Prevalence and predictors of psychosocial problems in informal caregivers of older cancer survivors – A systematic review: Still major gaps in current research
Funding information
This research was funded by Kom op tegen Kanker, the campaign of the Vlaamse Liga tegen Kanker VZW.
Abstract
Despite the abundance of studies concerning caring for patients with cancer, less is known about caring for an older cancer survivor (≥65 years). We aimed to systematically gather literature about the psychosocial well-being of caregivers of older cancer survivors and to identify possible risk factors for developing psychosocial problems. Fourteen articles met the following inclusion criteria: articles about (a) cancer, (b) informal caregivers, (c) older survivors and a (d) curative setting. After critical appraisal, nearly all were considered to be of moderate-to-strong quality. This results mainly from the specific study population, the valid and reliable measurement instruments and the appropriate statistical methods used in the articles. Main outcomes were burden, depression, anxiety, self-esteem, distress, communication issues, stress and QoL. For all these outcomes, measurement instruments and timing of measurements vary. Also, the results on studied predictors vary widely or not all of them were described in the reviewed articles. There seems to be a higher prevalence of distress, lower QoL and more anxiety in informal caregivers of older cancer survivors compared with the general population, but all were understudied. Based on these results and more focused future research, specific and qualitative support for this group of caregivers can be developed.
1 INTRODUCTION
Worldwide an estimated 14 million people were diagnosed with cancer in 2012 and this is expected to increase to 24 million by 2035 (Ferlay et al., 2013). A cancer diagnosis has a profound impact on the patient and his/her relatives. Increasingly, cancer becomes manageable or treatable, resulting in a number of concerns such as poorer functioning and dealing with more comorbidities (Avis & Deimling, 2008). Cancer incidence increases with age: individuals aged 65 and older account for 70% of all patients with a new cancer diagnosis in the Western world (Goldzweig et al., 2013; Yancik, 2005).
Older patients (≥65 years), like younger cancer patients, must cope with side effects of the cancer treatment. In addition, they have to deal with comorbidities and other consequences of ageing such as a changed sleeping pattern or reduced mobility. As a result of the current shift from inpatient to outpatient treatment and aftercare, older people will increasingly be cared by informal caregivers (Given & Sherwood, 2006; Haley, 2013; Kim & Given, 2008). A second shift in the current health care is the change from cure to care. Depending on patient's preferences and cancer stage, the focus can be on curing the tumour, or more on the needs and the quality of life of the patient, whereby the required intervention depends on the individual patient perspective. A paternalistic approach with the patient as passive partner is gradually disappearing. The new keyword is “Patient Empowerment” where patients take more responsibility for their own health situation and are encouraged to handle their problems with information, not directives, from professional caregivers. Both shifts reflect greater involvement of the older patient with cancer and more responsibilities for the informal caregiver. This is expected to cause an increase in psychosocial problems in informal caregivers of these older patients with cancer.
The care for a relative or friend with cancer includes a variety of tasks such as delivering emotional and physical support, but also daily care and the logistic organization of patient care, all of which can put a burden on the caregiver. Because of these care tasks, caregivers of patients with cancer (tend to) experience more stress-related symptoms than noncaregivers (Goren, Gilloteau, Lees, & DaCosta, 2014). They can also encounter sleep difficulties which may in turn enhance a decreased psychosocial and physical well-being (Carter & Chang, 2000; Scheen, Byrne, Plat, Leproult, & Van Cauter, 1996). Other problems caregivers of patients with cancer might be confronted with, are a dysregulation of pro- and anti-inflammatory signalling pathways, gain or loss of weight and negative changes in life style habits such as less exercise, eating less healthy and consuming more alcohol (Beesley, Price, & Webb, 2011; Klassen et al., 2012). All might be a consequence of the emotional and physical demands of caregiving (Rohleder, Marin, Ma, & Miller, 2009). This situation requires support for the caregiver (Janda, Eakin, Bailey, Walker, & Troy, 2006; van Ryn et al., 2011).
It is often the partner or an adult child who is taking care of the patient with cancer in an informal manner (Han et al., 2013; Lambert, Jones, Girgis, & Lecathelinais, 2012; Rhee et al., 2008; Siminoff, Wilson-Genderson, & Baker, 2010; Weitzner, Haley, & Chen, 2000). In the case of older patients with cancer, this means that the caregivers are often older persons themselves, who also experience their own health problems. Furthermore, they tend to ignore physical health issues that are brought on by the caregiving itself (Klassen et al., 2012). Caregiving children and especially daughters often combine caregiving for an ill parent with their own paid job and the care for their children (Forssen, Carlstedt, & Mortberg, 2005). Besides the burden and other psychosocial problems, caregiving can also have a positive impact on both the caregiver and the patient. It can tighten the bonds between caregiver and patient and improve their relationship (Forssen et al., 2005; Klassen et al., 2012; Stenberg, Ruland, & Miaskowski, 2010; Ussher, Sandoval, Perz, Wong, & Butow, 2013; Weitzner et al., 2000).
