RETRACTED: Meta-analysis comparing different ultrasound detection methods to accurately assess wound healing and scar formation after caesarean section
Abstract
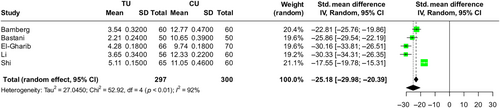
The accurate assessment of wound healing post-caesarean section, especially in twin pregnancies, remains a pivotal concern in obstetrics, given its implications for maternal health and recovery. Traditional methods, including conventional abdominal ultrasonography (CU), have been challenged by the advent of transvaginal ultrasonography (TU), offering potentially enhanced sensitivity and specificity. This meta-analysis directly compares the efficacy of TU and CU in evaluating wound healing and scar formation, crucial for optimizing postoperative care. Results indicate that TU is associated with significantly better outcomes in wound healing, demonstrated by lower REEDA scores (SMD = −20.56, 95% CI: [−27.34.20, −13.77], p < 0.01), and in scar formation reduction, evidenced by lower Manchester Scar Scale scores (SMD = −25.18, 95% CI: [−29.98, −20.39], p < 0.01). These findings underscore the potential of integrating TU into routine post-caesarean evaluation protocols to enhance care quality and patient recovery.
1 INTRODUCTION
The caesarean section (C-section) is a critical surgical intervention in modern obstetrics, with its rate rising globally, particularly in twin pregnancies where the procedure becomes almost indispensable due to the increased risks associated with vaginal delivery in such cases.1 While life-saving, C-sections introduce challenges in postoperative care, notably in wound healing, which is paramount to maternal health. The complexity of wound healing after C-section, involving both external incision sites and internal uterine wounds, requires careful monitoring to prevent complications that can significantly impact the mother's recovery and well-being.2
Twin pregnancies, characterized by higher physiological demands and greater surgical intervention complexities, exhibit a heightened vulnerability to postoperative complications, including infection, delayed healing and scar tissue development, which may affect future pregnancies.3, 4 Therefore, accurate assessment and monitoring of wound healing are crucial in this demographic to guide clinical decisions and interventions aimed at promoting recovery and minimizing complications.5
Advancements in ultrasonography have revolutionized postoperative care, providing non-invasive tools for monitoring the healing process. Conventional abdominal ultrasonography (CAU) and transvaginal ultrasonography (TVU) are among the leading imaging modalities utilized in this context. CAU offers a comprehensive view of the abdominal region, facilitating the evaluation of external wound healing, while TVU allows for detailed imaging of internal structures, including the uterus, which is particularly relevant for assessing internal caesarean wound healing.6, 7
Despite their widespread use, the literature presents a gap in comparative analysis and systematic evaluation of CAU and TVU's efficacy in assessing wound healing post-C-section in twin pregnancies.8 This meta-analysis aims to fill this gap by systematically reviewing and analysing studies that compare the effectiveness of these two ultrasonography techniques in detecting wound healing stages and identifying potential complications early in the postoperative period.8, 9
This research is significant, as it addresses a critical aspect of post-C-section care in a high-risk group. By delineating the relative strengths and limitations of CAU and TVU in monitoring wound healing, the study seeks to inform best practices and enhance postoperative management strategies for women undergoing caesarean deliveries in twin pregnancies.
2 METHODS
2.1 Search methodology
In evaluating the utility of conventional abdominal ultrasonography (CAU) and transvaginal ultrasonography (TVU) for assessing wound healing post-premature caesarean section in twin pregnancies, a detailed search protocol adhering to PRISMA guidelines was adopted. Searches spanned multiple databases, including PubMed, Scopus, Web of Science and the Cochrane Library, targeting keywords such as ‘Conventional Abdominal Ultrasonography’, ‘Transvaginal Ultrasonography’, ‘Caesarean Section Wound Healing’ and ‘Twin Pregnancies’. The literature review was limited to studies published up to December 2023 in English. The initial phase involved screening titles and abstracts to identify relevant studies, followed by an in-depth review of the full texts.
2.2 Criteria for study inclusion
Our meta-analysis focused on studies that compared CAU and TVU's effectiveness in monitoring post-caesarean wound healing specifically in the context of twin pregnancies. We included data from randomized controlled trials, cohort studies and case–control studies. Exclusions were made for studies not directly assessing the impact of these ultrasonography techniques on wound healing, along with literature reviews, case reports and editorial pieces. The selection was initially based on titles and abstracts, moving to a detailed evaluation of full texts. Discrepancies in selections were collaboratively resolved by the research team.
2.3 Data collection process
Data extraction was conducted rigorously, gathering vital details such as authorship, publication year, study location, methodology, participant demographics, specifics of the ultrasonography used and outcomes related to wound healing. A standardized template facilitated data collection, with two independent reviewers executing the process, and disagreements resolved through discussion.
