Developing an aftercare decision aid; assessing health professionals' and patients' preferences
Abstract
Personalising aftercare for curatively treated breast cancer patients is expected to improve patient satisfaction with care. A patient decision aid can support women in making decisions about their aftercare trajectory, but is currently not available. The aim of this study was to assess the needs of patients and health professionals with regard to an aftercare decision aid to systematically develop such a decision aid. Focus groups with patients and individual interviews with health professionals were digitally recorded and coded using the Framework analysis. Although most patients felt few aftercare options were available to them, health professionals reported to provide various options on the patients' request. Patients reported difficulty in expressing their need for options to their health professional. Although most patients were unfamiliar with decision aids, the majority preferred a paper-based patient decision aid, while most health professionals preferred an online tool. The practical implications for the intended patient decision aid are: that a digital tool with paper-based element should be developed, the patient decision aid should facilitate both rational and intuitive processes and should provide insight in patients' preferences concerning aftercare to discuss these explicitly.
1 INTRODUCTION
In the Netherlands, breast cancer is the single most prevalent type of cancer in women and the number of breast cancer patients is growing; a 23% increase in incidence was observed between 2001 and 2014 (IKNL, 2011). Moreover, due to improved treatment and screening options (La Vecchia et al., 2010), the five-year survival rate has increased by nine percent during that same period (IKNL, 2011). As a result, the number of women eligible for aftercare after completing curative treatment has increased as well.
Updated national clinical practice guidelines are currently in place to provide structure for the content and frequency of care after breast cancer. Aftercare serves two main purposes; to detect local recurrences early, and to guide patients in coping with side effects and psychosocial problems. Previously, aftercare consisted of frequent follow-up appointments (Kimman et al., 2011) to meet both purposes. This frequent aftercare, however, did not have a significant impact on earlier identification of cancer recurrence (Montgomery, Krupa, & Cooke, 2009) or subsequent life expectancy (Geurts et al., 2012). Therefore, breast cancer patients currently receive an annual physical exam and mammography to check for recurrences with additional appointments in case of hormonal treatment (Nabon, 2012). Furthermore, to screen for side effects and psychosocial problems, health professionals (HPs) are encouraged to meet with patients and to provide support, e.g. by providing consultations in between yearly follow-up appointments, especially in the first year after curative treatment completion (Nabon, 2012).
However, the guidelines do not specify how many times or by whom this individual psychosocial support should be conducted and therefore leave room to personalise care based on individual patients' preferences. An earlier study of our group showed that if patients could choose a personalised aftercare trajectory that best suits their preferences, satisfaction with aftercare increases (Benning, Kimman, Dirksen, Boersma, & Dellaert, 2012; Kimman, Dellaert, Boersma, Lambin, & Dirksen, 2010). In addition, several studies have shown that patient satisfaction, medical safety and health-related quality of life do not suffer when follow-up is performed in varying forms, for instance, appointments with a nurse instead of a medical specialist (Sheppard et al., 2009; Koinberg, Fridlund, Engholm, & Holmberg, 2004; Grunfeld et al., 2006; Kimman et al., 2011), or by telephone instead of a visit to the out-patient clinic (Kimman et al., 2011). Moreover, personalised aftercare would also be cost and time efficient, as patients choosing less frequent consultation trajectories will result in lower medical expenses (Benning et al., 2012).
Decision aids are tools that can support patients to understand their own preferences and to make decisions regarding their health care based on these preferences (Fagerlin et al., 2013; Elwyn et al., 2006). Generally, Patient Decision Aids (PTDAs) present patients with all health care options available in their medical centre and list their advantages and disadvantages. Moreover, PtDAs can also be used to assess personal values or preferences (Fagerlin et al., 2013), can serve as a tool to support communication about preferences with relevant HPs and stimulate shared decision-making (Slover, Shue, & Koenig, 2012; O'Connor et al., 2003). To date, several effective PtDAs have been developed to facilitate treatment choices (Garvelink et al., 2013; Elwyn, Frosch, Volandes, Edwards, & Montori, 2010), but no PtDA for aftercare and more specifically breast cancer aftercare exists. In order to develop such a PtDA and effectively implement it in aftercare procedures, information regarding patient preferences about their aftercare and HPs' preferences regarding application of the PtDA need to be assessed (Coulter et al., 2013).
