Favorable impact of hepatitis C virus infection control on recurrence after surgical resection for intrahepatic cholangiocarcinoma
This article relates to:
-
Impact of hepatitis C virus infection control on preventing the postoperative recurrence of intrahepatic cholangiocarcinoma
- Volume 55Issue 5Hepatology Research
- pages: 629-630
- First Published online: March 18, 2025
Corresponding Author
Masahiko Kinoshita
Department of Hepatobiliary-Pancreatic Surgery, Osaka Metropolitan University Graduate School of Medicine, Osaka, Japan
Correspondence
Masahiko Kinoshita, Department of Hepatobiliary-Pancreatic Surgery, Osaka Metropolitan University Graduate School of Medicine, 1-4-3 Asahimachi, Abeno-ku, Osaka 545-8585, Japan.
Email: [email protected]
Search for more papers by this authorHisashi Kosaka
Department of Hepatobiliary Surgery, Kansai Medical University, Hirakata, Japan
Search for more papers by this authorMasaki Kaibori
Department of Hepatobiliary Surgery, Kansai Medical University, Hirakata, Japan
Search for more papers by this authorMasaki Ueno
Second Department of Surgery, Wakayama Medical University, Wakayama, Japan
Search for more papers by this authorSatoshi Yasuda
Department of Surgery, Nara Medical University, Kashihara, Japan
Search for more papers by this authorKoji Komeda
Department of General and Gastroenterological Surgery, Osaka Medical and Pharmaceutical University, Takatsuki, Japan
Search for more papers by this authorYusuke Yamamoto
Division of Digestive Surgery, Department of Surgery, Kyoto Prefectural University of Medicine, Kyoto, Japan
Search for more papers by this authorMasaji Tani
Division of Gastrointestinal Surgery, Department of Surgery, Shiga University of Medical Science, Otsu, Japan
Search for more papers by this authorTsukasa Aihara
Division of Surgery, Meiwa Hospital, Nishinomiya, Japan
Search for more papers by this authorHiroji Shinkawa
Department of Hepatobiliary-Pancreatic Surgery, Osaka Metropolitan University Graduate School of Medicine, Osaka, Japan
Search for more papers by this authorShinya Hayami
Second Department of Surgery, Wakayama Medical University, Wakayama, Japan
Search for more papers by this authorYasuko Matsuo
Department of Surgery, Nara Medical University, Kashihara, Japan
Search for more papers by this authorNao Kawaguchi
Department of General and Gastroenterological Surgery, Osaka Medical and Pharmaceutical University, Takatsuki, Japan
Search for more papers by this authorRyo Morimura
Division of Digestive Surgery, Department of Surgery, Kyoto Prefectural University of Medicine, Kyoto, Japan
Search for more papers by this authorHaruki Mori
Division of Gastrointestinal Surgery, Department of Surgery, Shiga University of Medical Science, Otsu, Japan
Search for more papers by this authorTakayoshi Nakajima
Division of Surgery, Meiwa Hospital, Nishinomiya, Japan
Search for more papers by this authorShoji Kubo
Department of Hepatobiliary-Pancreatic Surgery, Osaka Metropolitan University Graduate School of Medicine, Osaka, Japan
Search for more papers by this authorTakeaki Ishizawa
Department of Hepatobiliary-Pancreatic Surgery, Osaka Metropolitan University Graduate School of Medicine, Osaka, Japan
Search for more papers by this authorCorresponding Author
Masahiko Kinoshita
Department of Hepatobiliary-Pancreatic Surgery, Osaka Metropolitan University Graduate School of Medicine, Osaka, Japan
Correspondence
Masahiko Kinoshita, Department of Hepatobiliary-Pancreatic Surgery, Osaka Metropolitan University Graduate School of Medicine, 1-4-3 Asahimachi, Abeno-ku, Osaka 545-8585, Japan.
