RETRACTED: Comparative analysis of pressure ulcer development in stroke patients within and outside healthcare facilities: A systematic review and meta-analysis
Guifen Yu, Changqing Sun and Sha Hao are Joint first authors.
Abstract
The risk of pressure ulcers in stroke patients is a significant concern, impacting their recovery and quality of life. This systematic review and meta-analysis investigate the prevalence and risk factors of pressure ulcers in stroke patients, comparing those in healthcare facilities with those in home-based or non-clinical environments. The study aims to elucidate how different care settings affect the development of pressure ulcers, serving as a crucial indicator of patient care quality and management across diverse healthcare contexts. Following PRISMA guidelines, a comprehensive search was conducted across PubMed, Embase, Web of Science and the Cochrane Library. Inclusion criteria encompassed studies on stroke patients in various settings, reporting on the incidence or prevalence of pressure ulcers. Exclusion criteria included non-stroke patients, non-original research and studies with incomplete data. The Newcastle–Ottawa scale was used for quality assessment, and statistical analyses involved both fixed-effect and random-effects models, depending on the heterogeneity observed. A total of 1542 articles were initially identified, with 11 studies meeting the inclusion criteria. The studies exhibited significant heterogeneity, necessitating the use of a random-effects model. The pooled prevalence of pressure injuries was 9.53% in patients without family medical services and 2.64% in patients with medical services. Sensitivity analysis confirmed the stability of these results, and no significant publication bias was detected through funnel plot analysis and Egger's linear regression test. The meta-analysis underscores the heightened risk of pressure injuries in stroke patients, especially post-discharge. It calls for concerted efforts among healthcare providers, policymakers and caregivers to implement targeted strategies tailored to the specific needs of different care environments. Future research should focus on developing and evaluating interventions to effectively integrate into routine care and reduce the incidence of pressure injuries in stroke patients.
1 INTRODUCTION
Stroke, one of the leading causes of long-term disability worldwide, annually impacts millions, posing substantial challenges for both individuals and healthcare systems.1 This condition is not only detrimental to the health of affected individuals but also imposes significant strains on medical care resources.2, 3 Among the myriad of post-stroke complications, pressure ulcers (PUs), also known as bedsores or decubitus ulcers, emerge as a common and critical issue. These lesions, resulting from sustained pressure leading to damage of skin and underlying tissues, are particularly prevalent in patients with reduced mobility, a frequent consequence of stroke.4, 5 The development of PUs in this patient population is a matter of considerable concern due to their adverse effects on quality of life, heightened infection risk and the complexities associated with their management.
The pathogenesis of PUs in stroke survivors is intricate and multifactorial. Stroke-related complications such as reduced mobility, sensory impairment and incontinence markedly escalate the risk of PU development. These ulcers not only inflict severe physical discomfort but also exert a substantial psychological toll on both patients and their caregivers. The economic impact of treating PUs is noteworthy, further exacerbating the already substantial financial burden of stroke management. Despite widespread recognition of PUs in stroke patients, there is a pronounced disparity in the reported incidence rates of PUs between patients in healthcare facilities and those in non-clinical settings.6 Healthcare facilities, equipped with specialized pressure-relieving mattresses and skilled healthcare personnel, are presumed to provide more effective prevention and management of PUs. Nevertheless, the variability in care practices, patient monitoring and resource allocation across different care settings potentially contributes to the observed differences in PU incidence rates. Moreover, environmental factors play a significant role in the risk of PU development among stroke survivors.7, 8 The level of care resources and expertise in home or community settings may differ from that in medical institutions, potentially affecting the effectiveness of PU prevention and treatment. Furthermore, while family members often serve as primary caregivers in non-clinical settings, their involvement in PU management is pivotal.9 Enhancing their knowledge and skills in areas such as proper positioning techniques, skin assessment protocols and early signs of pressure injury development could significantly contribute to the prevention and early intervention of PUs. Educational interventions targeting caregivers should emphasize the importance of regular repositioning, maintaining skin hygiene and identifying risk factors for PU development.10
Given this background, the purpose of this study is to conduct a systematic review and meta-analysis to comprehensively compare the development of PUs in stroke patients residing in healthcare facilities versus those in non-clinical environments. This research aims to identify the factors contributing to the variance in PU incidence rates and evaluate the effectiveness of different preventive and treatment strategies implemented across various settings. By examining existing literature and aggregating data from multiple studies, this analysis intends to provide insights into the effects of care settings on PU development in stroke patients.
