Present status and future directions: Surgical extrusion, intentional replantation and tooth autotransplantation
Abstract
Surgical extrusion, intentional replantation and tooth autotransplantation procedures are important treatment options that clinicians may consider performing in their day-to-day clinical practice. Despite compromised teeth are generally considered for extraction, clinicians must be aware that these cases could be suitable for management by these alternative predictable treatment options. Surgical extrusion, intentional replantation or tooth autotransplantation have similar treatment protocols which includes atraumatic tooth extraction, visualisation of the root portion and replantation. Surgical extrusion is defined as the ‘procedure in which the remaining tooth structure is repositioned at a more coronal/supragingival position in the same socket in which the tooth was located originally’. Intentional replantation is defined as the ‘deliberate extraction of a tooth and after evaluation of root surfaces, endodontic manipulation and repair, placement of the tooth back into its original position’. Tooth autotransplantation is defined as the ‘transplantation of an unerupted or erupted tooth in the same individual, from one site to another extraction site or a new surgically prepared socket’. The same team previously published a narrative review (International Endodontic Journal. 2020, 53, 1636) and European Society of Endodontology position statement (International Endodontic Journal. 2020, 54, 655) on this topic in International Endodontic Journal. The aim of the current updated review was to provide the reader a complete overview and background on these procedures, to established clear clinical protocols and step-by-step for technically perform these therapies in their clinical practice and to establish future directions on the topics. The clinicians must periodically update their knowledge about these three procedures to achieve success.
BACKGROUND AND OVERVIEW
Surgical extrusion
Surgical extrusion is considered as a treatment of last resort for unrestorable teeth with fractures or carious decay of the crown in proximity to the bone level (Kelly et al., 2016). This surgical approach, also referred to as intra-alveolar transplantation, involves the intentional repositioning of the remaining root portion within the socket to a more coronal position to obtain sufficient ferrule and restorability (Das & Muthu, 2013; Kahnberg, 1985).
Complete extraction from the socket may be performed to evaluate the integrity of the root structure before replantation and to detect potential additional fractures that would preclude any attempt to preserve the affected tooth. The success of surgical extrusion therapy is mainly based on a minimal invasive extraction with minimal damage to the cementoblast layer on the root surface (Oikarinen et al., 1996). Surgical extrusion treatment outcome is considered successful when periodontal healing is present, without root resorption or ankylosis. Nevertheless, in patients who have achieved physical maturity, ankylosis may be considered as an acceptable outcome, as root resorption in such cases progresses slowly and does not lead to significant infraposition and arrested alveolar bone growth, as would occur in a patient still in the phase of active growth (Krug et al., 2018b). However, age did not seem to have an impact on the results (Krug et al., 2018a). A favourable outcome also includes the presence of a stable marginal bone level without significantly increased tooth mobility (Elkhadem et al., 2014). Two systematic reviews, including most of the clinical studies that evaluated the success rates of surgical extrusion over the last four decades, have concluded that this treatment should be considered an important technique for managing teeth with subgingival fractures or caries (Das & Muthu, 2013; Elkhadem et al., 2014). These reviews have also demonstrated good periodontal healing and maintenance of marginal bone height and rare signs of ankylosis and root resorption.
Published in 1978, the first case report of surgical extrusion, described the exposure of the apical third of a tooth with a subgingival fracture by removing the bone to gain access to the tip of the root (Tegsjo et al., 1978). The root was luxated with a special crown remover that was placed at the apex in order to move the root coronally to the desired position using only axial forces. Subsequently, Tegsjo et al. (1987) and Kahnberg et al. (1982) reported a positive outcome of a case series. However, concerns over possible apical root resorption resulting from the rather invasive technique were raised and the need for bone transplants to support the root and prevent relapse was questioned (Kahnberg, 1985).
Further clinical studies demonstrated a lower incidence of apical root resorption extrusion by using a simplified extraction technique consisting of careful root mobilization using elevators and cutting of marginal periodontal fibres with a sharp carver, but with no apical bone transplant (Caliskan et al., 1999; Kahnberg, 1985, 1988, 1996; Warfvinge & Kahnberg 1989). The histologic evaluation of the root surfaces in dog teeth showed functional repair with normal periodontal ligament (PDL) and no ankylosis after 120 days (Kim et al., 2009).
