Honey therapies for dermatological disorders: more than just a sweet elixir
Conflict of interest: None.
Funding source: None.
Abstract
Honey possesses antibacterial, anti-inflammatory, and healing properties that benefit wound healing and tissue regeneration. For centuries, honey has been utilized in traditional medicine as a binder or vehicle for creams and lotions and also for therapeutic purposes. The overuse of antibiotics and antimicrobial agents leading to drug resistance has emphasized the resurgence of honey's application in wound care. For many dermatological disorders, there is an interest in developing therapeutics with fewer side effects than traditional therapies and enhanced wound healing abilities to expedite tissue regeneration. This paper reviews the properties and components of honey that contribute to its wound-healing-based applications, the types of honey employed in medicine, and its dermatological applications. Based on the evidence from case reports, clinical trials, and in vitro studies, honey has been characterized as a safe, cost-effective, and readily available treatment option for many skin conditions, including microbial infections, atopic dermatitis, psoriasis, necrotizing fasciitis, ulcers, as well as thermal and other types of wounds.
Introduction and background
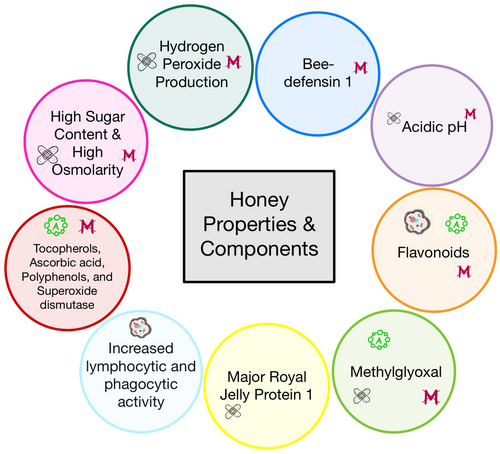
Honey has been utilized to treat infections and wounds since ancient times. However, the use of honey and other natural products decreased with the discovery and creation of modern antibiotics. Nowadays, microbial drug resistance is a growing concern, and honey has regained scientific and clinical interest as an antimicrobial agent due to its efficacy against antimicrobial-resistant organisms. Since honey has several antimicrobial components and different antimicrobial mechanisms, resistance to honey is unlikely (Figure 1).
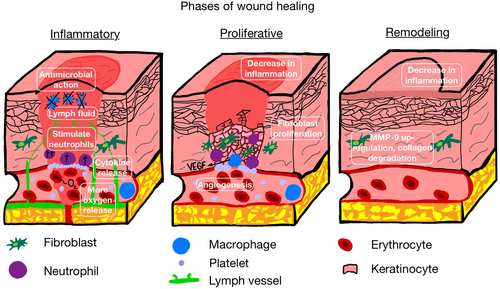
Wound healing has three overlapping phases: inflammation, proliferation, and remodeling. In the inflammatory phase, macrophages are induced to release pro-inflammatory cytokines: TNF-α, IL-6, IL-1β, etc., which encourage fibroblast proliferation. Neutrophils are also stimulated to remove debris and microbes. The proliferative phase involves angiogenesis, collagen deposition, granulation tissue formation, and epithelization. In the remodeling phase, collagen is remodeled and reorganized. Honey is involved in all three phases to accelerate the wound-healing process and minimize excessive scarring (Figure 2).1
In addition to honey's antimicrobial activity, it is also anti-inflammatory, an antioxidant, and can facilitate re-epithelization and angiogenesis by stimulating skin and immune cells. Honey has many components and properties that support its bactericidal, anti-inflammatory, and healing potential. Its acidic pH of around 3.2–4.5 promotes healing by increasing the release of oxygen from hemoglobin at the tissue site, decreasing protease activity, and increasing fibroblast activity.1 Honey's acidity also prevents bacterial growth and activity.1
Honey is mainly composed of sugars, such as glucose and fructose (70%); these sugars have high osmotic activity, which prevents bacteria from growing due to a lack of water. The increase in lymph outflow at the wound site also aids in the removal of debris, necrotic tissue, and slough.1
In addition, honey produces hydrogen peroxide using the enzyme glucose oxidase, which originates in bees. Catalase, which breaks down hydrogen peroxide, is obtained from flower pollen. Thus, the level of peroxide in honey depends on how much pollen the bee collects and the catalase activity of that pollen.2 Hydrogen peroxide produces hydroxyl radicals that attack the membrane lipids and the DNA of bacteria. It also can stimulate fibroblast proliferation and recruit macrophages to the wound site. Macrophages release vascular endothelial growth factor (VEGF) and stimulate angiogenesis.1 Honey may retain its antimicrobial activity even in the presence of catalase or the absence of glucose oxidase, and thus, this type of honey is known as “non-peroxide honey”.2, 3
