Subungual melanoma: molecular analysis of 31 cases from early stage to invasive melanoma
Abstract
Aims
The distinction between the benign subungual melanocytic lesions and an early lesion of subungual melanoma (SUM) remains a diagnostic challenge. We evaluated the routine diagnostic utility of array Comparative Genomic Hybridization (aCGH) to detect whole-genome copy number variations (CNV) as well as targeted next-generation sequencing (NGS) in SUM.
Methods and Results
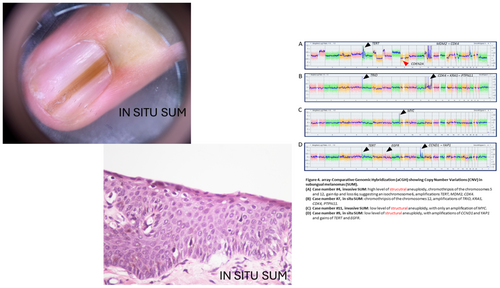
This retrospective study included 20 cases of in situ SUM and 11 cases of invasive SUM. Analysis by aCGH detected common oncogene amplifications in all but one case of invasive SUM (n = 10) and in all cases of in situ SUM with a melanocyte count (MC) >45/mm (n = 4 true positive) and the average number of CNV was 8.5. Thirteen remaining cases of in situ SUM gave false negative results (n = 13), owing to a lack of sufficient melanocytes to analyse (median MC of 35.35; range: 10.16–39.5). Molecular analysis failed in four cases (three in situ SUM and one invasive SUM) due to insufficient amounts of DNA. Across the whole cohort, the sensitivity of aCGH was 52%, but when adjusting the cutoff to MC >45/mm, the sensitivity was 93%. Targeted NGS was less informative than aCGH analyses in our series of SUM.
Conclusion
To distinguish malignant from benign lesions, especially in situ SUM versus atypical lentiginous melanocytic proliferations, aCGH analysis should be performed when the MC is above 45 melanocytes per linear millimetre. This pangenomic method can detect oncogene amplifications, as well as a number of CNV >3, which strongly support the diagnosis of malignancy.
Graphical Abstract
To distinguish malignant from benign lesions, especially in situ SUM versus atypical lentiginous melanocytic proliferations, aCGH analysis should be performed when the MC is above 45/mm. This pangenomic method can detect oncogene amplifications, as well as a number of CNV >3, which strongly support the diagnosis of malignancy.
Conflict of interest
None declared.
Open Research
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.