Healthcare resource use and associated costs for patients with an ileostomy experiencing peristomal skin complications
Abstract
Peristomal skin complications (PSCs) have a significant impact on quality of life and ostomy treatment costs. This study aimed to assess the healthcare resource use for patients with an ileostomy and PSCs symptoms. Two surveys were developed and, after validation by healthcare professionals and patients, data were collected on healthcare resource use while not experiencing any PSCs symptoms and while experiencing complications of various severities, as defined by the modified Ostomy Skin Tool. Costs applied to resource use were assigned from relevant United Kingdom sources. Additional healthcare resource use associated with PSCs, relative to no complications, was estimated to result in a total cost per instance of £258, £383, and £505 for mild, moderate, or severe PSC, respectively. The average estimated total cost per complication instance, weighted across mild, moderate, and severe PSCs, was £349. Severe-level PSCs were associated with the highest cost, because of the treatment-level required and the longer duration of symptoms. There is potential for clinical benefits and economising in stoma care if interventions are implemented that reduce the incidence and/or severity of PSCs.
1 INTRODUCTION
The creation of a stoma is a major operation that involves the surgical diversion of the digestive or urinary systems to an opening in the abdomen, and may be performed for a number of reasons, including cancer, inflammatory bowel disease, or diverticulitis.1 There are at least 176 000 people who are currently living with a stoma in the United Kingdom (UK), with more than 21 000 additional stomas formed annually.2, 3
Ostomy patients experience reduced quality of life relative to the general population, for example, because of embarrassment or worry about noises or odours from their stoma.4, 5 In addition, many people with a stoma will experience leakage of stomal output, which can result in irritant contact dermatitis, the primary risk factor for damage to the skin surrounding the stoma is known as a peristomal skin complication (PSC).6-8 PSCs can have a substantial negative impact on patients' quality of life as they can result in irritation or pain and can lead to difficulty affixing stoma appliances to the stoma, which can lead to increased leakage and a cycle of worsening PSCs.5, 9-11 This issue is further exacerbated by the fact that although PSCs account for the majority of visits to stoma care nurses (SCNs), a large number of patients currently fail to recognise or seek treatment for stoma-related skin problems.5, 7, 10, 12-14 As such, patients' first presentations to the healthcare system can be with serious PSCs that may be more resource intensive and thus more costly to treat, resulting in a substantial burden on healthcare systems.
Patients with an ileostomy (diversion of the small intestine) are at particularly high risk of PSCs because of the higher levels of corrosive proteolytic enzymes in their liquid faecal output.6, 7, 10, 14 The proportion of ostomy patients with ileostomies is estimated to be 36%, giving a total population of around 64 000 people with an ileostomy in the UK.15
There are a number of published studies that evaluate PSC-related healthcare costs.16-23 However, to our knowledge, none of these studies focus specifically on patients with ileostomies or on healthcare costs in the UK; furthermore, some are based only on small sample sizes and do not consider the patient perspective.6, 7, 10, 14 Therefore, the objective of this study was to assess the healthcare resource use (HCRU) for patients with an ileostomy in the UK while experiencing PSC symptoms of different severities and evaluate the magnitude of difference in resource use, and therefore cost, between the different specialties. It was hypothesised that the overall HCRU cost would be higher for patients with more severe PSCs, as the symptoms would last for a longer duration and require more intense and specialised treatment.
