Over- and underreporting of seizures: How big is the problem?
Abstract
Objective
Clinical decisions on managing epilepsy patients rely on patient accuracy regarding seizure reporting. Studies have noted disparities between patient-reported seizures and electroencephalographic (EEG) findings during video-EEG monitoring periods, chiefly highlighting underreporting of seizures, a well-recognized phenomenon. However, seizure overreporting is a significant problem discussed within the literature, although not in such a large cohort. Our aim is to quantify the over- and underreporting of seizures in a large cohort of ambulatory EEG patients.
Methods
We performed a retrospective data analysis on 3407 patients referred to a diagnostic service for ambulatory video-EEG between 2020 and 2022. Both patient-reported events and events discovered on review of the video-EEG were analyzed and classified as epileptic, psychogenic (typically clinical motor events, without accompanying EEG change), or noncorrelated events (NCEs; without perceivable clinical or EEG change). Events were analyzed by state of arousal and indication for referral. Subgroup analysis was performed in patients with focal and generalized epilepsies.
Results
A total of 21 024 events were recorded by 3407 patients. Fifty-eight percent of reported events were NCEs, whereas 27% of all events were epileptic. Sixty-four percent of epileptic seizures were not reported by the patient but discovered by the clinical service on review of the recording. NCEs were in the highest proportion in the awake and drowsy arousal states and were the most common event type for the majority of referral indications. Subgroup analysis found a significantly higher proportion of NCEs in the patients with focal epilepsy (23%) compared to generalized epilepsy (10%; p < .001, chi-squared proportion test).
Significance
Our results reaffirm the phenomenon of underreporting and highlight the prevalence of overreporting. Overreporting likely represents irrelevant symptoms or electrographic discharges not represented on scalp electrodes, identification of which has important clinical relevance. Future studies should analyze events by risk factors to elucidate relationships clinicians can use and investigate the etiology of NCEs.
Key Points
- NCEs constituted the highest occurrence among patients, comprising 58% of all recorded events, and 75% of studies recorded at least one NCE
- NCEs likely represent irrelevant symptoms or discharges not detected by scalp electrodes
- Sixty-four percent of all epileptic events were not reported by the patient but discovered by the clinical service on review of the recording
- Subgroup analysis of patients with focal versus generalized epilepsies found NCEs more prevalent in the focal group
- Continuing to identify risk factors for misreporting will hopefully improve clinical management of people with epilepsy
1 INTRODUCTION
A key issue with self-reported seizure frequency assessment is accuracy. Seizure reporting is predominantly obtained from patient histories or caregiver collateral histories, which neurologists state substantially influences management decisions, particularly with respect to antiseizure medications (ASMs).1, 2 Despite this reliance, neurologists believe that patients inaccurately report 40%–60% of their seizures,1 and most patients have been found to overestimate their ability to recognize seizures.3 Patients are aware that they underreport their seizures4 and utilize seizure diaries to address this problem, but these diaries have been fraught with inaccuracies.2, 5 Underreporting is a well-defined phenomenon in the literature. It has been explained by three impairments—perception, volition, and memory—with perception considered the chief culprit,6 whereas others suggest lack of seizure awareness to be the driver.2 Notably, one study found that 55% of all seizures were undocumented,5 with other studies noting similar rates of underreporting.7-11 In contrast, overreporting has begun to garner attention. Recently, patients with absence seizures were found to either over- or underreport their seizures but never both, positing personality traits as a possible explanation.12 Overreporting may comprise irrelevant symptoms misinterpreted by the patient or high false positives during studies to avoid any missed seizures,13 or they may represent clinically relevant events without scalp electroencephalographic (EEG) representation.10
Although studies have described the phenomena of over- and underreporting seizures,7-10, 12, 13 such analysis has not been performed in a large cohort. The size of our cohort demonstrates the magnitude of over- and underreporting of seizures. Our study assessed the quantum of over- and underreporting seizures in a single-center retrospective cohort of patients who underwent ambulatory video-EEG monitoring (avEEG) over a 2-year period.
2 MATERIALS AND METHODS
2.1 Study design
This was a retrospective chart review to determine the quantum of over- and underreported seizures. We obtained avEEG data from a diagnostic facility (Seer Medical Australia, Melbourne, Australia) that undertook studies at 24 sites across Australia. Ethics approval for this study was obtained from the St. Vincent's Hospital Melbourne Human Research Ethics Committee (project number 57392).