Because of the earlier described shifts, reflecting a greater involvement of the older patient (≥65 years) with cancer and more responsibilities for the informal caregiver, more insight into the psychosocial problems of these caregivers are essential to develop tailored support. Although most cancer survivors are older, studies concerning psychosocial problems of caregivers do not specify results for caregivers of older cancer survivors (≥65 years). This review specifically looks at caregivers of older cancer survivors (≥65 years), with the emphasis on the patient's age and the patient treated successfully or considered to be cured. The older age of the patients can have specific challenges for the informal caregivers, like the presence of other comorbidities resulting in a higher dependency of the patient. Besides, in this population of informal caregivers, whereby the older patients are treated successfully or considered to be cured, their psychosocial well-being may be influenced by risk factors other than bereavement or approaching death of the patient, as in the case of informal care in a palliative or terminal setting. The main goal of this review is to examine the literature about psychosocial problems of caregivers of older cancer survivors (≥65 years), aiming to clarify the prevalence of these psychosocial problems and identifying possible risk factors for psychosocial problems in caregivers of older cancer survivors. Although there are also positive aspects of caregiving, they will not be taken into account in this review. With the results of this review, areas where knowledge about psychosocial problems of caregiving for older cancer survivors is lacking can be identified. If further research is needed, necessary recommendations will be made. Additionally, it can inform the development of future interventions aimed at supporting caregivers of older cancer survivors (≥65 years).
2 METHODS
2.1 Search strategy
A systematic literature search was conducted to identify the available literature on the prevalence and risk factors of psychosocial problems of caregivers of older cancer survivors (≥65 years). Specific end-of-life care was not the focus of this review. The search included studies in any language published between January 1966 and July 2016. The following computerized databases were searched: MEDLINE, EMBASE, Cochrane, CINAHL and PsycInfo. The MEDLINE key search terms, a combination of MeSH and free terms, used were (“caregiver” or “carer” or “care giver”) AND (“neoplasm” or “cancer” or “tumor”) NOT (“palliative” or “terminal” or “end-of-life”), after consideration of the (dis)advantages of using the term “NOT.” For the other databases, similar search strategies were built. Besides electronic searches, the reference lists of all identified studies were also hand-searched for further relevant studies. In a later stage, experts and senior researchers were asked to scrutinize the included articles to see whether, to their knowledge, important articles or studies were missing.
2.2 Screening
Citations were managed using Endnote. After removal of duplicates, two researchers (LJ and SD) independently screened paper titles and abstracts. The researchers screened the titles and abstracts on the following exclusion criteria: articles (a) not about cancer, (b) not about informal caregivers, (c) not about older survivors or (d) about patients in a palliative or terminal phase of their disease.
2.3 Eligibility
After screening the titles and abstracts, the researchers read the full text of all retrieved articles. They also did this when there was disagreement about an article. For an article to be selected during the second stage, both researchers needed to agree that the following eligibility criteria were met: (a) It reported empirical research (e.g., no case studies, letters, editorials and commentaries), (b) it described experiences and first-hand accounts of informal caregivers of older cancer survivors (e.g., no interventions, literature reviews, tools, trials or only experiences of patients or others), (c) curative setting or in survivorship and (d) the article had to be available in full text. The researchers did not want to miss out on the whole spectrum of possible psychosocial problems reported by informal caregivers so there were no predefined outcomes in this review. After inclusion of the articles, reported outcomes and measurement methods were listed to assess whether pooling of the data is possible.
2.4 Critical appraisal
The remaining articles were critically appraised by the two researchers independently. Through the Cochrane website, the researchers identified a checklist that was found to be most suitable for the type of studies in this review. This was the EHPP “Quality Assessment Tool for Quantitative Studies” (Sherifali, Fitzpatrick-Lewis, & Peck Reid, 2010). Based on the outcomes of the checklist, the quality of the articles was scored to be either strong, moderate or weak. Disagreement about the quality assessment was solved through discussion by the two researchers and consultation with the third author MvdA, when necessary. No articles were excluded on the basis of this critical appraisal score. However, the quality of the studies was taken into account when reflecting on the results in the discussion.
