Pharmaceutical preparations of Periplaneta americana (KangFuXin liquid) in the treatment of pressure ulcer: A meta-analysis
Abstract
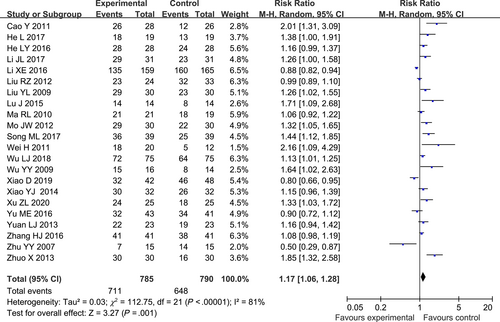
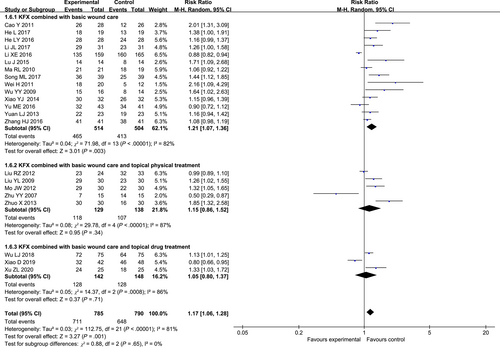
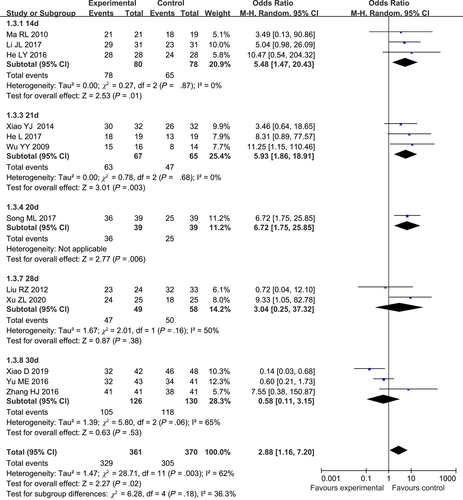
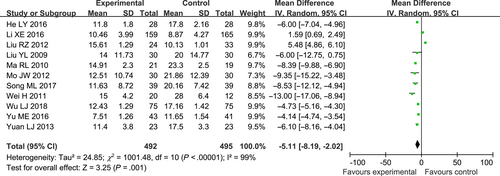
Pressure ulcers often become chronic wounds that are difficult to treat and that tend to recur after healing. In China, convincing data from randomised trials have demonstrated that the pharmaceutical preparations of Periplaneta americana (KangFuXin Liquid, KFX) have a significant efficacy for pressure ulcers. To provide more reference to the clinicians and experts, we conducted a meta-analysis based on the existing randomised controlled trials (RCTs). We searched the RCTs about KFX for the treatment of pressure ulcers published up to July 2022 in major English and Chinese databases with no language restriction, including PubMed, EMBASE, Web of Science (WOS), Cochrane Central Register of Controlled Trials (CENTRAL), China Network Knowledge Infrastructure (CNKI), Chinese Biomedicine (CBM), Chinese Scientific Journals Database (VIP), and WanFang database. Cochrane Handbook guidelines were used to assess the risk of bias and to evaluate the methodological quality of included RCTs. Estimates of the intervention's effects are expressed as the risk ratio (RR) (95% CI) for binary outcomes and mean difference or standardised mean difference (95% CI) for continuous outcomes. We applied fixed or random effects models, and all analyses were performed using Review Manager version 5.4 and Stata/SE version 12.0. We included 22 studies with a total of 1575 participants. Compared with controls, KFX combined with basic wound care or KFX combined with basic wound care and another topical drug or physical treatment significantly increase clinical efficacy (RR: 1.17; 95% CI, 1.06-1.28; P = 0.001; I2 = 81%) and shorten the complete healing time (MD = −5.11; 95% CI [−8.19, −2.02]; P = 0.001) for pressure ulcers. Subgroup analysis showed a significant difference in the total clinical effect rate between KFX combined with basic wound care and controls. (n = 1018, RR 1.21, 95% CI [1.07, 1.36], I2 = 82%, P = 0.003). No difference was found in the total clinical effective rate between patients using KFX combined with basic wound care and another topical drug or physical treatment with controls (KFX combined with basic wound care and topical physical treatment: n = 267, RR 1.15, 95% CI [0.86, 1.52], I2 = 87%, P = 0.34; KFX combined with basic wound care and topical drug: n = 290, RR 1.05, 95% CI [0.80, 1.37], I2 = 86%, P = 0.71). Based on treatment duration, subgroup analysis indicated that increasing treatment duration increased the total clinical effective rate when treatment duration was not long. (treatment duration: 14 days: n = 158, OR 5.48, 95% CI [1.47, 20.43], I2 = 0%, P = 0.01; 21 days: n = 132, OR 5.93, 95% CI [1.86, 18.91], I2 = 65%, P = 0.003). When treatment duration was 28 days or 30 days, the results showed that there was no significant difference in total clinical effective rate between interventions and controls (treatment duration: 28 days: n = 107, OR 3.04, 95% CI [0.25, 37.32], I2 = 50%, P = 0.38; 30 days: n = 256, OR 0.58, 95% CI [0.11, 3.15], I2 = 65%, P = 0.53). No data on side effects were reported in any of the 22 studies. The conclusion is that the combination of KFX and basic wound care is effective in increasing the total clinical effectiveness and shortening the complete healing time of pressure ulcers.
