Home setting after stroke, facilitators and barriers: A systematic literature review
Abstract
This paper seeks to improve the understanding of the interaction between patients with stroke and the physical environment in their home settings. Stroke care is increasingly performed in the patient's home. Therefore, a systematic review was conducted to identify the existing knowledge about facilitators and barriers in the physical environment of home settings for the stroke rehabilitation process. Based upon Arksey and O'Malley's framework, a Boolean search strategy was performed in the databases; CINAHL, Medline, Web of Science and Scopus. Fifteen articles were retained from the literature search conducted between August and November 2016, and two researchers independently assessed their quality based on the Swedish Council on Health Technology Assessment guidelines. The results suggest that despite the healthcare system's ongoing shift towards home-based rehabilitation, the role played by the physical environment of home settings is still considered a side finding. Moreover, the research appears to focus mainly on how this environment supports mobility and activities of daily living, whereas information regarding the psychosocial and emotional processes that mediate the interaction between stroke survivors and their home setting are missing. A lack of information was also found with regard to the influence of different geographic locations on the stroke rehabilitation process. Future investigations are therefore needed to advance the understanding of the role played by the physical environment of home settings in supporting stroke recovery.
What is known about this topic
- It is challenging for healthcare services to meet the needs of patients within the community.
- Stroke care is increasingly performed within home settings.
- A lack of knowledge about the interaction between the physical environment of home setting and patients with stroke is suggested.
What this paper adds
- It advocates that there is a lack of studies focusing on the physical environment of home settings; existing knowledge is mainly side findings.
- Moreover, it is studied exclusively in terms of how well it supports mobility and daily life activities after stroke.
- No information regarding the psychosocial processes and emotional attachment that mediate the interaction between home settings and stroke rehabilitation is found.
1 INTRODUCTION
Healthcare delivered at home is a rapidly emerging sector. It is central to healthcare reforms worldwide due to the growth of the elderly population, which faces complex health conditions (OECD, 2003; Swedish Council on Health Technology Assessment, 2014, 2015; WHO, 2015a, 2015b). Although acute stroke care is delivered in specialised stroke units with short stays, stroke care is increasingly performed in the patient's home setting (SOU, 2016). It is challenging for society and healthcare services to meet the needs of patients at home. These challenges include not only organising care delivery but also designing houses and neighbourhoods in the community to support patients receiving health services, e.g. people who have suffered a stroke.
Although the environment (both the built environment and the nearest surroundings) is suggested to be a key factor in the next generation of health reforms (OECD/EU, 2016; OECD, 2017), very little is known about how home settings support people after they have suffered a stroke. We therefore conducted a systematic review to identify the existing knowledge about facilitators and barriers in the physical environment of home settings for the stroke rehabilitation process.
Stroke is one of the most common diseases and a leading cause of disabilities (WHO, 2015a, 2015b). It can lead to major life changes in terms of cognitive and psychological functioning (Whyte & Mulsant, 2002), bodily disabilities (Kvigne & Kirkevold, 2003), profound fatigue (Elf, Eriksson, Johansson, Koch, & Ytterberg, 2016), and restricted independence and participation in community and social activities (Singam, Ytterberg, Tham, & von Koch, 2015). By hindering patients’ ability to return to everyday life activities, stroke episodes create a life course disruption (Ekstam, Uppgard, von Koch, & Tham, 2007) and negatively impact the overall quality of life of stroke survivors and their families (Algurén, Lundgren-Nilsson, & Sunnerhagen, 2009; Bergström, von Koch, Andersson, Tham, & Eriksson, 2015; Haewon & Hyeung Woo, 2016). The goals of stroke rehabilitation are thus to maximise patients’ independence and to provide the best possible life re-orientation to their own environment and community. These goals are challenging for patients due to their post-stroke disabilities and the potential gap between their desired and actual roles, which require them to learn how to live in a changed state and with a new sense of identity (i.e. psychosocial recovery) (Roman, 2008; Wade, 1992).
Research has suggested that early supported discharge (ESD) to home settings can influence the health and well-being of survivors of mild to moderate stroke (Fearon & Langhorne, 2012). The beneficial effects of ESD are supposedly associated with the development of a clear rehabilitation plan from the hospital units to the home setting (Nordin, Sunnerhagen, & Axelsson, 2015; Rousseaux, Daveluy, & Kozlowski, 2009) and the establishment of a positive relationship between patients and hospital staff within home settings where patients’ needs can be better acknowledged (Meijer & van Limbeek, 2005).