Email: [email protected]
Search for more papers by this authorHisashi Kosaka
Department of Hepatobiliary Surgery, Kansai Medical University, Hirakata, Japan
Search for more papers by this authorMasaki Kaibori
Department of Hepatobiliary Surgery, Kansai Medical University, Hirakata, Japan
Search for more papers by this authorMasaki Ueno
Second Department of Surgery, Wakayama Medical University, Wakayama, Japan
Search for more papers by this authorSatoshi Yasuda
Department of Surgery, Nara Medical University, Kashihara, Japan
Search for more papers by this authorKoji Komeda
Department of General and Gastroenterological Surgery, Osaka Medical and Pharmaceutical University, Takatsuki, Japan
Search for more papers by this authorYusuke Yamamoto
Division of Digestive Surgery, Department of Surgery, Kyoto Prefectural University of Medicine, Kyoto, Japan
Search for more papers by this authorMasaji Tani
Division of Gastrointestinal Surgery, Department of Surgery, Shiga University of Medical Science, Otsu, Japan
Search for more papers by this authorTsukasa Aihara
Division of Surgery, Meiwa Hospital, Nishinomiya, Japan
Search for more papers by this authorHiroji Shinkawa
Department of Hepatobiliary-Pancreatic Surgery, Osaka Metropolitan University Graduate School of Medicine, Osaka, Japan
Search for more papers by this authorShinya Hayami
Second Department of Surgery, Wakayama Medical University, Wakayama, Japan
Search for more papers by this authorYasuko Matsuo
Department of Surgery, Nara Medical University, Kashihara, Japan
Search for more papers by this authorNao Kawaguchi
Department of General and Gastroenterological Surgery, Osaka Medical and Pharmaceutical University, Takatsuki, Japan
Search for more papers by this authorRyo Morimura
Division of Digestive Surgery, Department of Surgery, Kyoto Prefectural University of Medicine, Kyoto, Japan
Search for more papers by this authorHaruki Mori
Division of Gastrointestinal Surgery, Department of Surgery, Shiga University of Medical Science, Otsu, Japan
Search for more papers by this authorTakayoshi Nakajima
Division of Surgery, Meiwa Hospital, Nishinomiya, Japan
Search for more papers by this authorShoji Kubo
Department of Hepatobiliary-Pancreatic Surgery, Osaka Metropolitan University Graduate School of Medicine, Osaka, Japan
Search for more papers by this authorTakeaki Ishizawa
Department of Hepatobiliary-Pancreatic Surgery, Osaka Metropolitan University Graduate School of Medicine, Osaka, Japan
Search for more papers by this authorAbstract
Aim
Hepatitis C virus (HCV) infection is a risk factor of intrahepatic cholangiocarcinoma (ICC). However, the impact of HCV infection control status on prognosis after surgery for ICCs is still unclear.
Methods
This multicenter retrospective study included patients who underwent curative resection for ICCs. The sera of 56 patients tested positive for anti-HCV antibody and negative for hepatitis B surface antigen (HCV group). Additionally, the sera of 358 patients tested negative for anti-HCV antibody and hepatitis B surface antigen (NBNC group). In the HCV group, 33 of 56 patients achieved sustained virologic response (SVR) for HCV (SVR group), whereas 23 patients did not (non-SVR group). To investigate the prognostic impact of HCV infection control status in the whole study cohort and in patients with solitary ICC without lymph node metastasis (StN0 study cohort), the postoperative prognosis of the SVR, non-SVR, and NBNC groups was compared.
Results
In the whole study cohort, there were no significant differences in terms of recurrence-free survival (RFS) or overall survival among the three groups. Based on the multivariate Cox regression analysis, non-SVR was an independent unfavorable prognostic factor of RFS. In the StN0 study cohort, the non-SVR group had a significantly lower RFS than the NBNC and SVR groups. Based on the multivariate analysis, non-SVR was an independent unfavorable prognostic factor of RFS.
Conclusions
The achievement of SVR for HCV infection in patients with HCV infection-related ICCs is associated with a better RFS after surgery for HCV-related ICCs, particularly solitary ICC without lymph node metastasis.
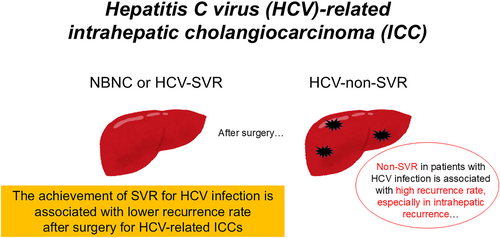
Graphical Abstract
The impact of hepatitis C virus (HCV) infection control on prognosis after surgery for intrahepatic cholangiocarcinomas (ICCs) is unclear. We revealed that the achievement of sustained viral reaction for HCV infection is associated with a better prognosis for HCV-related ICCs, particularly solitary ICC without lymph node metastasis.
CONFLICT OF INTEREST STATEMENT
Masaki Kaibori and Shoji Kubo are editorial board members of Hepatology Research. The other authors declare no conflicts of interest for this article.