2 MATERIALS AND METHODS
2.1 Ostomy skin tool 2.0
Current UK guidelines recommend that healthcare professionals assess the severity of PSCs using the Ostomy Skin Tool (OST).24, 25 PSCs are assessed based on the area affected and severity of symptoms for three different categories: discolouration, erosion, and tissue overgrowth (DET).24 The overall severity of the PSC is then quantified based on the composite DET score, defined on a scale from 0 to 15, and subjects are subsequently assigned to one of the four severity categories: ‘normal skin’ (DET = 0), ‘mild’ (DET = 2–3), ‘moderate’ (DET = 4–6), or ‘severe’ (DET = 7–15).26
One limitation, however, of the OST is that it is reliant on the presence of discolouration, to some degree, in the peristomal area. In the absence of any discolouration, the DET score will be zero, and the peristomal skin will be categorised as ‘normal skin’.26 However, 75% of participants in a recent multinational survey, for people with an ostomy, reported that they still experienced other symptoms of PSC despite the absence of discolouration in the peristomal area.27
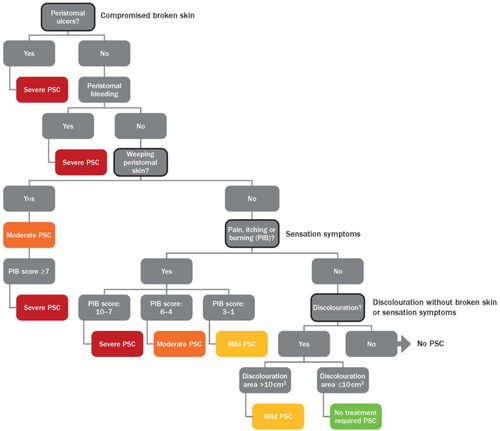
In light of the above, a modified OST, known as the OST 2.0, has recently undergone validation; Figure 1 provides further detail on the processes of the decision tree. Using a decision tree, PSCs are categorised based on predefined symptoms including peristomal ulcers; peristomal bleeding; peristomal weeping; pain, itch, or burning sensation; and discolouration.28 The OST 2.0 assesses a greater range of symptoms than the OST and uses an artificial intelligence-based approach to assess the area of peristomal skin affected by discoloration. As a result, in addition to the existing categories of ‘mild,’ ‘moderate,’ and ‘severe’ PSCs (but excluding ‘normal skin’), the OST 2.0 includes an additional ‘no treatment required’ category. Individuals presenting with exclusively peristomal discolouration will be categorised as having ‘no treatment required’ if they have ≤10 cm2 discoloured skin or ‘mild’ if they have >10 cm2.28
2.2 Survey development
This study involved two surveys designed to assess the HCRU associated with PSCs; a survey assessing the expert opinion of nurses with experience working with stoma patients in the UK, and a patient survey assessing the personal experience of UK patients with an ileostomy. Healthcare professionals (HCPs) and patients are expected to have complementary knowledge regarding the HCRU associated with PSCs. Patients may be able to provide a more accurate description of their day-to-day use of ostomy appliances and supporting products, while HCPs may be able to provide a clearer overview of the treatment that patients typically receive for different PSC symptoms.
A steering committee was formed, which consisted of four clinical experts (a dermatologist and three SCNs); the patient survey was additionally reviewed by two stoma patients. Materials relating to the surveys were validated by the steering committee, to ensure that the questions were appropriate and understandable.
2.3 Patient survey
Patients from the UK were identified through the study sponsor's research database; these individuals had consented to be contacted with respect to future market research relating to stoma care as part of the Coloplast Online Research Engine and for data to be published on an aggregated level. The survey was distributed by a third party and data were anonymised before being shared with the study sponsor. To qualify for inclusion in the study, survey respondents were required to be 18 years or older with an established ileostomy (at least six months post-surgery). A total of 105 patients completed the survey, all of whom met the inclusion criteria.
The survey questionnaire covered patient characteristics including type of appliance used, peristomal body profile, history of PSCs, and number of PSCs experienced in the last three months, as well as asking patients about their use of ostomy appliances and supporting products when not experiencing a PSC. Patients were also asked to recall up to three previous PSC instances that they had experienced within the past three months. Three months was selected based on feedback from the steering committee, as it was agreed that patients could be expected to accurately remember their HCRU over this length of time. In relation to these PSC instances, patients were asked about the symptoms experienced, the duration of symptoms, the use of ostomy appliances, use of supporting products, nurse consultations, and referrals to other specialists. Each PSC was classified as either ‘no treatment required, “mild,” “moderate,” or “severe”’ as per OST 2.0 criteria.28 The exact wording in the OST 2.0 was adapted to match the setting of the survey, asking patients about PSC symptoms in the last 3 months (as opposed to PSC symptoms because they last changed their appliance).
2.4 HCP survey
HCPs were identified from a database administered by the study sponsor, and the link to the online survey was distributed directly via email. To qualify for inclusion in this study, survey respondents were required to be nurses working in stoma care, with experience working with ileostomy patients in the UK within the last year. All HCPs with whom the survey was shared were qualified specialist SCNs, registered with the Nursing and Midwifery Council, and working in the UK. HCPs were reimbursed for their time spent completing the survey at fair market value.