1 INTRODUCTION
Pressure ulcer refers to the localised damage to the skin and/or underlying tissues including epithelial, dermal, and subcutaneous tissues, such as fat or muscle.Wounds from pressure ulcers are usually the results of pressure or pressure in combination with shear forces.1 Pressure ulcers often become chronic wounds that are difficult to manage. They are associated with substantial morbidity and mortality, and tend to recur. Because of the high costs of wound care, long healing time, high recurrence rate, and hospitalisation rate, pressure ulcers affect millions of individuals annually,2, 3 which entails significant health risks and financial burdens.4
To date, the standard of initial care for pressure ulcers, based on clinical presentation and classification, includes prevention strategies (repositioning and support surfaces), pressure off-loading, cleansing and debridement, dressings that promote a moist wound healing environment, antibiotics for infection control, and so on.4, 5 However, when these ulcers fail to heal with conventional approaches, it may be beneficial to consider more advanced adjuvant therapeutic options such as negative pressure wound therapy, platelet-derived growth factors, platelet-rich plasma, cellular and acellular matrices, hyperbaric oxygen, and some physical therapy such as a laser, etc.6, 7 However, there are still high costs, complicated operations, and other factors that prevent wound healing.
Despite the growing awareness of this serious and widespread public health problem, the pressure ulcer field continues to be plagued by a lack of well-designed randomised clinical trials (RCTs).6, 8 The tremendous difficulties in initiating appropriate research in the field of pressure ulcers, such as wound debridement and decompression, are often subjective and difficult to standardise and play an undeniable role in study failure.9 Therefore, there is an urgent need to find high-quality evidence that can enable improved treatment standardisation in this area.
KFX is an ethanol extract from the dried body of Periplaneta americana, including many active components such as polyhydric alcohols, anti-bacterium peptides, and mucin,10 which have the bioactive function of inhibiting inflammation, stimulating collagen production in human skin fibroblasts, facilitating epidermal cell growth, and the proliferation of granulation tissue to repair damage and thus accelerate wound healing.11 KFX with wound repair effect has been used in clinical practice in China for more than 20 years since its successful development. A large body of clinical research data, including RCTs, has been collected on the treatment of skin ulcers.
Unfortunately, to date, there has not been a full systematic evaluation of the efficacy of KFX in treating pressure ulcers. The purpose of this systematic review and meta-analysis of published RCTs was to evaluate the clinical efficacy of KFX in the treatment of pressure ulcers, to quantitatively compare the advantages and disadvantages of KFX and other basic treatments in the treatment of pressure ulcers, and to provide high-quality evidence for the formulation of treatment strategies for pressure ulcers.