Moreover, the affective effects of returning home are likely to contribute to positive ESD outcomes because home environments are known to shape people's identities (Twigger-Ross & Uzzel, 1996) and are often perceived to be ‘safe harbours’ from the unknown and demanding outside world (Marcheschi, 2015). These type of interactions are defined within the field of environmental psychology as indirect effects of the physical environment and are known to mediate human–environment interplay. Such effects imply that the environmental stimuli act through psychological processes as a result of sensory perception (Dijkstra, Pieterse, & Pruyn, 2006; Evans, 2003). These effects are often overlooked in research probably because such underlying processes are difficult to measure. However, a number of studies have shown that these type of indirect outcomes such as emotional bonds developed between patients and home and care settings affect their health (Brown & Perkins, 1992; Dijkstra, 2009; Evans & McCoy, 1998). For example, housing facilities for vulnerable groups in society are found to support users’ well-being when the architectural and interior design features sustain social interaction, privacy regulation and restoration possibilities (Marcheschi, 2015). The home setting has been found to facilitate the development of the attachment and identification with a place (Evans, Kantrowitz, & Eshelman, 2002), which in turn has a positive influence on quality of life outcomes (Marcheschi, Johansson, Brunt, Hansson, & Laike, 2015). The feelings of belonging, connectedness and safety that often are related to the home setting (Relph, 1976) are largely acknowledged to support individuals’ restorative functioning (Erikson, Park, & Tham, 2009; Giuliani, 1991). Therefore, home settings are often described as an extension of the self that sustains positive self-image and well-being outcomes (Cristoferetti, Gennai, & Rodeschini, 2011). The emotional bond established between stroke survivors and their home setting is still not largely investigated. However, place attachment could also be considered a central aspect of positive re-engagement with real-life situations among patients with stroke (Nanninga, Meijering, Schönherr, Postema, & Lettinga, 2015).
Studies on stroke rehabilitation have recently shown that enriched environments (EE) with specific physical factors (i.e. tactile features, sensory equipment, music, books and robotic devices) and places specially designed for meetings can enhance patients’ engagement in cognitive and social activities and make them less inactive and isolated (Janssen et al., 2014; White, Bartley, Janssen, Jordan, & Spratt, 2015). These results are supported by animal models that have shown that EE can facilitate brain plasticity and increase functioning, e.g. sensory, motor, cognitive and spatial map responses (Wang et al., 2016).
Yet, one of the major challenges of providing stroke care and rehabilitation within the community (i.e. in ordinary home settings) remains to determine how the physical environment should be designed to best address patients’ needs and health conditions. However, in line with ecological theory (Lawton & Nahemow, 1973), a positive fit between the person and the environment is crucial, as a good fit between individual competences and environmental demands supports well-being-related outcomes. A poor human–environment fit, in contrast, might have negative consequences for rehabilitation processes.
The importance of acknowledging the quality of human–environment interactions for health outcomes is advocated in the framework of The International Classification of Functioning (ICF), which suggests classifying the physical environment as either a facilitator or a barrier for individuals’ participation in major life activities (WHO, 2015a, 2015b). The physical environment can be further conceptualised in three dimensions (Harris, McBride, Ross, & Curtis, 2002): architectural (spatial layout, room size and window placement), interior design (flexible elements of the environment, such as furnishing, devices and artwork) and ambient features (lightning, sounds, noise, temperature and music) (Dijkstra et al., 2006).
A recent report from the OECD (2016) emphasises the importance of providing services and care with a person-centred approach during, and beyond, the transitions from inpatient care units to home settings. This implies that each dimension of a patient's health and well-being are in a continuous interaction with the environment (i.e. physical and psychosocial), the patient's personal characteristics and the patient's overall health conditions. However, the physical dimension of the environment has been overlooked even though environmental psychology research has widely shown that human–environment interactions cannot be fully understood without considering the physical scenario in which rehabilitation activities are performed (Baroni, 1998; Küller, 1991).
Thus, questions remain about what factors in the physical environment of home settings influence stroke recovery and in what ways (Swedish Council on Health Technology Assessment, 2015). The overall aim of this study was to explore, by means of a systematic review, the existing evidence on the interactions between stroke survivors and the physical environment of home settings. The specific aims were to: (1) map the literature addressing the above mentioned human–environment interaction, (2) identify the factors of the physical environment in home settings that stroke survivors experience as barriers and facilitators, especially for activities of daily living and (3) outline a research agenda to address knowledge gaps.