2.2 Ambulatory video-EEG monitoring
The avEEG used 10–20 EEG electrode placement, a 256 samples-per-second EEG recording device, and Bluetooth hardware for remote real-time monitoring of video and EEG traces. Recording periods were between 3 and 7 days. Events were logged by patients or carers through a mobile phone app. Additionally, a continuous three-channel electrocardiogram (ECG) was recorded throughout the study. Seizure and spike detection software was used to generate annotations of the date.14 Then the entire avEEG study was reviewed by a technician, and sections of clinical interest were flagged. The neurologist reporting assessed flagged segments, as well as the reported events and any additional events discovered by the EEG technicians or later reported by witnesses. Finally, the neurologist provided a conclusion.15 The data was reviewed as part of a clinical service, and the review protocol was tailored to each question. Full human review of the recording may have been required when indicated, such as cases of medicolegal or driving-related investigations, or if EEG negative seizures were likely. Automated analyses screened the EEG for interictal abnormalities only. Automated analysis also screened the ECG for abnormal morphologies, beat timings, and episodes of bradycardia and tachycardia.
2.3 Data collection
The data was collected over a 2-year period from April 2020 to April 2022 from patients who recorded at least one event. A recorded event is one that was either reported by the patient and/or caregiver, or detected by clinical staff on review of the recording because of clear clinical manifestations and EEG changes. Included in the data were age of patient, patient description of event, technician interpretation of video and EEG, arousal state of the patient, the neurologist's conclusion of the patients reporting period, and the referral information from the patient's treating clinician. The arousal state was determined as the state of the patient at the start of the event as determined by the reviewing neurologist. Each event was analyzed by assessing the patient's description, EEG and video notes, and the neurologist's conclusion. Using this information, each event was allocated as either epileptic, psychogenic nonepileptic seizure (PNES), noncorrelated event (NCE), cardiac, EEG not interpretable, data not available, or not relevant. We deemed PNES to be typically motor symptoms described on the video notes without EEG correlate; less often, these consisted of episodes of unresponsiveness or altered behavior. We deemed NCEs to be events without perceivable clinical or EEG correlate, but described by the patient as a "typical event." "Data not available" refers to the patient not being connected to the equipment, or loss of data for technical reasons. "Not relevant" events were those discovered by the technician for review but deemed not relevant by the neurologist. Furthermore, each study was categorized by the patient's referral type as diagnostic, characterizing the nature of the patient's seizures, assessing seizures in response to treatment, or a combination of the latter two. These categories represent the indications for monitoring established for reimbursement purposes by the Australian national health insurance authority, Medicare.
Patients with epileptic seizures were classified as having focal or generalized epilepsies based on the reporting neurologist's conclusion using the 2017 International League Against Epilepsy definitions.16
2.4 Data analysis
In this study, we analyzed the over- and underreporting of seizures. Overreporting was analyzed by the state of arousal and referral indication. Chi-squared proportion tests were performed on epileptic and NCE events by state of arousal, and by indication for referral, setting significance at α = .05. For underreported events, we analyzed the number of discovered epileptic seizures in total and based on the state of arousal.
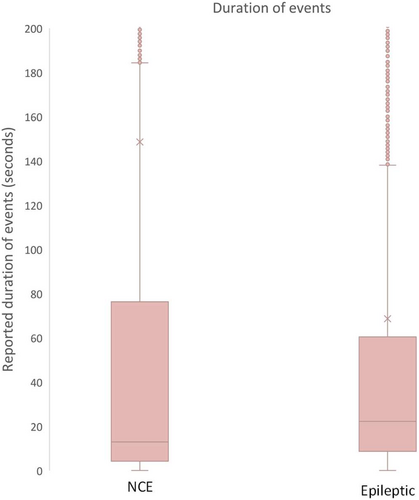
We compared the duration of epileptic seizures with NCEs with box and whisker plots. Wilcoxon rank sum tests were performed to determine whether groups were drawn from statistically similar distributions.
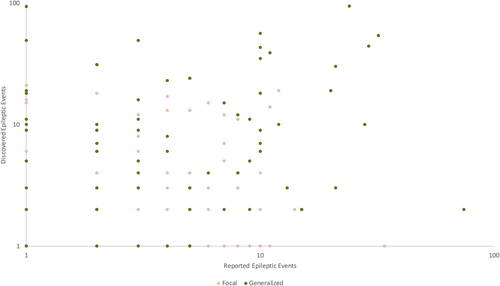
We performed subgroup analysis on patients with confirmed epilepsies based on the neurologist's conclusion and categorized them as either focal or generalized epilepsies. We performed chi-squared proportion tests on the types of events reported between the focal and generalized epilepsy groups. Additionally, we analyzed discovered epileptic event count as a function of reported epileptic event count.