2 MATERIALS AND METHODS
We conducted a systematic review and meta-analysis of RCTs for KFX in the treatment of pressure ulcers. The protocol for this systematic review was registered on INPLASY and is available in full on inplasy.com (https://doi.org/10.37766/inplasy2022.7.0082).
2.1 Data source and search strategy
Luo N and Bo Y searched the literature published up to July 2022 in major English and Chinese databases with no language restriction, including PubMed, EMBASE, Web of Science (WOS), Cochrane Central Register of Controlled Trials (CENTRAL), China Network Knowledge Infrastructure (CNKI), Chinese Biomedicine (CBM), Chinese Scientific Journals Database (VIP), and WanFang database. Luo N and Bo Y independently read the abstracts and titles, and finally cross-checked the included RCTs. Then, they screened the full text of these RCTs according to the inclusion criteria. Conflicts between the two reviewers were resolved by a third senior investigator.
2.2 Study selection and data extraction
Eligible study: (a) This study is a randomised controlled trial; (b) participants had localised pressure ulcers without topical medication before treatment, excluding skin ulcers caused by tumours; (c) the study evaluated an intervention group and a control group, including topical KFX combined with basic wound care or KFX in combination with basic wound care and other topical drug treatment or physical treatment in the intervention group and non-KFX in the control group; (d) specific steps for topical KFX: the medical gauze was soaked with KFX and applied externally to the affected area, and the outer layer was wrapped with sterile gauze. If there is any hole, fill it with a piece of gauze soaked with KFX, leaving no gap. The frequency of changing the gauze was once a day at least. The covering time was until the next change of gauze. (e) The baseline status before treatment was clear, and the baseline difference was not statistically significant.
The main outcome was the total clinical effective rate: complete healing rate plus remarkable effective rate and improvement rate, which was judged by the area of the ulcers, the amount of exudation, and the colour and growth of the granulation tissue before and after the treatment. The secondary outcome was the complete healing time of the ulcer. The complete healing time refers to the time when the ulcers are completely healed, the skin surface is covered with the epidermis, and the scab is peeled off.
Two reviewers (Luo N and Bo Y) independently extracted the study details, and two other reviewers (Zhong LY and Wang JL) assessed the risk of bias in the included RCTs using the revised version of the Cochrane risk of bias tool for randomised trials (RoB2).12 The conflicts of the assessment were resolved through negotiations.
2.3 Data analysis
We used Review Manager version 5.4 and Stata/SE version 12.0 for the statistical analysis. Estimates of the intervention's effects are expressed as the risk ratio (RR) (95% CI) for binary outcomes and mean difference or standardised mean difference (95% CI) for continuous outcomes. And because of the heterogeneity, which was tested by I2 statistics, we used the fixed effect model when I2 < 50% or the random effect model when I2 exceeded 50%. For heterogeneity, we conducted a sensitivity analysis to evaluate the robustness of our findings by excluding the specific study. Moreover, meta-regression and subgroup analysis were performed to explore the heterogeneity between the studies. Publication bias was evaluated using funnel plots, Egger's regression test, and trim-and-fill estimations.
3 RESULTS
3.1 Search results
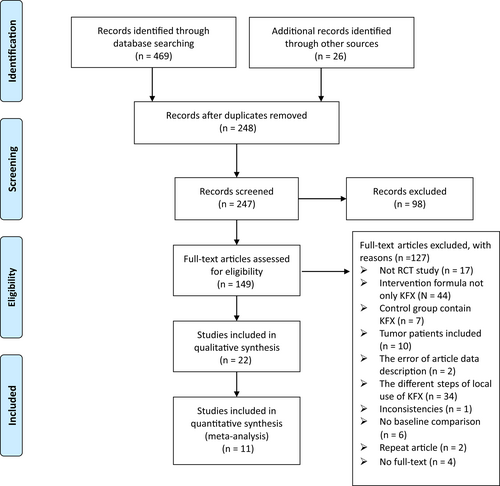
The initial search identified 495 citations, of which 248 were excluded because of duplication. After screening the titles and abstracts, 98 studies were excluded according to the inclusion criteria, while 127 studies were excluded after reading the full texts. Finally, we included 22 RCTs with a total of 1575 patients for data extraction and meta-analysis. Figure 1 shows the search process.