Consequently, the aim of this study was to investigate and compare patients' and HPs' experiences and preferred decision-making processes, as well as preferences for availability of options in aftercare and for the format of the PtDA. For this purpose, we chose to perform a qualitative study, since this is best suited for exploration and discovery of general opinions of a target group (Morgan & Krueger, 1998).
2 METHODS
2.1 Participants
Female patients who finished their curative breast cancer treatment in one of two medical centres in the southern part of the Netherlands in the last 12 months (surgery, radiotherapy, chemotherapy or a combination) were asked to participate in a focus group discussion. Focus groups were chosen as the best method to help patients form and organise their ideas together on the PtDAs, with which most patients are not familiar. In these focus groups, patients were stimulated to generate opinions and discuss these together. Exclusion criteria for participation were the development of local recurrences or metastases, no understanding of the Dutch language and still receiving curative breast cancer treatment. Women who were receiving hormone or immunotherapy were nevertheless eligible to participate.
HPs with different disciplines and from different medical centres in the south-eastern part of the Netherlands were asked to participate in a face-to-face interview. Most HPs are familiar with the use of PtDAs; their ideas had often times already been formed concerning the use of PtDAs, therefore conducting face-to-face interviews instead of focus groups was considered more appropriate to explore these ideas (Tong, Sainsbury, & Craig, 2007). The HPs were all currently involved in breast cancer aftercare. Patients or HPs who did not understand the Dutch language were excluded from participating.
Before participating in the focus group discussion, patients filled out a questionnaire to collect background characteristics, which consisted of eight open-ended and three multiple-choice questions. Patients were asked to state their date of birth (converted to age) and type of curative treatment (e.g. lumpectomy, mastectomy, radiation therapy and/or chemotherapy). Furthermore, current anti-cancer medication use was assessed (immunotherapy or hormonal therapy). HPs were asked to state their profession and their place of work.
2.2 Procedure
Patients were informed about the focus groups during their aftercare trajectory by their nurse practitioner, breast care nurse or radiation oncologist. Those interested were given an information letter detailing the study and were subsequently contacted by telephone to confirm study participation. The patients, 32 in total, received an information letter from their nurse practitioner. Of those patients, five were never reached via telephone and thus not asked to participate. One patient had developed metastases and was no longer eligible to participate. Three patients were willing to participate but fell ill on the day of the appointment. Participation was refused by 12 patients. The 11 patients willing to participate received a confirmation letter with an itinerary for the focus group and contact information. Focus groups were conducted in neutral surroundings outside the hospital to create a secure environment in which patients could speak their mind freely. A researcher (LK) not involved in breast cancer treatment or aftercare functioned as moderator in all three focus groups. Each focus group lasted 90–120 min. Before the focus groups commenced, patients filled out a short questionnaire to collect background information and signed an informed consent form. All focus groups were digitally recorded. Afterwards participants received a €10 gift certificate.
HPs were asked to participate in the study by e-mail. E-mail addresses were provided by the study steering group members from seven different medical centres. HPs from four different medical centres responded. In total, 10 surgeons, 14 nurses, four medical oncologists and two radiation oncologists were approached. Five surgeons, eight nurses, one medical oncologist and one radiation oncologist agreed to participate. Face-to-face interviews lasting 20–50 min were conducted at the HP's place of work. After oral permission, the interviews were digitally recorded. Data collection for both patients and HPs was completed after data saturation was reached.
2.3 Ethical considerations
The internal review board (IRB) of the MAASTRO Clinic was contacted to advise about the ethical considerations concerning the focus group study. The IRB deemed that the study did not meet compulsory ethics approval requirements described in the Dutch Act for Medical-Scientific Research in Humans (Centrale Commissie Mensgebonden Onderzoek, 2012) and European guidelines for Good Clinical Practice were followed (Centrale Commissie Mensgebonden Onderzoek, 2012). Therefore, patients and HPs were informed about the study and it was made clear that participation was voluntary and participants could stop at any time without having to give a reason. Informed consent forms were filled out by patients; HPs gave recorded oral consent for participation. The data will be stored anonymously for 15 years and destroyed thereafter.