2 MATERIALS AND METHODS
2.1 Search strategy
In conducting this meta-analysis, our search strategy strictly conformed to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.11 On 19th December 2023, we executed a thorough search across four major electronic databases: PubMed, Embase, Web of Science and the Cochrane Library. This search was not confined by any temporal limitations, ensuring a comprehensive data collection. We employed a range of carefully selected key terms to align with the patient, intervention, comparison, outcome (PICO) framework, thereby guaranteeing a thorough and relevant study retrieval. These terms included ‘Pressure ulcer,’ ‘pressure injury,’ ‘bed sore’ and ‘stroke,’ along with the term ‘prevalence.’ This approach was designed to capture the extensive scope of our research topic. Additionally, to enhance the inclusivity of our search, we imposed no restrictions based on language. We also meticulously screened the reference lists of pertinent articles to identify any additional records that could potentially contribute to our meta-analysis.
2.2 Inclusion criteria and exclusion criteria
2.2.1 Inclusion criteria
- Study design: We included randomized controlled trials (RCTs), cohort studies, case–control studies and cross-sectional studies.
- Participants: Studies involving stroke patients of any age, gender or stroke subtype were considered.
- Settings: The research needed to compare pressure ulcer development in stroke patients in healthcare facilities (such as hospitals and long-term care facilities) or those in non-clinical settings (like home care).
- Outcomes: Studies must have reported on the incidence or prevalence of PUs, their severity or associated risk factors.
- Time frame: No restriction was placed on the duration of follow-up for longitudinal studies.
2.2.2 Exclusion criteria
- Non-stroke patients: Studies not specifically focused on stroke patients were excluded.
- Non-original research: Reviews, editorials, opinions and animal studies were excluded.
- Incomplete data: Studies with incomplete or ambiguous data regarding pressure ulcer development in stroke patients were not considered.
2.3 Data extraction
During our meta-analysis, two independent evaluators conducted the literature screening and data extraction processes, ensuring accuracy through cross-checking. In instances of discrepancies, the evaluators engaged in discussions to resolve these issues and, if needed, consulted a third-party reviewer for an objective resolution. The extracted data encompassed essential details such as the author(s) of each study, publication year, number of cases examined, country of the study, study design and prevalence rates of PUs. In situations where the published reports did not provide specific data of interest, we reached out to the original study investigators via email to request any relevant unpublished data. This meticulous approach to data extraction was vital for the integrity and thoroughness of our meta-analysis.
2.4 Quality assessment
In our meta-analysis, the quality assessment of the included studies was meticulously conducted by two independent reviewers employing the Newcastle–Ottawa scale (NOS).12 This scale, recognized for its robustness, evaluates studies across three primary domains: selection, comparability and outcome. These domains are instrumental in identifying potential biases within the studies. The scoring system of the NOS is structured such that each criterion met within these domains is signified by an asterisk, contributing to the study's overall quality score, which can range from 0 to 9. The final quality assessment was classified as follows: studies with scores from 0 to 3 were categorized as low quality, those with scores ranging from 4 to 6 were considered of moderate quality, and studies with scores from 7 to 9 were classified as high quality. This rigorous quality assessment was crucial in ensuring the reliability and validity of our meta-analysis findings.