2 METHODS
2.1 Review design
The review procedure was designed in accordance with the literature on systematic reviews (Littell, Corcoran, & Pillai, 2008; Petticrew and Roberts, 2006) and based upon the five-step framework proposed by Arksey and O'Malley (2005). The framework aims to map the main sources of a research area, the key results and the type of evidence available, which implies a back-and-forth process between initial findings and new insights. The study followed the preferred schema for systematic reviews and meta-analysis (PRISMA) (Moher, Liberati, Tetzlaff, & Altman, 2009).
2.2 Search methods and strategy
A systematic review of literature published from 1996 to 2016 was performed in the following databases: CINAHL, Medline, Web of Science and Scopus. A Boolean search strategy was adopted that incorporated truncated search terms and potential synonyms (Table 1). A free search was performed based upon the reference list of the material included, and a manual search was further conducted across those journals with more than one hit on the topic of interest.
| Stroke rehabilitation | AND Physical environment | AND Home |
|---|---|---|
| ORStrokeStroke care | ORArchitectureArchitectural designBuilding designFacility designBuilt environmentEnriched environmentEnvironmental designEnvironmental context | ORHome settingHome-based careHome-based rehabilitationHome facilitiesHome ambiencesHousing environment |
The electronic search was performed by the first author between August and November 2016.
2.3 Search outcomes
All articles that studied the interaction between the physical environment of home settings and patients with stroke and were published in English in peer-reviewed scientific journals were eligible for inclusion.
The inclusion and eligibility of retrieved papers were independently assessed by two of the authors (EM, ME). The screening process involved four steps: (1) an initial selection for inclusion was performed based on the title and abstract, and all duplicates were deleted; (2) abstracts were screened to determine relevance; (3) the full text of relevant papers was retrieved; and (4) full-text copies of the papers were independently evaluated by the researchers to determine whether they fulfilled the inclusion criteria. Disagreement about inclusion was solved by discussion.
2.4 Data screening and quality appraisal
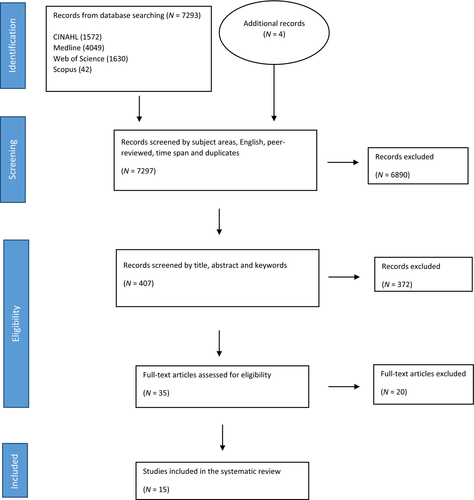
The literature search ended in November 2016 and generated 7,297 hits. These articles were screened by subject relevance (i.e. physical environment, home setting, stroke), and only papers from the past 20 years were included. The authors eliminated non-English sources, duplicates and non-peer-reviewed articles, which resulted in a total of 407 articles. This material was further screened by title, abstract and key words, which left a total of 35 relevant articles. Their full texts were read by two researchers separately to determine eligibility and inclusion in the systematic review. In an attempt to find articles that might have been missed by the search in databases, a manual search was also performed across those journals that had several relevant hits, which resulted in four additional papers.
Of these 39 relevant articles, 15 were deemed eligible for inclusion as they focused on the interaction between the physical environment of home settings and patients with stroke; the other 24 articles were excluded because they did not have that focus.
A quality appraisal of the 15 articles was performed based on the Swedish Council on Health Technology Assessment (2014) guidelines, which provide different grids of evaluations depending on the study design (randomised control trial, empirical studies, qualitative studies and systematic review). In the guidelines quality was defined by the use of the specific grading system “GRADE,” which builds upon experiences from previous systems and emphasises patients benefits and risks (Swedish Council on Health Technology Assessment, 2014). The degree of evidence was based on the reliability, consistency, transferability and precision of the data collected. The assessment was performed independently by EM and ME. In cases of disagreement, which occurred five times, the researchers discussed their views until they reached an agreement. A flow chart of the search is provided in Figure 1.
2.5 Data extraction
A summary of the studies included in the review is provided in Appendix S1 in a data extraction sheet, which indicates the name of the author(s), the publication year, the title and the journal. Appendix S1 also contains information regarding the study design, the methods and procedure, the participants, the settings and the quality appraisal of the research conducted. Information regarding which dimension of the physical environment was studied, the classification of facilitator vs. barrier and the rehabilitation process involved are also reported in Appendix S1.