Honey also contains various peptides and enzymes, such as polyphenols and bee defensin-1, contributing to its antibacterial activity.4 Bee defensin-1, a cysteine-rich antimicrobial peptide that disrupts the integrity of membranes of pathogenic organisms, also has potent activity against fungi and yeast mycelia, protozoa, mites, and viruses.1 The antioxidant activity of honey is attributed to multiple compounds such as tocopherols, ascorbic acid, and superoxide dismutase. These substances reduce the adverse effects of reactive oxygen and nitrogen species.5 Flavonoids in honey inhibit pro-inflammatory enzymes such as lipoxygenases, cyclooxygenases, and nitric oxide synthases, which produce pro-inflammatory mediators including cytokines, nitric oxide, and chemokines.6 Flavonoids are also antifungal and antioxidant agents. Research shows they can attach to the yeast cell wall, affecting membrane integrity, mitochondrial function, and biogenesis.7
Another protein found in honey, major royal jelly protein 1 (MRJP1), is responsible for the elevated production of matrix metalloproteinase-9 (MMP-9) and pro-inflammatory cytokines. Increased levels of MMP-9 in the epidermis lead to the degradation of type IV collagen in the basement membrane, allowing for vascular sprouting and maturation as well as cell migration and proliferation.1 In summary, honey is an excellent candidate for antimicrobial treatments and wound healing (Tables 1 and 2). Honey's key antimicrobial components include its high sugar content, hydrogen peroxide production, bee defensin-1, various antioxidants, and flavonoids. The key wound healing components and properties are acidic pH, high sugar content, hydrogen peroxide production, and MRJP1. This paper will discuss the potential therapeutic applications of honey-based products on various dermatological diseases, including amputation wounds, burns, skin grafting sites, and different types of ulcers.
| Honey properties and contents | Actions |
|---|---|
| Acidic pH | Antimicrobial activity |
| High sugar content/osmolarity | Bacterial cell shrinkage and antimicrobial dehydration |
| Hydrogen peroxide production | Antimicrobial activity |
| Bee defensin-1 | Antibacterial activity, antifungal activity, antiviral activity |
| Tocopherols, ascorbic acid, polyphenols, and superoxide dismutase | Antioxidant activity, antimicrobial activity |
| Flavonoids | Inhibition of pro-inflammatory enzymes and mediators, anticandidal, antioxidant |
| Increased lymphocytic and phagocytic activity | Stimulation of B-lymphocytes, T-lymphocytes, and monocytes to secrete cytokines which activate the immune response to infection |
| Methylglyoxal | Bactericidal agent |
| Honey properties and contents | Actions |
|---|---|
| Acidic pH | Increasing the release of oxygen at the tissue site, decreasing protease activity, and inducing fibroblast proliferation |
| High sugar content/osmolarity | Removes debris, slough, and necrotic tissue by increasing lymph fluid at the tissue site |
| Hydrogen peroxide production | Induces macrophages to produce VEGF, which induces angiogenesis and fibroblast proliferation |
| Major Royal Jelly Protein 1 | Upregulates expression of MMP-9, thus degrading collagen type IV during re-epithelialization |
| Methylglyoxal | Decreases lipid peroxidation and inflammation, promotes fibrosis |
Search strategy and selection criteria
Articles for this literature review were identified by searches of MEDLINE, PubMed, clinicaltrials.gov, and references from relevant articles using free-text terms including but not limited to: “honey,” “skin disorders,” “dermatology,” and “apitherapy.” In vitro, in vivo, case, and clinical trial studies published in English were included, focusing on articles published between January 2013 and September 2023. For more extensive studies focused on multiple diseases or wound types, the corresponding reference was cited regardless of the year it was published. Disorders related to oral mucosa, intra-abdominal wounds, and wounds outside the scope of dermatology were excluded.