All significance tests set significance at α = .05.
3 RESULTS
3.1 Overview
We analyzed avEEG recordings with at least one event from 3407 recordings, yielding 21 024 events as shown in Table 1. This population included pediatric and adult patients ranging from 1 to 97 years old with a median age of 34 years. Of the 3407 recordings, 79 of the patients had more than one study (74 patients had two studies, four patients had three studies, and one patient had more than three studies). The recordings with duplicate studies included a median of 10 events reported, with a minimum of two events and a maximum of 110 events. Most events captured were NCEs (58%), followed by epileptic seizures (27%) and then PNESs (6%). Events that were not interpretable or with no data made up 8% of total recordings, and <1% were cardiac events. NCEs were recorded in 75% of studies (2549), interictal epileptiform discharges (IEDs) in 42% of studies (1412), and 33% (1120) of studies recorded both NCEs and IEDs.
| Patients, n | 3322 |
| Studies, n | 3407 |
| Gender, F | 60.3% |
| Age, years, median (range) | 34 (1–97) |
| Number of ASMs | |
| 0 | 1420 (43%) |
| 1 | 853 (26%) |
| 2 | 574 (17%) |
| 3 | 279 (8%) |
| 4 | 120 (4%) |
| +4 | 76 (2%) |
| Referral indication | |
| Diagnostic | 2223 (65%) |
| Characterizing seizures | 706 (21%) |
| Assessment of treatment | 258 (8%) |
| Characterizing seizures and assessment of treatment | 220 (6%) |
| Study analysis | |
| Studies with epileptiform activity, n | 1675 (49%) |
| Studies with epileptic seizures, n | 765 (22%) |
| Focal epilepsy | 478 (62%) |
| Generalized epilepsy | 287 (38%) |
| Epileptic patients with NCEs | 712 (93%) |
| Studies with PNESs, n | 365 (11%) |
| Studies with cardiac etiologies, n | 14 (<1%) |
| Studies with normal recordings, n | 1353 (40%) |
- Abbreviations: ASM, antiseizure medication; NCE, noncorrelated event; PNES, psychogenic nonepileptic seizure.
We performed supplementary analysis on age and reporting. We observed a small, negative, nonsignificant relationship between age and mean reported events (r2 = .21, p < .001), and a small, positive, nonsignificant relationship between age and NCEs as a percentage of total reported events (r2 = .26, p < .001).
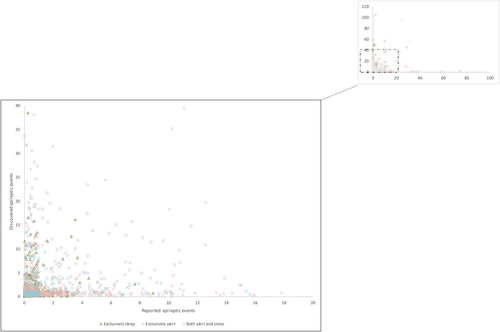
3.2 Epileptic seizures
With respect to epileptic seizures, most were discovered, representing 64% of all epileptic seizures as shown in Table 2. In the awake state, epileptic seizures were almost evenly discovered and reported by patients, 55% and 45%, respectively. The proportion of reported epileptic seizures was higher in the drowsy state, 72%, and even higher in the asleep state, 77%. This observation of discovered events in the awake state and patients who reported no events but had discovered events in the sleep state is further illustrated in Figure 1.
| Discovered | Reported | Total | |
|---|---|---|---|
| Total epileptic events | 3682 (64%) | 2057 (36%) | 5739 (100%) |
| Epileptic events by arousal state | |||
| Awake | 1943 (55%) | 1567 (45%) | 3510 (100%) |
| Drowsy | 140 (72%) | 54 (28%) | 194 (100%) |
| Asleep | 1181 (77%) | 357 (23%) | 1538 (100%) |
| Not stated | 418 (84%) | 79 (16%) | 497 (100%) |
3.3 Events by arousal state
Most events were reported in the awake state, representing 75% of total events, as shown in Table 3. In the asleep state, the category of event reported most frequently was epileptic, at 52%. In contrast, the awake and drowsy state's highest frequency category was NCEs at 63% and 58%, respectively. Additionally, a high frequency of NCEs was observed in the asleep state at 40%. In all states except drowsy, there was a significant difference between epileptic events and NCEs (Wilcoxon rank sum test).
