A reappraisal of oesophageal mucosal biopsy specimens showing sloughing
Abstract
Aims
Sloughing of the oesophageal squamous mucosa may be observed in biopsies from patients with a variety of conditions, in the absence or presence of inflammation. This study aimed to compare the histologic, endoscopic, and clinical findings of patients with histologic features of sloughing, with or without associated inflammation, including a detailed analysis of the medication history.
Methods and results
Retrospective histologic examination was performed on 51 biopsy specimens, with additional bacterial and fungal stains. Cases with sloughing in the absence of inflammation (n = 22) were classified as sloughing oesophageopathy, while cases with inflammation (n = 29) were classified as acute neutrophilic or eosinophilic sloughing esophagitis, based on the predominant inflammatory cell. As controls, oesophageal biopsies from patients with well-defined forms of oesophagitis were prospectively assessed. For all categories, lesions predominated in the mid-oesophagus (67%). Endoscopic sloughing and use of nasal/inhaled corticosteroids were more frequently observed in the oesophageopathy group compared to the oesophagitis group (55% versus 22%, P = 0.03 and 38% versus 10%, P = 0.04, respectively). Bacteria were more commonly found in the detached epithelium of the oesophageopathy cases (73%), suggesting colonization of the necrotic layer rather than infection. None of the biopsy specimens of patients with well-defined causes of oesophagitis showed sloughing.
Conclusions
In conclusion, sloughing of the luminal layer of the squamous mucosa is a histologic feature that may be identified in the absence (oesophageopathy) or presence of inflammation (oesophagitis). The frequent mid-oesophageal involvement and associations with multiple medications suggest that medication-induced oesophageal injury may be a key contributor to this pattern of injury.
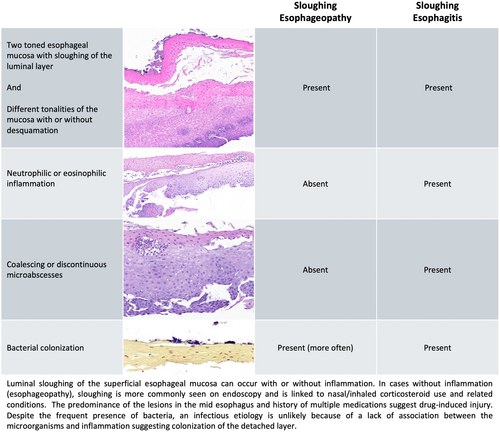
Graphical Abstract
Luminal sloughing of the superficial oesophageal mucosa can occur with or without inflammation. In cases without inflammation (oesophageopathy), sloughing is more commonly seen on endoscopy and is linked to nasal/inhaled corticosteroid use and related conditions. The predominance of the lesions in the mid-oesophagus and history of multiple medications suggest drug-induced injury. Despite the frequent presence of bacteria, an infectious aetiology is unlikely because of a lack of association between the microorganisms and inflammation, suggesting colonization of the detached layer.
Conflict of Interest
All authors declare that they have no conflicts of interest.
Open Research
Data Availability Statement
The data of the study are available and can be shared by the corresponding author upon a reasonable request and approval.