What is medical-grade honey?
Specific characteristics define medical-grade honey. It is sterilized by gamma irradiation to inactivate bacterial spores without modifying the original biological activity. It is also organic, free of toxic contaminants, and processed according to safety regulations and standards.8 Even though medical-grade honey is sterilized, no cases of wound infection due to spores in non-irradiated honey have been reported to date.5 Medical-grade honey is formulated into many components, including tubes, gels, and dressings.9 The effectiveness and potency of honey against microorganisms depend on the type of honey produced, which is contingent on the plant's biological origin, the bee's health, etc.
Mānuka honey, derived from the Leptospermum scoparium plant indigenous to New Zealand and coastal Australia, is a front-runner in the type of honey used for medicinal therapies due to its higher content of methylglyoxal (MGO), a bactericidal and antioxidant agent measured by the Unique Mānuka Factor (UMF) rating which makes the honey even stronger at combating bacteria and improving healing.10 Specifically, MGO attacks the arginine residues in collagen and leads to a disruption that promotes fibrosis in chronic tissue infections. In addition, MGO interacts with the nucleophilic centers of macromolecules such as DNA. In gram-positive organisms, MGO downregulates the autolysin enzyme involved in the cleavage of bacterial cell wall components and cell division.1 MGO also decreases lipid peroxidation, a free radical oxidation of polyunsaturated fatty acids implicated in various diseases and pathologies such as neurodegeneration, aging, and carcinogenesis1, 11 (Table 2). Furthermore, mānuka honey is unique because it exhibits antibacterial activity, which cannot be attributed to hydrogen peroxide, likely due to its high MGO content; this is known as “non-peroxide honey”.3 For its unique properties, mānuka honey is now cultivated globally. In addition to antibacterial activity, mānuka honey stimulates macrophages to release TNF-α, IL-1β, and IL-6 cytokines, aiding tissue healing by inducing keratinocyte migration and proliferation.5 Other types of honey utilized in medicine are kanuka honey, made from another New Zealand native tree, acacia honey, black locust from bees foraging in Appalachian forests, and Tualang honey, a wild multi-floral honey produced by Apis dorsata in Malaysia, amongst many other monofloral and multi-floral varieties.5, 12 Mānuka honey-mediated antimicrobial activity is mainly attributed to methylglyoxal, whereas other honey types are mainly due to hydrogen peroxide.13
Mānuka honey was approved as a recommended alternative for treating wounds by the U.S. Food and Drug Administration in 2007.10 In clinical practice today, several FDA-approved honey-based wound care products exist in gels, ointments, and dressings. Most of them are formulated with medical-grade mānuka honey. However, alternatives are made with other types of honey5 (Table 3). The FDA approved these treatments for various skin conditions, including exuding wounds, diabetic foot ulcers, leg ulcers, pressure ulcers, burns, traumatic injuries, surgical wounds, and recalcitrant wounds. Despite FDA approval and the wide availability of these products, their medical use is limited, likely because of the misconception that there is a lack of evidence supporting the efficacy of honey's therapeutic purposes.5
| Product name | Composition | Clinical applications referenced |
|---|---|---|
| L-Mesitran® Soft | 40% medical-grade honey (not Manuka) with lanolin, polyethylene glycol, and vitamins C and E | Herpes labialis and herpes simplex |
| Gingivostomatitis | ||
