Evaluation of an inner city HIV pre-exposure prophylaxis service tailored to the needs of people who inject drugs
Abstract
Objectives
HIV prevention strategies including pre-exposure prophylaxis (PrEP) must reach all in need to achieve elimination of transmission by 2030. Mainstream provision may inadvertently exclude key populations. Incidence of HIV in people who inject drugs (PWID) in Glasgow, Scotland's largest city, is increasing, partly due to sexual transmission. Scotland provides publicly funded oral PrEP for individuals at sexual risk of HIV through sexual health services; however, uptake by PWID has been negligible. We developed a tailored outreach PrEP service based in the local homeless health centre. We used active case finding, flexibility of assessment location, supervised community daily dispensing and active follow-up to optimise uptake and adherence. We describe a two-year service evaluation.
Methods
We reviewed the case records of all PWID identified by the outreach team as being at higher risk of sexual acquisition for whom PrEP was considered between November 2018 and November 2020. Evaluation focused on PrEP uptake, adherence and monitoring. We conducted a descriptive statistical analysis.
Results
Of 41 PWID assessed as eligible, 32 (78.0%) commenced PrEP. The proportion of PrEP-covered days was 3320/3400 days (97.6%); 31/32 (96.9%) had regular HIV serology monitoring. The service was feasible to run, but it relied on outreach provision and liaison with other services.
Discussion
Tailored PrEP services can reach PWID effectively. Uptake and adherence were high but the model was resource-intensive. Appropriately tailored PrEP delivery may be required to meet the needs of this and other key populations who experience barriers to accessing mainstream services.
INTRODUCTION
Globally, one in 10 HIV infections occur in people who inject drugs (PWID) [1]. Established combination prevention strategies have focused on needle exchange, opiate substitution therapy (OST) and drug rehabilitation [2], in addition to HIV testing and early antiretroviral therapy (ART). However, once an HIV outbreak is established within an injecting population, sexual transmission also becomes important. Oral tenofovir disoproxil/emtricitabine as pre-exposure prophylaxis (PrEP) is highly effective at reducing sexual transmission of HIV [3, 4]. It was associated with 48.9% reduction in HIV acquisition in the only study of PrEP effectiveness in PWID [5].
Since 2015, there has been an HIV outbreak among PWID in Scotland's largest city, Glasgow (population 1 million). It is associated with cocaine injecting, homelessness and incarceration [6] despite high coverage of needle exchange and OST. The link between cocaine use and sexual behaviours, as well as the higher than expected HIV incidence among females supports sexual transmission [6]. Indeed, sexual contact was reported as a potential transmission route by almost 50% of individuals at diagnosis [7].
Scotland implemented a national state-funded programme delivering PrEP and associated monitoring free of charge through sexual health clinics in 2017. Provision is for individuals at risk of sexual (but not injecting-associated) acquisition. A 20% reduction in new HIV diagnoses in gay and bisexual men followed implementation [8], but there has been limited impact on other groups [9, 10]. This is perhaps unsurprising among PWID, who may find it difficult to engage with mainstream health services [11]. PWID experience barriers to HIV testing and prevention [12], including fear of criminalization or stigma, lack of transport, and difficulties prioritizing healthcare.
In 2018, HIV prevalence in PWID in Glasgow inner city reached almost 11% [6]. As part of the outbreak control response, we commenced a bespoke PrEP service, providing daily oral tenofovir disoproxil/emtricitabine. We carried out a service evaluation with the objective of assessing uptake and adherence of PrEP among PWID identified as being at higher risk of sexual transmission of HIV. The service is described in the following to offer insights into the interventions used to achieve these outcomes.
Developing a tailored PrEP service model for PWID
A qualitative study exploring perceptions of PrEP among PWID at the epicentre of the outbreak [13] highlighted that, in addition to service barriers, PWID had poor health literacy and tended to underestimate HIV risk. Participants welcomed PrEP but had a strong preference for provision in familiar settings where they were engaging with other services and had trusting relationships with providers [13].
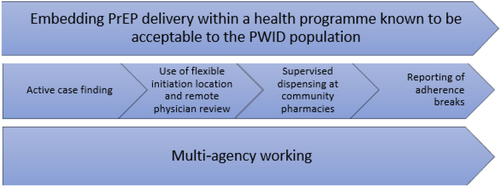
Building on experience of a successful model of collaborative HIV treatment delivery in PWID in Glasgow [7], a small team developed a tailored PrEP service. Novel strategies were needed to facilitate identification of PrEP candidates, initiation of PrEP and adherence. Key components are shown in Figure 1.
Identifying PWID with sexual risk of HIV acquisition and initiating PrEP
Active case finding rather than reliance on individuals’ self-identification as PrEP candidates was used. Sexual health (SH) nurses embedded within the homeless health clinic offered blood-borne virus information and testing, contraception and sexual healthcare. Service users were informed about PrEP during these consultations. The PrEP assessments and venepuncture were carried out for at-risk individuals. Sexual health staff also raised awareness among the allied services, encouraging staff to discuss HIV risk and signpost patients to the team.