| Events per patient, n, median (range) | 4 (1–118) |
| Events, n | 21 024 (100%) |
| Epileptic | 5739 (27%) |
| NCE | 12 239 (58%) |
| PNES | 1310 (6%) |
| Cardiac | 23 (<1%) |
| Not relevant | 132 (1%) |
| Not interpretable | 666 (3%) |
| No data | 915 (5%) |
| Arousal state | Awake | Asleep | Drowsy | Not stated |
|---|---|---|---|---|
| Epileptic | 3510 (22%) | 1538 (52%) | 194 (28%) | 497 (32%) |
| NCE | 9883 (63%) | 1190 (40%) | 398 (58%) | 768 (50%) |
| Test statistic | −28.1 | 29.77 | .46 | 5.8 |
| p | <.001 | <.001 | .65 | <.001 |
| PNES | 1047 (7%) | 86 (3%) | 54 (8%) | 123 (8%) |
| Cardiac | 19 (<1%) | 1 (<1%) | 0 (0%) | 3 (<1%) |
| Not interpretable | 460 (3%) | 103 (3%) | 31 (5%) | 72 (5%) |
| No data | 778 (5%) | 57 (2%) | 7 (1%) | 73 (5%) |
| Total | 15 697 (100%) | 2975 (100%) | 684 (100%) | 1536 (100%) |
| Indication | Diagnostic | Characterizing seizures | Assessment of treatment | Characterizing seizures and assessment of treatment |
|---|---|---|---|---|
| Epileptic | 2508 (19%) | 1717 (39%) | 1043 (59%) | 471 (34%) |
| NCE | 8496 (64%) | 2329 (52%) | 654 (37%) | 760 (55%) |
| Test statistic | −33.05 | 16.36 | 27.45 | 5.00 |
| p | <.001 | <.001 | <.001 | <.001 |
| PNES | 1119 (8%) | 160 (4%) | 7 (<1%) | 24 (2%) |
| Cardiac | 22 (<1%) | 1 (<1%) | 0 (0%) | 0 (0%) |
| Not interpretable | 387 (3%) | 128 (3%) | 41 (2%) | 110 (8%) |
| No data | 765 (6%) | 102 (2%) | 19 (1%) | 29 (2%) |
| Total | 13 297 (100%) | 4437 (100%) | 1764 (100%) | 1394 (100%) |
| Subgroup analysis | Focal | Generalized | Test statistic | p |
|---|---|---|---|---|
| Total number of events | 3203 (100%) | 3943 (100%) | ||
| Epileptic | 2288 (71%) | 3451 (88%) | −17.01 | <.001 |
| NCE | 742 (23%) | 397 (10%) | 15.04 | <.001 |
| PNES | 9 (<1%) | 7 (<1%) | .92 | .36 |
| Not relevant | 16 (<1%) | 8 (<1%) | 2.16 | .03 |
| Not interpretable | 115 (4%) | 44 (1%) | 7.05 | <.001 |
| No data | 33 (1%) | 36 (1%) | .50 | .61 |
- Note: Percentages shown are based on column total. Chi-squared proportions tests were performed between epileptic events and NCEs. Subgroup summary of patients with focal and generalized epilepsies is shown. Chi-squared proportions tests were performed. Results that were significant are shown in bold.
- Abbreviations: NCE, noncorrelated event; PNES, psychogenic nonepileptic seizure.
3.4 Events by diagnostic referral
Most (64% of total events) occurred in referrals performed for diagnostic purposes, followed by those performed for characterization of seizures (at 22%), as shown in Table 3. NCEs made up the highest proportion in each referral category except assessment of treatment, where 59% of all events were epileptic. In contrast, epileptic seizures were lower in the diagnostic, characterizing seizures, and characterizing seizures plus assessment of treatment groups (19%, 39%, and 34%, respectively). For all indications for referrals, there was a significant difference between epileptic seizures and NCEs (Wilcoxon rank sum test; Figure 2).