| Foot ulcers (some cases with L-Mesitran® Soft followed by L-Mesitran® Tulle, a polyethylene dressing impregnated with L-Mesitran® Soft) | ||
| Potential for C. auris treatment | ||
| L-Mesitran® Ointment | 48% medical-grade honey (not Manuka), lanolin, cod liver oil, sunflower oil, calendula, aloe vera, zinc oxide, and vitamins C and E | Recalcitrant heel pressure ulcers |
| Medihoney® Barrier cream | 30% Manuka honey and other components | Intertrigo |
| Medihoney® Gel Wound and burn dressing | 100% Manuka in a hydrocolloid suspension | Aplasia cutis congenita |
| Activon® | Paste formula—100% Manuka | Penile denudation |
| Various honey varieties and mixtures | Australian jarrah (eucalyptus honey) | Tinea infections |
| Honey, olive oil, beeswax mixture | ||
| Medical grade kanuka honey cream | 90% medical-grade kanuka honey and 10% glycerin | Herpes simplex labialis |
| Honey-containing cream | Mixture of royal jelly, bee venom, propolis, and honey | Visible appearance of wrinkles |
| Natural honey | Purchased from Langnese | Thermal wounds (honey compared to silver sulphadiazine) |
| Natural honey | Obtained from Syzygium cumini (locally known as Jamun, unprocessed and undiluted) | Fournier's gangrene |
| Natural honey | Kanuka honey | Psoriasis |
| Other honey-based products | Not listed in reference | Skin bacterial infections, pilonidal sinus disease, folliculitis decalvans, surgical wounds, thermal wounds, atopic dermatitis |
- Other commercially available medical-grade honey-based products are FDA approved and are not listed in this table.
Bacteria, fungi, and viruses
Different honey varieties have efficacy against a broad spectrum of bacteria, including Staphylococcus aureus, Pseudomonas aeruginosa, Escherichia coli, Acinetobacter baumannii, and Staphylococcus epidermidis. Honey is also effective against biofilms, which are particularly difficult to remove or penetrate, by preventing biofilm development, reducing the metabolic activity of already formed biofilms, or altering the gene expression of genes involved in biofilm formation.5 Honey has excellent antibacterial efficacy against MRSA and a variety of Pseudomonas species, making it a possible treatment for wound and burn infections. It also has efficacy against hemolytic streptococci and vancomycin-resistant enterococci.4
A worldwide fungal epidemic caused by Candida auris created even more complications for COVID-19 patients during the pandemic and has since continued to rise as a challenge for healthcare facilities.14, 15 C. auris is a severe and rising medical concern, causing mortality rates up to 60% in intensive care units. Some strains of C. auris are also notably resistant to current anti-fungal treatments, including fluconazole, amphotericin B, and echinocandins. In vitro studies on the highly resistant fungal species C. auris showed susceptibility to treatment by the trademarked medical-grade honey cream, L-Mesitran® Soft. Unprocessed honey also reduced the growth of five Candida species, including C. auris, C. albicans, C. glabrata, C. krusei, and C. parapsilosis. However, L-Mesitran showed a significantly higher antimicrobial activity, likely attributed to enhancement by different supplements such as Vitamins C and E.13, 16 It is important to note that C. auris' susceptibility to honey did not depend on its genetic origin, meaning that different honey varieties may be considered a C. auris treatment. Due to limited treatment options for these multiresistant isolates, honey may be a promising, safe, and cost-effective treatment for open wounds or skin colonized by C. auris.17 Future clinical studies are needed to evaluate the impact of honey on C. auris infections in patients.