2.6 Synthesis
A deductive thematic analysis was completed based upon Braun and Clarke's (2006) methodology. The analysis was conducted bearing in mind the classification of the physical environment proposed by the ICF as a facilitator and barrier, which in this study applied to the interaction between patients with stroke and their home settings. Furthermore, the thematic analysis was structured around the three proposed dimensions of the physical environment, i.e. architectural, interior design and ambient features. For each of these physical environment dimensions, the findings were then reported in terms of facilitators, barriers and the type of rehabilitation process involved.
3 RESULTS
The majority of the studies (N = 9) were qualitative case studies, five were cross-sectional investigations, and one was a randomised (controlled) trial. The quality evaluation resulted in seven articles with high-to-medium quality and eight articles with medium-to-low quality (Appendix S1). The articles were published in 12 journals between 1997 and 2016 and addressed different aspects of the interaction between the physical environment of home settings and stroke survivors. Five articles investigated several settings simultaneously (e.g. home, nursing home and community) (Appendix S1, article numbers 1, 4, 7, 13 and 14), whereas the remaining nine focused exclusively on home environments (2, 3, 5, 6, 8, 9, 10, 11, 12 and 15).
Four articles (Appendix S1, numbers 2, 7, 11 and 14) investigated all dimensions of the physical environment (i.e. architecture, interior and ambient features), whereas the remaining 11 focused exclusively on one or two dimensions, either architecture or interior design features. All articles addressed both facilitators and barriers, and overall, they presented a relatively equal number of facilitators and barriers in the environment. However, what was perceived to be a facilitator in some studies was found to be a barrier in others. For example, assistive electronic devices, such as wheelchairs and power wheelchairs, were commonly found to be facilitators of the stroke rehabilitation process (Jellema et al., 2016; Sørensen, Lendal, Schultz, & Uhrskov, 2003; Vincent et al., 2007), whereas other studies found that patients with agnosia, who could not recognise or control such devices, experienced this technology as a barrier (Lampinen & Tham, 2003).
The large majority of studies embraced the theoretical and methodological background derived from social sciences and health-related studies (e.g. nursing and medicine). Approximately half of the studies employed the framework proposed by the ICF (Appendix S1, article numbers 1, 6, 7, 9, 11, 14 and 15), and occupational therapy, which had focus on the development of independence in activities of daily living (1, 2, 5, 6, 8, 9, 10, 11 and 13–15).
3.1 Architectural features
For the environmental dimension of architectural features, accessibility and home adjustments appeared to be the most crucial facilitators for the stroke rehabilitation process in home settings. The articles discussed accessibility in terms of patients’ ability to exit, enter and move within home settings. Open space solutions arranged on one single-floor level were reported to be the most supportive solutions for the stroke rehabilitation process (Reid, 2004). Home adjustments such as layout changes, threshold removals and implementation of slip-resistant floor surfaces were other supportive solutions in the environment (Sørensen et al., 2003).
One barrier is that a small layout hinders patients’ ability to move around, especially when they use assistive devices such as wheelchairs and walker aids. Moreover, the height of things (e.g. closets and cupboards) and the localisation of rooms (e.g. toilet and bedrooms) were reported to be barriers when environmental demands and individual capacities do not match (e.g. too high to grab or too far to reach). For example, stroke survivors with visual impairments struggle to judge stair heights and the distance between objects (Brookfield, et al.,2015). Furthermore, slippery surfaces were found to be barriers for the rehabilitation process as they obstruct patients’ ability to safely move within the home setting (Zhang, et al., 2016).
The above-mentioned articles discussed architectural facilitators and barriers exclusively in terms of the extent to which they supported patients’ physical mobility (e.g. transfer mobility) and their participation and independence in daily activities.
3.2 Interior design features
Assistive devices, such as wheelchairs, walking aids, bathing aids, raised toilets and mobility ramps, were largely considered facilitators for the stroke rehabilitation process (Jellema et al., 2016; Vincent et al., 2007). Landmark objects, such as sofas or strong colourful elements (e.g. red material), were found to be facilitators for stroke survivors who had cognitive or visual-spatial disabilities (Lampinen & Tham, 2003). Moreover, the presence and absence of handrails within the home setting were reported to be, respectively, a facilitator and a barrier for mobility and participation activities (Brookfield, et al., 2015).