Open Research
DATA AVAILABILITY STATEMENT
The data that supporting the findings of this study are not publicly available because it could compromise the privacy of research participants; however, the data are available from the corresponding author (M.K.) upon reasonable request.
REFERENCES
- 1Bridgewater J, Galle PR, Khan SA, Llovet JM, Park JW, Patel T, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014; 60(6): 1268–1289. https://doi.org/10.1016/j.jhep.2014.01.021
- 2Tyson GL, El-Serag HB. Risk factors for cholangiocarcinoma. Hepatology. 2011; 54(1): 173–184. https://doi.org/10.1002/hep.24351
- 3Shaib YH, El-Serag HB, Davila JA, Morgan R, McGlynn KA. Risk factors of intrahepatic cholangiocarcinoma in the United States: a case-control study. Gastroenterology. 2005; 128(3): 620–626. https://doi.org/10.1053/j.gastro.2004.12.048
- 4Kubo S, Kinoshita H, Hirohashi K, Hamba H. Hepatolithiasis associated with cholangiocarcinoma. World J Surg. 1995; 19(4): 637–641. https://doi.org/10.1007/bf00294744
- 5Uenishi T, Hamba H, Takemura S, Oba K, Ogawa M, Yamamoto T, et al. Outcomes of hepatic resection for hepatolithiasis. Am J Surg. 2009; 198(2): 199–202. https://doi.org/10.1016/j.amjsurg.2008.08.020
- 6Yamamoto S, Kubo S, Hai S, Uenishi T, Yamamoto T, Shuto T, et al. Hepatitis C virus infection as a likely etiology of intrahepatic cholangiocarcinoma. Cancer Sci. 2004; 95(7): 592–595. https://doi.org/10.1111/j.1349-7006.2004.tb02492.x
- 7Kinoshita M, Kubo S, Tanaka S, Takemura S, Nishioka T, Hamano G, et al. The association between non-alcoholic steatohepatitis and intrahepatic cholangiocarcinoma: a hospital based case-control study. J Surg Oncol. 2016; 113(7): 779–783. https://doi.org/10.1002/jso.24223
- 8Kubo S, Nakanuma Y, Takemura S, Sakata C, Urata Y, Nozawa A, et al. Case series of 17 patients with cholangiocarcinoma among young adult workers of a printing company in Japan. J Hepatobiliary Pancreat Sci. 2014; 21(7): 479–488. https://doi.org/10.1002/jhbp.86
- 9Kinoshita M, Kubo S, Nakanuma Y, Sato Y, Takemura S, Tanaka S, et al. Pathological spectrum of bile duct lesions from chronic bile duct injury to invasive cholangiocarcinoma corresponding to bile duct imaging findings of occupational cholangiocarcinoma. J Hepatobiliary Pancreat Sci. 2016; 23(2): 92–101. https://doi.org/10.1002/jhbp.305
- 10Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, et al. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020; 76(2): 182–188. https://doi.org/10.1111/his.13975
- 11Kinoshita M, Sato Y, Shinkawa H, Kimura K, Ohira G, Nishio K, et al. Impact of tumor subclassifications for identifying an appropriate surgical strategy in patients with intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2024; 31(4): 2579–2590. https://doi.org/10.1245/s10434-023-14833-1
- 12Toyoda H, Tada T, Johnson PJ, Izumi N, Kadoya M, Kaneko S, et al. Validation of serological models for staging and prognostication of HCC in patients from a Japanese nationwide survey. J Gastroenterol. 2017; 52(10): 1112–1121. https://doi.org/10.1007/s00535-017-1321-6
- 13Kudo M, Izumi N, Kubo S, Kokudo N, Sakamoto M, Shiina S, et al. Report of the 20th Nationwide follow-up survey of primary liver cancer in Japan. Hepatol Res. 2020; 50(1): 15–46. https://doi.org/10.1111/hepr.13438
- 14Tanaka S, Shinkawa H, Tamori A, Takemura S, Uchida-Kobayashi S, Amano R, et al. Postoperative direct-acting antiviral treatment after liver resection in patients with hepatitis C virus-related hepatocellular carcinoma. Hepatol Res. 2021; 51(11): 1102–1114. https://doi.org/10.1111/hepr.13709
