RETRACTED: Knee and hip arthroplasty joint surgical site wound infection in end-stage renal disease subjects who underwent dialysis or a kidney transplant: A meta-analysis
Abstract
A meta-analysis study to assess the knee and hip arthroplasty joint surgical site wound infection (SSWI) in end-stage renal disease (ESRD) subjects who underwent dialysis or a kidney transplant (KT). A comprehensive literature examination till February 2023 was implemented and 1046 linked studies were appraised. The picked studies contained 5 471 898 subjects with total joint arthroplasty (TJA) at the baseline, 13 049 of them were haemodialysis or renal transplant, and 5 458 849 were control. Odds ratio (OR) in addition to 95% confidence intervals (CIs) were used to calculate the consequence of knee and hip arthroplasty SSWI in ESRD subjects who underwent dialysis or a KT by the dichotomous and continuous styles and a fixed or random model. Haemodialysis or renal transplant had a significantly higher postoperative SSWI (OR, 2.13; 95% CI, 1.73–2.62, P < .001) compared with control in TJA subjects. However, no significant difference was observed between haemodialysis and renal transplant in postoperative SSWI (OR, 0.93; 95% CI, 0.16–5.54, P = .94) and between haemodialysis or renal transplant and control in prosthetic joint infection (OR, 1.07; 95% CI, 0.25–4.55, P = .93) in TJA subjects. Haemodialysis had a significantly higher prosthetic joint infection (OR, 1.92; 95% CI, 1.21–3.03, P = .005) compared with renal transplant in TJA subjects. Haemodialysis or renal transplant had a significantly higher postoperative SSWI in TJA subjects. Also, haemodialysis had a significantly higher prosthetic joint infection compared with renal transplant in TJA subjects. Although precautions should be taken when commerce with the consequences because a low number of selected studies was picked for certain comparisons in this meta-analysis.
1 INTRODUCTION
End-stage renal disease (ESRD) is still a significant global health issue.1 Presently, there are two treatments for ESRD: dialysis and kidney transplant (KT). End-stage renal illness subjects are more likely to need arthroplasty surgery because of a number of risk factors, including morbid obesity, alcoholism, and poorly managed diabetes.2, 3 These subjects' mortality and morbidity rates after arthroplasty procedures have also been demonstrated to be greater.4 Complex comorbidities, renal osteodystrophy, which causes an increase in bone turnover, and beta 2-microglobulin deposition surrounding the prosthesis are among the factors contributing to the higher risk.5 Subjects receiving dialysis may be at an increased risk for the hematogenous spread of germs, which can eventually result in infections of prosthetic joints. There is an elevated risk of infection and implant loosening in people who have undergone kidney transplantation. The relative immunocompromised state of KT recipients explains this elevated risk.4 Yet, orthopaedic physicians are also quite concerned about postoperative problems. Many publications evaluating the results of total joint arthroplasty (TJA) in dialysis and KT are now available in the literature. Unfortunately, the majority of the research either used a small sample size. The majority of the studies do not accurately reflect current practice because of recent improvements in the medical care of dialysis subjects. Popat et al. conducted a meta-analysis, but this study only included individuals who had complete hip arthroplasty.6 So, this meta-analysis aimed to evaluate the knee and hip arthroplasty SSWI in ESRD subjects who underwent dialysis or a KT.
2 METHODS
2.1 Eligibility criteria
The studies showing the knee and hip arthroplasty SSWI in ESRD subjects who underwent dialysis or a KT were chosen to construct a summary.7
2.2 Information sources
- The study was observational, randomised controlled trial (RCT), prospective, or retrospective study.
- Subjects with ESRD and TJA subjects were the nominated subjects.
- The intervention encompassed haemodialysis or renal transplant.
- The study differentiated the outcome of knee and hip arthroplasty SSWI in ESRD subjects who underwent dialysis or a KT.
The studies that were excluded were those where the significance of the comparison was not emphasised in it, studies that did not inspect the properties of knee and hip arthroplasty SSWI in ESRD subjects who underwent dialysis or a KT, and research on TJA subjects' post-surgery wounds without ESRD.