2.5 Statistical analyses
In our meta-analysis, the statistical analyses were conducted following a structured and systematic approach. Initially, the heterogeneity among the included studies was assessed using chi-square statistics, quantified by the I2 value. When the I2 value was less than 50%, and the corresponding p-value was more than or equal to 0.10, indicating negligible heterogeneity, we employed the fixed-effect model to compute the combined effect size. Conversely, in scenarios where the I2 value equalled or exceeded 50%, or the p-value was less than 0.10, suggesting significant heterogeneity, the random-effects model was utilized for calculating the combined effect size. Sensitivity analysis played a crucial role in our study, aiming to ascertain the robustness of the results and to identify potential sources of heterogeneity. This involved sequentially omitting each study from the meta-analysis and recalculating the overall effect size to determine the influence of individual studies. To detect any potential publication bias, we analysed the symmetry of the funnel plot. A balanced distribution of data points on both sides of the funnel plot's apex would indicate a lower likelihood of the results being skewed by publication bias. Furthermore, Egger's linear regression test was employed as a quantitative tool for identifying any publication bias. All statistical tests were two-sided, with a p-value of less than 0.05 considered statistically significant. The data analysis was carried out using Stata version 17 (StataCorp, College Station, TX, USA), ensuring accuracy and reliability in our statistical evaluations.
3 RESULTS
3.1 Search results and study selection
In the initial stage of our systematic review and meta-analysis, an extensive search across multiple electronic databases yielded 1542 potentially relevant articles. We then implemented an algorithm to eliminate duplicates, ensuring each study was unique. Subsequently, titles and abstracts were rigorously evaluated against our predefined inclusion and exclusion criteria, which encompassed study methodology, participant demographics, clinical outcomes and research quality. This process resulted in a selection of 45 articles for detailed analysis. Independent investigators thoroughly reviewed the full texts of these articles, leading to the exclusion of 34 for various reasons: 14 were review articles, 7 were sequentially published works, 8 lacked sufficient data for analysis and 5 were clinical trials without control groups. Ultimately, 11 articles met all criteria and were included in our final meta-analysis6, 13-22 (Figure 1).

3.2 Summary of study characteristics in the meta-analysis
The meta-analysis incorporated a diverse range of studies, reflecting a broad spectrum of research on the prevalence of PUs in stroke patients across various countries and healthcare settings. The studies spanned from 2008 to 2019, encompassing research from countries including China, India, Thailand, Indonesia, the United States, Denmark and England. The sample sizes of these studies varied considerably, ranging from as few as 36 participants in smaller scale studies to as many as 903 467 in larger studies. A mix of study designs was represented, including cross-sectional, prospective, prospective observational studies and prospective cohorts. This diversity in methodology underscores the varied approaches to studying pressure ulcer prevalence in different patient populations and settings. The prevalence rates reported by these studies also showed a wide range, from as low as 0.8% to as high as 47.6%, indicating significant variability in pressure ulcer occurrence across different regions and study designs. The characteristics of studies included in this systematic review are presented in Table 1.
| Authors | Year | Study design | Country | Sample Size | Prevalence (%) | Setting |
|---|---|---|---|---|---|---|
| Cai et al. | 2019 | Cross-sectional | China | 6961 | 2 | Community |
| Liao et al. | 2019 | Prospective study | China | 12 415 | 0.8 | Hospital |
| Pandian et al. | 2016 | Prospective | India | 449 | 4 | Hospital |
| Kuptniratsaikul et al. | 2013 | Prospective observational study | Thailand | 240 | 2.6 | Community |
| Amir et al. | 2013 | Cross-sectional | Indonesia | 36 | 28 | Hospital |
| Rahman et al. | 2013 | Cross-sectional | The US | 903 467 | 2.19 | Hospital |
| Suttipong et al. | 2012 | Cross-sectional | Thailand | 168 | 47.6 | Community |
| Ingeman et al. | 2011 | Cross-sectional | Denmark | 11 757 | 1.2 | Hospital |
| Kitisomprayoonkul et al. | 2010 | Prospective observational study | Thailand | 118 | 1.7 | Community |
| Kwong et al. | 2009 | Prospective cohort | China | 120 | 35 | Community |
| Sackley et al. | 2008 | Prospective study | England | 122 | 22 | Hospital |
3.3 Quality assessment summary based on the Newcastle–Ottawa scale
The quality assessment of the cohort studies included in our meta-analysis was conducted using the Newcastle–Ottawa scale (NOS), a renowned tool for evaluating non-randomized studies in meta-analyses. Across the assessed studies, the quality scores varied, with the majority achieving high scores, indicative of robust methodological quality. The evaluation encompassed several critical dimensions, including the representativeness of the exposed cohort, selection of the non-exposed cohort, ascertainment of exposure, ensuring the outcome of interest was not present at the start of the study, comparability of cohorts on design or analysis basis, assessment of outcome, length of follow-up and the adequacy of follow-up of cohorts. Most studies demonstrated strong performance across these categories, reflecting a comprehensive and rigorous approach in their design and execution. Notably, several studies achieved the highest possible score of 9, suggesting exceptional quality in terms of selection, comparability and outcome assessment. Others, with scores of 7 or 8, still reflected a high standard of research quality, albeit with minor areas for improvement in certain aspects of their methodology. Overall, the quality assessment results using the NOS revealed that the majority of the studies included in this meta-analysis were of high quality, providing a strong and reliable basis for the analysis of pressure ulcer prevalence among stroke patients. The high scores across most studies reinforce the validity of their findings and contribute to the credibility of the overall meta-analysis results (Table 2).
