RETRACTED: Effect of platelet-rich plasma combined with negative pressure wound therapy in treating patients with chronic wounds: A meta-analysis
Abstract
A meta-analysis was conducted to comprehensively explore the effects of platelet-rich plasma (PRP) combined with negative pressure wound therapy (NPWT) in treating patients with chronic wounds. Computer searches were conducted, from database infection to November 2023, in EMBASE, Google Scholar, Cochrane Library, PubMed, Wanfang and China National Knowledge Infrastructure databases for randomized controlled trials (RCTs) on the use of PRP combined with NPWT technology for treating chronic wounds. Two researchers independently screened the literature, extracted data and conducted quality assessments according to the inclusion and exclusion criteria. Stata 17.0 software was employed for data analysis. Overall, 18 RCTs involving 1294 patients with chronic wounds were included. The analysis revealed that, compared with NPWT alone, the use of PRP combined with NPWT technology significantly improved the healing rate (odds ratios [OR] = 1.92, 95% confidence intervals [CIs]: 1.43–2.58, p < 0.001) and total effective rate (OR = 1.31, 95% CI: 1.23–1.39, p < 0.001), and also significantly shortened the healing time of the wound (standardized mean difference = −2.01, 95% CI: −2.58 to −1.45, p < 0.001). This study indicates that the treatment of chronic wounds with PRP combined with NPWT technology can significantly enhance clinical repair effectiveness and accelerate wound healing, with a high healing rate, and is worth further promotion and practice.
1 INTRODUCTION
Chronic wounds are typically defined as wounds that fail to heal or show no tendency to heal after more than 1 month of standard treatment and have entered a pathological inflammatory response state.1, 2 Common chronic wounds include diabetic foot ulcers,3 pressure ulcers,4 infectious ulcers5 and cancerous ulcers.6 Patients with these types of wounds often require long hospital stays, frequent dressing changes and multiple debridement surgeries, yet the clinical outcomes are often poor, leading to severe deformities, disabilities and even amputations.7 Chronic wounds have become a global public health issue, following diabetes, obesity and cancer, imposing a heavy burden on patients, their families and society as a whole.8, 9 Therefore, improving the healing rate of chronic wounds and alleviating the pain and economic burden of patients have become a focus and challenge in wound repair.
Traditional treatments for chronic wounds, such as regular dressing changes, surgical debridement and skin grafting, often fail to provide a conducive growth environment and are thus unable to achieve satisfactory treatment outcomes for patients.10 With the development of cell and molecular biology and scientific progress in tissue regeneration, the treatment methods for chronic wounds have increased, and the materials and methods used clinically are continually being updated.11 Recently, negative pressure wound therapy (NPWT) has been widely applied and developed. Essentially a dressing plus drainage, NPWT can protect the wound, absorb exudates, control infections and promote healing, and it does not require frequent dressing changes. However, it requires equipment and relatively complex operation.12, 13 Platelet-rich plasma (PRP) is a platelet concentrate containing a variety of growth factors and cytokines, which significantly promotes tissue and nerve repair and angiogenesis and has achieved remarkable therapeutic effects in treating chronic wounds.14 Researchers have found that the combined use of PRP and NPWT can accelerate the healing process of chronic wounds and improve the quality of wound healing.15 However, studies on PRP combined with NPWT for chronic wound repair are limited and have not yet reached a consensus. Therefore, this study uses meta-analysis to comprehensively investigate the treatment effect of PRP combined with NPWT technology on chronic wounds, providing a reference for clinical treatment.
2 MATERIALS AND METHODS
2.1 Literature search
Keywords such as chronic wounds, chronic refractory wounds, platelet-rich plasma, autologous platelet-rich plasma, PRP, negative pressure wound therapy, NPWT, topical negative pressure therapy, negative pressure sealing drainage and vacuum sealing drainage were used in a combination of subject and free words to search for randomized controlled trials (RCTs) on the use of PRP combined with NPWT technology for treating chronic wounds in EMBASE, Google Scholar, Cochrane Library, PubMed, Wanfang and China National Knowledge Infrastructure databases, up to November 2023.
2.2 Inclusion and exclusion criteria
2.2.1 Inclusion criteria
(1) Participants: patients with chronic wounds; (2) intervention: control group treated with NPWT technology, experimental group treated with NPWT combined with PRP; (3) outcomes: healing rate, total effective rate and wound healing time; (4) study design: RCTs.
2.2.2 Exclusion criteria
Repeatedly published articles; literature lacking complete original data or full text; reviews, case reports, systematic reviews, conference papers and animal studies.