In the first part of the questionnaire, HCPs were asked to estimate patients' use of ostomy appliances at baseline (while not experiencing a PSC) and while experiencing any of the PSC symptoms measured as part of the OST 2.0. In the second part of the questionnaire, HCPs were asked to estimate patients' HCRU while experiencing different sets of symptoms that aligned with each category of the OST 2.0 decision tree.28 The questions covered the duration of symptoms, number of consultations with a nurse, probability of stoma revision, proportion of patients referred to specialists, and proportion of patients prescribed PSC-related medications.
A total of 51 HCPs responded to the survey; one respondent did not pass the screening questions. Of the 50 respondents, 22 completed only the first part of the questionnaire, while the remaining 28 completed the full questionnaire.
2.5 Ethical considerations
Ethical approval for this study was not sought as the study was conducted as market research to understand, but not change, service delivery for ileostomy patients. Furthermore, patients were identified independently of the National Health Service (NHS), and HCPs were identified by virtue of their professional roles; both were noted as exclusions by the NHS Health Research Authority, precluding the need for NHS Research Ethics Committee Approval (http://www.hra-decisiontools.org.uk/ethics/).29 As for all studies involving human participants, basic ethical principles were followed, including gaining informed consent and respecting patient confidentiality.
2.6 Data analysis
Data were cleaned to exclude respondents who did not pass the screening questions and any missing answers (including when the ‘Don't know’ response was selected). Summary statistics were generated for each question. In the patient survey, subgroup analyses were also conducted, including appliance type (one-piece or two-piece), peristomal body profile (inward, outward, or regular), and PSC history (within the past 3 months, more than 3 months ago, or never). Results for patients who reported never experiencing any PSC symptoms were assigned to a distinct ‘no PSC’ category.
A student's t-test was used to compare the frequency of changing across different appliance types (one-piece appliance, two-piece pouch, and two-piece baseplate). In the patient survey, the frequency of changing appliances was compared between baseline and while experiencing PSC symptoms using a student's t-test. In the HCP survey, the same comparison was performed using a Welch's t-test to account for differences in variance as more respondents completed the first part of the survey (n = 50) than the second part of the survey (n = 28). In both surveys, the proportion of patients using each type of supporting product was also compared between baseline and while experiencing PSC symptoms using a Chi-squared test.
To provide inputs for HCRU by PSC severity for the cost analysis, data by symptom endpoint of the OST 2.0 were transformed into results for each severity category using a weighted average.28 Weightings were based on the distribution of endpoints within each severity category from data collected as part of the Coloplast Ostomy Life Survey 2019.28 For symptom endpoints for which no data were available, the weighted average was calculated across the remaining endpoints within the severity category.
2.7 Cost analysis
An estimated cost per PSC instance was calculated for each PSC severity category based on the reported HCRU relative to baseline (eg, cost of additional appliances used while experiencing a PSC in comparison to when not experiencing a PSC). Costs for ostomy appliances were based on a basket of comparators from the most common ostomy product manufacturers in the UK (Coloplast, Hollister, Salts, Convatec & Dansac), as published in the prescription cost analysis.30 The cost of nurse consultations and referrals was identified from the NHS Reference Costs and the PSSRU Unit Costs of Health and Social Care, and medication costs were sourced from the BNF and the drug and pharmaceutical market information tool.31-38 Supporting product costs were based on products available from Coloplast, as published in the prescription cost analysis.30 All products were selected from a single brand as a simplification, however given the low variation and overall costs of supporting products this is not expected to materially impact the results. The patient survey identified the proportion of patients using supporting products; however, the survey did not include a question relating to the number of supporting products used per week. This input was therefore sourced from Meisner et al., a population-based cost modelling study based on the OST.20
To assess which parameters the PSC cost estimates are most sensitive to, a deterministic sensitivity analysis was also conducted in which HCRU inputs were varied by ± 20% of their mean value.