Furthermore, an animal study in monkeys showed that, when using forceps for extraction with only rotational movements to reduce the risk of root resorption, mechanical damage to the PDL could not be entirely avoided. This is particularly relevant in cases with reduced coronal tooth structure, such deep fractures (Oikarinen et al., 1996). Since root cross-sections rarely depict circular cross-sections, and corner surfaces of the root are more compressed during tooth removal, cementoblast loss and root resorption occur in these specific areas. A histometric analysis showed that conventional forceps cause significantly more cementoblast loss than instruments specially designed for vertical tooth extraction (Oikarinen et al., 1996).
Minimally invasive vertical tooth extraction techniques enable the extraction of badly damaged teeth without the need for flap surgery and to reduce the extent of alveolar bone resorption (Hong et al., 2018; Muska et al., 2013; Saund & Dietrich, 2013). Atraumatic extraction systems deliver extrusive forces directed along the long axis of the root and minimizes damaging lateral forces. The first implementation of the minimal invasive approach for surgical extrusion was reported to facilitate the restoration of a severely decayed premolar (Kelly et al., 2016). This technique is also considered a recognized approach for a predictable and minimal invasive extrusion without socket expansion (Dietrich et al., 2019). A recent clinical study demonstrated successful vertical extrusion of 51 severely compromised teeth that would otherwise have been considered as unrestorable (Krug et al., 2018a). Even though surgical extrusion is considered a feasible treatment approach for unrestorable teeth, a balanced risk–benefit analysis, including other alternatives such as surgical crown lengthening or orthodontic extrusion (forced eruption), is recommended.
Intentional replantation
Intentional replantation is a procedure that involves the extraction of a tooth, followed by assessing the root surfaces, endodontic manipulation and repair, placing the tooth back into its original socket (Bender & Rossman, 1993; Grossman, 1966). It differs from surgical extrusion as the tooth is placed at the same bone level as it was before extraction without repositioning it more coronally. Intentional replantation is a treatment option for various situations, like failed non-surgical root canal treatment and apical microsurgery, perforations and external root resorption, teeth with crown-root fracture, periodontally compromised teeth and periodontal defects due to radicular grooves and cases in which the patient cannot afford longer and/or more expensive treatments (Mainkar, 2017). Favourable conditions exist for single-rooted teeth where extraction may be performed without major damage to the root surface and without the risk of fracture. However, all precautions must be taken to prevent the root surface from drying out during the extra-oral manipulation.
Current advancement in apical microsurgery have provided solutions to some of the limitations of non-surgical root canal treatment (Chércoles-Ruiz et al., 2017). Nevertheless, some cases cannot be treated adequately with apical microsurgery, due to the surrounding anatomic structures (i.e., closeness to the mental nerve or maxillary sinus) and the difficult accessibility of certain sites such as the palatogingival groove. Hence, intentional replantation provides a solution with fewer complications for such scenarios (Choi et al., 2014; Garrido et al., 2016). Another key factor that must be considered is the patient's financial restrictions for conventional implant placement (Grzanich et al., 2017), leaving intentional replantation as a more cost-efficient way to preserve a natural tooth.
Intentional replantation has also been used as a method that allows extra-oral bonding of teeth with vertical root fractures (Hayashi et al., 2002, 2004; Nizam et al., 2016; Okaguchi et al., 2018; Rosen et al., 2018; Sugaya et al., 2016). It has also been used as a treatment option to treat teeth considered as having a periodontally poot prognosis (Hou et al., 2016; Saida et al., 2018; Solakoglu & Filippi, 2017).
The main advantage of this procedure is that the inaccessible areas of the tooth surface, can be directly viewed and repaired without damaging the adjacent periodontal tissues. However, many practitioners consider this as a last option, because of the possible damage to the PDL and the attendant consequences for external root resorption. The most recent published literature on this topic reports an extremely favourable clinical outcome, that is highly encouraging (Asgary & Roghanizadeh, 2018). Wu and Chen (2021) reported that intentional replantation procedure performed with the use of Emdogain to cover the root surface in certain patients, was a viable treatment of choice with 82.8% survival rate at four years. A systematic review with meta-analysis showed that survival rates of intentionally replanted teeth was approximately 90% (Torabinejad et al., 2015). As a consequence, when surgical/non-surgical retreatment is not feasible, intentional replantation is an alternative, reliable and cost-effective procedure (Mainkar, 2017).
Tooth autotransplantation
The principal indications for tooth autotransplantation procedure includes impacted or ectopic teeth, premature and/or traumatic tooth loss and tooth loss due to tumour or to iatrogenic reasons. This technique is equally viable for congenitally missing teeth in one arch combined with arch length discrepancy or clinical signs of tooth crowding in the opposite arch, replacement of teeth with poor endodontic and restorative prognosis, as well as cleft lip and palate and/or developmental dental anomalies (Almpani et al., 2015; Chung et al., 2014; Tsukiboshi, 2002). Therefore, autotransplantation could be considered as a versatile technique that can be used for several indications both in adolescents and in adults.