| Study | Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Comparability of cohorts on the basis of the design or analysis | Assessment of outcome | Was follow-up long enough | Adequacy of follow-up of cohorts | Total score |
|---|---|---|---|---|---|---|---|---|---|
| Cai et al. | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| Liao et al. | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 7 | |
| Pandian et al. | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 7 | |
| Kuptniratsaikul et al. | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 8 |
| Amir et al. | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| Rahman et al. | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 8 | |
| Suttipong et al. | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | 8 | |
| Ingeman et al. | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| Kitisomprayoonkul et al. | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| Kwong et al. | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| Sackley et al. | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
- Note: ★ Each individual asterisk (‘★’) signifies one point.
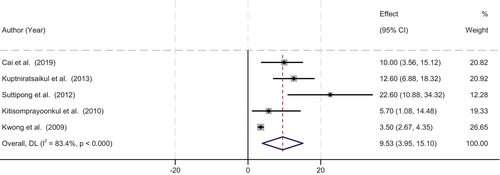
3.4 Meta-analysis results: Prevalence of pressure injuries in home patients without family medical services
Our meta-analysis scrutinized the prevalence of pressure injuries among home-based patients lacking family medical services, focusing on the insights gleaned from five distinct studies. A significant heterogeneity was observed across these studies (p < 0.001, I-squared = 83.4%), necessitating the application of a random-effects model for the analysis. The pooled prevalence rate of pressure injuries in this specific patient population was estimated at 9.53% (95% Confidence Interval [CI]: 3.95–15.10), as depicted in Figure 2. This high level of heterogeneity may be attributed to various factors, including differences in study populations, methodologies and the criteria used for diagnosing pressure injuries. It underscores the complexity and variability in the manifestation and reporting of pressure injuries in home-based patients without access to family medical services. This finding highlights a significant concern in home healthcare, particularly for patients who rely solely on non-family medical support. The absence of family medical services might contribute to a higher risk of pressure injuries due to factors such as inadequate routine monitoring, potential delays in seeking medical advice, or limited access to preventive care and patient education. This situation calls for an increased focus on developing effective strategies to manage and prevent pressure injuries in this vulnerable group, emphasizing the need for enhanced home healthcare services and patient education programmes.
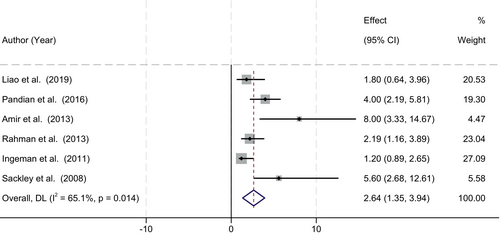
3.5 Meta-analysis results: Prevalence of pressure injuries in patients with medical services
In our meta-analysis, we focused on the prevalence of pressure injuries in patients receiving medical services, synthesizing data from six studies. Notably, these studies exhibited considerable heterogeneity (p = 0.014, I-squared = 65.1%), indicating varied outcomes and methodologies among the included research. Consequently, a random-effects model was employed to estimate the combined prevalence rate. The calculated pooled prevalence rate of pressure injuries in patients with access to medical services was found to be 2.64% (95% Confidence Interval [CI]: 1.35–3.94), as illustrated in Figure 3. This relatively lower prevalence, as compared with populations without medical services, suggests the potential benefits of medical supervision and intervention in the management and prevention of pressure injuries. The observed heterogeneity could be attributed to differences in the intensity and type of medical services provided, the severity of patient conditions and the variability in pressure injury assessment criteria across the studies. It reflects the complex nature of pressure injury development and the influence of medical care quality on its prevalence.