3 RESULTS
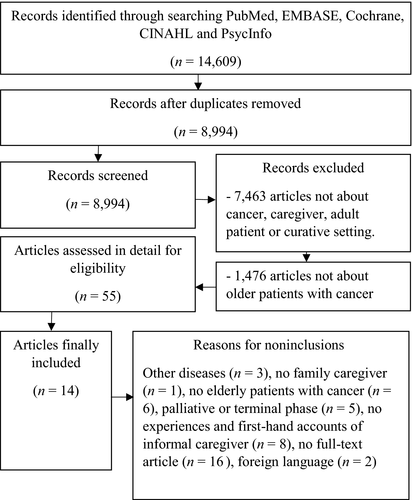
A total of 8,994 records were identified. After screening the titles and abstracts, 55 references were retained. The full text of these articles was screened against the inclusion criteria. This process with an inter-rater reliability of 0.78 (Cohen's Kappa) resulted in the exclusion of 41 articles. Finally, 14 articles were included in this review (see Figure 1), of which 13 were observational studies. Of these articles eight scored strong, three scored moderate and two scored weak on the critical appraisal (see Table 1). The remaining 14th article (Senden et al., 2015) reported a qualitative study. Although the researchers originally included both quantitative and qualitative articles, after the previous steps they decided not to take the one qualitative article into account when describing the results, but to use the article of Senden et al. (2015) to clarify points in the discussion while focusing on quantitative outcomes in the results section.
| Author(s) (year) | Study design/participants/setting | Methods (only caregivers) | Caregiver outcome measures | Critical appraisal |
|---|---|---|---|---|
| Bachner et al. (2009) | Survey of 313 American dyads of older patients (aged ≥60 years) with cancer and their caregiving daughters (n = 237) |
Structured caregiver interviews by telephone about:
|
Global self-esteem or overall self-worth | Strong |
| Fried et al. (2005) | Cross-sectional study of 71 older American patients (aged ≥60 years) with cancer and their informal caregivers (37 spouses (52.1%), 19 children (26.8%), 15 others (21.1%)), compared with older patients with congestive heart failure or COPD and their family caregivers |
Structured caregiver interviews at home separately about:
|
Communication concerns | Strong |
| Gilbar (1994) | Survey of 32 older Israeli patients with cancer (aged ≥65 years) and their spousal caregivers (21 husbands (65.6%), 11 wives (34.4%)) |
Structured caregiver interviews at home separately about:
|
Level of burden | Moderate |
| Gilbar (1999) | Cross-sectional study of 60 Israeli spousal caregivers (aged ≥65 years, 39 wives (65%) and 21 husbands (35%)) of older patients with cancer |
Self-report caregiver questionnaires at home, supervised by social work students, about:
|
Level of burden | Strong |
| Goldzweig et al. (2016) | Cross-sectional study of 45 older Israeli cancer patients (aged ≥86 years) and their spousal caregivers |
Structured caregiver interviews about:
|
Psychological distress Depression Social support Hope |
Strong |
| Jones et al. (2015) | Cross-sectional study of 76 Australian informal caregivers of older cancer patients with cancer |
Structured caregiver interviews about:
|
Level of burden Psychological morbidity (depression, anxiety, stress) |
Strong |
| Kurtz et al. (2004) | Cohort study with follow-up at 4–6 weeks, 2–3 months, 7 months and after 1 year of 491 dyads of older American patients (aged ≥65 years) with cancer and their informal caregivers (378 spouses (77%), 113 nonspouses (23%)) |
Self-administered caregiver questionnaires about:
|
Depression Psychosocial health |
Moderate |
| Lkhoyaali et al. (2015) | Survey of 150 Moroccan informal caregivers (61 males (40.7%), 89 females (59.%)) of older cancer patients (aged ≥70 years) |
Structured caregiver interviews at home about:
|
Level of burden | Weak |
| Lowenstein and Gilbar (2000) | Cross-sectional study of 64 older Israeli patients (≥65 years) with cancer and their spousal caregivers (primary caregivers, n = 32 (50%)) and their adult caregiving children (secondary caregivers, n = 32 (50%)) |
Self-report caregiver questionnaires at home, supervised by social work students, about:
|
Level of burden Personal strain Role strain |
Strong |
| Raveis et al. (1998) | Survey of 164 older American patients (aged ≥60 years) with cancer and their caregiving daughters |
Structured caregiver interviews by telephone about:
|
Perceived depression | Strong |
| Raveis et al. (1999) | Survey of 164 older American patients (aged ≥60 years) with cancer and their caregiving daughters |
Structured caregiver interviews by telephone about:
|
State anxiety | Strong |
| Rusinak and Murphy (1995) | Survey of 30 American spousal caregivers (5 husbands (17%), 25 wives (83%)) of older patients with cancer (both ≥ 65 years) |
Structured caregiver interviews at home about:
|
Perceptions of preparedness Knowledge and skills in cancer care Coping strategies |
Moderate |
| Washio et al. (2002) | Cross-sectional study of 20 older Japanese patients (≥ 70 years) with cancer and their informal caregivers (8 spouses (40%), 12 children (60%) |
Self-administered caregiver questionnaires about:
|
Level of burden | Weak |
| Senden et al. (2015) | Qualitative study of 32 older Belgian patients with cancer (≥ 70 years) and 19 informal caregiver | Separate semi-structured patient and caregiver interviews conducted by the same interviewer with experience in qualitative research | Lived caregiving experiences | NA |
- a Validated scale or measurement.