Distinct to the immovable osseointegrated dental implant, which impedes alveolar development in growing patients, autotransplanted teeth ensure vital periodontium and are compatible with the eruption process of adjacent teeth (Gilijamse et al., 2016; Park et al., 2010; Plakwicz et al., 2013). The long-term prognosis of tooth autotransplantation, principally with an immature donor tooth, is comparable to that of dental implants (Chung et al., 2014; Kafourou et al., 2017; Tsukiboshi, 2002). Studies on replanted and transplanted teeth have reported that immature young teeth have sufficient blood supply and stem cells to promote pulp revascularization following transplantation (Almpani et al., 2015; Atala-Acevedo et al., 2017; Kafourou et al., 2017; Kumar et al., 2013). This process takes place due to the growth of vascularized connective tissue into the pulp space or the anastomosis of both transplanted tooth blood vessels and periodontal blood vessels (Skoglund & Bjercke 1978, Skoglund & Tronstad, 1981). Pulp revascularization promotes continuous root development and tooth vitality. In addition, autotransplantation maintains the natural shape of attached gingiva, resulting in a good aesthetics (de Freitas Coutinho et al., 2021; Jang et al., 2016a). In the light of these benefits, autotransplantation of immature teeth is often the treatment of choice in young patients (Czochrowska et al., 2002; Mejàre et al., 2004).
There have also been reports of high success rates in mature teeth; consequently, autotransplantation procedure has become an additional treatment of choice in current rehabilitation strategies (Bae et al., 2010; Sugai et al., 2010; Yu et al., 2017). Although pulp healing would not be an expected healing outcome, periodontal healing should not be compromised while transplanting teeth with complete root development. Chung et al. (2014) reported that the projected 1- and 5-year survival rates of mature autotransplanted teeth were 98.0% and 90.5% respectively. Most of the adult donor teeth have a closed apex, which requires root canal treatment before, during or after transplantation procedure (Chung et al., 2014).
Favourable PDL healing is the key factor for success, regardless of whether teeth are mature or immature (Tsukiboshi, 2002). The PDL not only aids bone induction and prevents severe complications, such as replacement root resorption, but also allows the possibility of performing subsequent orthodontic tooth movement (Jonsson & Sigurdsson, 2004; Tsukiboshi, 2002). A traumatic extraction or trauma caused by inadequate socket preparation at the recipient site may mechanically damage PDL cells of the donor tooth, resulting in gradual root resorption. The PDL cells can also be bio-chemically damaged due to various extra-oral conditions, such as variable pH, osmotic pressure, dehydration (Andersson et al., 1989; Andreasen, 1981; Andreasen et al., 1995; Patil et al., 1994), making extra-alveolar time before placement into the new site an important prognostic factor of success.
The fabrication of a 3D tooth replica and 3D-printed guiding templates contribute to reducing possible mechanical damage to the PDL during extraction, reduce the extra-oral time of donor tooth, improve surgical preparation of the recipient site and reduce the potential damage to the PDL of the donor tooth (Anssari Moin et al., 2017; Lee et al., 2001; Strbac et al., 2016). Surgical planning software allows the clinician to select the most appropriate donor tooth according to tooth anatomy, design the ideal position of the donor tooth in 3D and calculate the required dimensions of the alveolus during surgery. In addition, the use of tooth replicas reduces the additional extra-oral socket time and reduces the number of fitting attempts before an optimum fit is obtained (Lee et al., 2001; Lee & Kim, 2012; Oh et al., 2018; Strbac et al., 2016), minimizing the chances of iatrogenic damage to the PDL (Anssari Moin et al., 2017). Recently, Strbac et al. (2020) presented a surgical technique using virtually preplanned 3D-printed templates for guided osteotomies to ensure a guided atraumatic approach and facilitate highly complex treatments.
When planning the ideal 3D position of the donor teeth for a successful transplantation, a sufficiently large recipient site is crucial (Kafourou et al., 2017; Tsukiboshi, 2002). However, conditions at the recipient site are not always optimum and may vary depending on when the tooth was lost (Zufía et al., 2017). In cases of transplantation to a fresh extraction site immediately after extraction of the hopeless tooth, sufficient bone is usually available (Lundberg & Isaksson, 1996; Mejàre et al., 2004). In cases of previous extraction with partial or complete regeneration of the alveolar socket, an adequate recipient site can usually be surgically created (Conklin, 1974; Yu et al., 2017).
