Head to head: do neuroendocrine tumours in the breast truly exist?
Emad Rakha
University of Nottingham and Nottingham University Hospital NHS Trust, Department of Histopathology, Nottingham City Hospital, Nottingham, UK
Search for more papers by this authorCorresponding Author
Puay Hoon Tan
Division of Pathology, Singapore General Hospital, Singapore
Address for correspondence: Dr P H Tan, Division of Pathology, Singapore General Hospital, Academia Diagnostics Tower Level 7, 20 College Road, Singapore 169856. e-mail: [email protected]Search for more papers by this authorEmad Rakha
University of Nottingham and Nottingham University Hospital NHS Trust, Department of Histopathology, Nottingham City Hospital, Nottingham, UK
Search for more papers by this authorCorresponding Author
Puay Hoon Tan
Division of Pathology, Singapore General Hospital, Singapore
Address for correspondence: Dr P H Tan, Division of Pathology, Singapore General Hospital, Academia Diagnostics Tower Level 7, 20 College Road, Singapore 169856. e-mail: [email protected]Search for more papers by this authorAbstract
Breast cancer (BC) is a heterogeneous disease with a spectrum of morphological features. Concepts of histogenesis and differentiation in BC remain controversial. Recent evidence supports differentiation rather than histogenesis as the underlying mechanism for the myriad morphological appearances of BC. Prognosis and response to therapy are determined by a combination of factors, including tumour grade, stage and receptor status, whereas tumour histological types play an independent role in only limited examples. Neuroendocrine tumours (NETs) comprise one of the most debated entities in the breast since their first description. Apart from the rare small-cell NE carcinoma (NEC), which has well-characterized features similar to their counterparts in other organs, the true existence, diagnostic criteria and clinical significance of NE neoplasms (NENs) in the breast are shrouded in controversy. At the core of this discussion is whether normal NE cells exist in the breast, and if breast NETs have distinct morphology and clinical behaviour. When NETs are encountered in the breast, metastatic origin has to be excluded. The more frequent situation in which NE differentiation is observed in breast cancers is in the context of recognizable, morphologically well-described special-type neoplasms such as the hypercellular mucinous carcinoma and solid papillary carcinoma. In this review, arguments for and against maintaining the category of NENs in the breast are articulated in relation to existing literature on this group of unusual tumours.
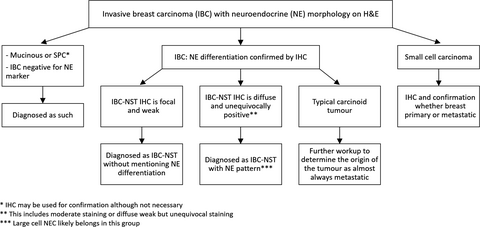
Graphical Abstract
Conflicts of interest
None.
Open Research
Data availability statement
Data sharing not applicable - no new data generated
References
- 1 World Health Organisation (WHO) Classification of Tumours Editorial Board. Breast tumours. 5th ed. Lyon, France: IARC, 2019.
- 2Rakha EA, El-Sayed ME, Lee AH et al. Prognostic significance of Nottingham histologic grade in invasive breast carcinoma. J. Clin. Oncol. 2008; 26; 3153–3158.
- 3Feyrter F, Hartmann G. on the carcinoid growth form of the carcinoma mammae, especially the carcinoma solidum (gelatinosum) mammae. Frankf. Z. Pathol 1963; 73; 24–39.
- 4Azzopardi JG, Muretto P, Goddeeris P, Eusebi V, Lauweryns JM. ‘Carcinoid’ tumours of the breast: the morphological spectrum of argyrophil carcinomas. Histopathology 1982; 6; 549–569.
- 5Bussolati G, Gugliotta P, Sapino A, Eusebi V, Lloyd RV. Chromogranin-reactive endocrine cells in argyrophilic carcinomas (‘carcinoids’) and normal tissue of the breast. Am. J. Pathol. 1985; 120; 186–192.
- 6Tavassoli F, Devilee P. Pathology and genetics of tumours of the breast and female genital organs. 3rd ed. IARC: Lyon, France, 2003.
- 7Sapino A, Papotti M, Righi L, Cassoni P, Chiusa L, Bussolati G. Clinical significance of neuroendocrine carcinoma of the breast. Ann. Oncol. 2001; 12(Suppl. 2); S115–S117.
- 8Bussolati G, Badve S. Carcinomas with neuroendocrine features. In SR Lakhani, IO Ellis, SJ Schnitt, PH Tan, MJ Vijver eds. WHO classification of tumours of the breast. France, Lyon: IARC, 2012; 62–63.