Another in vitro study found that Australian jarrah, also known as eucalyptus honey, inhibits and kills dermatophyte species that cause tinea infections. Clinical studies on honey treatment for tinea infections in humans are limited. However, an open pilot study tested the topical application of a honey, olive oil, and beeswax mixture on 37 patients with tinea infections in various locations. Clinical response was obtained in 86% of patients with pityriasis versicolor, 78% with tinea cruris, and 75% with tinea corporis. A complete cure was obtained in 75, 71, and 62% of patients with pityriasis versicolor, tinea cruris, and tinea corporis, respectively.18
The exact mechanism by which honey prevents viral infections is complex and unknown. However, specific bioactive components, such as methylglyoxal, quercetin, chrysin, kaempferol, etc., may provide antiviral activity by preventing the entry, entrapment, and replication of viruses.19, 20
Enhancing the antimicrobial activity of honey
Some medical-grade honey formulations, including L-Mesitran Soft, are supplemented with other ingredients, such as Vitamins C and E, which enhance the antimicrobial activity of honey by synergistic effects. These vitamins promote immunomodulatory effects and increase antimicrobial sensitivity via diverse mechanisms, including reducing the synthesis of extracellular polymers that form bacterial biofilms and altering the bacterial cell surface to render it more permeable to antibiotics.13
In addition, combination formulations such as Oxymel, a combination of honey and vinegar utilized in traditional medicine settings, may merit further evaluation.21 The acetic acid in vinegar has antibacterial activity at low concentrations and, synergistically with honey, can eradicate biofilms. While honey is now clinically used to treat infected wounds, this use of a complex, raw natural product (NP) mixture is unusual in modern Western medicine. Finally, studies show that honey has more significant antibiotic activity when combined with traditional antibiotics like fosfomycin against multidrug-resistant bacteria.22 In summary, honey has greater antimicrobial potential against various microorganisms when combined with other substances.
Human herpesvirus types 1 and 2
Herpes labialis is evident as vesicles in the nasolabial region caused by herpes simplex virus HSV-1 or HSV-2 infections.23 Recurrent herpes labialis may respond to a trademarked medical-grade honey formulation, L-Mesitran®, decreased sore healing time, increased subjective healing score, and decreased pain and itching compared to conventional cold sore treatments such as oral and topical acyclovir.24 In another clinical trial, with a 1 : 1 random assignment of 952 adult patients experiencing a herpes simplex labialis episode, there was no evidence of a difference between medical grade kanuka honey and 5% acyclovir topical treatments.25 In a clinical trial of 100 children aged 2–8, the group receiving a combination of honey and oral acyclovir had significantly earlier disappearance of herpes simplex gingivostomatitis than those receiving acyclovir alone. The treatment group also had significantly lower pain scores, better eating and drinking ability, and less analgesic need than the control group.26 These studies confirm that honey is a potent antiherpetic agent and should be considered in a treatment regimen for lesions caused by the herpes virus.
Atopic dermatitis & psoriasis
Twelve patients with atopic dermatitis treated with topical honey improved with diminished erythema, edema, and no side effects. Five patients with atopic dermatitis significantly decreased their Scoring Atopic Dermatitis index after 4 and 8 weeks of consuming forest honey compared to patients who did not consume honey.27 Six honey-treated patients with psoriasis vulgaris improved with psoriasis area and severity index score to 80 1 month after finishing the honey treatment.6 In a clinical trial with 15 adult patients with psoriasis, medical-grade honey and an aqueous cream provided the same impact on the visual analog score, a method used to measure itch intensity on different lesions with no side effects. However, aqueous creams are less effective than topical steroids, implying honey may represent an alternative to non-medicated creams. Further studies with a larger patient population are needed.28
Necrotizing fasciitis