2.3 Search strategy
A search protocol methodologies were established based on the PICOS perception, and we characterised it as next: topics for ESRD and TJA subjects, P; haemodialysis or renal transplant is the ‘intervention’ or ‘exposure’, while the ‘comparison’ was haemodialysis or renal transplant compared with control or haemodialysis compared with renal transplant; different type of wound infection and prosthetic joint infection (PJA) was the “outcome” and lastly, there were no boundaries on the study's proposal.8
We have carried out a full search of Google Scholar, Embase, Cochrane Library, PubMed, and OVID databases till February 2023 using an organisation of keywords and linked terms for prosthetic joint infection; wound infection; total joint arthroplasty; and end-stage renal disease as shown in Table 1. To evade studies that did not show a joining between the outcomes of the knee and hip arthroplasty SSWI in ESRD subjects who underwent dialysis or a KT, papers were united into one EndNote file, replications were omitted, and the titles and abstracts were checked over and revised.
| Database | Search strategy |
|---|---|
| Pubmed | #1 “end-stage renal disease”[MeSH Terms] OR “wound infection”[All Fields] [All Fields] #2 “total joint arthroplasty”[MeSH Terms] OR “prosthetic joint infection”[MeSH Terms] [All Fields] #3 #1 AND #2 |
| Embase | ‘end-stage renal disease’/exp OR ‘wound infection’ #2 ‘total joint arthroplasty’/exp OR ‘prosthetic joint infection’ #3 #1 AND #2 |
| Cochrane library | (end-stage renal disease):ti,ab,kw (wound infection):ti,ab,kw (Word variations have been searched) #2 (total joint arthroplasty):ti,ab,kw OR (prosthetic joint infection): ti,ab,kw (Word variations have been searched) #3 #1 AND #2 |
2.4 Selection process
Following the epidemiological statement, a method was created, which was then organised and analysed in the arrangement of a meta-analysis.
2.5 Data collection process
The primary author's name, study date, year of study, nation or province, populace type, medical and management physiognomies, categories, the qualitative and quantitative valuation technique, the data source, the result assessment, and statistical analysis were among the criteria used to gather data.9
2.6 Data items
We independently gathered the information if there were variable consequences from a study according to the appraisal of the knee and hip arthroplasty SSWI in ESRD subjects who underwent dialysis or a KT.
2.7 Study risk of bias assessment
To define whether there was a chance that each study might have been biased, two authors independently assessed the chosen papers' methodologies. The ‘risk of bias tool’ from the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 was used to weigh the methodological quality. Each study was denoted one risk of bias of those listed below after being classified according to the appraisal criteria: low: If the entire quality necessities were encountered, a study was considered as having a low bias risk; if one or more necessities were not encountered or were not included, a study was classified as having a medium bias risk. In the occasion that one or more quality necessities were not encountered at all or were only partially encountered, the study was considered as having a high bias risk.
2.8 Effect measures
Sensitivity studies were only performed on studies that evaluated and reported the knee and hip arthroplasty SSWI in ESRD subjects who underwent dialysis or a KT. To compare the effects of haemodialysis or renal transplant compared with control or haemodialysis compared with renal transplant on wound infection in TJA subjects' sensitivity, a subclass analysis was used.
2.9 Synthesis methods
The odds ratio (OR) in addition to a 95% confidence interval (CI) was calculated using a random- or fixed-effect model using dichotomous or continuous methods. The I2 index, between 0% and 100%, was calculated. Heterogeneity was absent, low, moderate, and high for the values at 0%, 25%, 50%, and 75%, respectively.10 To ensure that the right model was being used, additional traits that exhibit a high degree of resemblance among the involved research were also examined. If I2 was 50% or higher, the random effect was taken into consideration; if I2 was <50%, the prospect of using fixed-effect increased.10 By stratifying the first evaluation according to the earlier-mentioned results categories, a subclass analysis was finished. The analysis used a P-value of <.05 to denote statistical significance for differences amid subcategories.
2.10 Reporting bias assessment
Using the Egger regression test and funnel plots that show the ORs' logarithm versus their standard errors, studies bias was evaluated both qualitatively and quantitatively (studies bias was judged present if P ≥ .05).11
2.11 Certainty assessment
All of the P-values were examined using two-tailed testing. Using Reviewer Manager Version 5.3, the graphs and statistical analyses were produced (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
3 RESULTS
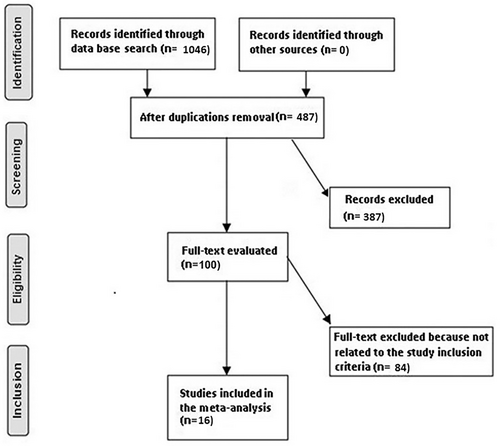
From a total of 1046 linked investigation that was inspected, 16 articles published between 2010 and 2023 fit the inclusion criteria and were selected and involved in the study.2, 4, 5, 12-24 Table 2 offers the verdicts from these studies. The 5 471 898 subjects with TJA were in the picked studies' baseline; 13 049 of them were haemodialysis or renal transplant, and 5 458 849 were controls. The sample size ranged between 107 and 4 182 887 subjects.