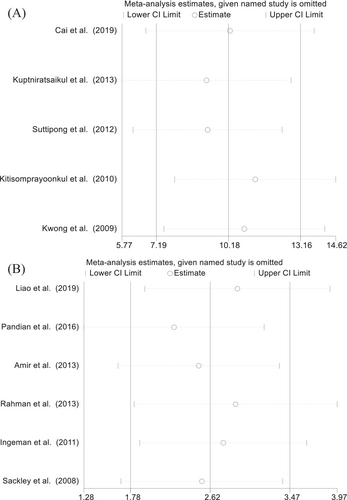
3.6 Sensitivity analysis for meta-analysis: Assessing the robustness of findings
In light of the significant heterogeneity identified among the studies in our meta-analysis, we undertook a sensitivity analysis to evaluate the robustness and stability of our combined results. This process involved a methodical exclusion of each study in a sequential manner, followed by a re-calculated estimation of the combined effect sizes for the remaining studies. This thorough approach to sensitivity analysis demonstrated that the aggregate results were consistently stable and robust, regardless of the exclusion of any particular study. Such a finding is indicative of the fact that no single study disproportionately swayed the overall outcomes of the meta-analysis. This aspect considerably strengthens the reliability and credibility of our pooled results. Moreover, the consistent nature of the outcomes across these sensitivity analyses highlights the solidity of our primary conclusions. It affirms the integrity of the methodological approach and the collective findings of the included studies. This comprehensive sensitivity analysis not only reinforces the validity of the meta-analysis but also provides confidence in the generalizability and applicability of its conclusions, as represented in Figure 4.
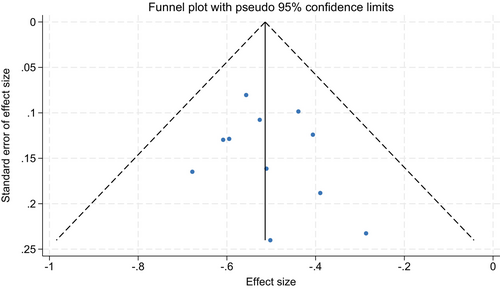
3.7 Publication bias assessment in the meta-analysis
To evaluate potential publication bias within our meta-analysis, we conducted a comprehensive analysis using funnel plots and Egger's linear regression test. The funnel plots, which graphically represent the relationship between study size and effect size, were constructed using the data from the included studies. These plots demonstrated a symmetric distribution (as shown in Figure 5), suggesting the absence of publication bias. Additionally, Egger's linear regression test was employed to quantitatively assess publication bias across various variables within the meta-analysis. The results of this test revealed no significant publication bias (p > 0.05), further corroborating the symmetry observed in the funnel plots. This lack of significant publication bias in Egger's test provides additional evidence supporting the reliability and robustness of our meta-analysis findings.
4 DISCUSSION
The prevalence of PUs in stroke patients is a pressing concern due to its implications for patient morbidity, healthcare costs and quality of life. Stroke patients are particularly susceptible to PUs due to factors such as immobility, neurological deficits and the overall compromised health status.23 This vulnerability is compounded by the care environment, be it within healthcare facilities with structured medical care or in home settings where medical resources might be more limited.24, 25 Our analysis revealed notable differences in the prevalence of PUs between stroke patients in healthcare facilities and those in non-clinical settings. This disparity could be attributed to several factors. In healthcare facilities, the presence of trained healthcare professionals, access to specialized equipment (like pressure-relieving mattresses) and adherence to established protocols for pressure ulcer prevention can significantly reduce the incidence. Conversely, in non-clinical settings, limited access to medical resources, lack of professional care and potential delays in identifying and treating PUs can increase risks. However, the occurrence of PUs in healthcare facilities also highlights the challenges in preventing these conditions even in resource-rich environments. It points to the need for continuous evaluation and improvement of existing protocols and practices, emphasizing the importance of individualized patient care plans and regular monitoring.