At baseline, consent was sought to liaise with allied services, including patients’ OST prescribers and community pharmacies. The physician reviewed the cases and results remotely, overseeing prescribing, monitoring and requesting additional investigations as appropriate.
Facilitation of adherence to PrEP, retention in care and resources
Almost all individuals identified were receiving OST supervised at community pharmacies. PrEP was dispensed at community pharmacies alongside OST as directly observed therapy (DOT). Community pharmacists informed HIV specialist pharmacists of lapses in adherence. Any lapses triggered the SH nurses to contact the individual via phone (or liaise with other key services if necessary) to ascertain the reason and facilitate recommencement. Recall for regular monitoring was done in the same way. Individuals were offered flexible timings and locations (most often homeless health or addiction services) for subsequent appointments, enabling PrEP to be integrated with other needs. Some were ad hoc whilst individuals attended health/addiction services for other purposes. Communication with prison services was also important as incarceration caused adherence breaks.
This model relied upon highly experienced SH outreach nurses (37 h/week), HIV physician (2 h/week), HIV pharmacist (1 h/week), HIV pharmacy technician (2 h/week), and a clinical room at the homeless health centre.
For comparison, in mainstream SH services in Glasgow, PrEP is accessed by appointment. Quarterly reviews consist of a 15-min telephone assessment with a SH nurse/junior doctor followed by a clinic visit for monitoring tests and PrEP collection. Adherence is self-reported and disengagement from care is assumed to indicate cessation of PrEP with no active follow-up. HIV physician support is available, but it is not required for the majority of clients.
METHODS
We reviewed electronic case records of all PWID who had been identified by outreach SH nurses as being at high risk of sexual acquisition of HIV and could potentially benefit from PrEP, from November 2018 until November 2020. Data on acceptability and uptake of PrEP, adherence to correct PrEP dosing and proportion of individuals undergoing regular monitoring were extracted into a bespoke data collection tool. Adherence break data were retrieved from clinical documentation in patient records. Data were stored on an anonymized, password-protected database, analysed and comparisons drawn, using descriptive statistics using SPSS.
RESULTS
Eligibility for PrEP
Forty-seven PWID were identified as eligible for PrEP (Table 1) [9]. Factors included sexual contact within this high-prevalence group; transactional sex; and sexual contact with someone living with HIV without a consistently undetectable viral load.
| Eligibility criteria | Number (%) |
|---|---|
| 1. Current sexual partners, irrespective of gender, of people who are HIV-positive who have a detectable viral load | 16/47 (34.0) |
|
2. Cis and transgender gay and bisexual men, other men who have sex with men, and transgender women with a documented bacterial rectal sexually transmitted infection in the last 12 months |
0 |
|
3. Cis and transgender gay, bisexual men and other men who have sex with men, and transgender women reporting condomless penetrative anal sex with two or more partners in the last 12 months and likely to do so again in the next 3 months |
5/47 (10.6)a |
|
4. Individuals, irrespective of gender, at an equivalent highest risk of HIV acquisition, as agreed with another specialist clinician |
28/47 (59.6)a, b |
- a Two individuals met both criteria 3 and 4.
- b Individuals who met criteria 4 either had transactional sex, or sexual partners of unknown HIV status from within the population affected by the HIV outbreak.
Characteristics of PrEP candidates
Four out of 47 (8.5%) individuals were identified through partner notification of people living with HIV. The remaining 43/47 (91.5%) were identified at the homeless health centre, drug rehabilitation facilities or other community services. The mean age was 36 years (range 19–48) and 26/47 (55.3%) of the cohort were female.
Most of the cohort (41/47, 87.2%) were currently injecting drugs, with 12/41 (29.3%) injecting heroin alone, 3/41 (7.3%) cocaine alone and 26/41 (63.4%) both heroin and cocaine during the 3 months prior to baseline assessment. Hepatitis infection was common: 26/47 (55.3%) had active hepatitis C infection and 1/47 (2.1%) had active hepatitis B. Hepatitis B vaccination was offered to those without immunity. Those with active hepatitis were referred for treatment.
Pre-exposure prophylaxis was recommended for 41/47 (87.2%) individuals. Physicians did not recommend immediate PrEP for six people currently at a reduced risk of HIV due to incarceration or in-patient rehabilitation.
Uptake of PrEP
Of the 41 PWID recommended PrEP, 34/41 (82.9%) accepted the baseline assessment and recommendation to commence PrEP. 32/41 (78%) commenced PrEP as two individuals were untraceable after initial consultations. Of those who declined PrEP, 4/7 (57.1%) felt they were not at risk of HIV.
There was a median of 10 days from identification of PrEP candidacy to commencing PrEP [interquartile range (IQR) 13]. All patients who commenced PrEP had a baseline HIV test. Half of the individuals declined urinary protein assessment, but all had an estimated glomerular filtration rate > 90 mL/min. Two individuals who were not receiving OST declined supervised dispensing.
Adherence and retention in care
A total of 31/32 (96.9%) individuals on PrEP had regular HIV serology monitoring (all ‘window period’ tests and no periods > 4 months on PrEP without an HIV test).
