The predictive value of cumulative plantar tissue stress on future plantar foot ulceration in people with diabetes—A 12-month prospective observational study
Abstract
Aims
Plantar foot ulcers are a burdensome complication of diabetes caused by abnormal foot biomechanics. Predicting foot ulcers aids in their prevention, but the value of peak pressure—the most used biomechanical parameter—is only moderate. We aimed to improve prediction based on the more comprehensive load measure cumulative plantar tissue stress (CPTS).
Methods
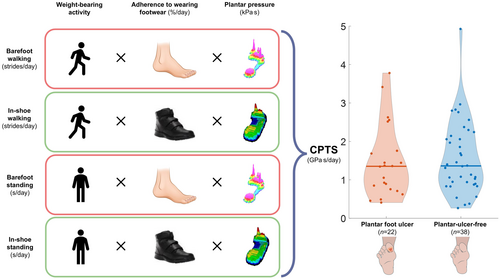
We prospectively observed 60 participants with diabetes at high foot ulcer risk for 12 months. At baseline, we assessed demographic and clinical characteristics—including plantar pre-ulcers (i.e., abundant callus, haemorrhage, blister, fissure)—and measured barefoot and in-shoe plantar pressures during walking and standing. Daily-life weight-bearing activity and adherence to prescribed footwear were assessed over 7 days after baseline. The primary outcome was plantar foot ulceration during the 12-month follow-up. CPTS was calculated (in GPa.s/day) from the above foot-loading factors and analysed for predicting foot ulcers and its association with pre-ulcers, using multivariate regression analyses.
Results
Twenty-two participants (37%) developed a plantar forefoot ulcer. CPTS was not a significant predictor (odds ratio (OR) = 0.90 (95% confidence interval (CI): 0.50–1.59)) but pre-ulcers at baseline (OR = 9.97, 95%CI: 1.41–70.65) and walking speed (in m/s) (OR = 0.01, 95%CI: 0.00–0.32) were. CPTS was significantly associated with pre-ulcers (OR = 2.38, 95%CI: 1.02–5.54).
Conclusions
CPTS did not predict plantar foot ulceration in our high-risk participants, but our findings support the mechanical pathway of plantar foot ulceration through pre-ulcer development and indicate lower walking speed as an important predictor. Assessing walking speed and early identifying and treating pre-ulcers will help predict and prevent plantar foot ulcers in high-risk people with diabetes.
What's new?
What is already known?
- Abnormal mechanical stress causes plantar foot ulcers in diabetes.
- Peak pressure is only a moderate predictor for ulceration.
- Cumulative plantar tissue stress (CPTS) may better predict ulceration by integrating different foot-loading factors.
What this study has found?
- Baseline CPTS did not predict ulceration during 12-month follow-up in high-risk people.
- Pre-ulcer presence and lower walking speed were predictors of ulceration.
- CPTS was significantly associated with pre-ulcer presence.
What are the implications of the study?
- This study emphasises the need to assess walking speed and the early identification and treatment of pre-ulcers to improve diabetes-related foot ulcer prediction and prevention.
1 INTRODUCTION
Plantar foot ulcer development in people with diabetes and peripheral neuropathy is strongly associated with abnormal biomechanics while bearing weight.1, 2 These abnormal biomechanics are reflected by higher, mostly repetitive mechanical stresses, suggested to lead to callus formation or pre-ulcerative lesions, and eventually plantar foot ulceration.1, 2 This pathway is the most commonly reported mechanism of diabetes-related plantar foot ulcers.1, 2 Despite 18.6 million people worldwide living with a diabetes-related foot ulcer and 130 million at risk,3 our understanding of the precise role of mechanical stress in plantar foot ulceration remains limited. To help prevent plantar foot ulcers and reduce their impact on people and society, a better understanding of their aetiology is needed.4
Peak plantar pressure is most commonly used to assess foot biomechanics in people with diabetes. While high barefoot peak plantar pressure is a proven risk factor for plantar foot ulcers,5 it is only a moderate predictor.6 Other foot-loading factors, including in-shoe plantar pressure, shear stress, weight-bearing activity and adherence to wearing footwear, have limited or no predictive value in foot ulcers.4, 5 However, the total mechanical stress that the foot endures is the interplay of these foot-loading factors.4, 7, 8 For example, if someone with high barefoot peak plantar pressures uses their pressure-reducing footwear at all times, total mechanical stress is lower than a person with moderate barefoot peak plantar pressure who does not adhere to wearing their footwear. Such differences are captured in the ‘cumulative plantar tissues stress’ (CPTS), a concept in which all foot-loading factors are taken into account. CPTS has therefore been suggested as a better predictor for plantar foot ulceration than any individual foot-loading factor.4, 8 CPTS can be estimated by integrating multiple foot-loading factors in a biomechanical model. Waaijman and colleagues8 found a non-significant trend towards higher CPTS in people who developed a recurrent plantar foot ulcer compared to those who did not. However, in their CPTS model, they only included walking, while people with diabetes and peripheral neuropathy stand longer than they walk, affecting CPTS.9 However, studies to date have shown limited or no predictive value for CPTS in plantar foot ulceration, meaning that further investigation is needed.5 We recently developed a more comprehensive CPTS model that includes both walking and standing, better reflecting the mechanical stress on the foot.10 The mechanical pathway of plantar foot ulceration suggests that CPTS may be indirectly linked to ulceration via callus formation or pre-ulcerative lesions,2, 11, 12 known predictors of plantar foot ulcers.2, 8, 11-14 However, the relationship between CPTS, callus formation or pre-ulcerative lesions, and plantar foot ulceration remains unclear.