The size of patient samples ranged from 20 to 491 and the individual cancer survivor's age ranged between 60 and 94 years. Patients suffered from a variety of tumours with gastrointestinal, urological and breast cancer being the most prevalent cancer types. The range of caregiver sample sizes was the same as the patients and overall caregiver age ranged from 22 to 104. These caregivers consisted of, in descending order, spouses, adult children (particularly adult daughters), other relatives and friends. In all but one article, the majority of the caregivers were female, ranging from 44% to 100%. The patients and spousal caregivers included in the analyses of the articles of Gilbar (1999) and Lowenstein and Gilbar (2000) were the same persons. Only the children caregivers in the latter study were new. Because of this, the researchers decided to only include data concerning the children caregivers from Lowenstein and Gilbar (2000)'s article, which was also the most recent. In the two articles from Raveis, Karus, and Siegel (1998), Raveis, Karus, and Pretter (1999), the study samples of adult daughters consisted of the same people. Here, the researchers only included the data from the additional outcomes in the most recent article (Raveis et al., 1999), in order to avoid duplication.
During critical appraisal, nearly all the articles were considered to be of moderate-to-strong quality. This results mainly from the specific study population, the valid and reliable measurement instruments (see Table 1) and the appropriate statistical methods used in the studies. The lack of reporting confounders was an important reason to devalue articles. The main reason for the weak scores of two articles was the unclear or missing information about the participants, the measurement and statistical methods. We considered this result important enough to indicate, but not sufficiently weak enough to exclude the papers from our analysis.
Data on psychosocial problems without a proper explanation of the measurement tool were excluded. Because of the variety in outcomes, study populations and measurement instruments, conducting a meta-analysis was not possible. The outcomes reviewed in this article are as follows: (a) burden, (b) depression, (c) anxiety, (d) self-esteem, (e) distress, (f) communication issues, (g) stress and (h) quality of life.
3.1 Impact on psychosocial well-being
3.1.1 Burden
Studies measuring burden used different instruments. The ZBI scale was the most popular one, used in four studies (Gilbar, 1994, 1999; Lowenstein & Gilbar, 2000; Washio et al., 2002). Jones, Whitford, and Bond (2015) used the BASC scale. Bachner, Karus, and Raveis (2009) and the two studies of Raveis et al. (1998, 1999) measured the summary caregiver burden. By this, they meant burden created by caregiving with regard to employment, financial situation, social life, time, and physical well-being (Bachner et al., 2009; Raveis et al., 1998). There is a wide variety in results concerning burden (see Table 1), but the study of Washio et al. (2002) is the only one describing a kind of prevalence of caregiver burden: 40% (n = 8) of their study population experienced heavy caregiver burden. Also, Rusinak and Murphy (1995) categorized caregivers as either lightly or heavily burdened and another study found fairly low scores on burden (Jones et al., 2015), but both did not specify the prevalence of caregiver burden in their study population. On average, male spousal caregivers felt more burdened than their female counterparts in the study of Gilbar (1999). When compared to patients and spousal caregivers, adult children experienced the least personal strain, role strain and total burden. This difference was statistically significant for personal strain and total burden, but not for role strain between the patients, spousal caregivers and caregiving children (Lowenstein & Gilbar, 2000). Comparing adult daughters and spousal caregivers, one study found that adult daughters reported significantly higher levels of burden than spouses (Raveis et al., 1998). Mean scores from adult daughters on summary caregiving burden indicate an overall feeling of light burden (Bachner et al., 2009; Raveis et al., 1998, 1999).
3.1.2 Depression
Depression was measured with: DSM-IV (Lkhoyaali et al., 2015), the depression subscale of the Depression Anxiety Stress Scale (DASS21) (Jones et al., 2015), the Geriatric Depression Scale (5-item GDS) (Goldzweig, Baider, Andritsch, & Pfeffer, 2016) and (a subscale of) the Center for Epidemiological Studies Depression Scale (CES-D) (Bachner et al., 2009; Kurtz, Kurtz, Given, & Given, 2004; Raveis et al., 1998). All of the above are validated scales except the DSM-IV. However, if properly used by trained professionals, this can also be seen as a valid and reliable instrument. The results on depression also vary. Almost one-quarter of family caregivers participating in study of Lkhoyaali et al. (2015) were depressed. Another study showed that the caregivers scored considerably higher on depression compared to the UK adult general population sample with almost one-quarter of all these caregivers being moderately, severely or even extreme severely depressed (Kurtz et al., 2004). Kurtz et al. (2004) collected data in four waves over the course of 1 year, following surgery or initial therapy or treatment from the index patient. They found that after 1 year overall caregiver depression decreased with 22% compared to baseline. Raveis et al. (1998) found that the average mean scores of depressive symptomatology of the daughters were slightly higher than the scores of women of the same age in two community samples. One-third reported a level at or above the cut-off score for a clinical definition of depression. In the two community samples, these percentages were fairly lower. Caregiving daughters also reported higher scores on a depression subscale than spousal caregivers. Here, the average score indicated mild depression in the daughters versus no depression in the spouses (Jones et al., 2015). All these results point to overall substantial depression scores. On the contrary, Bachner et al. (2009) and Goldzweig et al. (2016) found low levels of depression in caregiving spouses.