- 15Tanaka S, Shinkawa H, Tamori A, Takemura S, Takahashi S, Amano R, et al. Surgical outcomes for hepatocellular carcinoma detected after hepatitis C virus eradiation by direct-acting antivirals. J Surg Oncol. 2020; 122(8): 1543–1552. https://doi.org/10.1002/jso.26184
- 16Koda M, Tanaka S, Takemura S, Shinkawa H, Kinoshita M, Hamano G, et al. Long-term prognostic factors after hepatic resection for hepatitis C virus-related hepatocellular carcinoma, with a special reference to viral status. Liver Cancer. 2018; 7(3): 261–276. https://doi.org/10.1159/000486902
- 17Tanaka S, Tamori A, Takemura S, Hamano G, Ito T, Kawada N, et al. Surgical outcomes in hepatitis C virus-related hepatocellular carcinoma: special reference to sustained virological responses to interferon therapy. Am Surg. 2017; 83(11): 1246–1255. https://doi.org/10.1177/000313481708301127
- 18Uchiyama K, Yamamoto M, Yamaue H, Ariizumi S, Aoki T, Kokudo N, et al. Impact of nodal involvement on surgical outcomes of intrahepatic cholangiocarcinoma: a multicenter analysis by the study group for Hepatic Surgery of the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepatobil Pancreat Sci. 2011; 18(3): 443–452. https://doi.org/10.1007/s00534-010-0349-2
- 19Uenishi T, Ariizumi S, Aoki T, Ebata T, Ohtsuka M, Tanaka E, et al. Proposal of a new staging system for mass-forming intrahepatic cholangiocarcinoma: a multicenter analysis by the study group for Hepatic Surgery of the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepatobiliary Pancreat Sci. 2014; 21(7): 499–508. https://doi.org/10.1002/jhbp.92
- 20Yamamoto M, Ariizumi S. Surgical outcomes of intrahepatic cholangiocarcinoma. Surg Today. 2011; 41(7): 896–902. https://doi.org/10.1007/s00595-011-4517-z
- 21Ariizumi SI, Kotera Y, Takahashi Y, Katagiri S, Chen IP, Ota T, et al. Mass-forming intrahepatic cholangiocarcinoma with marked enhancement on arterial-phase computed tomography reflects favorable surgical outcomes. J Surg Oncol. 2011; 104(2): 130–139. https://doi.org/10.1002/jso.21917
- 22Okabayashi T, Yamamoto J, Kosuge T, Shimada K, Yamasaki S, Takayama T, et al. A new staging system for mass-forming intrahepatic cholangiocarcinoma: analysis of preoperative and postoperative variables. Cancer. 2001; 92(9): 2374–2383. https://doi.org/10.1002/1097-0142(20011101)92:9<2374::aid-cncr1585>3.0.co;2-l
10.1002/1097-0142(20011101)92:9<2374::AID-CNCR1585>3.0.CO;2-L CAS PubMed Web of Science® Google Scholar
- 23Kubo S, Shinkawa H, Asaoka Y, Ioka T, Igaki H, Izumi N, et al. Liver Cancer Study Group of Japan clinical practice guidelines for intrahepatic cholangiocarcinoma. Liver Cancer. 2022; 11(4): 290–314. https://doi.org/10.1159/000522403
- 24 American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2003; 26(Suppl l_1): S33–S50. https://doi.org/10.2337/diacare.25.2007.s33
- 25Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015; 33(6): 550–558. https://doi.org/10.1200/jco.2014.57.9151
- 26Hiraoka A, Michitaka K, Kumada T, Izumi N, Kadoya M, Kokudo N, et al. Validation and potential of albumin-bilirubin grade and prognostication in a nationwide survey of 46,681 hepatocellular carcinoma patients in Japan: the need for a more detailed evaluation of hepatic function. Liver Cancer. 2017; 6(4): 325–336. https://doi.org/10.1159/000479984
- 27Kudo M, Izumi N, Kokudo N, Sakamoto M, Shiina S, Takayama T, et al. Report of the 22nd nationwide follow-up survey of primary liver cancer in Japan (2012–2013). Hepatol Res. 2022; 52(1): 5–66. https://doi.org/10.1111/hepr.13675
- 28Sakamoto Y, Kokudo N, Matsuyama Y, Sakamoto M, Izumi N, Kadoya M, et al. Proposal of a new staging system for intrahepatic cholangiocarcinoma: analysis of surgical patients from a nationwide survey of the Liver Cancer Study Group of Japan. Cancer. 2016; 122(1): 61–70. https://doi.org/10.1002/cncr.29686