2.3 Data extraction and quality assessment
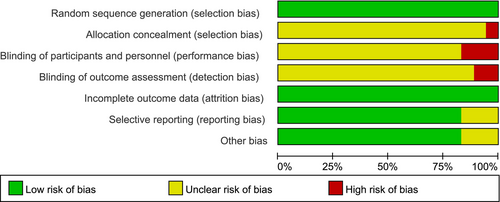
The retrieved literature was imported into Endnote X9, duplicates were removed, and two researchers independently read the titles, abstracts and full texts for screening based on inclusion and exclusion criteria, resolving discrepancies through discussion or with a third researcher. Data extraction was performed using Excel software, including the first author, year of publication, sample size, gender, age and outcome indicators (healing rate, effectiveness rate and wound healing time). The quality of RCTs was assessed using the bias risk tool recommended by the Cochrane Collaboration, focusing on selection bias, implementation bias, measurement bias, follow-up bias, reporting bias and other biases.
2.4 Statistical analysis
Stata 17.0 software was employed for data analysis. Dichotomous variables were expressed as odds ratios (OR) with 95% confidence intervals (CI), while continuous variables were expressed as standardized mean difference (SMD) with 95% CI. Heterogeneity was determined using the χ2 test and I2 values. A fixed-effect model was employed when I2 < 50% and p > 0.1; otherwise, a random-effects model was employed. Sensitivity analysis was conducted to evaluate the robustness of the study results. Publication bias was assessed using funnel plots when the number of included studies exceeded 10.
3 RESULTS
3.1 Basic characteristics
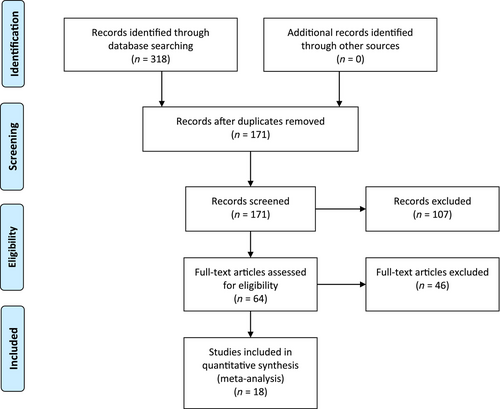
The literature screening process is shown in Figure 1. A total of 318 articles were initially identified, 147 duplicates were removed manually and using software, 107 articles not meeting the study criteria were excluded after reading titles and abstracts, and after full-text reading of the remaining 64 articles, 18 RCTs16-33 were finally included, involving 1294 patients with chronic wounds, with 646 and 648 patients in the experimental and control groups, respectively. The basic characteristics of the included literature are shown in Table 1. Literature quality assessment is shown in Figure 2.
| Author | Year | Number of patients | Age (years) | Sex (male/female) | |||
|---|---|---|---|---|---|---|---|
| Experimental group | Control group | Experimental group | Control group | Experimental group | Control group | ||
| Li | 2021 | 36 | 36 | 44.82 ± 2.30 | 44.78 ± 2.23 | 23/17 | 22/18 |
| Hui | 2020 | 30 | 30 | 62.2 ± 2.4 | 61.3 ± 2.5 | 16/14 | 17/13 |
| Cai | 2021 | 30 | 30 | 47.03 ± 6.72 | 46.17 ± 6.46 | 17/13 | 18/12 |