2.4 Data collection
A semi-structured question guide was used during the focus group interviews. A similar but adjusted semi-structured question guide was used to conduct the face-to face interviews. The questions on both question guides were divided into four topics: (1) experiences with aftercare options, (2) shared decision-making, (3) decision-making processes and (4) preferences concerning an aftercare PtDA.
First, patients' expectations and experiences regarding the options in current aftercare trajectory were assessed with the following question: “What are your expectations regarding aftercare?.” HPs were stimulated to describe the current aftercare options in their medical centre.
Second, questions pertaining to shared decision-making were posed in both the focus groups and the individual interviews, for example “What is your role in the decision-making process?” and “How do you experience this role?”.
Third, current decision-making processes were explored. Participants were asked to think about aspects involved in reaching a decision with regard to aftercare (e.g. social norms, emotions) by asking focus group participants: “What factors are involved in reaching a decision?” and the HPs: “What factors are involved when providing advice to patients”.
Finally, expectations or preferences for the development and implementation of a PtDA to support decisions in aftercare were assessed. After a brief explanation of the intended PtDA and its purpose, participants elaborated on how this PtDA would be most helpful to them. HPs and patients were asked: “What information should the PtDA provide?” and “In which format should the PtDA be presented?” As the proposed PtDA is currently not available for either patient or HP, concepts of the diffusion of innovations theory (Rogers, 2002) were used as a basis for questions pertaining to the implementation of the PtDA. According to this theory, the level of adoption is based on five factors, which are relative advantage, complexity, compatibility, trialability and observability. Based on these factors, HPs were asked questions about the implementation of the PtDA, such as: “In what way is the PtDA in keeping with your regular practice in making decisions about aftercare?”. In the focus groups, these concepts were not assessed due to the complex nature of the questions.
2.5 Analysis
The recordings of the focus groups and interviews were transcribed verbatim. The transcripts were in turn analysed using NVIVO 10. The data were analysed systematically by two independent researchers (LK and TH coded the focus group transcripts, and LK and KH coded the interview transcripts) according to three key stages of the framework analysis (Lacey & Luff, 2009). The framework method was used because it is often used in applied sciences to reach recommendations on specific topics in a relatively short amount of time by thematically analysing qualitative data (Lacey & Luff, 2009), which suits the aim of the current study.
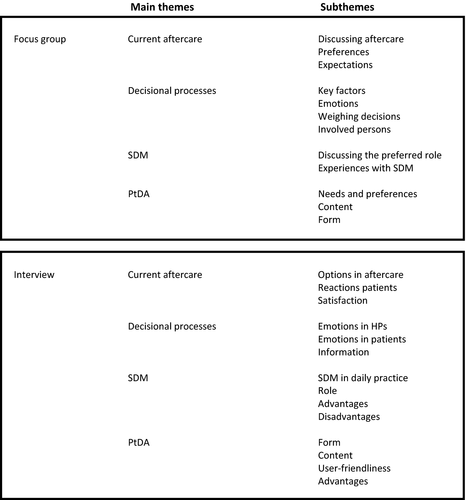
This approach pertains forming a coding scheme based on the transcripts and then order the different quotes under each theme. First, a general overview of the themes identified in the transcripts was made. These general themes were: current aftercare, decisional processes, SDM and PtDA. Then two coding schemes, one for the focus groups and one for the face-to-face interviews, were developed by gathering and grouping together the different subthemes. The most important themes are visible in Fig. 1. Both coder duos discussed and agreed upon the coding schemes. Subsequently, the coding schemes were applied to the relevant transcripts as follows: first, quotes were sorted under the main themes of the coding schemes. Second, quotes under the main themes were sorted to the subthemes. The quotes belonging to the specific themes were compared and interpreted to analyse the data. To illustrate the interpretations and conclusions made based on the data, implicit and explicit quotes were used.