3.1.3 Anxiety
The two studies reporting on anxiety used the anxiety subscale of the validated DASS21 (Jones et al., 2015) and the State Anxiety Scale of the State Trait Anxiety Inventory (STAI-S) (Raveis et al., 1999). Jones et al. (2015) found that caregivers have greater anxiety than the normal adult UK population of the same age. Of these caregivers, around one-fifth scored moderate or higher on anxiety. Spouses only, however, showed no anxiety. Anxiety was investigated in adult daughters as well. In comparison with a normative sample consisting of working women aged 19–69, the caregiving daughters scored somewhat higher on the anxiety scale. With regard to the mean scores, the daughters also scored higher: around one-thirds scored at or above the 80th percentile of the normative sample scores (Raveis et al., 1999). Results from Jones et al. (2015) showed that the average level of anxiety measured in adult daughters reflects levels of mild anxiety. Also here, adult daughters scored higher on anxiety compared with spouses (Jones et al., 2015).
3.1.4 Self-esteem
Sense of self-esteem was only measured in adult caregiving daughters using the validated Rosenberg Self-Esteem Scale. Bachner et al. (2009) found a fairly high mean score, compared to general US population samples.
3.1.5 Distress
The level of distress was only measured in spousal caregivers, using the Distress Thermometer. This is a one-item screening tool that also has been validated for caregivers of cancer patients. Goldzweig et al. (2016) found a quarter of the spousal caregivers suffered clinical levels of distress.
3.1.6 Communication issues
Communication issues between caregivers and patients were not measured with a validated scale but with three straightforward questions on communication between the patient and the caregiver regarding the patient's illness. Fried, Bradley, O'Leary, and Byers (2005) showed that caregivers of patients with cancer found it important to talk to the patient about the illness and that they would talk about it more than they had done before. More than one-thirds stated they had difficulty talking to the patient about the illness, indicating communication issues.
3.1.7 Stress
In the study of Jones et al. (2015), the mean score of stress level, as measured with the stress subscale of the DASS21, was low in caregivers. However, comparison of mean score differences of this group with UK general adult population showed that the caregivers had considerably increased stress levels. Comparing spouses and daughters, adult daughters scored substantially higher. Their mean score indicated mild stress, whereas the spousal caregivers average score pointed to a very low level of stress.
3.1.8 Quality of life (QoL)
Results show that caregivers had 28.6% lower QoL, measured with the Functional Assessment of Cancer Therapy-General Population (FACT-GP), comparing the mean score differences between them and the Australian population norm. Nevertheless, the mean caregiver score indicated that they value their QoL fairly high. The spousal caregivers in this study rated their QoL better than the whole group, whereas the caregiving daughters rated their QoL poorer than the spouses (Kurtz et al., 2004).
3.2 Predictors for caregiver's psychosocial issues
The reviewed articles did not provide any data on predictors for stress, QoL or communication issues. For the other psychosocial issues, again the results on predictors vary widely. With regard to burden, one study described that being a female caregiver was a predictor for burden while another study found that being a male spousal caregiver was a risk factor for burden (Gilbar, 1999; Rusinak & Murphy, 1995). Three studies found a relation between burden and depression: Caregiver depression was a risk factor for burden and vice versa (Gilbar, 1999; Raveis et al., 1998; Washio et al., 2002). Low self-esteem also significantly correlated, among others, with depressive affect of adult caregiving daughters (Bachner et al., 2009). All predictors are described in Table 2.