- 9Rindi G, Klimstra DS, Abedi-Ardekani B et al. A common classification framework for neuroendocrine neoplasms: an International Agency for Research on Cancer (IARC) and World Health Organization (WHO) expert consensus proposal. Mod. Pathol. 2018; 31; 1770–1786.
- 10Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van de Vijver MJ. WHO classification of tumours of the breast. 4th ed. Lyon, France: IARC, 2012.
- 11Wang J, Wei B, Albarracin CT, Hu J, Abraham SC, Wu Y. Invasive neuroendocrine carcinoma of the breast: a population-based study from the surveillance, epidemiology and end results (SEER) database. BMC Cancer 2014; 14; 147.
- 12Miremadi A, Pinder SE, Lee AH et al. Neuroendocrine differentiation and prognosis in breast adenocarcinoma. Histopathology 2002; 40; 215–222.
- 13Bogina G, Munari E, Brunelli M et al. Neuroendocrine differentiation in breast carcinoma: Clinicopathological features and outcome. Histopathology 2016; 68; 422–432.
- 14Rakha E, Reis-Filho J, Sasano H, Wu Y. Neuroendocrine neoplasms. In World Health Organisation (WHO) classification of tumours breast tumours. Lyon, France: IARC, 2019; 155–161.
- 15Hu J, Han B, Huang J. Morphologic spectrum of neuroendocrine tumors of the prostate: An updated review. Arch. Pathol. Lab. Med. 2020; 144; 320–325.
- 16Wachter DL, Hartmann A, Beckmann MW et al. Expression of neuroendocrine markers in different molecular subtypes of breast carcinoma. Biomed. Res. Int. 2014; 2014; 408459.
- 17Shin SJ, DeLellis RA, Ying L, Rosen PP. Small cell carcinoma of the breast: a clinicopathologic and immunohistochemical study of nine patients. Am. J. Surg. Pathol. 2000; 24; 1231–1238.
- 18Mirza IA, Shahab N. Small cell carcinoma of the breast. Semin. Oncol. 2007; 34; 64–66.
- 19Weigelt B, Geyer FC, Horlings HM, Kreike B, Halfwerk H, Reis-Filho JS. Mucinous and neuroendocrine breast carcinomas are transcriptionally distinct from invasive ductal carcinomas of no special type. Mod. Pathol. 2009; 22; 1401–1414.
- 20Marchio C, Geyer FC, Ng CK et al. The genetic landscape of breast carcinomas with neuroendocrine differentiation. J. Pathol. 2017; 241; 405–419.
- 21Pereira B, Chin SF, Rueda OM et al. The somatic mutation profiles of 2,433 breast cancers refines their genomic and transcriptomic landscapes. Nat. Commun. 2016; 7; 11479.
- 22Inno A, Bogina G, Turazza M et al. Neuroendocrine carcinoma of the breast: current evidence and future perspectives. Oncologist 2016; 21; 28–32.
- 23Visscher DW, Yasir S. Neuroendocrine tumors of the breast. Endocr. Pathol. 2017; 28; 121–127.
- 24Rosen LE, Gattuso P. Neuroendocrine tumors of the breast. Arch. Pathol. Lab. Med. 2017; 141; 1577–1581.
- 25Gallo M, Campione S, Di Vito V et al. Primary neuroendocrine neoplasms of the breast: Still open issues. Front. Endocrinol. 2021; 11; 610230.
- 26Uccella S. The classification of neuroendocrine neoplasms of the breast and its clinical relevance. Virchows Arch. 2021.
- 27Rakha E, Toss M, Quinn C. Specific cell differentiation in breast cancer: a basis for histological classification. J. Clin. Pathol. 2022; 75; 76–84.
- 28Tay TKY, Tan PH. Papillary neoplasms of the breast-reviewing the spectrum. Mod. Pathol. 2021; 34; 1044–1061.
- 29Tan BY, Thike AA, Ellis IO, Tan PH. Clinicopathologic characteristics of solid papillary carcinoma of the breast. Am. J. Surg. Pathol. 2016; 40; 1334–1342.
- 30Yang L, Roy M, Lin H et al. Validation of prognostic significance of the proposed uniform classification framework in neuroendocrine neoplasms of the breast. Breast Cancer Res. Treat. 2021; 186; 403–415.
- 31Cloyd JM, Yang RL, Allison KH, Norton JA, Hernandez-Boussard T, Wapnir IL. Impact of histological subtype on long-term outcomes of neuroendocrine carcinoma of the breast. Breast Cancer Res. Treat. 2014; 148; 637–644.