The current evidence recommends autotransplanted teeth with complete/ incomplete root formation have favourable survival and success rates with less complications (Chung et al., 2014; Rohof et al., 2018). Various clinical studies have reported 80%–100% of survival rate (Almpani et al., 2015; Borring-Møller & Frandsen, 1978; Chung et al., 2014; Hernandez & Cuestas-Carnero, 1988; Kristerson, 1985; Kristerson & Lagerström, 1991; Kugelberg et al., 1994; Plotino et al., 2020; Rohof et al., 2018; Schatz & Joho, 1992; Slagsvold & Bjercke, 1978).
CLINICAL TECHNIQUES AND MATERIALS CURRENTLY AVAILABLE
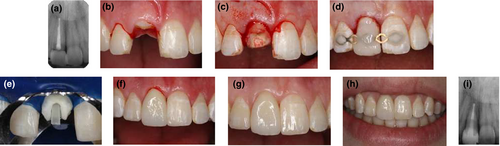
Surgical extrusion (Figure 1)
Surgical extrusion is indicated in single-rooted permanent teeth with fractures or carious decay of the crown in proximity to the bone level, irrespective of the patient age. In general, after extrusion, the root should be long enough to provide adequate alveolar support and a favourable crown-to root ratio (Penny & Kraal, 1979). However, in special cases even the extrusion of short roots may be regarded as a success if temporary tooth preservation helps to postpone a dental implant until adulthood. Before treatment the patient or the legal guardian should be provided with specific information regarding the clinical procedure as well as the treatment alternatives.
Any carious dentine must be removed to assess the remaining tooth structure and to determine the intended amount of extrusion. After local anaesthesia, the gingival fibrous attachment is incised using a scalpel blade. During mobilization of the root, utmost care should be taken to avoid extensive mechanical damage of the root surface. In particular, the elevators should be used with gentle pressure. The cervical portion of the tooth can be grasped with a forceps using rotation movements. Preparation of a circumferential groove between the root and the surrounding bone with a tapered-point diamond rotary instrument may be considered to enable a firm grip of the forceps on the root (Angerame et al., 2021). For difficult cases a vertical extraction device can be recommended for an atraumatic extraction of the root (Dietrich et al., 2019). This can be the case when long roots such as canines need to be extruded and the use of elevators and forceps is not feasible due to completely missing coronal tooth structure. Furthermore, extraction in older patients appears more challenging than it is in children and adolescents due to a higher density of the alveolar bone and a decrease in the PDL space with age (Van der Velden 1984).
The clinical application of the Benex vertical extraction system (Benex; Helmut Zepf Medizintechnik GmbH) has been described in detail recently (Dietrich et al., 2019). Briefly, a screw hole is prepared in the root canal orifice with a diamond-coated drill. A matching self-tapping screw is anchored in the prepared root canal and connected to the extractor with a flexible pull rope. The extraction force is increased by slowly turning the handle of the extractor clockwise until rupture of dento-alveolar fibres will typically be indicated by mild bleeding from the sulcus and a drop in the tension in the pull rope. When the desired coronal position of the root is achieved, the screw is removed. Careful, visual inspection of the exposed root is highly recommended in order to detect any additional fractures.
Even though surgical extrusion with the Benex extraction system seems to fully prevent progressive root resorption and ankylosis, removal of sound hard tissues during preparation of the screw hole and a risk of perforation that cannot be completely ruled out may be regarded as possible drawbacks (Krug et al., 2018a). Further, insertion of the screw may induce dentinal cracks, thus potentially limiting the long-term prognosis of the tooth.
A typical indication for surgical extrusion is the management of teeth with crown-root-fractures. In maxillary anterior teeth, crown-root-fractures have a typical fracture line: on the labial side, the fracture is localized paragingivally or supragingivally, while palatally the defect often extends into the infraosseous root region. In contrast, the bone level of the alveolar process in the upper anterior region is more coronally on the palatal side compared to the labial side. For that reason, rotation of the root by 180 degrees before replantation is ideal to expose the defect margin on both aspects while minimizing the extrusion distance at the same time (Krastl et al., 2011). In case of surgically extruded maxillary premolars, rotation of the tooth by 180° did not seem to affect the clinical outcome (Choi & Lee, 2019).