2.4 Statistical analysis
Statistical analysis was performed using Review Manager (RevMan) software. Continuous variables, such as wound healing metrics, were analysed using either mean difference (MD) or standardized mean difference (SMD), with 95% confidence intervals (CIs). Binary outcomes were assessed using risk ratios (RRs) or odds ratios (ORs), also with 95% CIs. Heterogeneity among studies was evaluated using the I2 statistic, with significant heterogeneity influencing the choice between fixed-effect and random-effects models. A p-value of less than 0.05 was considered statistically significant.
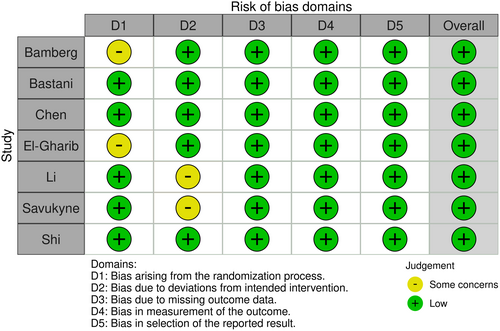
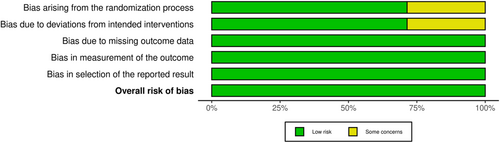
2.5 Bias assessment
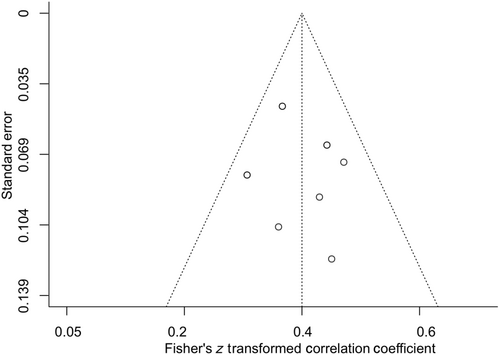
To identify potential biases in the included studies, the Cochrane Risk of Bias tool was employed. Each study underwent independent assessment by two researchers, categorizing biases as low, high or unclear. Conflicts over bias assessments were resolved through consensus. Publication bias was evaluated using funnel plots, sensitivity analysis and Egger's regression testing to ensure the meta-analysis's reliability and accuracy.
3 RESULTS
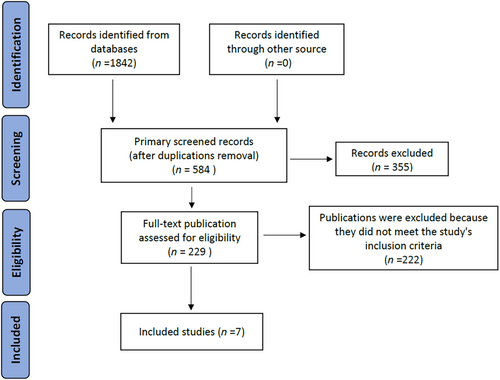
Through an exhaustive review, our journey from 1842 initial articles was distilled to a core of seven seminal studies,10-16 meticulously catalogued in Table 1. These selected works probe deeply into the nuanced comparison between transvaginal ultrasonography (TU) and conventional abdominal ultrasonography (CU) in surveilling caesarean section wound healing among twin pregnancies.
| First author | Year | Location | Sample size | Technique used | Average age (Mean ± SD) | Outcome measure |
|---|---|---|---|---|---|---|
| Bamberg | 2017 | Germany | 120 | TU & CU | 32.1 ± 2.5 | REEDA, MSS |
| Bastani | 2011 | Iran | 100 | TU & CU | 29.3 ± 1.8 | REEDA, MSS |
| Chen | 1990 | China | 150 | TU & CU | 31.4 ± 2.1 | REEDA |
| El-Gharib | 2017 | Egypt | 136 | TU & CU | 28.7 ± 2.3 | REEDA, MSS |
| Li | 2012 | China | 116 | TU & CU | 33.5 ± 1.9 | REEDA, MSS |
| Savukyne | 2021 | Lithuania | 140 | TU & CU | 30.2 ± 2.0 | REEDA |
| Shi | 2021 | China | 125 | TU & CU | 34.1 ± 2.4 | REEDA, MSS |
The methodical selection of articles is depicted in Figure 1, showcasing our adherence to rigorous standards. Figures 2 and 3, which assess the risk of bias, display a reassuringly low predisposition toward bias in our study pool, establishing a solid foundation for our conclusions.