| Author(s) | Prevalence of psychosocial problems in caregivers of older cancer patients | Predictors |
|---|---|---|
| Bachner et al. (2009) |
Decreased global self-esteem Rosenberg Self-Esteem Scale: Ma = 35.03, SDb = 4.37 (rangec 10–40) |
Being employed (Bd = 2.538, pe = 0.030) Caregiver's income (B = 0.000, p < 0.001) Caring for a child/grandchild (B = 4.545, p < 0.001) Being married/living with a partner (B = –1.681 p = 0.048) Depressive affect caregiving daughter (B = –0.394, p < 0.001) Poor functional status of the patient (B = –0.495, p = 0.026) |
| Fried et al. (2005) |
Communication concerns Need for more communication with patient: n = 34 (47.9%) Difficult to talk with patient: n = 26 (36.6%) |
N/af |
| Gilbar (1994) |
Burden Zarit Burden Inventory (ZBI): M = 2.11, SD = 0.33 |
N/af |
| Gilbar (1999) |
Burden Zarit Burden Inventory (ZBI): Husbands: M = 54.1, SD = 9.4 (range 29–141) Wives: M = 48.1, SD = 9.9 (range 29–141) |
Being a male caregiver (B = 19.87, Fg = 11.31 p = 0.002) Caregiver age (B = 1.07, F = 5.19, p = 0.032) Patient's psychological distress (B = 10.79, F = 7.01, p = 0.013) |
| Goldzweig et al. (2016) |
Distress Distress Thermometer: M = 3.02, SD = 2.76 (range 0–10) |
No significant predictors |
| Jones et al. (2015) |
Burden Brief Assessment scale for caregivers of the medically ill (BASC): M = −10.11, SD = 12.37 (range −28 to 28) |
Being a caregiving daughter vs. a spouse (th = 2.94, p = 0.05) |
|
Depression Depression Anxiety Stress Scale (DASS-21): M = 7.48, SD = 8.24 (range 0–21) |
N/af | |
|
Anxiety Depression Anxiety Stress Scale (DASS-21): M = 5.76, SD = 8.23 (range 0–21) |
N/af | |
|
Stress Depression Anxiety Stress Scale (DASS-21): M = 11.21, SD = 9.55 (range 0–21) |
Being a caregiving daughter vs. a spouse (t = 2.57, p = 0.01) | |
| Kurtz et al. (2004) |
Depression Centre of Epidemiologic Studies Depression Scale (CES-D): (range 0–60) 4–6 weeks: M = 10.86, SD = 7.42 2–3 months: M = 9.98, SD = 7.82 5–7 months: M = 8.83, SD = 7.40 After 1 year: M = 8.47, SD = 7.19 |
No High school degree (B = −1.8753, p = 0.027) Living with patient (B = −2.560, p = 0.050) Impact on caregiver schedule (B = 1.0471, p = 0.000) Caregiver social functioning (B = −0.0282, p = 0.021) Caregiver sense of abandonment (B = 1.2828, p = 0.000) Patient symptom severity (B = 0.1089, p = 0.004) Patient depression (B = 0.1102, p = 0.000) |
|
Physical health Medical Outcome Study (MOS), Physical Health perceptions: (range 0–100) 4–6 weeks: M = 67.20, SD = 18.54 2–3 months: M = 67.19, SD = 17.84 5–7 months: M = 69.11, SD = 17.92 After 1 year: M = 68.95, SD = 20.39 |
High school degree (B = 6.5003, p = 0.004) Impact on caregiver schedule (B = −1.5517, p = 0.032) Caregiver social functioning (B = 0.0759, p = 0.027) Caregiver sense of abandonment (B = −2.1475, p = 0.012) |
|
| Lkhoyaali et al. (2015) |
Depression According to DSM-IV: n = 34 (22.7%) At least one depressive sign: n = 94 (62.7%)
Severe depression: n = 4 (2.7%) |
Urban origin: n = 100 (67%) Sleep disorder: n = 69 (46%) Loss appetite: n = 59 (39.3%) Fear of contagion: n = 16 (10.7%) Less socializing and neglecting their families: n = 68 (45%) Fear of inheriting cancer: n = 112 (74.6%) |
|
Anxiety According to DSM-IV: n = 119 (79.3%)
Anxiolytic taken: n = 15 (10%) |
Urban origin: n = 100 (67%) Sleep disorder: n = 69 (46%) Loss appetite: n = 59 (39.3%) Fear of contagion: n = 16 (10.7%) Less socializing and neglecting their families: n = 68 (45%) Fear of inheriting cancer: n = 112 (74.6%) |
|
| Lowenstein and Gilbar (2000) |
Personal strain Zarit Burden Inventory (ZBI): Spouse caregiver (M = 2.54, SD = 0.46) Child caregiver (M = 2.16, SD = 0.45) |
Being a spouse (F = 9.86, p < 0.001) |
|
Role strain (p < 0.001) Zarit Burden Inventory (ZBI): Spouse caregiver (M = 1.97, SD = 0.79) Child caregiver (M = 1.61, SD = 0.84) |
Caregiver age (F = 6.68, p = 0.001) Type of group (patient, spouse or child) (F = 5.05, p = 0.02) |
|
|
Total strain (level of burden) (p < 0.05) Zarit Burden Inventory (ZBI): Spouse caregiver (M = 2.25, SD = 0.55) Child caregiver (M = 1.89, SS = 0.61) |
Being a spouse (S > P < C) (F = 6.30, p <0.05) Age caregiver (F = 6.68, p = 0.001) Type of group (patient, spouse or child) (F = 5.05, p = 0.02) |
|
| Raveis et al. (1998) |
Depression CES-D (cut-off ≥16): M = 12.0, SD = 10.6 30% reported a level of depression at or above the cut-off score |