- 32Irelli A, Sirufo MM, Morelli L, D'Ugo C, Ginaldi L, De Martinis M. Neuroendocrine cancer of the breast: a rare entity. J. Clin. Med. 2020; 9; 1452.
- 33Masab M, Gross A, Flanagan M, Goldberg R, Malla M. Neuroendocrine neoplasm of the breast presenting as a liver metastasis: a rare diagnostic challenge. Cureus 2021; 13; e16860.
- 34Metovic J, Castellano I, Marinelli E et al. INSM1 expression in breast neoplasms with neuroedocrine features. Endocr. Pathol. 2021; 32; 452–460.
- 35Wei Y, Ke X, Yu J et al. Clinical and genomic analyses of neuroendocrine neoplasms of the breast. Mod. Pathol. 2021. https://doi.org/10.1038/s41379-021-00965-w.
10.1038/s41379?021?00965?w Google Scholar
- 36Lai BS, Tsang JY, Poon IK et al. The clinical significance of neuroendocrine features in invasive breast carcinomas. Oncologist 2020; 25; e1318–e1329.
- 37Liu Q, Zhang J, Kulkarni HR, Baum RP. 177Lu-DOTATOC peptide receptor radionuclide therapy in a patient with neuroendocrine breast carcinoma and breast invasive ductal carcinoma. Clin. Nucl. Med. 2020; 45; e232–e235.
- 38Marijanovic I, Kraljevic M, Buhovac T, Karan KD. Rare human epidermal growth factor receptor 2 (HER-2)-positive neuroendocrine carcinoma of the breast: A case report with 9-year follow-up. Am. J. Case Rep 2020; 21; e925895.
- 39Ozdirik B, Kayser A, Ullrich A et al. Primary neuroendocrine neoplasms of the breast: case series and literature review. Cancer 2020; 12; 733.
- 40Arslan E, Cermik TF, Didem Can Trabulus F, Canan Kelten Talu E, Basaran S. Diagnostic impact of (18)F-FDG PET/CT on the management of rare breast carcinomas: apocrine and neuroendocrine carcinomas. Rev. Esp. Med. Nucl. Imagen. Mol. (English edition) 2019; 38; 147–153.
- 41Vranic S, Palazzo J, Sanati S et al. Potential novel therapy targets in neuroendocrine carcinomas of the breast. Clin. Breast Cancer 2019; 19; 131–136.
- 42Del Arco CD, Sastre J, Peinado P, Diaz A, Medina LO, Fernandez Acenero MJ. Neuroendocrine neoplasms in rare locations: Clinicopathological features and review of the literature. Indian J. Endocrinol. Metab. 2018; 22; 308–315.
- 43Kelten Talu C, Leblebici C, Kilicaslan Ozturk T, Hacihasanoglu E, Baykal Koca S, Gucin Z. Primary breast carcinomas with neuroendocrine features: Clinicopathological features and analysis of tumor growth patterns in 36 cases. Ann. Diagn. Pathol. 2018; 34; 122–130.
- 44Lavigne M, Menet E, Tille JC et al. Comprehensive clinical and molecular analyses of neuroendocrine carcinomas of the breast. Mod. Pathol. 2018; 31; 68–82.
- 45Vats M, Sachan V, Prajapati S, Mandal S. Triple receptor-positive primary neuroendocrine carcinoma of breast in a young patient. BMJ Case Rep. 2018; 2018. https://doi.org/10.1136/bcr-2017-223280.
10.1136/bcr?2017?223280 Google Scholar
- 46Abou Dalle I, Abbas J, Boulos F, Salem Z, Assi HI. Primary small cell carcinoma of the breast: a case report. J. Med. Case Reports 2017; 11; 290.
- 47Albright EL, Keeney ME, Bashir A, Weigel RJ. Poorly differentiated neuroendocrine carcinoma of the breast with Merkel cell features. Breast J. 2018; 24; 644–647.
- 48Li Y, Du F, Zhu W, Xu B. Neuroendocrine carcinoma of the breast: a review of 126 cases in China. Chin. J. Cancer 2017; 36; 45.
- 49Munoz-Zuluaga CA, Kotiah S, Studeman KD. High-grade poorly differentiated neuroendocrine carcinoma of the breast with low oncotype DX recurrence score: a case report. Breast Dis. 2017; 37; 99–103.
- 50Roininen N, Takala S, Haapasaari KM et al. Primary neuroendocrine breast carcinomas are associated with poor local control despite favourable biological profile: a retrospective clinical study. BMC Cancer 2017; 17; 72.