Source: Reference13.
3.2 Study characteristics and risk of bias in included studies
Among all included 22 studies with a total of 1575 participants, the publication dates range from 2007 to 2020. The baseline characteristics between the two groups were well comparable in each included RCT. KFX used in each study was from several different manufacturers, but all are ethanol extracts from the dried body of P americana. Fourteen trials use KFX combined with basic wound care (cleansing and debridement) in the intervention group,14-27 while other eight trials combined another topical drug or physical treatment with the above methods in the intervention group.28-35 The specific procedure for using the KFX involves covering the wound with gauze soaked in KFX and then wrapping the outer layers with sterile gauze. The treatment duration was the complete healing time of the wounds,17, 18, 29, 31, 33 7 days,16 14 days,15, 21, 26 15 days,22 20 days,27 21 days,14, 19, 25 28 days,30, 35 30 days,23, 24, 34 and 45 days,28 not mentioned in two studies.20, 32 The frequency of gauze changes with KFX was once daily,16, 21, 23, 25, 28-30, 33, 34 twice daily,15, 17, 19, 22, 26, 27, 31, 32 thirds per day,14, 18, 20 once every other day,35 and once every 4 to 5 days.24 Eleven RCTs reported complete healing time.15, 17, 18, 21-23, 27, 29-31, 33 None of the included studies described the AEs and the given duration. The characteristics of the included studies are presented in Table 1. Basic wound care was used in both the intervention group and the control group.
| First author, publication year, country | Disease | Intervention (route of administration, frequency, dosage) | Control (route of administration frequency, dosage) | Duration of treatment (days) | Main outcomes | Sample | Age (range or mean [SD]), years; gender (M/F) | ADs | Manufacturer |
|---|---|---|---|---|---|---|---|---|---|
| Zhu YY 2007, China | PU | KFX (topical, qd) and EWTLI (topical, qd) | CMP (topical, qod) and EWTLI (topical, qod) | 45 | Total effective rate | E: 15 C: 15 |
65-95; 72.9; NA | NA | IMDP |
| Liu YL 2009, China | PU | KFX (topical, qd) and TDP (topical, qd) | TDP (topical, qd) | NA | Total effective rate Compete healing time |
E: 30 C: 30 |
E: 73.4 (10.2); 18/12 C: 71.1 (11.3); 20/10 |
NA | Good doctor |
| Wu YY 2009, China | PU | KFX (topical, tid) | Gentamicin (topical, NA) | 21 | Total effective rate | E: 16 C: 14 |
50-88; 68; 21/9 | NA | NA |
| Ma RL 2010, China | PU | KFX (topical, bid) | Gentamicin (topical, bid) | 14 | Total effective rate Compete healing time |
E: 21 C: 19 |
78-96; NA; 38/2 | NA | NA |
| Cao Y 2011, China | PU | KFX (topical, qd) | Routine disinfection (topical, bid) | 7 | Total effective rate | E: 28 C: 26 |
37-85; 60; 30/24 | NA | Good doctor |
| Wei H 2011, China | PU | KFX (topical, bid) | Gentamicin (topical, bid) | NA | Total effective rate Compete healing time |
E: 20 C: 12 |
18-69; NA; 22/10 | NA | NA |
| Liu RZ 2012, China | PU | KFX (topical, qd) and IR (topical, qd) | IR (topical, qd) and YNB (topical, qd) | 28 | Total effective rate Compete healing time |
E: 20 C: 23 |
NA; 66.7 (6.5); 22/21 | NA | NA |
| Mo JW 2012, China | PU | KFX (topical, bid) and TDP (topical, bid) | TDP (topical, bid) | NA | Total effective rate Compete healing time |
E: 30 C: 30 |
NA; 72.1 (10.8); 32/28 | NA | Good doctor |