Using NVIVO 10 Coding Comparison Query, the level of agreement was calculated for both the focus groups and the interviews. The level of intercoder agreement was well above cut-off point (focus groups = 96% and interviews = 97%) (Lombard, Snyder-Duch, & Campanella Bracken, 2002).
The background characteristics of the patients, measured by the short questionnaire were analysed using SPSS 20 by computing descriptive statistics and frequencies.
3 RESULTS
3.1 Participants
In three focus groups, 11 patients participated. Four patients took part in the first focus group, four patients in the second and three in the third and final focus group. After three focus groups saturation was reached and data collection was completed. The average age of the patients was 62 years (range 49–75). Patients had finished their primary treatment on average 4.2 months (range 1–11 months) before participation. The primary treatment of patients varied. Eight patients had a lumpectomy, two of which were DCIS patients and did not need further treatment and three patients had a mastectomy. Six patients received radiotherapy and one patient had chemotherapy.
In total, eight HPs were interviewed face-to-face and after eight interviews saturation was reached, such that interviews with the other HPs who had agreed were cancelled. Due to an inaudible recording, one interview with a nurse practitioner could not be included in the analysis.
3.2 Experiences with and preferences for aftercare options
-
- Patient A
-
- If I remember correctly… she said that it [aftercare consultation] was every three months
-
- Patient B
-
- The first [year], the second every six months and thereafter every year
-
- Patient A
-
- yes, and [consultations] are with her (nurse)
-
- Patient
-
- But I got a business card…….if you are not feeling well or if you have questions, you can always call
-
- Medical oncologist
-
- ……it is discussed with patients if they would like to have [a consultation] every three months or if they want to be approached via telephone or if they do not feel the need [for consultations] at all
-
- Nurse
-
- And if you ask them if they would prefer telephone or face-to-face consultations, almost everyone chooses face-to-face
-
- Nurse
-
- Five years ago we initiated a personal aftercare plan. Patients could come [to the hospital] every three months, but that is their choice. And then you see that this is so often [the preferred frequency] that it becomes standardized
-
- Patient
-
- I went to the breast care nurse…..she did a check-up and [with that] she really reassured me
Therefore, they would prefer a higher frequency of consultations thus wanting there to be options to match their preferences.
-
- Patient
-
- I think an oncologist can explain it better if you have questions….
-
- Patient
-
- It is a pity, you complete a whole trajectory with your oncologist; and then, you do not see her anymore
-
- Patient
-
- It is difficult to say; you are afraid you might offend her
-
- Surgeon
-
- We try to facilitate patients [when providing aftercare]…this should be practiced more…the main goal for aftercare is to increase the patients' comfort
-
- Nurse
-
- Aftercare could be tailored more to the patients' needs
-
- Medical oncologist
-
- [Nurses] are focused on psychosocial problems and can provide better support; that is appreciated by the patient
3.3 Perceived roles in decision-making
-
- Patient
-
- It feels good [to have a big influence] it is after all your own body and your own health and you have to stand up for that
-
- Surgeon
-
- The role of the patient is not very large I think……the process of deciding on a direction with you is fairly restricted by the guidelines
-
- Nurse practitioner
-
- [Patients] have their own opinions and they have a say…..patients feel heard; not like before: that what the doctor says is what is going to happen. No, it is a different time now, thankfully
-
- Radiation oncologist
-
- The most annoying patients are patients that say: Just do whatever you think is good for me. This makes you feel very uncomfortable…[because] you want patients to support the chosen path….there is a smaller chance of regret if the patient has thought about it and knows what (s)he has started
-
- Patient
-
- You have to make your own decisions [according to HPs]….. if they said you had to do a [lumpectomy] and the cancer returns, then you can say: well yes doctor [the cancer returned] because you said I had to do it
-
- Nurse
-
- [SDM] is applied in many of the consultations especially with [choosing between] different treatments……. [patients] have to make more and more decisions……so it should be applied in the follow-up consultations as well
-
- Medical oncologist
-
- Mainly the elderly patients, because they put their trust in the doctor's autonomy
-
- Patient
-
- I just take whatever is offered to me, [because] that is what is best for me
-
- Surgeon
-
- If we cannot figure it out together, then a decision has to be made and we [professionals] will make this decision
3.4 Decision-making processes
-
- Patient
-
- It is something from your inner core, which is your [will to] survive
-
- Patient
-
- I would have chosen the same thing, but it is more about certainty
-
- Nurse practitioner
-
- You have to inform them very carefully, that is most important. That [patients] can make a decision based on the information or advice they gathered from you
Contrary to patients, HPs stated that their advice was based solely on medical empirical evidence and that their intuition played no part.