In a cross-sectional study of 17 adult men with a necrotizing infection of the scrotum (Fournier's gangrene), topical honey application reduced healing, hospitalization time, and costs compared to patients in other studies where honey was not utilized to treat the infection.29 In a clinical trial with 30 male patients, the honey-treated group showed faster clearing of necrotizing tissue and a reduced hospital stay than the control group treated with a Eusol-soaked dressing. In these studies, honey was found to be beneficial, and no irritation was reported. However, larger scale trials are needed before honey can be recommended as an addition to the treatment for Fournier's gangrene.30
Wrinkles, photoaging, and sun damage
In vitro studies on human immortalized keratinocytes and human skin tissue models showed that honey extracts lower the levels of DNA strand breaks and attenuated the decrease in cell viability following UVB exposure. Honey extracts also reduced the UVB-induced upregulation of matrix metalloproteinases (MMPs), specifically MMP-3, -7, and -9, which are responsible for degrading collagen and contributing to tumor progression.31 When combined with royal jelly, bee venom, and propolis, a honey-containing cream formulation reduces the visible appearance of wrinkles. However, this study did not test the formulation's impact on long-term skin aging.32
Intertrigo
A trademarked honey-containing barrier cream, Medihoney® Barrier Cream, has been shown to help treat intertrigo. The recommended treatment for intertrigo is cleansing, moisturizing, and applying a topical barrier product such as a lipid, silicone, or silicone-based polymer paste. The barrier cream containing mānuka honey has an additional antimicrobial property advantageous in treating intertrigo. In four patients with intertrigo, from infants to elderly adults, the trademarked honey cream reduced pain, discomfort, inflammation, and redness in certain areas. However, further research is needed to compare the efficacy of this honey barrier cream to other barrier creams.33
Thermal wounds
Thermal burns are a severe, debilitating type of trauma, often incurring profound medical, social, and financial burdens on patients. In the last few decades, rigorous research efforts have been aimed at finding healing modalities for treating burn injuries, either by novel medications, natural therapeutics, or a combination. In a combined in vivo and in vitro study, medicinal honey, in conjunction with photobiomodulation, a non-invasive form of phototherapy, enhanced wound area contractions and re-epithelization in burn wounds of rats compared to each therapy alone. This combined treatment also reduced inflammation and pain and accelerated the repair process of burn wounds by augmenting various factors involved in cellular proliferation.34 In 150 patients with superficial and partial-thickness burns, the rate of re-epithelialization and healing was significantly faster in sites treated with honey than in sites treated with silver sulfadiazine (SSD), a traditional topical burn treatment. In addition, sites treated with honey were less likely to become infected with Pseudomonas species than sites treated with SSD.35 In summary, honey may be utilized in treating burns to enhance re-epithelization and prevent infections.
Surgical and other complex wounds
Since surgical wounds can take weeks or even months to heal, clinicians are interested in finding therapeutics to expedite the healing process. In one study, 59 patients with complicated surgical, chronic, and acute traumatic wounds were treated with a honey-medicated dressing for 3 weeks. Wound healing was achieved in 57 of the 59 patients, with decreased edema and wound exudate and increased advanced epithelialization. In the remaining two patients, honey treatment prevented the wounds from worsening.36 Similarly to other wound types, honey may be a useful addition to managing surgical and complex wounds.
Foot ulcers
A meta-analysis, which included 22 studies with a combined total of 1,030 patients, examined honey's use for diabetic foot ulcers. Using a honey dressing was associated with higher bacterial clearance as early as after 1 week of treatment compared to other wound dressings. It also shortened wound debridement time, defined as the period from the beginning of treatment to when necrotic tissue is cleared, and decreased the risk of amputation.37 Other studies have found that honey reduces the length of hospital stays and pain severity.38 In a case series with nine elderly patients suffering from recalcitrant heel pressure ulcers, the infection resolved within 1–4 weeks, and ulcers were healed entirely within an average of 128 days using the trademarked medical grade honey ointment, L-Mesitran®.39 Thus, medical-grade honey may be a safe and cost-effective method for treating complicated wounds with antibiotic-resistant infections at risk of amputation.