No. of other accumulated roles (B = −3.555, p ≤ 0.001) Caregiver health condition (B = 4.668, p ≤ 0.01) Sense of filial obligation (B = 0.410, p = ≤0.01) Attitudes regarding caregiving experience (B = −0.430, p ≤ 0.01) No. of domains of patient need for which daughter provides assistance (B = −1.523, p ≤ 0.01) Summary caregiver burden (B = 0.184, p ≤ 0.001) Perceived sufficiency of ill parent's care (B = −2.128, p ≤ 0.01) No. days since cancer diagnosis (B = 0.05, p ≤ 0.05) Graduated college (B = −3.747, p = ≤0.05) |
| Raveis et al. (1999) |
Caregiver Anxiety STAI-S: M = 38.6, SD = 13.0 |
General health patient (B = 2.556, p = <0.01) Health condition caregiver (B = 5.836, p = <0.01) Sense of filial obligation (B = 0.477, p < 0.05) Interpersonal support (B = 0.190, p < 0.05) No of ill parent need domains (B = 2.069, p < 0.01) Caregiving overload (B = 0.935, p < 0.05) No. days since cancer diagnosis (B = 0.06, p < 0.05) |
| Rusinak and Murphy (1995) |
Knowledge and skills in cancer care KSCC: M = 12.70, SD = 3.06 |
Education level (B = 0.33, p = 0.04) |
|
Perceptions of preparedness M = 12.97, SD = 3.19 |
Education level (B = −0.37, p = 0.02) | |
| Washio et al. (2002) |
Caregiver burden ZBI (cut-off ≥41): M = 41.2, SD = 23.1 Heavily burdened caregivers: n = 8 (40%) |
Physical health caregiver (p = 0.03) Depression caregiver (p < 0.01) Being a female (p = 0.03) No. of behavioural disturbances (M = 4.6, SD = 4.8, p < 0.01) Time of physical care (hr/day) (p = 0.03) Time of attending (hr/day) (p = 0.05) No. of family members (p = 0.02) |
- aMean score, bStandard deviation, cScore range of the scale, dUnstandardized coefficient, fNo information about risk factors, ep-value (significance ≤0.05), gF-test, ht test.
4 DISCUSSION
A wide spectrum of issues was found in different populations. There seems to be a higher distress, lower QoL and more anxiety in informal caregivers of older cancer survivors compared with the general population, but all were understudied. More research is needed to obtain a clear understanding of the psychosocial problems of caregivers of older cancer survivors, regarding to the type of caregiver, age, gender, time of measurement, patient's psychosocial problems and needs.
An abundance of the literature about caregivers of cancer survivors was found. Many articles, however, focused on older patients in an advanced cancer stage or receiving palliative care, but research about informal caring for an older cancer survivor is less of a topic considering the limited amount of 13 observational studies included in this review.
The authors do not consider this as a setback because the aim of this review also was to identify gaps in current research on psychosocial problems in informal caregivers of older cancer survivors (≥65 years) and to provide recommendations for future specific and comprehensive research.
A wide variety in used instruments measuring depression, burden and anxiety was found, and different or unclear cut-off points were used, or interpretation of the results was not straightforward. This hampered summarizing and interpreting the results. Therefore, only preliminary conclusions are possible based on this literature review and further meta-analysis of the results was impossible. A more robust and aligned framework for assessing the psychosocial experiences by caregivers in future research could remedy this situation.
The type of caregiver varied in the different studies. In daily practice, informal caregivers can be anyone, from a spouse or a child to a neighbour or a friend. The caregivers encountered in the reviewed articles included informal caregivers on this whole spectrum, sometimes clustered all together or focusing on a particular group such as spousal caregivers or adult daughters. The latter two stand out as the most frequent groups of informal caregivers in this review and presumably also in reality.
Psychosocial problems in caregivers of older cancer survivors are widespread. Also, there seems to be no agreement about which type of caregiver most seriously experiences burden. It seems to be a combination of several factors such as age, gender, patient's psychosocial problems, patient's treatment, time of measurement and other activities besides the caregiving. In their qualitative study, Senden et al. (2015) explained the disagreement in caregiver burden by the context of caregiving and the relationship between the patient and his/her caregiver. Depending on this relationship, in which both the caregivers maintain his/herself as well as the relationship, they experience more or less burden or other psychosocial problems. This might explain the contradictions between the studies, especially because coping styles (how a person faces stressful situations), attitudes towards caregiving and positive effects of caregiving are poorly reported in the included studies.