We primarily aimed to investigate the predictive value of CPTS alongside socio-demographic and clinical characteristics in plantar foot ulceration in high-risk people with diabetes, and hypothesised that CPTS is an independent predictor of plantar foot ulceration.5, 8 Secondarily, we explored the association between CPTS and abundant calluses and pre-ulcerative lesions, to for the first time experimentally test the mechanical pathway of plantar foot ulceration.1, 2
2 METHODS
2.1 Participants
The DIAbetic foot LOAD capacity study (DIALOAD) is a 12-month prospective observational study, prospectively registered in the Dutch Trial Registry (https://onderzoekmetmensen.nl/en/trial/26874; NL8839) and reported according to the STROBE statement.15 Participants were recruited between August 2020 and May 2022 at Amsterdam University Medical Centre (UMC), location AMC and VUmc, and podiatry practice ‘Voeten op Texel’, in the Netherlands.
The inclusion criteria were: age ≥18 years, diagnosis of diabetes mellitus type 1 or 2, loss of protective sensation. In addition, people had to have had a foot ulcer heal in the 1 year before inclusion or a barefoot peak plantar pressure >600 kPa at any region in either foot or both. The exclusion criteria were: a foot ulcer, amputation wound, active Charcot neuro-osteoarthropathy, toe pressure <30 mmHg16 or continuous use of a walking aid for full body support. Written informed consent was obtained from all participants prior to inclusion. All study procedures were in accordance with the Declaration of Helsinki. The requirement for ethical review of the study was waived under the Medical Research Involving Human Subjects Act in the Netherlands by the medical ethics committee of Amsterdam UMC (W19_429#19.495).
2.2 Study procedures
2.2.1 At baseline
A trained investigator screened participants for socio-demographic characteristics and medical and ulcer history, and examined participants' feet for deformities, bony prominences and amputations. According to International Working Group on the Diabetic Foot (IWGDF) guidelines, we tested for loss of protective sensation using a 10-gram monofilament and tuning fork, and vascular status by testing pedal pulses.12 In addition, photographs of participants' feet were taken from the plantar, dorsal, medial and lateral view, plus close-ups from any potential pre-ulcerative lesion or abundant callus. We defined a pre-ulcerative lesion as an intra- or subcutaneous haemorrhage, blister or skin fissure, not penetrating into the dermis.17 We defined abundant callus as increased thickness of the outer layer of the skin requiring foot care.17 For the remainder of the manuscript, we use the term ‘pre-ulcers’ to denote both pre-ulcerative lesions and abundant callus.
Details of the measurement equipment, participant instructions, criteria for valid data, analysis method and outcomes are provided in Appendix S1.
Barefoot plantar pressures during walking and standing were measured using the EMED-X platform (Novel GmbH, Munich, Germany). In-shoe plantar pressures during walking and standing were measured at the sock–insole interface in the participant's most commonly used footwear using the Pedar-X system (Novel GmbH, Munich, Germany). In this footwear, walking speed was determined during midgait walking (i.e. self-selected walking speed) using two photocells (Tag Heuer, Neuchâtel, Switzerland) at Amsterdam UMC, and using pylons and a stopwatch at podiatry practice ‘Voeten op Texel’. No debridement was performed prior to measuring plantar pressures.