The presence of memories in the environment was found to be emotionally supportive, and objects such as TVs, books and notes were also found to be facilitators for cognitive activities (Axelrod et al., 2009). Technical and electronic devices (e.g. heating control systems, bed and chairs control devices) were, instead, reported to be barriers for the cognitive understanding of patients with stroke. The demand that these relatively new features place on patients was perceived to hinder the rehabilitation process (Axelrod et al., 2009).
Similar to the architectural dimension, the articles discussed interior design features almost exclusively in terms of how such features support mobility and everyday activities. However, one of the articles discussed interior design memories, such as ornaments and lifetime possessions, as potential facilitators for stroke emotional recovery (Axelrod et al., 2009).
3.3 Ambient features
Ambient features were the least addressed element of the environment. The articles mainly discussed this environmental dimension as a moderator of the interaction between patients with stroke and the other two environmental dimensions. Furthermore, the reports of ambient features focused more on environmental barriers than facilitators. High levels of noises, simultaneous sounds and poor illumination negatively affect patients’ capability to concentrate on different rehabilitation tasks (cognitive and motor) (Lampinen & Tham, 2003).
Music, however, was found to be a facilitator for rehabilitation in terms of facial recognition tasks and emotional connection to a place (Carruth, 1997; Axelrod et al., 2009). The few studies addressing ambient features were related to cognitive, emotional or mobility rehabilitation after stroke.
4 DISCUSSION
The review confirms the lack of research investigations of the physical environmental factors of home settings that patients with stroke experience as facilitators and barriers. Only 15 articles focused on this human–environment interaction. Moreover, the majority of the studies included in the review did not have as their primary aim to study the physical environment; instead, they focused on other factors affecting rehabilitation after stroke, e.g. rehabilitation interventions, medical treatments and social support. The importance of the physical environment was a side finding.
The ongoing transformation of healthcare systems implies a shift towards home-based rehabilitation (SOU, 2016). Thus, an improved understanding of the role played by the home environment in supporting patients’ health and well-being appears to be central to any strategy aimed at supporting patients’ stroke recovery (WHO, 2015a, 2015b Furthermore, as the physical environment has been shown to affect people's well-being (Evans, 2003), more studies are needed that focus on and identify the environmental factors that may contribute to a positive rehabilitation process.
The results of this thematic analysis showed that all studies, with the exception of one (Axelrod et al., 2009), evaluated the physical environment of home settings exclusively in terms of how well it supports mobility and daily life activities, whereas they did not investigate psychosocial (e.g. perceived control and social interaction) or emotional processes. Thus, the physical environment features that support patients’ psychosocial health (indirect environmental effects) (Evans, 2003) remain largely unknown.
However, the findings of previous studies have shown how home settings symbolise an expression and extension of the self (Cristoferetti et al., 2011) and therefore hold special meaning for individuals’ psychological processes (Evans, 2003). Moreover, a positive experience with the living place is known to mediate the effect of the physical environment on well-being outcomes (Evans et al., 2002) and to be a predictor of positive human–environment interactions and restoration processes (Erikson et al., 2009; Rollero & De Piccoli, 2010; Tognoli, 2003). Future research is thus required for a better understanding of the psychosocial processes (i.e. self-efficacy, motivation, perceived control, place attachment and identity) that mediate the interaction between patients with stroke and their home settings (Nanninga et al., 2015) and how such processes relate to specific characteristics of the environment and in turn affect rehabilitation outcomes.
Consistent with the ecological model and the person-centred approach, a beneficial person–environment fit is achieved when the patient's individual needs (i.e. mobility, cognitive, psychological and social) are evaluated and matched with the available environment by means of appropriate interventions and services (Lawton & Nahemow, 1973). In this view, the physical environment is acknowledged to be an important factor to increase awareness of disabilities after a stroke (Tham, Bernspång, & Fisher, 1999; Von Koch, Wottrich, & Holmqvist, 1998) and also to develop personal strategies to address everyday life matters (Von Koch, Holmqvist, Wottrich, Tham, & de Pedro-Cuesta, 2000) and to re-engage in real-life situations.
The results of this systematic review showed that the most common supportive features of the physical environment of home settings were accessibility (single-floor planning) and environmental modifications (supportive of mobility into, out of and within the home setting), handrails, wheelchairs and ramps. In contrast, when the room localisation and the height of objects did not match with the patient's motoric abilities, barriers arose. This was the case, for instance, for stroke survivors with diverse types of visual impairments that caused problems in judging stair heights or the distance between objects and consequently negatively affected their mobility and their daily life activities (Brookfield, et al., 2015).