3 RESULTS
3.1 Health care resource use
3.1.1 Patient survey
The patient survey included 105 respondents reporting on a total of 172 PSCs. The majority of respondents used a one-piece appliance (74%), and they commonly had an outward (43%), or regular (41%) body profile. Most respondents had experienced a PSC in the past three months (76%), with almost half having experienced three or more in this time period (46%). Only 11% of respondents reported having never had a PSC. No variation in ostomy appliance use was found across patients with different body profiles or PSC histories. Respondents reported more frequent changing of appliances for two-piece pouches than for one-piece appliances, whereas the changing frequency for two-piece baseplates was significantly lower than for one-piece appliances (P = 0.006; Table 1).
| OST 2.0 category | One-piece | Two-piece | All appliance types | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Appliances per week | n | Pouches per week | Baseplates per week | n | Duration of symptoms (weeks) | n | Visits to an SCN | n | Online/telephone consultations with a nurse | n | Home care nurse visits | ||
| Patient survey | No PSC | 72 | 4.59 (3.83) | 26 | 5.71 (3.26) | 2.43 (1.27) | NA | NA | NA | NA | NA | NA | NA | NA |
| No treatment required | 0 | – | 0 | – | – | 0 | – | 0 | – | 0 | – | 0 | – | |
| Mild PSC | – | 5.40 | – | – | 5.00 | – | 0.82 | – | 0 | – | 0 | – | 0 | |
| Moderate PSC | – | 9.68 | – | – | 4.70 | – | 0.54 | – | 0 | – | 0 | – | 0 | |
| Severe PSC | – | 10.82 | – | – | 6.39 | – | 2.10 | – | 0.20 | – | 0.06 | – | 0.03 | |
| HCP survey | No PSC – No history of PSCs | 49 | 4.50 (1.70) | 48 | 5.58 (2.26) | 2.54 (0.60) | NA | NA | NA | NA | NA | NA | NA | NA |
| No PSC – History of PSCs | 49 | 5.43 (3.96) | 47 | 6.34 (3.87) | 3.57 (3.89) | 0 | – | 0 | – | 0 | – | 0 | – | |
| Mild PSC | 28 | 6.96 (2.41) | 28 | 7.13 (2.23) | 5.62 (1.91) | – | 1.67 | – | 1.70 | – | 1.40 | – | 0.81 | |
| Moderate PSC | – | 2.63 | – | 2.44 | – | 1.90 | – | 1.53 | ||||||
| Severe PSC | – | 3.61 | – | 3.06 | – | 2.27 | – | 1.94 | ||||||
- Note: Results are provided as weighted averages across the decision tree categories when presented by PSC severity category, and as mean (SD) for all other results. Visits to an SCN are reported as a proportion of the week. No n-values are available for results calculated as weighted averages. In the HCP survey, respondents were asked to estimate appliance use for patients experiencing any PSC symptoms, rather than by severity category. For the purposes of calculating costs, two-piece pouch use was based on the higher value out of baseline two-piece pouch use and PSC two-piece baseplate use from the patient survey.
- Abbreviations: HCP, healthcare professional; NA, not applicable; OST, ostomy skin tool; PSC, peristomal skin complications; SCN, stoma care nurse.
Of the PSC instances reported by patients, 81% were severe (n = 139), 13% were moderate (n = 22) and 6% were mild (n = 11); no patients reported symptoms categorised as no treatment required. For both one-piece appliances and two-piece baseplates, the number of appliances used per week was higher when experiencing PSC symptoms than when not experiencing PSC symptoms (both P < .001), particularly for the most severe symptoms (Table S1). The proportion of respondents using supporting products at baseline varied substantially across product categories (Figure 2), and there was no clear trend in the proportion of patients using supporting products when experiencing PSCs compared with baseline or across PSC severity categories. On average, only patients with the most severe symptoms of peristomal ulcers, sores, or peristomal bleeding reported that they consulted with a nurse as a result of their symptoms (Table 1).

3.1.2 HCP survey
The results of the HCP survey indicate that HCPs expected ileostomy patients to change their appliances with a similar regularity to that reported by patients (Table 1). HCPs did not expect patients with a history of PSCs to have a significantly higher baseline use of one-piece appliances, two-piece baseplates, or two-piece pouches than patients with no history of PSCs (P > .05 for all comparisons). However, they did estimate that the frequency of changing one-piece appliances, two-piece baseplates, and two-piece pouches would be significantly higher when experiencing PSC symptoms than when not experiencing symptoms (P < .001, P < .001, and P = .04, respectively).