| Yuan LJ 2013, China | PU | KFX (topical, tid) | Gentamicin (topical, qd) | NA | Total effective rate Compete healing time |
E: 23 C: 23 |
E: 46-83; 67.6; 13/10 C: 48-80; 64.5; 15/8 |
NA | NA |
| Zhuo X 2013, China | PU | KFX (topical, bid) and IR (topical, qd) | IR (topical, qd) | NA | Total effective rate | E: 30 C: 30 |
65-93; NA; 26/34 | NA | NA |
| Xiao YJ 2014, China | PU | KFX (topical, bid) | Routine dressing change (topical, bid) | 21 | Total effective rate | E: 32 C: 32 |
52-86; 75; 35/29 | NA | NA |
| Lu J 2015, China | PU | KFX (topical, tid) | Gentamicin (topical, qd) | NA | Total effective rate |
E: 14 C: 14 |
45-89; 68.1 (6.7); 18/10 | NA | NA |
| He LY 2016, China | PU | KFX (topical, qd) | Gentamicin (topical, NA) | 14 | Total effective rate Compete healing time |
E: 28 C: 28 |
60-90; 70.5; 32/24 | NA | NA |
| Li XE 2016, China | PU | KFX (topical, bid) | LOEA (topical, bid) | 15 | Total effective rate Compete healing time |
E: 138 C: 145 |
E: NA; 68.98 (18.37); 78/60 C: NA; 73.08 (16.22); 73/72 |
NA | HZKPCL |
| Yu ME 2016, China | PU | KFX (topical, bid) | FHEA (topical, qod) | 30 | Total effective rate Compete healing time |
E: 43 C: 41 |
NA; NA; NA | NA | NA |
| Zhang HJ 2016, China | PU | KFX (topical, 4 to 5 times every day) | GSWS (topical, 4-5 times every day) | 30 | Total effective rate | E: 41 C: 41 |
E: 30-82; 67; 25/16 C: 31-81; 66; 23/18 |
NA | IMJXPCL |
| He L 2017, China | PU | KFX (topical, qd) | Routine dressing change (topical, qd) | 21 | Total effective rate | E: 19 C: 19 |
36-78; NA; 30/8 | NA | Good doctor |
| Li JL 2017, China | PU | KFX (topical, bid) | Routine dressing change (topical, bid) | 14 | Total effective rate |
E: 31 C: 31 |
72-93; 82.2 (1.3); 45/17 | NA | NA |
| Song ML 2017, China | PU | KFX (topical, bid) | Routine disinfection (4 times a day) | 20 | Total effective rate Compete healing time Serum IL-6 levels Serum CRP levels |
E: 39 C: 39 |
E: 39-76; 55.6 (3.6); 26/13 C: 40-75; 56.1 (3.5); 24/15 |
NA | Good doctor |
| Wu LJ 2018, China | PU | KFX (topical, qd) and Li Fuping (topical, qd) | Li Fuping (topical, qd) | NA | Total effective rate Compete healing time VAS score |
E: 75 C: 75 |
E: 45-68; 56.71 (2.39); 44/31 C: 44-68; 56.14 (3.02); 45/30 |
NA | NA |
| Xiao D 2019, China | PU | KFX (topical, qd) and metronidazole (topical, qd) and CMFEU (topical, qd) | LOEA (topical, qd) | 30 | Total effective rate VRS score PSQI score |
E: 42 C: 48 |
E: NA; 80.14 (10.2); NA C: NA; 77.25 (8.5); NA |
NA | IMJXPCL |
| Xu ZL 2020, China | PU | KFX (topical, qod) and Gene Time (topical, qod) | Gene time (topical, qod) | 28 | Total effective rate | E: 25 C: 25 |
E: 45-75; 55.5;18/7 C: 41-73; 55.2; 19/6 |
NA | HKLPCL |
- Abbreviations: Ads, adverse effects; bid, twice a day; C, control group; CMFEU, Chinese medicine for external use; CMP, Chinese medicine powder; E, intervention group; EWTLI, electromagnetic wave treatment lamp irradiation; FHEA, Fulin honey external application; GSWS, gauze soaked with saline; HZKPCL, Hunan Zhongnan Kelun Pharmaceutical Co., Ltd; HKLPCL, Hunan Kelun Pharmaceutical Co., Ltd; IMDPCL, Inner Mongolia Demo Pharmaceutical Co., Ltd; IR, infrared irradiation; IMJXPCL, Inner Mongolia Jingxin Pharmaceutical Co., Ltd; LOEA, Lithospermum oil external application; NA, not available; PU, pressure ulcers; qd, once a day; qod, once every other day; tid, third a day; TDP, TDP Lamp irradiation; YNB, Yunnan Baiyao for external use.
