viral infections.
Lymphoproliferative disorder
We experienced a case of an adult woman with Castleman disease whose auricular keloids were exaggerated during the course of her disease.56 Castleman disease is defined as a rare lymphoproliferative disorder that is characterized by the unregulated overproduction of interleukin-6 (IL-6), leading to systemic lymphadenopathy and constitutional inflammatory symptoms. When the circulating concentrations of inflammatory cytokines were increased, her auricular keloids were aggravated. Systemic inflammation is likely to occur in patients with extensive burns due to the associated cytokine storm that significantly increases the risk of developing keloids and hypertrophic scars.
Bacterial infections
Moreover, keloids may develop due to bacterial infections, for instance, leprosy which is a bacterial disease caused by Mycobacterium leprae bacillus, affects mainly peripheral nerves and skin.57 In the skin, M. leprae has an affinity for keratinocytes, macrophages, and histiocytes,58 thus produces dermatological manifestations including keloids development occasionally in some types of leprosy such as Erythema Nodosum Leprosum (ENL), which results in cellular dysfunction as well as antigen–antibody complexes being deposited directly into tissues,59 resulting in both acute nerve and skin inflammation, which is another predisposing cause to keloids. Previous reports have also shown that chronic inflammation in acne patients predisposed by Propionibacterium acnes is associated with high risk of developing scars such as keloids,60 Majorly by pathogenesis of androgen-induced increased sebum hyperproduction, altered follicular keratinization.61, 62
Viral infections
Despite the lack of literature on viral infection involvement with the development of keloidal scars, some existing reports have demonstrated the possibility of herpes zoster lesions to heal with the formation of keloids on top of herpes zoster scar, which can be explained either as an isotopic phenomenon or presence of deeper, long standing herpes zoster lesions and development of secondary bacterial infection due to the long-term immunosuppressive therapy may be the other possible mechanisms of this keloids formation.63
1.2 Genetic disorders and keloids
The incidence of keloids varies among different ethnicities, which reflects the association with multiple genetic variation. Many reports have been published on keloidogenesis associated with gene mutations.64
Particularly, several Mendelian disorders manifest keloids as part of their clinical features. For instance, individuals with a connective-tissue disorder, for example, have a possibility of developing keloids as part of their disease. The diseases that associate with an increased risk of keloid include: the Rubinstein-Taybi syndrome (RSTS), the Ehlers-Danlos syndrome, the Lowe syndrome, Goeminne syndrome and others.
1.2.1 Rubinstein-Taybi syndrome
Rubinstein-Taybi syndrome (RSTS) patients have been reported to develop keloids with high frequency occurring in 24% (15/62) of RSTS patients, either spontaneously or secondary to minor trauma.65 RSTS is an autosomal dominant neurodevelopmental disorder characterized by growth deficiency, broad thumbs and great toes, intellectual disability and characteristic craniofacial appearance. A questionnaire-based study of 61 adults with RSTS ranging in age from 18 to 67 years found that 57% of patients developed keloids. In addition, 28 patients exhibited keloids in a series of 574 examined individuals with RSTS.66
1.2.2 Ehlers-Danlos syndrome type IV
The Ehlers-Danlos syndrome type IV (the vascular subtype) is an inherited disorder of connective tissue that is characterized by acrogeria, translucent skin, propensity to bruising, and significant arterial, digestive and uterine complications.67 The causative mutation is in COL3A1 gene, which encodes the pro-α1(III) chain of collagen type III.68 Several case reports show that this syndrome can paradoxically associate with extensive keloid formation.69
1.2.3 The Lowe syndrome
The so-called oculocerebrorenal syndrome of Lowe (OCRL) affects the eyes, nervous system and kidneys due to mutation in the OCRL gene that reduces the amount of the OCRL-1 protein.70 The formation of corneal keloids in patients with Lowe syndrome is relatively common. It is generally provoked by corneal contact lens use or after intraocular lens implantation.71
1.2.4 Goeminne Torticollis-keloids-cryptorchidism-renal dysplasia syndrome
Goeminne Torticollis-keloids-cryptorchidism-renal dysplasia syndrome was reported in a family with six affected members in whom two patients also developed multiple keloids.72 Another distinct X-linked syndrome of FLNA mutations leads to joint contractures, keloids, large optic cup-to-disc ratio and renal stones.73
1.3 Lifestyle and daily habits
1.3.1 Physical work
During the process of daily physical work, mechanical force is induced, which strongly modulates the cellular behaviour, resulting in keloids formation, not only does the mechanical force affect their location and shape, but also it plays a role in keloids generation, even in patients who are genetically predisposed to develop keloids.74
More recently, the interplay between mechanical factors such as stress, strain and stiffness in keloids revealing enhanced keloids progression via mechanotransduction pathway and elevated inflammation and proliferation due to combination of high stress in the edge of the keloids, and increased mechanical strain in the peripheral tissue surrounding keloids when subjected to mechanical loading such as skin stretching.75