This meta-analysis sheds light on the prevalence of pressure injuries in two distinct patient populations: those without family medical services and those with access to medical care. Our findings reveal a stark contrast in the prevalence rates between these groups, with a higher prevalence observed in patients without family medical services. This disparity can be attributed to several underlying mechanisms and factors, which we discuss here. First, the higher prevalence of pressure injuries among home-based patients without family medical services (9.53%) compared with those with medical services (2.64%) highlights the critical role of medical supervision and intervention. The absence of family medical services often correlates with a lack of regular health monitoring, delayed medical interventions and limited access to preventive measures.18, 26 This situation can lead to a higher risk of developing pressure injuries, as routine monitoring and early intervention are key components in preventing the onset and exacerbation of these injuries.
The significant heterogeneity observed in both patient groups (83.4% in patients without medical services and 65.1% in those with medical services) underscores the complexity of pressure injury development. This heterogeneity might be influenced by varying methodologies in the studies, different patient demographics and the criteria used for diagnosing pressure injuries. It also reflects the diverse nature of healthcare practices and patient management strategies across different settings. The higher prevalence in the non-medical service group suggests a need for targeted interventions. This includes enhancing home healthcare services, increasing patient and caregiver education about pressure injury prevention, and improving access to medical resources.27, 28 For patients with access to medical services, the emphasis should be on maintaining the quality of care and ensuring consistent implementation of best practices for pressure injury prevention and management.
Our sensitivity analysis indicated that the results of the meta-analysis were robust and stable, unaffected by the exclusion of any single study. This finding suggests that the overall conclusions drawn from the meta-analysis are reliable and not overly influenced by individual study variations. It strengthens the argument for the need for improved care strategies in both patient groups, especially for those lacking family medical services. Furthermore, the absence of significant publication bias, as confirmed by the symmetric funnel plots and Egger's linear regression test, adds credibility to our results. This indicates that our findings are likely representative of the true situation and not skewed by selective reporting of studies.
This meta-analysis, while comprehensive, does have several limitations. First, the significant heterogeneity among the included studies poses a challenge. Variations in study designs, patient demographics and methodologies can influence the comparability of the results. Second, the majority of the studies rely on observational data, which, despite being informative, cannot establish causality. Additionally, there might be a publication bias, as studies with negative or inconclusive results are less likely to be published. Moreover, the data predominantly come from high-resource settings, which may not be generalizable to low-resource environments where healthcare infrastructure and practices differ substantially. Finally, language bias may exist as studies published in languages other than English were not included, potentially omitting relevant data.
To overcome these limitations in future research, there is a need for more rigorous study designs, including prospective cohort studies with well-defined control groups and, where feasible, RCTs. Such studies would allow for a more detailed analysis of causative relationships between care environments and pressure ulcer development in stroke patients. Additionally, incorporating mixed-methods research could enrich quantitative findings with qualitative insights, providing a more nuanced understanding of patient care dynamics in different settings. Future studies should also aim to include data from a broader range of geographic locations and healthcare contexts, particularly from low-resource settings, to enhance the generalizability of the findings. Efforts to minimize publication and language bias by encouraging the publication of studies with negative or inconclusive results and including research published in multiple languages would further strengthen the evidence base.
5 CONCLUSIONS
In conclusion, this systematic review highlights the increased risk of pressure injuries in stroke patients, particularly post-discharge, underscoring a significant challenge in patient care. It calls for a collaborative effort among healthcare providers, policymakers and caregivers to bridge care gaps and implement effective, environment-specific strategies. Future research should focus on developing and evaluating interventions that can be seamlessly integrated into routine care for stroke patients, aiming to substantially reduce the incidence of pressure injuries.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