A flexible splint allowing physiologic tooth mobility is applied to reduce the risk of ankylosis (Kahler et al., 2016). Due to mismatch between the socket and the extruded root the splinting period may be longer than that after replantation of avulsed teeth and can be extended up to 6 weeks, particularly in cases of high mobility of the extruded root (Kelly et al., 2016; Mohamed et al., 2021). Endodontic treatment should be initiated in accordance with the treatment of avulsed teeth within the first 2 weeks after replantation to avoid infection-related root resorption (Fouad et al., 2020; Krastl et al., 2021b). Within the first week, calcium hydroxide should be avoided as an intra-canal dressing due to a possible negative impact on periodontal healing if placed immediately after replantation (Lengheden 1994; Lengheden and Jansson 1995). An antibiotic-corticosteroid paste such as Odontopaste (Australian Dental Manufacturing) is a good alternative since it may be placed following replantation and additionally acts as an anti-inflammatory and anti-clastic intra-canal medicament (Krastl et al., 2021a). The more commonly available Ledermix (Riemser) may cause discoloration of the teeth, which will have aesthetic implications. Extra-oral root canal treatment is usually not recommended because manipulation under dry conditions is likely to interfere with PDL cell viability and increase the risk for root resorption (Andreasen, 1981). However, in case of surgical extrusion of root-filled teeth, apicoectomy with retrograde sealing of the root canal may be considered.
Restorative treatment is usually performed 6 to 8 weeks after surgical extrusion. If crown placement is indicated, a biologically oriented preparation technique, as recently described, may be helpful to achieve an improved gingival architecture and greater long-term soft-tissue stability (Llaquet Pujol et al., 2021). Although systemic antibiotics were prescribed in some clinical reports on surgical extrusion, there is insufficient evidence to support or reject their use.
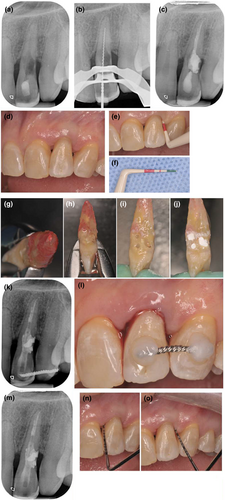
Intentional replantation (Figures 2 and 3)
A pre-operative CBCT can help in assessing the root anatomy (Akhlef et al., 2018; Shahbazian et al., 2010; Verweij et al., 2017). Whenever necessary it is recommended to perform the orthograde endodontic treatment before starting the intentional replantation procedures; this will help to get an affordable seal surgically, while performing intentional replantation procedure. A systematic review reported that systemic antibiotic prophylaxis (e.g. amoxicillin/clavulanic acid) might reduce the failure rate after intentional replantation (Chung et al., 2014).
It is recommended to perform local debridement of plaque and calculus before the surgical treatment (Becker, 2018). After local anaesthesia, an atraumatic extraction should be performed, thus avoid damaging the PDL cells present in the coronal portion of the root surface. Krug et al. (2019) reported that the use of atraumatic extraction has improved the outcome of intentional replantation in teeth with extensive cervical root resorption. To avoid damaging the gingival fibres, a sterile gauze can be placed on the tooth under the beaks of the extraction forceps. A rubber band on the forceps handle may help in securing this step (Kratchman, 1997). While performing extra-oral procedures a protection of the blood-filled socket with sterile gauzes could be used to reduce the contamination in the site (Cho et al., 2016). Before starting the extra-oral procedures on the extracted tooth, it is recommendable to have a visual inspection under microscope to find the presence of anatomical variations, accessory portals of exit or cracks (Choi et al., 2014; Jang et al., 2016a, 2016b; Kratchman, 1997; Niemczyk, 2001). In case, any doubts regarding the anatomical complexities can be cleared using methylene blue dye.
During the entire extra-oral procedures, the root surface must be wet, using sterile saline solution or Hank's balanced salt solution (HBSS) (Niemczyk, 2001). The total extra-oral time of manipulation is an important parameter for the long-term prognosis of the treatment, to avoid damaging the PDL and reduce the incidence of root resorption and ankylosis (Hupp et al., 1998). Lower survival rates were observed when the extra-oral time was more than 15 min (Jang et al., 2016a, 2016b).
Intentional replantation procedure can be performed to save the teeth with failed non-surgical root canal treatment. The procedure involves extra-oral retrograde filling of the root canal. In this procedure, apical one third (2–3 mm) of the root should be resected. The extra-oral orthograde root canal treatment improves the technical quality of the root canal filling. However, this procedure is recommended for highly selected cases since it can extend the extra-oral time and expose the root surface to the chemical risk due to the usage of irrigating solution.