| Chen | 2018 | 28 | 30 | 49.54 ± 1.55 | 49.59 ± 1.54 | 13/15 | 12/18 |
| Ge | 2022 | 51 | 51 | 46.58 ± 10.30 | 46.51 ± 10.22 | 36/15 | 38/13 |
| He | 2022 | 38 | 38 | 54.39 ± 10.56 | 54.22 ± 10.76 | 16/22 | 14/24 |
| Peng | 2020 | 15 | 15 | 43.0 ± 6.1 | 42.1 ± 5.6 | 11/4 | 10/5 |
| Mei | 2023 | 35 | 35 | 71.36 ± 1.89 | 70.13 ± 1.58 | 19/16 | 17/18 |
| Ma | 2018a | 36 | 36 | 19–45 | 18–46 | 24/12 | 25/11 |
| Ma | 2018b | 42 | 42 | 54 ± 12 | 54 ± 12 | 29/13 | 28/14 |
| Qiu | 2021 | 32 | 32 | 48.82 ± 2.73 | 48.97 ± 2.75 | 16/16 | 18/14 |
| Zhang | 2017 | 43 | 44 | 64.0 ± 1.5 | 63.0 ± 2.1 | 29/14 | 30/14 |
| Yang | 2020 | 30 | 30 | 42.16 ± 2.12 | 42.35 ± 2.18 | 18/12 | 17/13 |
| Yang | 2022 | 39 | 39 | 58.74 ± 5.19 | 60.20 ± 4.83 | 27/12 | 21/18 |
| Xia | 2020 | 31 | 31 | 47.85 ± 6.47 | 48.26 ± 6.57 | 20/11 | 21/10 |
| Wang | 2023 | 58 | 57 | 68.27 ± 5.84 | 69.19 ± 5.36 | 30/28 | 30/27 |
| Song | 2023 | 40 | 40 | 46.25 ± 5.11 | 45.67 ± 4.51 | 22/18 | 24/16 |
| Zheng | 2022 | 32 | 32 | 52.26 ± 15.34 | 53.32 ± 15.37 | 17/15 | 18/14 |
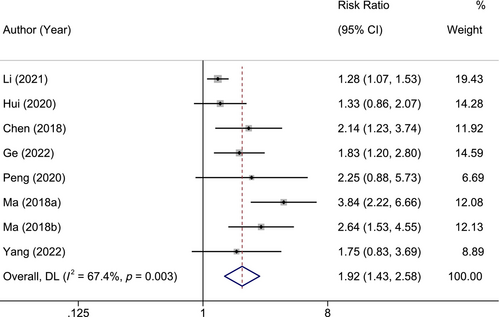
3.2 Healing rate
Eight RCTs reported the healing rate. In the experimental group, 197 out of 277 patients were healed; in the control group, 103 out of 279 patients were healed. There was significant heterogeneity (I2 = 67.4%, p = 0.003), and random-effects model was employed. It was found that in terms of the healing rate, the experimental group was significantly higher than the control group (OR = 1.92, 95% CI: 1.43–2.58, p < 0.001), as shown in Figure 3.
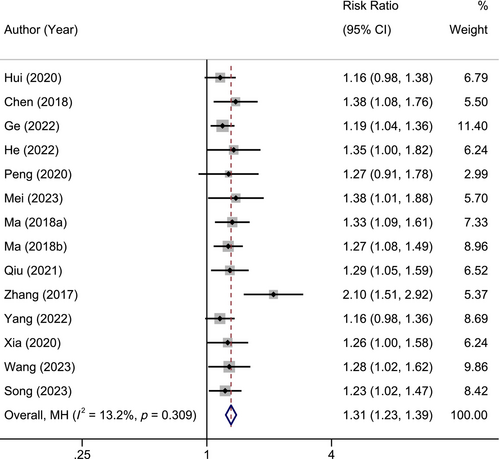
3.3 Total effective rate
Fourteen RCTs reported the total effective rate. In the experimental group, 481 out of 518 patients had effective treatment; in the control group, 369 out of 520 patients had effective treatment. There was no significant heterogeneity (I2 = 13.2%, p = 0.309), and fixed-effect model was employed. It was found that in terms of the total effective rate, the experimental group was significantly higher than the control group (OR = 1.31, 95% CI: 1.23–1.39, p < 0.001), as shown in Figure 4.
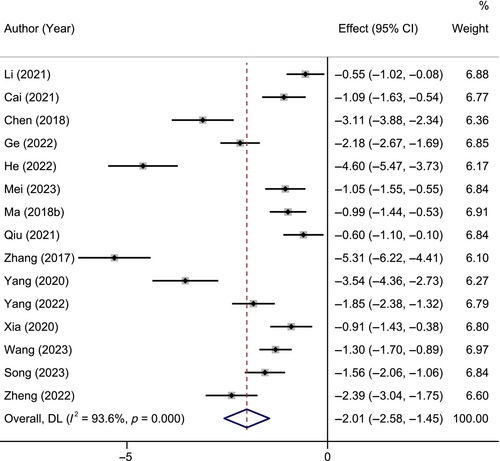
3.4 Wound healing time
Fifteen RCTs reported wound healing time. In the experimental group, 565 patients; in the control group, 567 patients. There was significant heterogeneity (I2 = 93.6%, p < 0.001), and random-effects model was employed. It was found that in terms of wound healing time, the experimental group was significantly shorter than the control group (SMD = −2.01, 95% CI: −2.58 to −1.45, p < 0.001), as shown in Figure 5.