Rare diagnoses and special cases
In a 55-year-old man with penile denudation, mānuka honey, specifically Activon®, was a successful treatment after an unsuccessful split-thickness skin graft.40 Topical Mānuka honey, Medihoney®, was utilized effectively to treat a full-term neonate with a large patch of aplasia cutis congenita. It closed after applying Medihoney® twice daily for eight weeks, followed by nonadherent dressings. Despite a lack of evidence-based guidelines for treating aplasia cutis congenita, mānuka honey is a possible therapy for even large lesions of this type.41 Another case report described the at-home treatment of a male diabetic foot ulcer during the COVID-19 lockdowns. Complete healing was achieved within 4 weeks using a wound dressing with a medical-grade honey-based product alongside oral antibiotics. This treatment combination was an accessible and cost-effective alternative to debridement by an orthopedic surgeon.42 In a clinical trial with 48 adult patients who underwent surgical resection for pilonidal sinus disease, patients receiving an unprocessed honey gel had significantly lower wound healing time and volume than a placebo gel. However, this study also found increased postoperative pain and analgesic consumption using the honey gel versus placebo, possibly due to honey's low pH causing a stinging or burning sensation.5, 43 Further studies are needed to determine the efficacy of honey, especially medical-grade honey, for this specific disease.
Folliculitis decalvans
Folliculitis decalvans is a form of rare scarring alopecia with areas of follicular pustules, crusts, and erosions. Abnormal host response to Staphylococcus aureus has been implicated in the disease's pathogenesis, and thus, anti-staphylococcal antibiotics are used as first-line treatment. Other treatments for folliculitis decalvans include systemic anti-inflammatory agents, which can cause unpleasant side effects. Given these side effects, the lack of a “gold standard” therapy, and the rise in antibiotic resistance, alternative treatments are needed. One 20 year old man utilized topical Mānuka honey application and oral cephalexin to clear his scalp pustules in 6 months, allowing him to taper off cephalexin completely. Since honey is safe and cost-effective and has anti-staphylococcal properties, medical-grade honey may be considered as an adjuvant therapy to systemic treatments for folliculitis decalvans.44
Leishmaniasis
Leishmaniasis is an insect-borne disease caused by the parasite Leishmania major, typically found in Asia and Africa, whose clinical manifestations range from skin ulcers to systemic disease.45 Antimony compounds, like sodium stibogluconate, are currently the primary treatment in many countries; however, they may cause severe side effects such as cardiotoxicity. In India, sodium stibogluconate has high failure rates due to parasite resistance, and alternative treatments, like liposomal amphotericin B, are unavailable due to cost.46, 47 Thus, novel therapeutics to treat leishmaniasis are needed. An in vitro study showed that honey reduces the number of promastigotes of the Leishmania major parasite and the number of amastigotes in infected macrophages compared to a control. An in vivo study indicated that topical honey treatment on mice with an induced leishmaniasis lesion decreased the wound diameter and improved the ulcer.48 However, in a clinical trial of 100 patients with ulcers caused by Leishmaniasis, those treated with honey-soaked dressings had fewer healed lesions than those not receiving the dressing, although this difference was not statistically significant. Honey may have efficacy in treating cutaneous leishmaniasis, and further studies are needed to clarify the benefit.49
Conclusion
Honey has been employed for centuries to treat a variety of ailments. Today, its antimicrobial properties are vital due to the rise in antimicrobial resistance. Because of multiple antimicrobial components and properties, resistance to honey is unlikely. In addition, other characteristics of honey, including low pH, low water content, and peptides, make it an excellent wound-healing treatment. Honey shows promising results in case reports and clinical trials for ailments due to resistant bacterial and fungal infections, herpes lesions, photodamage, intertrigo, burns, foot ulcers, and other rare wounds. Medical-grade honey is available in many forms and has diverse applications. Practitioners may consider availability and formulation when choosing a product for their patients. In summary, honey is an easily accessible, low-cost, natural product with minimal to no cosmetic or clinical side effects that can be used worldwide to replace other, more expensive treatments or when other treatments are inaccessible. Honey and other natural products should be considered in the treatment of wounds, especially when other treatments are costly or unusable due to microbial resistance.