After the apical root resection, a root-end preparation should be performed to ensure tight apical seal (Jang et al., 2016b). The root-end preparation is performed using a thin (0.5 mm tip) cylindrical, cut ended, diamond-coated or carbide high-speed bur (Deeb, 1971; Fegan & Steiman, 1991). The use of sonic or ultrasonic tips are also recommended, if the root is extremely thin (Cho et al., 2016). A retro cavity preparation should be performed under copious irrigation with sterile saline and extended to a depth of 3 mm (Becker, 2018).
Several retro-filling materials have been used such as amalgam, gutta-percha, zinc-oxide based materials and Mineral Trioxide Aggregate (Choi et al., 2014). Modern calcium silicate-based materials with different consistency and physical properties could be considered to be the materials of choice (Giacomino et al., 2019; Leal et al., 2013). The radiopacity and the setting time of the material should be considered as relevant factors while selecting the material (Khalil et al., 2016). Socket curettage is not recommended by several authors (Asgary et al., 2014; Cho et al., 2016; Kratchman, 1997). However, curettage can be performed gently when a periapical granuloma or extruded filling materials need to be removed. Once blood clot is removed, the tooth should be reinserted in the socket with digital pressure and the occlusion carefully checked (Becker, 2018). The replanted tooth should be immobilized using a flexible splint for a minimum period of 2 weeks. Alternatively, in posterior teeth, a crossed suture may be suspended above the occlusal surface with or without the use of resin composite to fix the suture to the tooth surface. The occlusion has to be relieved from occlusal contacts (Asgary et al., 2014; Becker, 2018; Choi et al., 2014; Jang et al., 2016b).
When the root canal treatment has not been performed before replantation, as described above, it is crucial to initiate orthograde endodontic treatment within 14 days from the replantation; even when apicoectomy and retrograde filling are performed extra-orally, an early root canal treatment after the surgical procedures increased the success rate of the intentionally replanted teeth (Chung et al., 2014). Necrotic pulp tissue inside the replanted tooth may induce a periapical lesion of endodontic origin or an infection-related root resorption (Bae et al., 2010; Tsukiboshi, 2002).
Intentional replantation also offers a suitable treatment option for teeth with inaccessible cervical resorptions. During this procedure, the granulation tissue within the defect is curetted to avoid recurrence. Depending on where the resorption is located in relation to the alveolar crest, glass-ionomer cements, composites or fast setting calcium silicate-based materials are the materials of choice to restore the cavity (European Society of Endodontology developed et al., 2018).
Teeth with vertical root fractures are traditionally deemed non-treatable. However, intentional replantation with extra-oral fragment bonding using a 4-methacryloxyethyl trimellitate anhydride/methacrylate-tri-n-butyl borane (4-META/ MMA-TBB) resin cement has been recommended to manage and maintain such teeth (Rosen et al., 2018). Two case series presented promising short term but unfavourable long-term data (Hayashi et al., 2002, 2004; Nizam et al., 2016). Thus, the treatment of teeth with vertical root fractures must still be regarded as unfeasible.

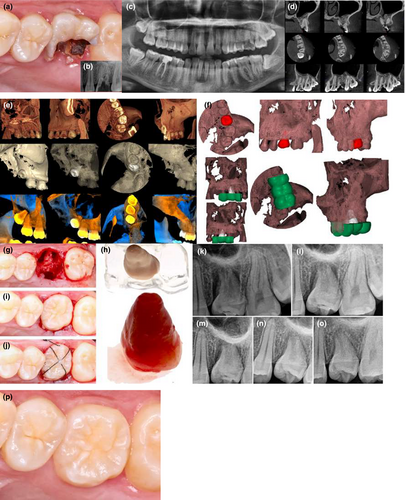
Tooth autotransplantation (Figures 4 and 5)
Despite the lack of evidence, the clinician should consider prescribing oral systemic antibiotics a few hours before the procedure to prevent bacterial infection from extra-oral and intra-oral sources. In children where the transplants are usually placed under general anaesthesia, a single dose of an antibiotic adjusted according to the weight of the child, can be administered intravenous by the anaesthetist after induction of general anaesthesia.
Teeth should be cleaned before surgery and surgical sites must be disinfected. The donor tooth and the recipient site have to be anaesthetized at same time. In donor tooth with immature root, revascularization can be expected after transplantation, hence local anaesthetic solution without vasoconstrictor should be preferred.
During the extraction of the tooth to be replaced, the dentist must be careful not to damage either the buccal or the lingual/palatal cortical plate surrounding the tooth. Extraction is relatively free from risk of root fractures, especially in children, who have immature teeth with incomplete roots. Therefore, placement of sterile gauge on the donor tooth to be extracted, under the beaks of the extraction forceps, can minimize injury to the gingival fibres around the neck of the tooth.