| Study | Country | Total | Haemodialysis or renal transplant | No haemodialysis or renal transplant |
|---|---|---|---|---|
| McCleery12 | UK | 55 732 | 162 | 55 570 |
| Lim13 | Korea | 141 | 45 | 96 |
| Ponnusamy14 | USA | 4 182 887 | 1683 | 4 181 204 |
| Erkocak15 | USA | 1077 | 359 | 718 |
| Ottesen16 | USA | 163 810 | 250 | 163 560 |
| Patterson17 | USA | 214 005 | 339 | 213 666 |
| Browne4 | USA | 4412 | 1103 | 3309 |
| Inoue2 | Japan | 107 | 107 | 0 |
| Labaran5 | USA | 36 734 | 1779 | 34 955 |
| Malkani18 | USA | 55 297 | 395 | 54 902 |
| Kii19 | Japan | 587 | 18 | 569 |
| Kothandaraman20 | USA | 398 | 134 | 264 |
| Douglas21 | USA | 1164 | 1164 | 0 |
| Stavrakis22 | USA | 4179 | 4179 | 0 |
| Khanna23 | USA | 367 890 | 383 | 367 507 |
| Harris24 | Australia | 383 478 | 949 | 382 529 |
| Total | 5 471 898 | 13 049 | 5 458 849 |
Haemodialysis or renal transplant had a significantly higher postoperative SSWI (OR, 2.13; 95% CI, 1.73–2.62, P < .001) with low heterogeneity (I2 = 26%) compared with control in TJA subjects as shown in Figure 2.
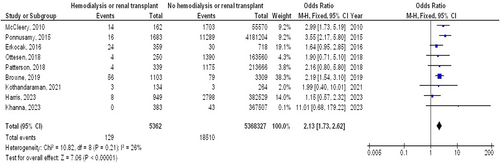
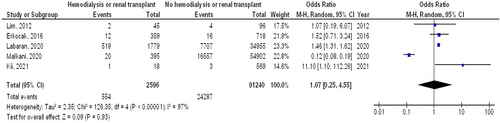
However, no significant difference was observed between haemodialysis and renal transplant in postoperative SSWI (OR, 0.93; 95% CI, 0.16–5.54, P = 0.94) with moderate heterogeneity (I2 = 66%) and between haemodialysis or renal transplant and control in PJI (OR, 1.07; 95% CI, 0.25–4.55, P = .93) with high heterogeneity (I2 = 97%), in TJA subjects as shown in Figures 3, 4.
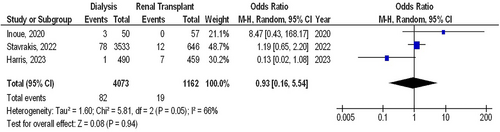
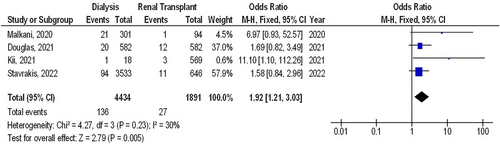
Haemodialysis had a significantly higher PJI (OR, 1.92; 95% CI, 1.21–3.03, P = .005) with low heterogeneity (I2 = 30%) compared with renal transplant in TJA subjects as shown in Figure 5.
Becuase of paucity of data, stratified models could not be used to investigate the impact of specific variables, for example, gender, ethnicity, and age on comparison results. Visual interpretation of the funnel plot and quantitative evaluations by the Egger regression test exposed no indication of study bias (P = .87). However, it was shown that the mainstream of the involved RCTs had poor methodological quality and no bias in selective reporting.
4 DISCUSSION
In the studies nominated for the meta-analysis, 5 471 898 subjects with TJA were in the picked studies' baseline, 13 049 of them were haemodialysis or renal transplant, and 5 458 849 were control.2, 4, 5, 12-24 Haemodialysis or renal transplant had a significantly higher postoperative surgical site wound infection (SSWI) however no significant difference was found in PJI compared with control in TJA subjects. Haemodialysis had a significantly higher PJI, however, no significant difference was observed in postoperative SSWI compared with renal transplant in TJA subjects. Although precautions should be taken when commerce with the consequences because a low number of selected studies was picked for certain comparisons in this meta-analysis, for example, comparison between dialysis and renal transplant that would affect the P-value and the level of confidence of the comparison.