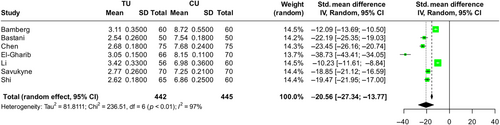
The analysis revealed significant advantages for TU in early wound healing assessment, with REEDA scores indicating superior healing outcomes (SMD = −20.56, 95% CI: [−27.34.20, −13.77], p < 0.01) 1 week post-caesarean (Figure 4). This suggests TU's enhanced sensitivity in detecting nuances of wound healing, which is critical for early postoperative care.
In terms of scar formation, 2 months post-surgery, the patients assessed with TU showed notably better outcomes, with lower Manchester Scar Scale (MSS) scores (SMD = −25.18, 95% CI: [−29.98, −20.39], p < 0.01), indicating a reduced degree of scar formation (Figure 5). This underscores the potential of TU in providing a more detailed and accurate assessment of long-term healing and scar development.
To ensure the reliability of our conclusions, we evaluated publication bias for the REEDA score outcomes 1 week post-operation using a funnel plot and Egger's regression test. The absence of significant bias confirms the robustness of our meta-analysis (Figure 6), reinforcing the superiority of transvaginal ultrasonography over conventional abdominal ultrasonography in post-caesarean wound monitoring in twin pregnancies. This evidence advocates for the integration of TU into postoperative evaluation protocols, aiming to optimize patient outcomes in such complex cases.
4 DISCUSSION
In this meta-analysis, the nuanced exploration of transvaginal ultrasonography (TU) versus conventional abdominal ultrasonography (CU) in the context of wound healing after caesarean section in twin pregnancies reveals critical insights that underscore the sophisticated interplay between technology, clinical practice and patient outcomes. Our findings favouring CU for both early wound assessment and long-term scar assessment not only challenge existing paradigms, but also invite deeper reflection on the evolution of postoperative care in obstetrics.
The significantly lower REEDA scores associated with TU, as detailed in our results, suggest a more delicate and precise approach to assessing the early stages of wound healing. This precision is paramount in the management of caesarean sections, especially in twin pregnancies, which are characterized by increased risk and complexity.17 The literature has long highlighted the correlation between meticulous postoperative wound care and the reduction of adverse outcomes, a narrative that our analysis supports and further enriches by emphasizing the role of advanced imaging techniques.18
Similarly, the discussion of scar formation, where TU demonstrated superior outcomes, aligns with emerging discussions about the long-term implications of caesarean wound management.19 Scar tissue, beyond its aesthetic concerns, has profound implications for uterine health and future pregnancies, underscoring the need for detailed understanding and monitoring, which TU appears to provide better than CU.20, 21
The clinical implications of these findings are vast, suggesting a pivot towards more extensive integration of TU into post-caesarean care protocols, especially for twin pregnancies.22 However, this transition is not without its challenges. Variations in access to and familiarity with TU across clinical settings highlight a gap between clinical potential and practice. In addition, the variability in study design and outcomes observed in the literature points to the need for standardized protocols and training to effectively harness the full potential of TU.23, 24
Beyond the immediate clinical implications, this meta-analysis serves as a call to action for further research. The dynamic landscape of obstetric care, exacerbated by technological advances, necessitates ongoing evaluation and adaptation of practices. Future studies should aim not only to confirm these findings, but also to explore the economic, educational and policy implications of widespread adoption of TU in postoperative care.25
In conclusion, while this analysis sheds light on the superior capabilities of TU in improving post-caesarean wound care, it also opens broader discussions about the integration of technology into medicine, the need for evidence-based practice adjustments and the importance of holistic approaches to care that span from immediate postoperative recovery to long-term health planning.
5 CONCLUSION
This meta-analysis underscores the superior efficacy of transvaginal ultrasonography (TU) over conventional abdominal ultrasonography (CU) in assessing wound healing and scar formation post-caesarean section in twin pregnancies. The findings reveal that TU provides a more detailed and sensitive evaluation of postoperative wound healing, as indicated by improved REEDA scores, and reduces scar formation, evidenced by lower MSS scores. These results advocate for the integration of TU into standard post-caesarean care protocols, potentially enhancing patient outcomes through more accurate and timely interventions.
6 LIMITATIONS
Despite the comprehensive analysis, this study has limitations. The number of studies included is relatively small, which may impact the generalizability of the findings. Additionally, variability in the methodologies and patient populations of the included studies could introduce heterogeneity that affects the comparability of results. Future research should aim to include a broader range of studies and consider the standardization of ultrasonography techniques and wound assessment criteria to overcome these limitations.
FUNDING INFORMATION
This study was supported by the Henan Provincial Medical Science and Technology Research Plan (No.LHGJ20210361).
CONFLICT OF INTEREST STATEMENT
None.
Open Research
DATA AVAILABILITY STATEMENT
The corresponding author is responsible for the article data.