2.2.2 After baseline
Weight-bearing activities of daily life and use of prescribed footwear were measured for seven consecutive days directly after baseline. Weight-bearing activities (i.e. walking steps and standing duration) were measured using a tri-axial accelerometer, worn on the back of the participant at the 5th lumbar vertebra level (MoveMonitor, McRoberts, the Hague, the Netherlands). Wearing time of prescribed footwear was measured using a validated temperature sensor (Orthotimer, Rollerwerk, Balingen, Germany) that was secured in the proximal midfoot region of the left or right insole, under the top layer, to avoid risk to the participant.18 A maximum of four pairs of footwear were equipped. Adherence to wearing footwear was calculated as the proportion of steps and standing duration that the prescribed footwear was worn, per day (Appendix S1).
2.3 Cumulative plantar tissue stress
2.3.1 Note equation 1
‘CPTSregion’ concerns the cumulative plantar tissue stress level in the forefoot region with the highest barefoot peak plantar pressure (expressed as GPa.s/day); ‘activity’ concerns the specific activity, either walking or standing; ‘condition’ concerns the specific plantar pressure measurement, either barefoot or in-shoe; ‘PTIregion’ concerns the pressure–time integral level in the forefoot region with the highest barefoot peak plantar pressure (expressed as kPa.s); and ‘activity level’ concerns the activity level of walking (expressed as number of strides) and of standing (expressed as the total standing duration in seconds).
2.4 Primary outcome—plantar foot ulceration
The primary outcome was the percentage of participants who developed one or more plantar foot ulcers in 12 months, defined as ‘a break of the skin of the foot that involves a minimum the epidermis and part of the dermis at the plantar foot surface’.17 During follow-up, participants were instructed to call the investigating team if they identified or suspected a foot ulcer. In addition, participants had 3-monthly study visits, during which the investigator asked about any foot ulcer in the previous months and checked the feet for ulcers. Furthermore, participants' medical and podiatry records were screened for foot ulcers. Plantar foot ulcer identified during visits were photographed. If an ulcer was reported by the medical team, photographs were collected from the medical record. These photographs were assessed and confirmed by a non-involved experienced podiatrist or rehabilitation physician, blinded to the participant's level of CPTS, for confirmation of ulcer presence.
2.5 Pre-ulcer presence assessment
Three assessors (i.e. a rehabilitation specialist, podiatrist and investigator), all blinded for CPTS or ulcer outcomes, scored the photographs taken at baseline for plantar pre-ulcer(s) presence in the fifth metatarsal base, first to fifth metatarsal heads, hallux and second to fifth digits. Fleiss' kappa was 0.69, showing substantial agreement between assessors for all regions scored.19 All disagreements were discussed with a fourth assessor (an investigator) to reach final consensus on pre-ulcer presence at baseline.
2.6 Sample size calculation
We expected that 40% of participants would develop a foot ulcer within 12 months.1 To avoid overfitting in the CPTS prediction model for the primary aim, 5 to 9 cases per variable were needed.20 Under these conditions, a sample size of 60 participants, with no expected loss to follow-up, was required to investigate the prediction of plantar foot ulceration through CPTS level and other related parameters.
2.7 Data imputation
Primary outcome data were complete for all but one participant, who passed away 6 months after study start. For data analysis, we used the last observation carried forward. Missing data were processed with multiple imputation using a fully conditional specific predictive mean matching model, based on iterated conditional models, using variables associated with the missing data as predictors. This was required for weight-bearing activity (n = 4), using the variables ‘living alone’, ‘use of walking aid’ and ‘employed’, and for adherence to wearing footwear (n = 7), using ‘HbA1c’, ‘fit of footwear’ and ‘physical functioning’.21
2.8 Statistical analysis
Statistical analyses were performed using SPSS Statistics for Windows, version 28 (IBM Corp., Armonk, N.Y., USA) using a significance level of p < 0.05. We used Student's t-test, Mann–Whitney test and chi-squared test in univariate analyses to compare people with a plantar foot ulcer with those without during 12-month follow-up.