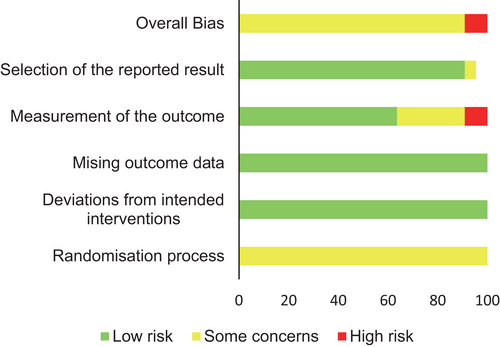
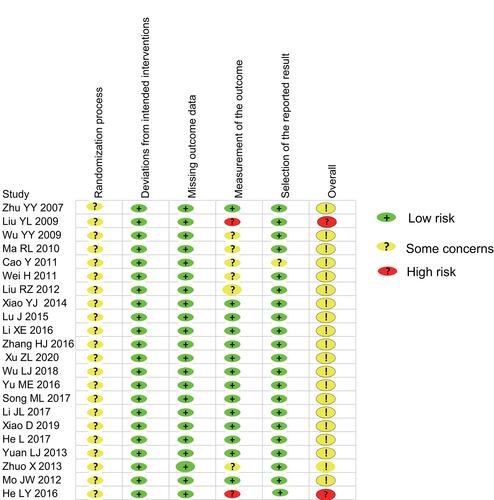
Overall, the methodological quality of the included studies was categorised as moderate. All studies mentioned the randomization principle, but only two RCTs described the details of the specific method.18, 35 Also, only two RCTs26, 35 reported the blind information to participants and researchers. There was no evidence of selective reporting bias or other biases in the included studies. The risk of bias in the articles was mostly assessed as ‘some concerns’. Figures 2 and 3 show all of the bias assessment details in each study.
3.3 Primary outcomes
3.3.1The total clinical effective rate of KFX in the treatment of pressure ulcer
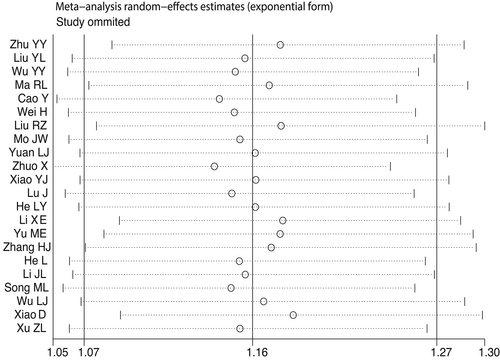
As shown in Figure 4, the 22 RCTs with 1575 participants provided data for the outcome. Using the random effects model, the analysis showed that compared with management without KFX, KFX combined with basic wound care or KFX combined with basic wound care and another topical drug or physical treatment was associated with a statistically significantly better total clinical effective rate. (RR: 1.17; 95% CI, 1.06-1.28; P = .001; I2 = 81%) (shown in Figure 4). Because of the high heterogeneity (81%), we conducted a sensitivity analysis that indicated a robust result (Figure 5). In addition, a meta-regression analysis was performed to identify covariates that might affect the total clinical effective rate. No significant correlations were found between year of publication (P = .155), frequency of dressing change (P = 1.01), and the total clinical effective rate. However, both treatment duration (P = .017) and use of KFX combined with basic wound care or KFX combined with basic wound care and another topical drug or physical treatment (P = .016) were statistically significantly associated with the total clinical effect.