Among the 32 individuals, there were 40 PrEP episodes (we define these as a period of continuous time during which someone is prescribed PrEP, ending when PrEP stopped and is not restarted within 1 week). Reasons for stopping included rehabilitation, prison incarceration or complete disengagement. Adherence data during PrEP episodes were collected for the 30/32 (94%) participants who used DOT. In total, PrEP was prescribed on 3400 days, and was taken on 3320/3400 days (97.6%). A total of 27/40 (67.5%) PrEP episodes had 100% adherence.
Crucially, of the 32 people who have been prescribed PrEP at least once in 2 years, none have been diagnosed with HIV infection.
DISCUSSION
Our tailored model of PrEP provision for PWID was feasible but required highly specialist staffing and appropriate facilities. We were able to carry out baseline assessments and monitoring for those eligible for PrEP. Uptake was high and adherence was excellent, suggesting acceptability among most PWID who were recommended PrEP.
Pre-exposure prophylaxis services for PWID are relatively under-studied. Three service models have been reported in Bangkok [5], Philadelphia [14] and Boston [15]. These sites also recruited participants from services already used by PWIDs and implemented additional measures to assist retention in care.
We observed high uptake of PrEP after specialist staff carefully discussed potential benefits. This aligns with perceptions from Smith's study among Glasgow PWID and exceeds levels of theoretical willingness from a study in Washington, DC [16]. High levels of acceptance were seen in other services: Philadelphia reported week 1 uptake at 70.8%. In Boston, 64% of individuals were prescribed PrEP and 85% of those commenced PrEP.
Adherence to PrEP is associated with efficacy [4, 5] and appears highly variable across many societal groups [17]. Little is known about PrEP adherence among PWID. Adherence was noted as a challenge by the team in Philadelphia. It was not an outcome measured in the Boston study. We based our PrEP service on existing successful models of ART provision alongside OST [7, 18]. Bazzi et al. [19] examined adherence to ART in PWID living with HIV to inform PrEP delivery. Facilitators included engagement with OST, referrals to allied services, strong patient–provider relationships, provider experience in HIV care, accessibility of services and directly administered ART. We believe these factors contributed to the high levels of PrEP adherence observed in our cohort.
The effectiveness of PrEP in reducing HIV acquisition in PWID is unclear. The Bangkok study recruited individuals who had injected drugs in the past year. Directly observed therapy was optional and people were contacted if they missed an appointment. This was associated with a 48.9% reduction in risk of HIV acquisition [5]. In our evaluation period there were no seroconversions, but numbers are small and we did not set out to measure PrEP effectiveness.
Multi-agency working was invaluable for case finding, DOT and follow-up. It is not reported in existing PWID PrEP models, which highlighted concerns regarding adherence [5, 14]. We show that it is possible to achieve high levels of adherence with regular monitoring among this vulnerable group but it required much more intensive support than usual care within SH clinics. Studies examining cost-effectiveness of delivering PrEP to PWID in the USA [20] found that it is an expensive intervention but highlighted that selecting PWID at high risk of HIV acquisition (a strategy we employed) increased cost-effectiveness. Cost-effectiveness is likely to increase as generic formulations become available in all settings.
This evaluation brings new knowledge to an important but under-researched area of HIV prevention. As an evaluation of a service with a small number of users, there are limitations to the conclusions we draw and generalizability to other settings; however, they are an indication of what can be achieved. It is notable that the individuals have differing durations of PrEP use, and we have therefore presented the adherence data collectively. It is not possible to infer any efficacy data from the evaluation.
This model of PrEP care may be useful in settings where there are PWID or other vulnerable groups not utilizing mainstream PrEP services. Aspects of this model, including active case finding, multi-agency working, appointment flexibility and remote specialist physician overview, could be utilized to reach other key populations. However, models should be tailored to the individual population in partnership with existing services. As long-acting injectable PrEP formulations become available, we believe this could be easily integrated into this PrEP pathway.
CONCLUSIONS
To achieve elimination of HIV transmission by 2030 [21], prevention approaches including PrEP must reach all individuals at higher risk of HIV acquisition, including key populations. Delivering PrEP to PWID at higher risk of sexual acquisition of HIV in the context of an outbreak is both feasible and acceptable and can achieve high levels of drug adherence and monitoring. Modifications to service delivery are required to remove barriers to case finding, PrEP initiation and adherence. Although such services are resource-intensive, equity of access to HIV prevention is vital for both population health and human rights.
ACKNOWLEDGEMENTS
We acknowledge the work of the wider clinical team with particular thanks to Euan Proud, Kathryn Brown, Sharon Jordan, Ashley Milrine, Caroline Scade, Fiona Mollison and Natasha Walker.
CONFLICT OF INTEREST
No conflict of interest declared.
AUTHOR CONTRIBUTIONS
CG: evaluation design, data collection, data analysis, discussion and preparation of manuscript. LB: data collection, data analysis, discussion and preparation of manuscript. MS: discussion and preparation of manuscript. CE: data analysis, discussion an preparation of manuscript. RM: evaluation design, data collection, data analysis, discussion and preparation of manuscript.