HCPs also expected more severe PSC symptoms to be associated with a longer duration of treatment and that all patients with PSCs would require consultation with a nurse, with patients with more severe PSC symptoms consulting more frequently (Table 1). Similarly, HCPs expected that patients with more severe symptoms were more likely to be prescribed medications and to be referred to other HCPs than those with less severe symptoms (Table S2). However, on average, HCPs estimated that the proportion of patients requiring stoma revision or re-surgery would be low regardless of the severity of symptoms (consistently around 1%).
3.2 Cost of PSCs
The patient survey was used to inform estimates of ostomy appliance use and supporting product use for the cost calculations, while the HCP survey was used to inform estimates of symptom duration and treatment received by PSCs, including nurse consultations, referrals, medication, and stoma revision. The HCP survey asked respondents to estimate the number of nurse consultations that patients would receive across three different categories: visits to a nurse, home care nurse visits, and non-face-to-face (online or telephone) consultations. There is some uncertainty regarding whether respondents may have considered these categories separately or in combination. Taking a conservative approach, the base case cost analysis counts only in-person visits to an SCN, which was the most frequent type of nurse consultation reported by HCPs (Table 1).
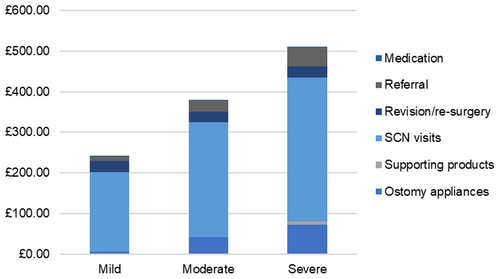
On the basis of these estimates, a total HCRU cost was calculated for each PSC severity. Total HCRU is estimated to cost £258, £383, and £505 for the duration of a mild, moderate, or severe PSC, respectively (Figure 3), as a result of both direct treatment costs and increases in ostomy appliance use compared to when not experiencing a PSC.
The impact of the nurse visits assumption was explored in a scenario analysis. When all nurse consultation types were included, the estimated cost per PSC increased by approximately 36% relative to the base case. Alternatively, if all nurse visits reported by the HCPs were assumed to be non-face-to-face visits, reflecting the potential situation during the COVID-19 pandemic, PSC costs reduce by approximately 63%. However, it is expected that this reflects an extreme rather than likely scenario, and would very likely result in an increase in other forms of HCRU, a longer duration of PSC symptoms, or a reduction in the quality of care experienced by patients.
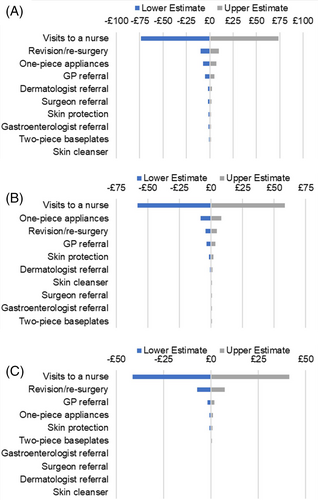
Deterministic sensitivity analysis results indicate that nurse visits were the largest cost driver across all three PSC severity categories (Figure 3). The top four parameters across all three categories were the cost of nurse visits, one-piece appliances, revision/re-surgery and GP referral (although the ordering varied across PSC severity categories). All other parameters resulted in a variation in the total PSC cost estimate of less than ± £2.50 (Figure 4).
As a scenario analysis, the PSC costs were recalculated using the number of nurse visits recalled by patients and reported in the patient survey, which were considerably lower compared to the visits reported by HCPs. As a result, the PSC costs for mild, moderate, or severe were estimated to be £51, £91, and £161 respectively.