- 29Zhang XF, Bagante F, Chakedis J, Moris D, Beal EW, Weiss M, et al. Perioperative and long-term outcome for intrahepatic cholangiocarcinoma: impact of major versus minor hepatectomy. J Gastrointest Surg. 2017; 21(11): 1841–1850. https://doi.org/10.1007/s11605-017-3499-6
- 30Lv Y, Liu H, He P, Xie S, Yin X, Cai Y, et al. A novel model for predicting the prognosis of postoperative intrahepatic cholangiocarcinoma patients. Sci Rep. 2023; 13(1):19267. https://doi.org/10.1038/s41598-023-45056-9
- 31Wang J, Qiu Y, Yang Y, Shen S, Zhi M, Zhang B, et al. Impact of cirrhosis on long-term survival outcomes of patients with intrahepatic cholangiocarcinoma. Cancer Med. 2022; 11(19): 3633–3642. https://doi.org/10.1002/cam4.4740
- 32Iida H, Kaibori M, Tanaka S, Takemura S, Wada H, Hirokawa F, et al. Low incidence of lymph node metastasis after resection of hepatitis virus-related intrahepatic cholangiocarcinoma. World J Surg. 2017; 41(4): 1082–1088. https://doi.org/10.1007/s00268-016-3843-0
- 33Kaibori M, Yoshii K, Kashiwabara K, Kokudo T, Hasegawa K, Izumi N, et al. Impact of hepatitis C virus on survival in patients undergoing resection of intrahepatic cholangiocarcinoma: report of a Japanese nationwide survey. Hepatol Res. 2021; 51(8): 890–901. https://doi.org/10.1111/hepr.13676
- 34Luh F, Kuei A, Fann P, Chu P, Yen Y. Intrahepatic cholangiocarcinoma and hepatitis: case study and literature review. Anticancer Res. 2009; 29: 3239–3243.
- 35Liu W, Chen JR, Hsu CH, Li YH, Chen YM, Lin CY, et al. A zebrafish model of intrahepatic cholangiocarcinoma by dual expression of hepatitis B virus X and hepatitis C virus core protein in liver. Hepatology. 2012; 56(6): 2268–2276. https://doi.org/10.1002/hep.25914
- 36Fujimoto A, Furuta M, Shiraishi Y, Gotoh K, Kawakami Y, Arihiro K, et al. Whole-genome mutational landscape of liver cancers displaying biliary phenotype reveals hepatitis impact and molecular diversity. Nat Commun. 2015; 6(1):6120. https://doi.org/10.1038/ncomms7120
- 37Uenishi T, Nishiguchi S, Tanaka S, Yamamoto T, Takemura S, Kubo S. Response to interferon therapy affects risk factors for postoperative recurrence of hepatitis C virus-related hepatocellular carcinoma. J Surg Oncol. 2008; 98(5): 358–362. https://doi.org/10.1002/jso.21111
- 38Tsai CY, Wang SY, Chan KM, Lee WC, Chen TC, Yeh TS, et al. Hepatectomy or/with metastatectomy for recurrent intrahepatic cholangiocarcinoma: of promise for selected patients. J Personalized Med. 2022; 12(4):540. https://doi.org/10.3390/jpm12040540
- 39Sulpice L, Rayar M, Boucher E, Pracht M, Meunier B, Boudjema K. Treatment of recurrent intrahepatic cholangiocarcinoma. Br J Surg. 2012; 99(12): 1711–1717. https://doi.org/10.1002/bjs.8953
- 40Kaneko S, Kurosaki M, Tsuchiya K, Yasui Y, Inada K, Kirino S, et al. Prognosis of intrahepatic cholangiocarcinoma stratified by albumin-bilirubin grade. Hepatol Res. 2021; 51: 902–908. https://doi.org/10.1111/hepr.13673
- 41Tsilimigras DI, Hyer JM, Moris D, Sahara K, Bagante F, Guglielmi A, et al. Prognostic utility of albumin-bilirubin grade for short- and long-term outcomes following hepatic resection for intrahepatic cholangiocarcinoma: a multi-institutional analysis of 706 patients. J Surg Oncol. 2019; 120(2): 206–213. https://doi.org/10.1002/jso.25486
- 42Kobayashi S, Ikeda M, Nakachi K, Ueno M, Okusaka T, Todaka A, et al. A multicenter survey on eligibility for a randomized Phase III trial of adjuvant chemotherapy for resected biliary tract cancer (JCOG1202, ASCOT). Ann Surg Oncol. 2023; 30(12): 7331–7337. https://doi.org/10.1245/s10434-023-13913-6