Patients with ESRD are susceptible to problems with wound healing.25 There are several reasons why the incidence is higher in certain subjects. For instance, platelet dysfunction and long-term anticoagulant use put ESRD patients at risk for bleeding.26 A thorough investigation by Ponnusamy et al. found that dialysis patients had an increased risk of wound hematoma, seroma, and infection.14 Wound healing still presents a significant problem for doctors despite recent improvements in postoperative care for KT patients.27 The processes that influence wound healing in KT patients have been examined in a variety of research. First, a variety of long-term immunosuppressants, such as steroids, sirolimus, and everolimus, have anti-proliferative effects that negatively affect the wound healing process.27 Moreover, these people are more likely to have wound problems because of greater infection rates and post-transplant blood abnormalities (such as platelet malfunction, acute myeloid leukaemia, etc.).28 There are currently very few reports on this subject population that address the management of wound complications following TJA. In their analysis of the risk factors for surgical wound complications following KT,27 the authors specifically advised the insertion of a drain and the application of subcutaneous sutures to stop ongoing wound leakage.27 Future research should concentrate on this cohort's postoperative wound problems after orthopaedic operations like TJA. After TJA, PJI is one of the most severe side effects. Infection rates following TJA are 2% or less in the general population.29 Orthopaedic surgeons must determine all controllable hazards in this population because infection is the second greatest cause of death in people receiving dialysis or who received a KT.30 Dialysis patients are more vulnerable to infections for a variety of reasons. Those receiving haemodialysis had a 25–50-fold higher chance of developing bacteremia, with Gram-positive bacteria accounting for the majority of infections.31 Because dialysis requires ongoing intravenous access via a central catheter or a dialysis shunt, numerous studies have linked this greater prevalence to catheter-related infections.30 Furthermore, dialysis patients have a much greater risk of methicillin-resistant Staphylococcus aureus (MRSA) infections.30 MRSA is a well-documented pathogen for PJIs and is infamous for having significantly higher management failure rates.32 The mixture of immunodeficient status, and tendency for MRSA infection have caused a number of specialists to advice against arthroplasty surgery for dialysis subjects.14 To evade these catastrophic actions, all adjustable risks, for example, making a permanent arteriovenous fistula before surgery, empirical antibiotics with vancomycin or waiting for KT were suggested by authors.30 Remarkably, Browne et al measured the consequence after TJA for subjects on peritoneal dialysis (PD) and determined that PD subjects did not convey the same risk for bacteremia and that PD was related to less systemic inflammation.4 PJIs rate was somewhat higher in dialysis subjects (dialysis versus KT). Present literature also supports this tendency, but there could be possible bias in these consequences. First, the baseline subject status for haemodialysis subjects is often complicated with multiple comorbidities, making these subjects less suitable for transplant surgery.2 Their complex subject status could possibly influence the consequence of dialysis subjects after TJA. Future studies must comprise matched cohorts to eliminate possible confusing features and to better outline the alterations between these two cohorts.
This meta-analysis verified the outcome of the knee and hip arthroplasty SSWI in ESRD subjects who underwent dialysis or a KT. More examination is still desirable to elucidate these probable connections.33-42 Bigger, more homogeneous samples are mandatory for this examination. This was also emphasised in preceding studies that used a linked meta-analysis technique and found equivalent consequences of the influence.6, 43, 44 Well-led RCTs are necessary to weigh these features as well as the blend of diverse ethnicities, ages, gender, and other parameters of subjects because the meta-analysis could not define whether differences in them are linked to the outcomes studied. In conclusion, haemodialysis or renal transplant had a significantly higher postoperative SSWI however no significant difference was found in PJI compared with control in TJA subjects. Haemodialysis had a significantly higher PJI, however, no significant difference was observed in postoperative SSWI compared with renal transplant in TJA subjects.
5 LIMITATIONS
There may have been selection bias because a number of the studies involved in the meta-analysis were not covered. However, the excluded publications did not meet the criteria for enclosure in the meta-analysis. Also, we were incompetent to ascertain whether variables like ethnicity, age, and gender influenced results. The purpose of the study was to measure the knee and hip arthroplasty SSWI in ESRD subjects who underwent dialysis or a KT. Because of the inclusion of missing or erroneous data from prior studies, bias may have been increased. The individuals' nutritional states as well as their age and gender characteristics were potential sources of bias. Undesirably, some unpublished work and insufficient data can skew the consequence under investigation.
6 CONCLUSIONS
Haemodialysis or renal transplant had a significantly higher postoperative SSWI however no significant difference was found in PJI compared with control in TJA subjects. Haemodialysis had a significantly higher PJI, however, no significant difference was observed in postoperative SSWI compared with renal transplant in TJA subjects. Although precautions should be taken when commerce with the consequences because a low number of selected studies was picked for certain comparisons in this meta-analysis, for example, comparison between dialysis and renal transplant that would affect the P-value of the comparison.
Open Research
DATA AVAILABILITY STATEMENT
On request, the corresponding author is required to provide access to the meta-analysis database.