3.5 Focal versus generalized subgroup analysis
Of the 765 patients with epilepsy, 478 (62%) had a focal epilepsy and 287 (38%) had a generalized epilepsy. The highest proportion of events in both groups was epileptic; however, the focal group reported a significantly greater proportion of NCEs than the generalized group (focal, 23% NCEs; generalized, 10% NCEs; p < .001), as noted in Table 3. Both groups had more discovered epileptic seizures than reported (focal, 56% discovered; generalized, 70% discovered). We plotted discovered epileptic seizures by reported epileptic seizures and found that participants with generalized epilepsies had a greater variance of discovered events compared to patients with focal epilepsies (variance, generalized = 7.20; variance, focal = 1.80), as noted in Figure 3. No linear correlations were found between these two groups (generalized, R2 = .01, p = .36; focal, R2 = .01, p = .02).
4 DISCUSSION
In this study, we described the magnitude of over- and underreporting of seizures. With respect to underreporting of seizures, we found 64% of all epileptic seizures were unreported and discovered only on review of the data. Unsurprisingly, a large proportion of events in the asleep state were discovered (77%), but alarmingly 55% of seizures in the awake state were also discovered episodes. Our study includes a large population relative to the existing literature, which reinforces the phenomenon of underreporting.5 This also illustrates the importance of clinicians' skepticism regarding patient seizure counts. Conversely, our other major finding was the quantum of overreporting, with 58% of all events being NCEs. Furthermore, the proportion of NCEs was significantly different from epileptic seizures in all states of arousal (except drowsy) and all indications for referrals. Given the magnitude of NCEs in our study, future research is warranted to elucidate their importance within epilepsy management, as well as common symptoms reported during these events.
Our results relating to discovered seizures are consistent with other studies3, 5, 7 and align with the proposed perception impairment to underreporting. Consistently, the sleep state produced the highest proportion of discovered events when a patient's perception was most impaired. Therefore, the discovered events in the awake state are likely to be related to a deficit in perception too. Comparably, an inpatient video-EEG study found 85.8% of seizures in sleep were discovered.5 This higher proportion may be related to characteristics of inpatient evaluation including ASM withdrawal, sleep deprivation, and acclimatizing to an unfamiliar environment. avEEG does not enforce such conditions on patients and allows them to remain in their own home, one of the key strengths of avEEG17 and our results. However, multiple factors have been identified to impact seizure reporting including seizure localization, preictal vigilance memory function, and seizure type.18 With respect to seizure type, one study observed 52% of patients with epilepsy were unaware of focal seizures and 69% of focal to bilateral tonic–clonic seizures.19 This is consistent with our subgroup analysis: 56% discovered in our focal epilepsy group and 70% discovered in our generalized epilepsy group. These results suggest the quantum of underreporting differs by type of epilepsy and would help neurologists stratify likelihood of underreporting when evaluating a patient with a focal or generalized epilepsy. However, our study did not control for the other variables mentioned (seizure localization, preictal vigilance, and memory function). Future research should analyze these relationships as this would best help elucidate risk factors for underreporting.
Overreporting has been observed in several avEEG studies with similarly high proportions.8-10, 20, 21 Additionally, we note the low count of cardiac events, which makes a cardiogenic etiology less likely. The question remains as to what NCEs most likely represent: irrelevant nonepileptic symptoms, or seizures not detectable on scalp EEGs because of deep origin or involving insufficient cortical extent.22 Although the highest proportions of NCEs were observed in the awake and drowsy state, surprisingly 40% of events in the asleep state were also NCEs. Because a large a proportion of patients are either waking from sleep to record an NCE or remembering to record an NCE the next morning, the perceptual disturbance described in ictal events does not impair their recount, lending weight to the irrelevant symptom argument. However, NCEs were also prevalent in the population with known epilepsy diagnoses, constituting 37% of events in the assessment of treatment population. Additionally, 69% of studies with interictal discharges reported at least one NCE. NCEs may indicate events that feature EEG discharges that are undetectable on scalp recordings. Studies of simultaneous scalp and intracranial EEG have shown approximately one third of focal aware and subclinical seizures are not seen on scalp recordings.23 Furthermore, we observed significant differences between the proportions of epileptic seizures and NCEs based on indication for referral and state of arousal. Importantly, these observations were consistent with what would be expected; the treatment population that had been diagnosed with epilepsy had a significantly higher proportion of epileptic seizures than NCEs. When we consider these results together with the differences in reported duration of the two events, which were also significant, NCEs and epileptic seizures possess different characteristics. It may be event specific or patient specific. Recently, a study on absence seizure reporting found that patients over- or underreported seizures, never both, positing personality traits or some other intrinsic difference.12 Therefore, more in-depth analysis of the characteristics of NCEs and epileptic seizures is warranted.