In some cases, there are patients with certain conditions such as congenitally missing teeth or with early tooth loss, in which the recipient site for autotransplantation needs to be created surgically (Yu et al., 2017). With modern instrumentation used for placement of implants this is relatively an easy procedure. Anssari Moin et al. (2017) described a method of computer-assisted template-guided autotransplantation with custom 3D designed/printed surgical tooling that may possibly offer an alternative and more precise method for socket preparation.
To make sure that the donor tooth is not inserted with undue pressure, the recipient site should be larger according than the 3D dimensions of the tooth replica. The tooth replica is optimally positioned in the recipient site as digitally planned. The donor tooth should be extracted atraumatically and then compared to the tooth replica for shape and size. It is preferable to make an intra-crevicular incision before luxation to preserve as much PDL as possible. As soon as possible the donor tooth is placed in the recipient site in slight infraposition, leaving it free from occlusal and articulation forces.
In the case of sufficient transplant stability, post-operative fixation is carried out with a suture crossing the occlusal surface, leaving the site left to heal for 7 days. In case of inadequate stability and in children and adolescents, a buccal composite and flexible wire splint, to confirm the physiological mobility of the transplant, is applied for 4 weeks. Occlusal adjustment can be repeated after placing the splint. To achieve a tight fit around the donor tooth, it is recommended to trim the flap and suture it before placing the donor tooth in the socket. Some authors such as Tsukiboshi (2002) recommend the use of a surgical dressing to protect the transplant against infection during the first 2–3 days of healing, although the authors do not recommend this as it could prevent access to the area for effective plaque removal, thereby possibly compromising healing of the gingival fibres.
A radiograph might be taken before splinting to corroborate the position of the donor tooth in the recipient socket, although this is not usually required. Having observed that the position is adequate, the clinician will can place the splint if this is required.
After tooth transplantation, root apex closure and positive response to electric pulp tests are expected if the donor tooth had an immature root or an incomplete root development and revascularization is expected to occur. However, these might not be possible in the first few months after the procedure. In case of any signs or symptoms of pulp pathology like irreversible pulpitis or inflammatory root resorption, the clinician has to initiate the root canal treatment immediately.
In teeth with mature roots, if the donor is accessible, the root canal treatment can be completed before surgery. However, if the donor is impacted or erupted in a position that makes endodontic access difficult, non-surgical root canal treatment should be started before splint removal at 2 weeks post-surgery. The clinician can opt to complete the endodontic treatment in the same visit or place an interim dressing of calcium hydroxide in the root canal system. An alternative option is to perform the root canal treatment extra-orally at the time of transplantation; however, this is not recommended during the procedure because there is a clear risk of damage to PDL and extend the extra-oral time.
Once the splint is removed, the transplanted tooth should be allowed to settle naturally into its new position; however, it is adviceable to periodically check the occlusion. According to the aesthetics and function of the tooth, restorative treatment can be performed.
On many occasions, especially in growing patients, tooth autotransplantation may be part of a global orthodontic treatment. However, no studies have been carried out as to whether orthodontic forces affect the success and/or survival rate of the autotransplanted teeth (Rohof et al., 2018). As transplanted teeth are considered as any traumatized tooth with a PDL injury, any planned orthodontic movement of the transplanted teeth should be delayed for 6 months after surgery (Day et al., 2008; Kindelan et al., 2008).
The teeth should be re-evaluated as often as is done with the other teeth. It is important to inform the patient that the transplanted tooth is subject to the same risks as those of any other natural tooth.

FUTURE DIRECTIONS
Although the described methods, surgical extrusion, intentional replantation and autotransplantation, have been used clinically for decades, they share a limited level of evidence. For unrestorable teeth, intended for extrusion, comparative data addressing both orthodontic and surgical extrusion are highly desirable. So far only one animal study is available, which demonstrated that a functional periodontal ligament was restored irrespective of the extrusion modality (Kim et al., 2009). However, comparative clinical studies are needed to generate evidence on which approach is more likely to maximize both the long-term survival and the aesthetic outcome of the affected teeth.
In general, clinical studies must focus more on the study design with adequate sample size, long-term follow-ups and possible factors influencing the outcome of these procedures. Multi-centre clinical studies can help the researchers to achieve higher sample sizes, an important drawback in many studies is a small sample. Studies on quality of life and cost effectiveness of these three procedures are also needed. The overall satisfaction should be compared to the assessment done by the professionals, as professionals may be more critical than patients regarding the assessment of the aesthetic aspects of autotransplanted teeth.