4 DISCUSSION
PSCs have a substantial impact on the quality of life of patients living with a stoma, with symptoms ranging from mild eczema to painful ulcers, and causing difficulty attaching appliances leading to increased leakage, which can in turn further damage peristomal skin.5, 9-11 As a result, PSCs account for approximately 40% of visits to SCNs and are associated with substantial clinical and economic burden.12 This is of particular concern for patients with an ileostomy, who are at higher risk of PSCs than other ostomy patients as they are more likely to experience leakage and have higher levels of corrosive proteolytic enzymes in their output.6, 7, 10, 14, 15, 39 Leakage of stomal output can result in irritation and damage to the skin, resulting in progressive worsening of PSCs over time if appropriate treatment is not sought.5, 9-11
In the patient survey, the vast majority of reported PSC instances fell into the severe category (81%). Few patients reported mild PSC symptoms, and no patients reported symptoms categorised as no treatment required. Previous studies have found that, when assessments are carried out by HCPs, severe PSCs are the least common type of PSC.10, 19, 20 The patient survey findings therefore likely reflect the fact that patients are more likely to recognise severe symptoms as a PSC, potentially considering milder symptoms to be a normal part of having a stoma.7, 10
To our knowledge, this study is the first HCRU investigation that has surveyed both patients and HCPs to obtain estimates of the HCRU associated with PSCs.6, 7, 10, 14 Across both surveys, HCPs and patients provided consistent estimates of ostomy appliance use. However, HCPs gave higher estimates for symptom duration and the level of treatment received compared to that reported in the patient survey. This again may be because of patients not seeking out treatment for their PSC symptoms. For example, Herlufsen et al. 2006 found that, in Denmark, more than 80% of patients with a skin disorder did not seek professional assistance.10 This may also have been further impacted by the dissemination of the surveys during the COVID-19 pandemic, during which many aspects of clinical practice are likely to have changed. For example, stretched resources may have reduced the availability of nurses, and fears of catching COVID-19 may have reduced patients' likelihood of seeking treatment, thus leading to fewer face-to-face nurse consultations. Patients were asked to recall PSC instances over the past three months, so these changes may have affected their responses, particularly on questions regarding consultations with HCPs and referrals.
For the cost analysis, estimates relating to PSC treatment were therefore sourced from the HCP survey, while estimates of ostomy appliances and supporting product use were sourced from the patient survey. As such, the cost estimates apply to patients once they present to the healthcare system, not necessarily when they first develop a PSC. As expected, HCRU estimates from the surveys were highest for severe PSCs, and thus severe PSCs were associated with the highest cost per PSC instance in the cost analysis. This is aligned with a previous model estimating the cost of PSCs in the UK, based on resource use estimates from 11 SCNs across nine countries.18 Direct PSC treatment costs were higher for severe PSCs than mild or moderate PSCs, which may be partially driven by the longer duration of symptoms for severe PSCs. Overall, the cost to treat severe PSCs to resolution was found to be 1.32 times the cost required to treat moderate PSCs and 1.96 times the cost required to treat mild PSCs.
The surveys were comprehensive and accounted for a wide range of different HCRU categories. Across all PSC severities, visits to a nurse were the greatest contributor to overall costs, accounting for 73%, 76%, and 80% of the costs of mild, moderate, and severe PSCs, respectively. This is similarly reflected in the deterministic sensitivity analysis results, where visits to a nurse were shown to be the largest cost driver. However, it is important to note that visits to a nurse are critical to the resolution of PSCs, which tend to increase in severity if left untreated, and costs could be higher in their absence.
The UK has an estimated 64 000 patients currently living with an ileostomy.3 The annual prevalence of PSCs is estimated at around 88% and the severity distribution across mild, moderate and severe PSCs at 29%, 16%, and 55% respectively, with figures derived by aligning results of symptoms collected via survey to PSC categories, as defined by the OST 2.0 tool.15, 27, 28 The average total cost for additional PSC-related HCRU was £349 per PSC instance, weighted by the PSC severity distribution. In addition, these estimates result in a predicted total cost to the UK healthcare system as high as £23.2 million. Severe PSCs contribute the most to this, as they are estimated to be more costly and more frequent than mild and severe PSCs. Even considering the fact that some of these patients may not seek treatment for their PSCs,5, 7, 10, 12-14 this study highlights that PSCs in ileostomy patients likely represent a sizeable cost to the UK healthcare system in addition to the substantial burden placed on patients.
4.1 Limitations
This study has important strengths, such as consulting both patients and HCPs to gain a clear picture of HCRU and having a large sample size of HCPs used to determine PSC-associated HCRU.16, 20 To our knowledge, this study is also the first to investigate HCRU specifically in the UK and to focus on patients with an ileostomy.6, 7, 10, 14 However, there are also some important limitations to acknowledge.
The lower response rate in the second part of the HCP questionnaire may have been because of the increased complexity of the questions, despite the steering committee previously agreeing that the questions were appropriate. The response rate may have also been impacted by the COVID-19 pandemic, as HCPs would have less time available for engaging in research activities. However, despite these factors, to our knowledge, 28 SCNs represent the largest sample of HCPs used to determine HCRU associated with PSCs to date.16, 20
Secondly, patients were asked to report up to three previous instances of PSCs that they had experienced within the past three months, meaning that the results are reliant on accurate recall. On the basis of feedback from the steering committee, patients could be expected to accurately remember PSCs and associated HCRU over this length of time, however, it is likely that the results are subject to some recall bias.