- 51Soe AM, Joseph G, Guevara E, Xiao P. Primary neuroendocrine carcinoma of the breast metastatic to the bones, which chemotherapy? Breast J. 2017; 23; 589–593.
- 52Steinhof-Radwanska K, Barczyk A, Powazka P et al. Primary neuroendocrine carcinoma of the breast – a report of four cases. Endokrynol. Pol. 2017; 68; 597–602.
- 53Tremelling A, Samuel S, Murray M. Primary small cell neuroendocrine carcinoma of the breast – a case report and review of the literature. Int. J. Surg. Case Rep. 2017; 38; 29–31.
- 54D'Antonio A, Addesso M, Memoli D, Cascone A, Cremone L. A case of multicentric low-grade neuroendocrine breast tumor with an unusual histological pattern. Breast Dis. 2016; 36; 161–164.
- 55Del Rosario M, Tsai H, Dasanu CA. Multicentric neuroendocrine carcinoma of the breast presenting with multiple osteolytic bone metastases. Conn. Med. 2016; 80; 525–528.
- 56Gevorgyan A, Bregni G, Galli G, Zanardi E, de Braud F, Di Cosimo S. HER2-positive neuroendocrine breast cancer: case report and review of literature. Breast Care 2016; 11; 424–426.
- 57Alva KA, Tauro LF, Shetty P, Saldanha E. Primary neuroendocrine carcinoma of the breast: a rare and distinct entity. Indian J. Cancer 2015; 52; 636–637.
- 58Ang D, Ballard M, Beadling C et al. Novel mutations in neuroendocrine carcinoma of the breast: possible therapeutic targets. Appl. Immunohistochem. Mol. Morphol. 2015; 23; 97–103.
- 59Hare F, Giri S, Patel JK, Hahn A, Martin MG. A population-based analysis of outcomes for small cell carcinoma of the breast by tumor stage and the use of radiation therapy. Springerplus 2015; 4; 138.
- 60Janosky M, Bian J, Dhage S et al. Primary large cell neuroendocrine carcinoma of the breast, a case report with an unusual clinical course. Breast J. 2015; 21; 303–307.
- 61Kawasaki T, Ishida M, Tada T et al. Well-differentiated neuroendocrine tumor of the breast with recurrence due to needle tract seeding. Virchows Arch. 2015; 466; 479–481.
- 62Kwon SY, Bae YK. Reclassification of mammary carcinomas with neuroendocrine features in accordance with neuroendocrine morphologies in the revised World Health Organisation classification. Histopathology 2015; 66; 755–756.
- 63Lee DH, Park AY, Seo BK, Kim YS, Lee KY, Cha SH. Primary neuroendocrine carcinoma of the breast with clinical features of inflammatory breast carcinoma: a case report and literature review. J. Breast Cancer 2015; 18; 404–408.
- 64Malowany JI, Kundu U, Santiago L, Krishnamurthy S. Fine-needle aspiration detects primary neuroendocrine carcinoma of the breast in a patient with breast implants. Cytojournal 2015; 12; 1.
- 65Rana V, Kakkar S, Anand S, Singh Y. Primary neuroendocrine carcinoma of breast: a rare tumor. Indian J. Cancer 2015; 52; 85–86.
- 66Sherwell-Cabello S, Maffuz-Aziz A, Hernandez-Hernandez B, Bautista-Pena V, Rodriguez-Cuevas S. Primary neuroendocrine tumor of the breast. Breast J. 2015; 21; 312–313.
- 67Wei X, Chen C, Xi D et al. A case of primary neuroendocrine breast carcinoma that responded to neo-adjuvant chemotherapy. Front. Med. 2015; 9; 112–116.
- 68Yavas G, Karabagli P, Araz M, Yavas C, Ata O. HER-2 positive primary solid neuroendocrine carcinoma of the breast: a case report and review of the literature. Breast Cancer 2015; 22; 432–436.
- 69Yoshimura N, Sasada T, Yonehara S. Primary large-cell neuroendocrine carcinoma of the breast occurring in a pre-menopausal woman. Breast Care 2015; 10; 281–283.
- 70Tan PH, Schnitt SJ, van de Vijver MJ, Ellis IO, Lakhani SR. Papillary and neuroendocrine breast lesions: the WHO stance. Histopathology 2015; 66; 761–770.
- 71Cserni G. Histological type and typing of breast carcinomas and the WHO classification changes over time. Pathologica 2020; 112; 25–41.