Within our subgroup analysis, overreporting was significantly more prevalent in patients with focal epilepsy compared to participants with generalized epilepsy. This is most likely related to seizure phenotypes. Patients with generalized seizures do not usually feature psychic or other experiential phenomenon, although overreporting has been reported in this context also.13 In contrast, normal experiential, sensory, or motor phenomenon may be interpreted as related to the patient's typical focal seizure activity, as it may have a similar quality, resulting in more NCEs being reported as these ordinary experiences are overinterpreted. Therefore, knowing whether a patient has a focal epilepsy may increase a neurologist's suspicion that the number of reported events may be overstated. Although it has been shown that scalp EEG detects one third of true electrographic focal seizures compared to invasive electrodes,23 the events described here have no clinical correlate, and require a different therapeutic perspective. Given the size of our study, we were unable to perform such analysis, but future studies with subgroups may yield results that are similarly beneficial to clinicians.
Our study has several limitations. As a retrospective data analysis, we were unable to draw any conclusions about causation, and our population was limited to patients who underwent monitoring at a commercial diagnostic facility, which may result in selection bias. Furthermore, we used a heterogenous cohort and did not stratify our observations by potentially confounding factors such as semiology, comorbidities, or socioeconomic status, all of which may influence our observations. Additionally, psychiatric comorbidities (which were not considered in this study) have been discussed to have an influence on both epileptic seizures and NCEs.13 Another consideration is the home environment and whether the presence or absence of relatives and carers impacted seizure frequency. Seizure reporting was also sometimes performed collaterally in the case of young patients or patients with comorbidities. Additionally, our definition of PNESs excluded sensory symptoms, and an expanded definition may have lowered the proportion of NCEs. Finally, we must consider the modality of reporting in our study. Patients undergoing an avEEG study may have a low threshold to event reporting to ensure a relevant event is captured, and thus this may lead to irrelevant symptom reporting. To combat irrelevant symptom reporting for outpatient monitoring and clinical studies, standardization of reported events may need to be implemented.10 A successful event requires patients to record the event as typical or atypical and be cross-checked by the interpreting clinician.
Future studies should be targeted toward understanding the basis of NCEs. High proportions are reported in multiple studies, and our results further illustrate this. The disparity between confirmed clinically relevant seizure activity and both over- and underreporting of events highlights the potential role for both subscalp and deeply implanted EEG devices,2 currently being investigated for clinical utility in the management of epilepsy.24, 25
5 CONCLUSIONS
We performed a retrospective data analysis on a large cohort of patients referred for avEEG to determine the quantum of over- and underreporting of seizures. Of 21 024 events, we found that 58% were NCEs, representing overreporting. These may represent irrelevant symptoms, overinterpreted by the patient, or epileptic seizures without scalp EEG correlation. With respect to underreporting, 64% of all epileptic seizures were discovered. The highest proportion was in the asleep state at 77%, but more than half of events in the awake state were also discovered. Our subgroup analysis yielded consistent observations of increased discovered events in patients with generalized epilepsies when compared to focal epilepsies. These results are consistent with the known issue of underreporting of seizures. Whereas this study provides insight into the magnitude of the problem, future studies should be directed at evaluating the causal factors of misreporting of seizures. Understanding the risk factors behind seizure over- and underreporting would be most beneficial to neurologists when evaluating patient histories to better inform clinical management decisions.
AUTHOR CONTRIBUTIONS
Ewan S. Nurse and Mark J. Cook conceptualized the study. Timothy Hannon wrote the manuscript. Ewan S. Nurse and Mark J. Cook reviewed and edited the manuscript. Timothy Hannon, Victoria Wong, and Kiran M. Fernandes conducted data curation and analysis.
ACKNOWLEDGMENTS
None. Open access publishing facilitated by The University of Melbourne, as part of the Wiley - The University of Melbourne agreement via the Council of Australian University Librarians.
CONFLICT OF INTEREST STATEMENT
E.S.N. and M.J.C. declare a financial interest in Seer Medical. None of the other authors has any conflict of interest.
ETHICS STATEMENT
Ethics approval for this study was approved by the St. Vincent's Hospital Melbourne Human Research Ethics Committee under project 57 392. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Open Research
DATA AVAILABILITY STATEMENT
The data used in this work are available upon reasonable request to the corresponding author.