-
- Patient
-
- I make the decision, but I will check with the others [family members] [to find out] if they would do the same
-
- Patient
-
- Hands-on experts, they are important to me as well. I will contact them….to make sure I am fully informed
-
- Patient
-
- In my case, because of the emotions, I can't think rationally anymore, while I should….and then you are happy if there is someone there that can do it for you, like your partner or child. They say that you have choices but due to [emotions] you feel like you cannot make a choice.
-
- Medical Oncologist
-
- Fear, I think that many people [choose] an approach out of fear….even if we inform them properly
3.5 A patient decision aid
-
- Patient
-
- If alternatives are listed, then you need to think about these alternatives, because I do not know all the options that exist
-
- Patient
-
- I can imagine that it could clarify a lot or that there are options listed that you did not think of yourself
-
- Nurse practitioner
-
- Particularly, patient satisfaction, HP satisfaction of course…..and time. You do not have to spend as much time on it [a consultation] every year
-
- Surgeon
-
- I wonder if a surgeon should do it. I know that research shows that patients are more at ease with a non-specialist….a breast care nurse. Patients would rather have consultations with them than with a medical specialist
-
- Patient
-
- [A paper PtDA] on the one hand it is old-fashioned, but on the other hand, you can always keep it close by and have a look at it again
-
- Patient
-
- In [the form of] a consultation and afterwards in writing that would be pleasing for me….There will be a lot of information in a consultation and afterwards at home you can take a look at the options again
-
- Radiation oncologist
-
- I would prefer it to be an online device, which is what you often see these days. And I have heard it [confirmed] with research a lot; you do not have to fear that elderly people will not be able to do it
-
- Medical Oncologist
-
- I think the best option is during a consultation, then you can answer patients' questions and letting them do it at home does not work….patients forget
-
- Nurse practitioner
-
- If they can do it beforehand, it can help during the consultation. Then they know what to expect concerning aftercare
-
- Nurse practitioner
-
- I would do it at two points in time. First, the patients can inform themselves at home and form an idea. Then we can discuss their idea and take a look at [the PtDA] together
-
- Patient
-
- Step by step, not too much at once, I am not going to let it drive me crazy
-
- Patient
-
- I think I want to know as early as possible. You can decide for yourself what to do with the information, but I would like to know that it exists, so for me it can be used early on
-
- Surgeon
-
- I think when the initial treatment has just finished; then the treatment is over with and things settle down
-
- Radiation oncologist
-
- When the treatment plan is decided upon. You know you will receive treatment and at the same time you know what the corresponding aftercare options are
4 DISCUSSION
The aim of the current study was to compare patients' and HPs' needs and preferences regarding a PtDA for breast cancer after care. The results will provide input for the development of this PtDA.
4.1 Experiences with and preferences for aftercare options
The results showed a discrepancy between patients' and HPs' perception of available options; although the majority of HPs reported there were several aftercare options patients could choose from, patients could not recall a discussion of aftercare options or having the opportunity to make a decision about their aftercare trajectory. Additionally, patients were reluctant to ask their HP (medical specialist or nurse) about alternative aftercare options in fear of damaging their relationship. The discrepancy between the perception concerning available aftercare options might be due to patients not recognising that options were provided, or to patients forgetting which options were given. Moreover, it can be caused by a lack of communication between doctors and patients in regard to the patients' preferences in aftercare. Research showed for instance that HPs are not always aware of what the patient wants and are often unsuccessful in predicting what a certain patient would choose regarding treatment and care (Rozenblum et al., 2011) but do base the conversation about options upon their assumptions. Moreover, the reluctance of patients to vocalise their preferences and expectancies is reported in this study due to a fear of damaging the relationship with the HP. Earlier research has shown similar results namely that patients have a fear to be viewed by HPs as being difficult (Frosch, May, Rendle, Tietbohl, & Elwyn, 2012). HPs on the other hand might think patients' expectations concerning aftercare are met and patients underwrite this by not telling HPs otherwise (Frosch et al., 2012), thus resulting in decisions that do not take individual patient preferences into account.