According to the result of the meta-regression analysis, we explored the differences in the efficacy of using KFX combined with basic wound care or KFX combined with basic wound care and another topical drug or physical treatment by subgroups (Figure 6). The results showed a significant difference in the total clinical effect rate between KFX combined with basic wound care and controls. (n = 1018, RR 1.21, 95% CI [1.07, 1.36], I2 = 82%, P = .003). No differences in the total clinical effective rate between patients using KFX combined with basic wound care and another topical drug or physical treatment with controls (KFX combined with basic wound care and another topical drug: n = 290, RR 1.05, 95% CI [0.80, 1.37], I2 = 86%, P = .71; KFX combined with basic wound care and topical physical treatment: n = 267, RR 1.15, 95% CI [0.86, 1.52], I2 = 87%, P = .34). Results indicated that using KFX combined with basic wound care was effective, but combining KFX with other topical drugs or physical treatments did not increase the total clinical effective rate.
Moreover, based on treatment duration, we performed a subgroup analysis based on 12 articles.14, 15, 19, 21, 23-27, 30, 34, 35 (Figure 7). The results showed that there was no significant difference in total clinical effective rate between interventions and controls when the treatment duration was 28 days or 30 days (treatment duration: 28 days: n = 107, OR 3.04, 95% CI [0.25, 37.32], I2 = 50%, P = .38; 30 days: n = 256, OR 0.58, 95% CI [0.11, 3.15], I2 = 65%, P = .53). But when treatment duration was not so long, increasing the treatment duration increased the total clinical effective rate (treatment duration: 14 days: n = 158, OR 5.48, 95% CI [1.47, 20.43], I2 = 0%, P = .01; 20 days: n = 78, RR 6.72, 95% CI [1.75, 25.85], P = .006; 21 days: n = 132, OR 5.93, 95% CI [1.86,18.91], I2 = 65%, P = .003).
3.4 Secondary outcome
3.4.1 The complete healing time
Eleven RCTs with 987 cases reported complete healing time.15, 17, 18, 21-23, 27, 29-31, 33 Using the random effects model, the results showed that complete healing time was shorter in the experimental group that used KFX combined with basic wound care or KFX combined with basic wound care and another topical drug or physical treatment (MD = −5.11; 95% CI [−8.19, −2.02]; P = .001) (Figure 8). The sensitivity analysis showed that the result was robust when we exclude any study from the analysis.
3.5 Adverse effects
No data on side effects were reported in any of the 22 studies.
3.6 Publication bias
We then conducted a publication bias analysis of the total clinical effective rate of the 22 studies included in the meta-analysis. We found publication bias in included studies (Begg's test, P = .002, Egger's test, P = .002 as well as asymmetric funnel plot). Moreover, trim-and-fill estimations for the adjustment of publication bias indicated that publication bias impacted our results. But we found no publication bias in the complete healing time of the 11 included studies (the funnel plot appears asymmetric, but Begg's test, P = .640, Egger's test, P = .134).
4 DISCUSSION
Overall, we conclude that the use of KFX combined with basic wound care or KFX combined with basic wound care and another topical drug or physical treatment increases the total clinical effective rate of pressure ulcers and shortens the complete healing time of pressure ulcers based on the results of 22 RCTs involving 1575 participants. In addition, the subgroup analysis shows that using KFX combined with basic wound care is effective for the treatment of pressure ulcers. But adding KFX to other topical treatments (physical or drug) may not improve the total clinical effective rate. Part of the reason for the above results may be because of the topical physical treatments or drugs that are effective for the pressure ulcers themselves. The topical physical treatments cover infrared irradiation, TDP lamp irradiation, and electromagnetic wave treatment lamp irradiation, all of which have thermal effects to accelerate blood circulation, promote epithelial cell growth, and aid in wound healing.7, 28, 36 Drug treatment includes the antibiotic (Li Fuping, Metronidazole) or gene time (composed of recombinant human epidermal growth factor). Generally, physicians often use antibiotics topically to reduce the risk of infection in pressure ulcer wounds, but this may not be supported by other experts. They do not recommend antibiotics if there is no clear evidence of infection.6 A meta-analysis found no consistent evidence of a difference in pressure ulcer healing between ulcers treated with interventions with antimicrobial properties and those treated with alternative interventions.37 The combined use of antibiotics requires caution.