Again, these environmental factors were associated exclusively with motor and mobility functions, and information regarding cognitive and emotional processes was absent. This finding emphasises the need for more research addressing the interplay of the physical environment with cognitive and emotional processes and participation in social activities.
Another important aspect that appeared to be missing in the current research on stroke care in home settings is the aspect of time and its significance for stroke survivors. Differences in perceptions of and experiences in the physical environment as a facilitator or a barrier have been suggested to vary over time depending on the interaction between the individual functioning and the setting characteristics (Roman, 2008). What is perceived to be supportive during early rehabilitation phases might not be relevant for the long-term goals for daily life reintegration. Thus, future investigations are needed to address the temporal aspects by means of longitudinal studies on person–environment interactions and the facilitators and barriers in relation to time since stroke onset. Moreover, it is important to understand how patients’ perceptions of what are facilitators or barriers might vary with their life roles and goals.
Furthermore, information was lacking regarding the possible impact of the geographic location of the home-care setting on rehabilitation processes. It has been suggested that geographic distance from meaningful activities is a barrier for social participation. However, the literature reviewed provided no further information regarding this aspect, and future investigations are needed to fill this knowledge gap (Algurén et al., 2009).
In conclusion, the findings of this review suggest that the impact of the physical environment varies depending on the type of disability associated with stroke. For example, wheelchairs, which are most commonly classified as facilitators, might be barriers for stroke survivors affected by visual-spatial agnosia (Jellema et al., 2016; Lampinen & Tham, 2003). Moreover, the physical objects interact with the design of the overall setting in which they are used; therefore, the extent to which patients perceive them as supportive for their functioning also depends on how well such objects fit in the overall housing design (e.g. home layout) (Jellema et al., 2016; Küller, 1991).
The above-mentioned consideration is in line with the framework proposed by the ICF, which states that individual functioning and well-being result from dynamic interactions among several factors, such as health conditions and environmental factors. Human–environment interactions are unique, and their prerequisites must be defined for each case as the same physical features can be experienced very differently depending on the interactions among body functioning, activities of engagement and physical characteristics of the setting (Algurén et al., 2009).
Today, the paucity of information regarding the physical environment of home settings for stroke survivors makes it impossible to identify evidence-based design solutions for future planning. The existing findings can be seen exclusively as supportive information for decisional processes about what aspects might support vs. hinder rehabilitation after stroke in home settings. However, due to the complexity of human–environment interactions, future research on stroke patients and home ambience are not only needed but might also profit from the integration of conceptual framework and knowledge from several disciplines. For example, by embracing an environmental psychology perspective, together with the more classic medical and nursing approaches, could advance our understanding of stroke recovery in home settings and reduce the knowledge gap about the indirect environmental effects that are responsible for those psychological processes involved in rehabilitation outcomes.
4.1 Limitations
Our findings should be interpreted within the context of the study's limitations. The search strategy focused on the physical environment in home care; thus, terms such as robotic devices were not included, despite being amenities that are provided to patients with stroke. Future investigations might consider the interplay between technological aids and patients with stroke within a more classic definition of the physical environment, such as that used in this work. Additionally, we did not search the grey literature; therefore, we might have missed eligible papers. Several factors made this literature challenging to synthesise. We found considerable heterogeneity within and across the included articles with regard to population characteristics, locations considered, measures used and outcomes reported, which prevents firm conclusions. Some studies addressed the interactions among the physical environment, rehabilitation processes and several diagnoses (e.g. dementia and Alzheimer's) rather than focusing exclusively on patients with stroke (Carruth, 1997; Brookfield, et al., 2015). However, due to the lack of investigations focusing on the topic of interest, the authors decided that the information retrieved in such mixed population studies was still relevant, and therefore, it was included in the present work. Moreover, the physical environment was considered to be poorly described in the literature found, which made it hard to put forward any strong evidence regarding how home setting could be designed or adapted to support positive rehabilitation outcomes among stroke patients. Future investigation, might want to address more into detailed the physical dimension of home settings for stroke rehabilitation purposes by, for example, integrating architects and environmental psychologists’ evaluations. However, the purpose of a systematic review was to provide an overview and a high-level description of the state of the evidence (Moher et al., 2009), which is still missing with regard to the interaction between the physical environment of the home setting and patients with stroke. Therefore, the present work can be considered a valuable contribution to the field of stroke care at a community level and a support for future research that seeks to advance the understanding of the vulnerable societal group of stroke survivors.