4.2 Perceived roles in decision-making
Patients and HPs reported regular involvement of patients in general medical decision-making. Both groups expressed positive evaluations of patient involvement; patients felt heard and HPs appreciate at least sharing responsibility for the final decision. However, most patients expressed a desire to have the final say in the ultimate decision. Although patients value opinions of others like HPs, family members and other breast cancer patients, they felt the ultimate decision should be theirs. This is in line with other studies suggesting that involving patients in decision-making increases their perceived autonomy (Sandman & Munthe, 2010; Joosten, De Jong, De Weert-Van Oene, Sensky, & van der Staak, 2011). The HPs considered their role in the decision-making process as providing the patient with the appropriate information to make a decision. They therefore seemed to respect the patient's autonomy.
4.3 Decision-making processes
Some patients made decisions based on rational considerations, such as medical information or the HP's expertise. HPs perceived their role in the decision-making process was mainly to provide the patient with evidence-based medical information. Previous studies have shown that rationally based health decisions are viewed as more viable and credible by HPs than intuitive-based decisions; for these are thought to be more bias prone (Buetow & Mintoft, 2011). Therefore, some HPs claim to base their health decisions on rational deductions and are reluctant to take patients' intuition into account (Buetow & Mintoft, 2011). In contrast, recent research shows HPs do use their own intuition in clinical decision-making (Gillespie, Chaboyer, St John, Morley, & Nieuwenhoven, 2014) and patients in this study indicated that their decisions were based much more on intuitive processes as well. Thus, in order to support decision-making according to both patients and HPs, rational and intuitive processes should both be taken into account.
4.4 A patient decision aid
Regarding the patient decision aid, both patients and HPs reported that a PtDA would be a helpful tool. They disagreed, however, about the format of the PtDA. Most patients preferred a paper-based PtDA, primarily as they wanted to have a work of reference that they can look back on once at home. Research shows that this preference for paper over digital devices might be age-related, with younger patients showing a higher preference for digital devices (Saied et al., 2014; Barentsz et al., 2014) and patients in this study can be viewed as older. Older patients that do use digital information have a high use of paper-based information as well; they seem to use the two types together as a combination (Medlock et al., 2015). In contrast, HPs preferred a digital PtDA, which is in line with previous research showing that HPs increasingly make use of tablets and smart phones for information seeking and decision support (Divall, Camosso-Stefinovic, & Baker, 2013; Mickan, Atherton, Roberts, Heneghan, & Tilson, 2014).
Patients and HPs had both differing opinions about when the PtDA should be introduced. Most HPs reported that the aftercare trajectory is currently discussed after primary treatment so this would seem like the natural time in existing trajectories to introduce the PtDA. Not many studies have been performed to test the timing of a PtDA. van Roosmalen et al. (2004) performed a study to assess the best timing to introduce a PtDA for genetic testing for breast cancer patients. They found that timing in this case did not influence the effectiveness of the PtDA. However, further research concerning the timing for this PtDA should be performed to assess if it does not influence effectiveness in this case. Moreover, patients and some HPs reported to want to use the PtDA during a consultation. Research showed that using a PtDA during consultations can enhance cognitive processing in patients and stimulate active decision-making roles in patients and HPs (Brown, Bradley, Ng, Colwell, & Mathers, 2014). Thus, using the PtDA during a consult is in line with preferences of both patients and HPs and is expected to facilitate the decision-making process effectively.