In addition, based on the duration of 12 RCTs, the subgroup shows that the treatment duration (above or including 28 days) may not be related to the increase in total clinical effective rate. However, if the treatment duration is not so long, the effective rate may increase by increasing treatment duration, except when the treatment duration is 15 days (15 days: n = 324, RR 0.18, 95% CI [0.07, 0.47], P = .0006). The lower total clinical effective rate of 15 days compared with 14 days could be caused by the controls' treatment measurement, which was Lithospermum oil for external application, a very effective method for treating pressure ulcers.
One study27 reported the serum IL-6 levels and serum CRP levels before and after the treatment. The serum levels of IL-6 and CRP apparently decreased after treatment with KFX (the difference was statistically significant P < 0.05), suggesting that KFX can reduce the local inflammatory response of pressure ulcers.
Pressure ulcers often become chronic wounds that are difficult to treat. Healing of chronic pressure ulcers contains three phases: the inflammatory phase, the proliferative phase, and the remodelling phase.38 In wounds with non-healing pressure ulcers, the three processes get lost and the ulcers are locked into a state of chronic inflammation that prevents them from healing.39 The molecular effect and signalling pathways of KFX in skin wound healing are still unclear. Some studies have demonstrated that KFX can inhibit inflammation and promote cell proliferation, fibrogenesis, and remodelling by enhancing JAK/STAT3 signalling, Smad3 activities, nuclear factor kappa B(NF-κB), as well as extracellular signal-regulated kinase (ERK) pathways.10, 11, 40, 41 Besides, KFX has the effect of improving microcirculation, enhancing immunity, and being antibacterial and antitumor.41, 42 Overall, KFX can speed up the healing process of pressure ulcers and shorten the complete healing time.
As we all know, pressure ulcers often trouble the elderly who have been lying in bed for a long time. Nursing care for pressure ulcers is complex and time-consuming and requires a multifaceted approach such as support surfaces, proper nutrition, proper wound care, dressings, non-surgical and surgical treatments as needed, etc.6 In clinical practice, the nursing physician makes plans according to the specific conditions of the patients. In pressure ulcer patients treated with the aim of promoting wound healing, the nursing physician should consider the efficacy and safety of the clinical treatment. For frail pressure ulcer patients treated with palliative care as a goal, nursing physicians should not only consider the clinical efficacy of the treatment but also pay attention to seeking a comfort-oriented and safe approach with low economic burden for these patients. KFX, pharmaceutical preparations of P americana, has high penetration and little irritation to the skin. Using the medical gauze soaked with KFX on the surface of the wound creates a moist and safe wound environment that is conducive to wound healing43 and prevents wound surface from infection. In order to relieve the pain of the patients and protect nascent granulation tissue, it is better to change the dressing gauze as little as possible. We can change the gauze once or twice a day and then keep the gauze filled with KFX by a syringe. This type of dressing procedure is simple in operation, inexpensive, and easily accepted by patients.
The present study was limited by the selection bias generated by the design and reporting of the included studies. The included 22 RCTs all use the random sequence generation method, but only two studies adequately and accurately described these methods, no information about allocation hiding was mentioned. The detection bias could be unavoidable as only two studies used the blind method (one is double-blind and another is single-blind). Besides, the 22 RCTs were all published in Chinese and assessed as having a high risk of bias of concern. Although we have already used a comprehensive range of databases and search terms to increase the number of studies retrieved, publication bias is still detected. In addition, the reported data were insufficient for an overall analysis as no side effects were assessed in the included studies.
In future research, RCTs need to be prevented from selection bias by adequate allocation concealment and detection bias by blind measurement methods. Future studies should also evaluate the equality of life, relief of wound pain, and wound recurrence rate. And long-term follow-up would be needed to examine the durability of the clinical effect of the disease.
5 CONCLUSION
The combination of KFX and basic wound care is effective in increasing the total clinical effectiveness and shortening the complete healing time of pressure ulcers.
ACKNOWLEDGEMENTS
Hospital of Chengdu University of TCM Scientific Research Capacity Enhancement “Hundred Talents Program” (Grant No. 20ZXB04).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request and the research data are not shared.