Studies showed that keloids also tend to occur in sites that are highly mobile and of high tension, (e.g., the anterior chest, shoulder, and upper arm) (Figure 5), while rarely occurring on the regions possessing little forces (e.g., the scalp or the anterior lower leg).76 Moreover, the direction and shapes of keloids depend on their location and force. For example, keloids on the anterior chest grow in a ‘crab's claw’, whereas shoulder keloids grow in a ‘butterfly’ or ‘dumbbell’ shape, which demonstrates the predominant direction of mechanical force distribution, unlike normal scars.77, 78
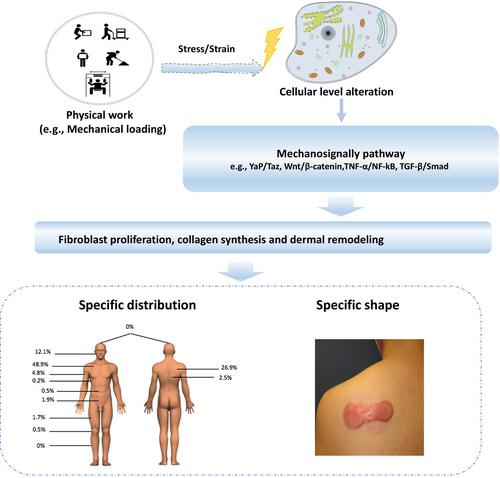
The mechanism is highly linked to the skin mechanotransduction pathways (e.g., Yap/Taz, Wnt/β-catenin, TGF-β/Smad),79, 80 nerve growth factor (NGF) activation,81 the enhanced inflammation and weakened apoptosis, as well as the stimulated mechanosensitive nociceptors in nerve fibres when the skin is subjected to stretch, thus driving fibroblast proliferation, collagen synthesis and dermal remodelling. Moreover, it is suggested that high tension with cyclic skin stretch may alter cell physiology more effectively than continuous stretch through mechanoreceptors.82
These observations suggest that we should focus on reducing the mechanical forces on the inflammation of wounds/pathologic scars in the clinical setting and daily life.
1.3.2 Other lifestyle-related factors
Cutaneous pathological scarring may also be shaped, albeit more indirectly, by the systemic environment that is created by lifestyle habits, including diet, alcohol intake and smoking.
High-fat diets and alcohol intakes are linked with various malfunctions including increased inflammatory phase, dyslipidaemia, insulin resistance and increased formation of reactive oxygen species (ROS).83, 84 ROS formation can damage cell structures as lipids, proteins and DNA, altering the immune response and decreasing mediators' release. The excessive ROS generation can lead to chronic inflammation, degeneration and cell death, compromising the wound healing process.85 Besides, other factors such as vascular alterations are also associated with high-fat diets and alcohol consumption, potentially affecting cell metabolism and tissue healing.86
Pre-clinical study investigating the effect of high-fat diet and alcohol intake in wound healing has shown it may lead to disorganized deposition of collagen fibres, usually observed during inflammation, leading to an incorrect deposition of the extracellular matrix, keloids formation and hypertrophic scars.87
Academically, there is no evidence describing a certain link between spicy food (the main effective constitution is capsaicin) and keloids development. However, from our clinical experience and collected reports from keloids patients, spicy/hot food as well as the alcohol intake have been observed to aggravate the inflammation, increase their itchiness, pain and redness of the scar.
The mechanism of capsaicin can briefly be described as capsaicin enhances endothelium-dependent vasodilation through perivascular sensory neurons.88
Smoking is generally believed to impair wound healing, causing higher postoperative wound infection and other perioperative complications.89 These mechanisms involve impairing the phagocytic and bactericidal activity of inflammatory cells, inhibiting fibroblast migration and reducing collagen deposition.90-92
Smokers were also found to have broader and more disfiguring-coloured scars after laparotomy sterilization than non-smokers.93
Thus, smoking may alter the inflammatory response resulting in more wound complications but also less active scarring.
2 OVERALL DISCUSSION AND FUTURE DIRECTIONS
The aetiology of pathological scars particularly keloids remains multifactorial and unclearly elucidated; contributing factors may involve genetic, local mechanical and systemic factors.
Herein, we summarized the main systemic factors that shape cutaneous pathological scarring, especially keloid formation and aggravation such as circulating cytokines, chemokines, growth factors, particular cell types, sex hormones, and the systemic renin-angiotensin system involved in systemic and genetic disorders, all of which directly shape the angiogenesis, inflammation, fibrosis and remodelling in pathological scars.
Moreover, several environmental factors indirectly influence pathological scar formation or progression, namely physical exercise, diet, alcohol intake and smoking. Notably, much of the evidence on these systemic factors focus on their effects on one pathological scar characteristic, namely their fibrosis.
These findings suggest that molecular, cellular and/or tissue-level approaches that target one or more of these risk factors may be promising scar therapies. Indeed, there is increasing evidence that these approaches may be effective in the clinic.
Despite this, the current clinical treatment strategies continue to focus on decreasing inflammatory processes. Further research into scar-related genetics, epigenetics and mechanobiology is needed,94 as it is likely to help identify more effective prophylactic and clinical treatment strategies for wounds and scars.
3 CONCLUSION
Keloids development and severity are influenced by systemic diseases, genetic disorders and lifestyle as well as natural environment. Dysregulated inflammation contributes to the pathogenesis of scar formation. Immune cells, soluble inflammatory mediators and the related intracellular signal transduction pathways are subtopics encompassing the events occurring in inflammation associated with scar formation.
And studies into their association with keloids along with considering strategies to control such factors may help clinicians to prevent keloids and widen the therapeutic options.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data openly available in a public repository that issues datasets with DOIs.