Future studies are required to investigate whether orthodontic forces affect the success or survival of extruded or replanted teeth as well as the role of CBCT planning and use of 3D tooth replicas. It should also be further verified if preapplication of orthodontic force may be beneficial for the extraction phase in all these procedures, as it may increases PDL width, which induces tooth mobility, helping atraumatic extraction and PDL healing (Choi et al., 2014; Suzaki et al., 2008).
If the tooth autotransplantation or replantation cannot be undertaken immediately after the extraction of the recipient tooth, due to severe damage to the alveolar bone or to a previously extracted donor tooth, the cryopreservation systems could possibly be used to store donor teeth for a long period (Kaku et al., 2015). Teeth extracted due to orthodontic reasons or impacted third molars are most suitable for cryopreservation and future transplantation (Osathanon, 2010). Mechanical properties like cracks of cryopreserved tooth are important after autotransplantation, for which randomized clinical studies are needed to obtain more evidence on masticatory function and periodontal healing of transplanted cryopreserved teeth (Kaku et al., 2010).
The use of growth factors provided by platelet-rich plasma might have helped to maintain the vitality of the transplanted teeth, promote root formation and neurosensory development. Researchers are encouraged to conduct multi-centre randomized clinical studies to investigate the role of such different types of plasma and/or growth factors.
During tooth autotransplantation, the recipient socket must have enough alveolar supporting buccal and palatal/lingual plates to accommodate the donor tooth and the clinician must ensure that the flap in the cervical area is tightly repositioned (Imazato & Fukunishi, 2004). Post-transplantation, studies have shown rapid bone regeneration and the emergence of lamina dura, such that bone graft materials are unnecessary between bone walls and transplant roots even in a wide space (Inoue et al., 1988, Inoue et al., 1990). However, cases have been recorded in which the width of the root of the transplanted tooth is greater than the width of the recipient site, leading to root protrusion though bone dehiscence. In these situations, clinicians can place graft materials over the exposed root to promote bone regeneration, or they can rotate or resect one or more roots to fit into the socket (Yu et al., 2017). Guided tissue regeneration (GTR) or autogenous bone graft effects appears to be based on maintaining space for osteoblastic cells by excluding contact between gingival connective tissue and PDL (Imazato & Fukunishi, 2004). In patients with inadequate bone support, outcome of transplantation of teeth including GBR or GTR procedures or transplantation of teeth with cortical bone plates attached should be investigated (Zufía et al., 2017).
Because revascularization rates of mature teeth are significantly low, endodontic treatment is the standard procedure to avoid pulpal necrosis with subsequent periapical inflammation and inflammatory root resorption (Bae et al., 2010; Lundberg & Isaksson, 1996; Schwartz et al., 1985; Tsukiboshi, 2002). However, some studies (Skoglund & Tronstad, 1981; Skoglund et al., 1978) and published clinical cases (Gaviño Orduña et al., 2020; Jakse et al., 2018) have demonstrated that an extra-oral apicoectomy could enlarge the foramen of the transplant and achieve higher rates of revascularization. The critical diameter of the apical foramen of the transplanted tooth is considered to be 1 mm for successful revascularization (Andreasen et al., 1990). Raabe et al. (2021) concluded that extra-oral root-end resection of mature transplants may lead to higher rates of revascularization and post-operative pulp canal obliteration than those reported on unmodified mature transplants. However, prospective controlled clinical studies on extra-oral apicoectomy are needed to corroborate these results, and currently this is not a recommended clinical practice due to the risk of damage to the PDL while performing such procedures.
| Procedure | Definition |
|---|---|
| Surgical extrusion | Intra-alveolar transplantation to make unrestorable teeth restorable through intentional coronal displacement of the remaining root within the socket (Tegsjõ et al., 1978). |
| Intentional replantation | Surgical procedure to primarily treat inaccessible endodontic or resorptive lesions through intentional atraumatic extraction, extra-oral repair and subsequent reinsertion of the tooth into the extraction socket (Bender & Rossman, 1993). |
| Tooth autotransplantation | Surgical procedure to replace hopeless teeth through transfer of an impacted or erupted tooth from a donor site to an extraction or surgically prepared recipient site (Natiella et al., 1970). |
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this manuscript.
AUTHOR CONTRIBUTIONS
All the authors have made substantial contributions to the manuscript. All the authors of this manuscript have read and approved the final version of the manuscript.
ETHICAL STATEMENT
Ethical approval was not acquired as this article does not contain research that involved any human or animal experiments.