Other systematic reviews looking at psychosocial problems of caregivers concern patients with cancer, dementia or other chronic diseases, such as COPD or ALS. Besides the difficulty to compare results, because of the sometimes conflicting results or unclear methods, they mainly report stress, anxiety and depression, to be positively correlated with a higher care burden, patient's poorer mental and physical health, and sleeping problems of the caregivers (McCurry, Logsdon, Teri, & Vitiello, 2007; Sansoni, Anderson, Varona, & Varela, 2013; Schoenmakers, Buntinx, & Delepeleire, 2010). Also, loneliness seems to be an important but underestimated psychosocial problem in caregivers (Greenwood & Smith, 2016). Caregivers also struggle with emotions, such as anger, worry, fear and guilt, which are difficult to deal with and they have the feeling of being invisible for the professional caregivers (Seal, Murray, & Seddon, 2015). Regarding interventions to support informal caregivers, other systematic reviews mainly report that these should be approachable and adjusted to the needs of caregivers, to prevent the most vulnerable caregivers from being excluded (Applebaum & Breitbart, 2013; Bunn et al., 2012; Dias et al., 2015; Greenwood & Smith, 2016; Jones, Edwards, & Hounsome, 2012; Sansoni et al., 2013; Schoenmakers et al., 2010; Seal et al., 2015; Wheelwright, Darlington, Hopkinson, Fitzsimmons, & Johnson, 2016). To adjust interventions to the caregivers’ needs, further research is needed to compare caregivers of different gender and demographic backgrounds (Greenwood & Smith, 2015, 2016; Sansoni et al., 2013; Schoenmakers et al., 2010). Also, they suggest more longitudinal research focusing on caring dyads and caregiving networks (Applebaum & Breitbart, 2013; Greenwood & Smith, 2016), because of their important influence on caregiver's psychosocial problems. The results of other systematic reviews support our findings that all except two studies showed a tendency towards a higher prevalence of caregiver psychosocial problems, such as depression, compared to the general population (Bachner et al., 2009; Goldzweig et al., 2016). They also report differences between the studies concerning the variety of measurement instruments. It is no surprise that it is difficult to agree on the interpretation and use of the concepts of depression, depressive affect, depressive symptoms or the level of depression. Keeping this differences in mind and comparing the types of caregivers, there seems to be a higher prevalence of depression in caregiving daughters, compared to caregiving spouses (Jones et al., 2015; Raveis et al., 1998).
According to the authors, there are three possible reasons for the lack of reporting psychosocial problems of caregivers of older cancer survivors. The first one is the changing cancer population over the last decades, where the majority of articles described older patients with cancer in an advanced or even palliative stage, in the current ageing population with better treatments older patients are also cancer survivors. Second, an ageing population requires changes in the current healthcare system. With the shift to more outpatient care, informal caregivers become more important which in turn increases the pressure on these caregivers. Because of their important role in the care for the older patient, insight into and support for the well-being of these caregivers becomes essential. Finally, informal care given by spouses, children, neighbours and friends is not a new phenomenon, it already exists for generations, and it is more or less embedded in the social relationships between people. Nowadays, the difference is that caregivers increasingly have to juggle multiple roles and responsibilities which interfere with that taken-for-granted aspect of caregiving. Currently, informal caregivers of older cancer survivors do not feature prominently in the literature, but there is a growing emphasis on them as an important research population.
4.1 Strengths and limitations
To our knowledge, this is the first review to explore the psychosocial problems of caregivers of older cancer survivors. The strength of this review is the fact that the researchers focused especially on the caregivers of older cancer survivors and two researchers independently carried out the search and selection based on title, abstract, full text and critical appraisal of the articles.
This review described the impact of caring for an older cancer survivor on the psychosocial well-being of caregivers as good as possible, but the authors are aware of some important limitations. First, because of the small number of articles and the wide variety of measurement instruments, study populations and times of measurement, it was impossible to make a proper synthesis or meta-analysis. However, this review provided a narrative synthesis of all available scientific literature as a best method to describe the available results. Second, the authors are aware of the variety of outcomes and the fact that some outcomes were only described in one article. Nevertheless, they decided to include these outcomes to give a comprehensive overview of the psychosocial problems described in the literature, aiming to clarify the prevalence and possible risk factors for these psychosocial problems. Therefore, there were no predefined outcomes in this review and the authors considered it important to describe all outcomes, even when described poorly with not always a proper explanation of the measurement tool. At last, not all predictors were adequately described in this literature review, which represents the reality in the included articles. In summary, this review shows more than ever the need to further standardize research, which was also an aim of this review.
5 CONCLUSION
This overview of published research on psychosocial problems in informal caregivers of older cancer survivors identifies major gaps in the literature. It was impossible to perform a proper meta-analysis because of the wide variety of measurement instruments, study populations and times of measurement found in the included studies. This makes for a somewhat vague and intangible end result but there is a definite upside to this. This review shows more than ever the need to further standardize research in this area in order to obtain better insights into the psychosocial problems of these caregivers. More integrated research will also provide the opportunity to accurately compare different types of caregivers, such as spouses and caregiving children. Based on the current results, no firm guidelines for improvement of the care for these caregivers can be formulated yet. However, with more integrated and specific future research, targeted and qualitative support for this group of caregivers can be developed.
ACKNOWLEDGEMENTS
This research was funded by Kom op tegen Kanker, the campaign of the Vlaamse Liga tegen Kanker VZW.
CONFLICT OF INTERESTS
The authors have declared no conflict of interests.