4.5 Practical implications
The results have implications for the development as well as the implementation of a PtDA to support decision-making in aftercare. The finding that both HPs and patients appreciate patients playing a comprehensive role in the decision-making process, thus making informed decisions, means this should be integrated in the PtDA. Furthermore, to resolve the discrepancy between patients and HPs concerning perceived available aftercare options, the PtDA should provide both patients and HPs with an insight in patients' preferences to discuss these together.
Moreover, patients reported to use rational processes, intuitive processes or a combination as is in line with current viewpoints about medical decision-making (Buetow & Mintoft, 2011; Bate, Hutchinson, Underhill, & Maskrey, 2012; Ubel, 2010). Therefore, both rational and intuitive processes should be facilitated by the PtDA (De Vries, Fagerlin, Witteman, & Scherer, 2013). Rational processes can be activated by providing the patient with an overview of the available aftercare options. The overview should show how well these options match with their individual preferences. De Vries et al. (2013) suggested that intuitive processes can be stimulated by asking patients to state their first reaction to the available options without thinking about the reason behind it.
In addition, patients prefer a paper PtDA, while HPs prefer the PtDA to be a digital tool. As both patients and HPs will use the PtDA, their preferences should both be taken into account. Patients prefer paper because they like to have a work of reference they can access later on. To comply with both preferences, the PtDA should be a digital tool with a printable overview for patients to take home.
4.6 Strengths and limitations
The patient sample used in this study seems to form a good representation of the target population. The mean age of participants for instance, was 62 year and the age group wherein in recent years most breast cancer incidences occurred is 60–69 (IKNL, 2011).
Another strength of this study is that although previous studies were performed to assess preferences of both patients (Brennan, Butow, Marven, Spillane, & Boyle, 2011) and HPs concerning aftercare (Kwast, Drossaert, & Siesling, 2013), insights in decisional processes of patients' decision-making were not studied before from both perspectives. The current study does provide this insight, which is essential for the systematic development of a PtDA effective in facilitating the patients' decisional processes according to IPDAS criteria (Elwyn et al., 2006; Coulter et al., 2013).
A possible limitation is that the current study was performed in the southeast region of the Netherlands and results may therefore not be completely generalisable. However, HPs from different parts of the region participated in the study and the focus groups were held in different locations as well, resulting in data representative for the region as a whole.
5 CONCLUSIONS
To develop a PtDA to personalise aftercare, needs and preferences of both patients and HPs need to be assessed and compared. The needs and preferences identified in this study will have practical implications for the intended PtDA. Since patients especially older patients, prefer paper-based information while HPs prefer digital tools, the PtDA should at least contain a paper-based element for patients to use as a reference. Furthermore, the PtDA should provide insight in patients' preferences for the patient as well as the HP concerning aftercare as these are often not discussed explicitly but are important to reach a suitable decision.
As the PtDA is meant to support the medical decision-making process in patients, the processes involved need to be assessed as well. The results show that patients use both rational and intuitive processes but HPs base their advice mostly on evidence-based information. This implicates that the PtDA should facilitate both intuitive and rational decision-making processes. The patients should therefore be presented with an overview including the options, their preferences and their first reaction concerning the available options.
ACKNOWLEDGEMENTS
This research was funded by CZ Health Insurance and VGZ Health Insurance and was performed on behalf of the B-beslist! Group. We would like to thank F. Kurris for her input on behalf of the Breast Cancer Association Netherlands, A. Degenaar for her input on behalf of the Comprehensive Cancer Centre the Netherlands and J.H.E. Rooijen for her help with the recruitment process.
Appendix A:
Members of the B-beslist! Group are: Portz, M.J.G., MANP representing Zuyderland Hospital in Sittard-Geleen; Mertens, P.M.G. representing Viecuri Hospital in Venlo, MANP; Janssen-Engelen, I.L.E., MANP representing SJG in Weert; Lenssen, A.M.M.R.N., MANP representing Zuyderland Hospital in Heerlen; Finaly- Marais, M.B.Ch.B., FCS (SA) representing Laurentius Hospital in Roermond and Starren-Goessens, C.M.J., representing Maastricht University Medical Centre in Maastricht.