A third limitation is that the patient survey did not provide an estimate for the HCRU associated with symptoms categorised as ‘no treatment required’, as no patients reported a PSC instance that met the criteria for this category. Patients with minor PSC symptoms may be less likely to consider these as indicative of a skin disorder, instead considering these symptoms to be a normal consequence of having a stoma.5, 7, 10, 12-14 HCPs provided non-zero estimates for the treatment of PSCs categorised under the new OST 2.0 as ‘no treatment required’ (Table 1). This may reflect the fact that the current OST does not include this category, and therefore, under the current assessment, nurses would likely expect all symptoms identified as a PSC to receive treatment. However, according to the OST 2.0, these patients would not be expected to need treatment and would therefore likely be associated with minimal additional costs relative to someone who was not experiencing a PSC.28 The omission of such patients from this cost analysis is therefore unlikely to result in a meaningful underestimation of PSC costs, but rather represents a conservative estimate.
Finally, previous cost analyses have assumed an increased use of supporting products while experiencing a PSC.19, 23 This was not included in the present cost analysis as the patient HCRU survey did not ask about the frequency of supporting product use while experiencing a PSC. Therefore, the current analysis may underestimate the costs associated with supporting product use while experiencing a PSC. However, given the small unit costs for supporting products, this is similarly not expected to have a substantial impact on PSC cost estimates.
5 CONCLUSIONS
There is considerable evidence that PSCs are associated with high costs in addition to having a substantial impact on patients' quality of life, with the impact increasing the more severe the symptoms.5, 9-11 This study supported the hypothesis that severe PSCs are the most expensive to treat and that there is therefore strong potential for both clinical benefits and cost savings in stoma care if interventions can be put in place that reduce both the incidence and severity of PSCs. There is still potential for stoma products to be improved in the future, in order for there to be further cost savings opportunities while still ensuring patients' quality of life is improved. In addition, allowing nurses the opportunity to evaluate the peristomal skin remotely might also prove beneficial in order to detect evolving skin complications early, thereby avoiding severe PSCs in the first instance. This study represents the first analysis to provide HCRU estimates specifically for patients with an ileostomy in the UK using a large sample of both patients and HCPs. The sample size for the HCP survey was, to our knowledge, larger than that used for all previous resource estimates in this area and thus provides more accurate estimates of the treatment cost associated with mild, moderate, and severe PSCs in this patient group compared with previous analyses.6, 7, 10, 14 These results therefore provide a useful overview of the cost of PSCs in these patients as well as the potential to be used to inform future economic modelling relating to novel ileostomy interventions in the UK.
ACKNOWLEDGEMENTS
The authors thank the patients, the investigators and their teams who took part in this study. The authors acknowledge Brian Devlin, Sarah James-Reid and Terri Porrett for their roles on the steering committee for the survey. The authors also acknowledge Joseph Smith, PhD, from Costello Medical, UK, for medical writing and editorial assistance based on the authors' input and direction, and Rachel Crosby, from Costello Medical, UK, for support in initial survey development.
FUNDING INFORMATION
This study was sponsored by Coloplast A/S. Support for conducting the study, analyses and writing assistance for this article was provided by Costello Medical, UK in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
L. de Fries Jensen, F. Mthombeni and J. Håkan-Bloch were employed by Coloplast A/S. V. Vardanega and N. van Hest were employed by Costello Medical UK, who were contracted by Coloplast A/S to support this analysis. N. Rolls and T. Karlsmark were compensated at fair market value by Coloplast A/S for providing their expert opinion.
CONFLICT OF INTEREST STATEMENT
L. de Fries Jensen, F. Mthombeni, J. Håkan-Bloch: Employees of Coloplast A/S. V. Vardanega, N. van Hest: Employees of Costello Medical UK, contracted by Coloplast A/S. N. Rolls, T. Karlsmark: Compensated at fair market value by Coloplast A/S.
Open Research
DATA AVAILABILITY STATEMENT
Data available on request due to privacy/ethical restrictions. The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.