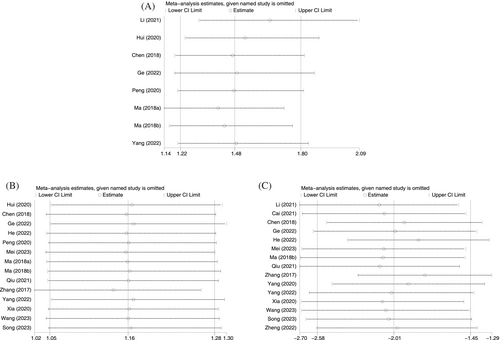
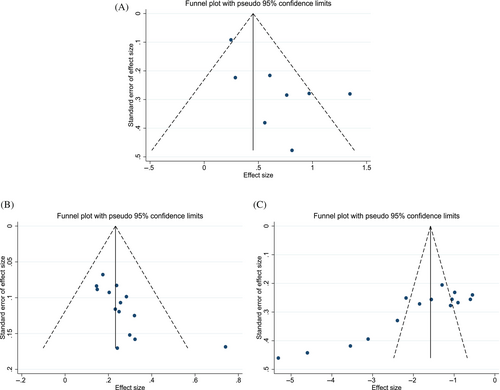
3.5 Sensitivity analysis and publication bias
Sensitivity analysis was conducted by sequentially excluding individual studies, and the results showed that the conclusions of this study were robust (Figure 6). The funnel plot, as shown in Figure 7, was mostly symmetrical for the healing rate, indicating a low likelihood of publication bias; however, the plots for total effective rate and wound healing time were asymmetric, suggesting the possibility of publication bias.
4 DISCUSSION
Normal wound healing is a dynamic and highly coordinated process that involves various cells, extracellular matrix and inflammatory mediators in phases of inflammation, proliferation and remodelling, promoting tissue repair.34 Disruption in the cellular microenvironment, lack of growth factors and disordered functioning of cells and cytokines can lead to delayed wound healing and the formation of chronic wounds.35 Patients with chronic wounds often undergo prolonged treatment, imposing a heavy burden on them and society.36 Currently, chronic wound treatment still primarily involves conventional dressing changes and surgical repair, with problems such as high dressing change rates and long treatment times.37 Therefore, there is an urgent need to improve traditional treatment methods to enhance efficacy, which is a focus and challenge for clinicians.
NPWT can replace conventional wound treatment methods, reducing the frequency of dressing changes while improving the self-healing rate of wounds.38 The negative pressure environment formed by NPWT can effectively remove fluid from tissue spaces, reduce oedema and collect bacteria adhering to the wound surface into a drainage bottle through negative pressure, allowing the wound to adhere closely and achieve therapeutic effects.39 Studies have confirmed the advantages of NPWT in reducing wound oedema, promoting granulation tissue formation, increasing blood flow to the wound and triggering wound healing.40 PRP is a plasma concentrate obtained after centrifuging whole blood, rich in growth factors, which can promote cell proliferation, regulate inflammatory responses and promote angiogenesis, thus facilitating wound repair.41, 42 PRP, due to its simple preparation, high growth factor content and low immunogenicity, is widely used in various surgical operations and clinical treatments, showing good experimental and clinical results in wound healing, especially in chronic wound healing.43, 44 Although both NPWT and PRP can promote chronic wound healing, single therapy is often insufficient. Studies have suggested that combining the two can effectively improve the treatment effect of chronic wounds.45 Based on this, our study aimed to investigate the treatment effect of PRP combined with NPWT technology on chronic wounds via meta-analysis.
In this meta-analysis, the results showed that the treatment of chronic wounds with PRP combined with NPWT significantly shortened wound healing time and increased healing rates, effectively improving the clinical efficacy of chronic wound treatment. The superior efficacy of PRP combined with NPWT compared with NPWT alone might be attributed to several factors: PRP can release various growth factors, addressing the deficiency of vital growth factors in chronic wounds, thereby promoting vascular regeneration and blood circulation;46 concurrently, NPWT can prevent the invasion of pathogens from outside the wound, promote the growth of vascular granulation tissue, improve local blood circulation and provide the required nutrition for wound healing, thus accelerating wound healing.47, 48 Therefore, the combined use of these two can accelerate the healing process of chronic wounds and improve their clinical efficacy.
However, this study still has some limitations: firstly, due to the lack of standardized PRP preparation methods, the PRP obtained through different methods may vary, and its potential impact cannot be excluded; secondly, the included literature is only in Chinese, lacking high-quality articles published in other languages, which may lead to language bias; thirdly, the sample size of the included literature is generally small, and further research with larger sample sizes is needed for validation.
5 CONCLUSIONS
In conclusion, the application of PRP combined with NPWT in patients with chronic wounds is significantly effective, can promote wound healing, shorten wound healing time and increase healing rates, and has substantial practical value in clinical practice.
FUNDING INFORMATION
This work was supported by Natural Science Foundation of China (no. 81270358), and the Scientific Research Project of Southwest Medical University (no. 2023QN084).
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