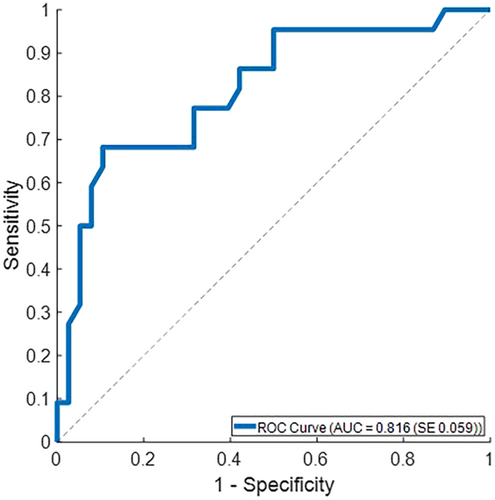
A backward multiple logistic regression analysis was used to investigate whether the baseline level of CPTS (i.e. independent variable) predicted plantar foot ulceration (i.e. outcome). We focused in this study on the first developed plantar forefoot ulcer during follow-up; therefore, subsequent ulcers and ulcers located in the midfoot and hindfoot were not included in the analyses. The level of CPTS per participant was determined in the forefoot region with the highest CPTS level in either the left or the right foot (considering the forefoot is most susceptible for plantar foot ulcers22). Baseline characteristics that differed significantly between both groups were also included in the regression model. The assumption of collinearity between predictors (correlation coefficient >0.5 or <−0.5, or a variance inflation factor >2.5) led us to exclude the predictor with the weaker association found with the other characteristics. The assumption of linearity of continuous predictors was tested using an interaction term of the continuous predictor and its logit in the regression analysis. Significant interaction terms were added to the model. The performance of the final regression model was tested using the receiver-operating characteristic (ROC) curve and the area under the ROC curve (AUC).
A similar analysis was performed using CPTS in the forefoot region that was selected based on clinical history (Appendix S2).
A generalised estimating equation analysis was used to test the association between CPTS and pre-ulcer presence at baseline; we compared CPTS between forefoot regions with and without a pre-ulcer present. The outcome variable was the presence of a pre-ulcer in each forefoot region at baseline, and the covariate was the level of CPTS in the corresponding region, using a logistic regression framework. The analysis incorporated a repeated measures approach, accounting for clustering of data within participants and within-participant correlation across the left and right foot and the different forefoot regions.
3 RESULTS
3.1 Participants
We informed 103 people about the DIALOAD study, of which 63 signed informed consent and 60 were included after screening for eligibility criteria (Appendix S3). All but one participant had a high foot ulcer risk, stratified as IWGDF risk 3.12
During 12-month follow-up, 22 participants (37%) developed a plantar forefoot ulcer (see Appendix S4 for a flowchart on ulcer development). Median time to plantar foot ulceration was 5 months after study start and 7 months after healing of the last ulcer.
Participants with a plantar foot ulcer compared to those without had a significantly shorter time since healing of their last ulcer before baseline (1 [interquartile range (IQR) 0; 6] vs. 6 [IQR 2; 19] months, p = 0.003), more often a pre-ulcer (91% vs. 61%, p = 0.012), a lower walking speed (0.9 vs. 1.1 m/s, p = 0.002) and were more often users of a walking aid (46% vs. 11%, p = 0.002) (Table 1, Appendix S5).
| All participants (n = 60) | Participants with plantar foot ulcer (n = 22) | Participants plantar-ulcer-free (n = 38) | p-value | |
|---|---|---|---|---|
| Age (years) | 65.3 (SD 9.2) | 66.1 (SD 9.7) | 64.9 (SD 9.0) | 0.624 |
| Gender (% (n)) | 0.173 | |||
| Female | 18% (n = 11) | 27% (n = 6) | 13% (n = 5) | |
| Male | 82% (n = 49) | 73% (n = 16) | 87% (n = 33) | |
| Diabetes type (% (n)) | 0.159 | |||
| Type 1 | 18% (n = 11) | 9% (n = 2) | 24% (n = 9) | |
| Type 2 | 82% (n = 49) | 91% (n = 20) | 76% (n = 29) | |
| Diabetes duration (years) | 18.8 (SD 11.5) | 19.2 (SD 9.4) | 18.5 (SD 12.7) | 0.827 |
| Body mass index (kg/m2) | 29.6 (SD 5.4) | 30.5 (SD 5.7) | 29.1 (SD 5.2) | 0.346 |
| HbA1c | ||||
| mmol/mol |
60 (SD 17) (n = 53) |
63 (SD 19) |
59 (SD 16) (n = 31) |
0.391 |
| % |
7.7 (SD 3.4) (n = 53) |
7.9 (SD 3.9) |
7.5 (SD 3.6) (n = 31) |
|
| Ulcer history (% (n)) | 0.274 | |||
| Yes | 97% (n = 58) | 100% (n = 22) | 95% (n = 36) | |
| No | 3% (n = 2) | 0% (n = 0) | 5% (n = 2) | |
| Time since last ulcer healed (months)a |
4.0 [IQR 1.0; 12.0] (n = 55) |
1.0 [IQR 0.0; 6.0] |
5.5 [IQR 2.1; 19.0] (n = 33) |
0.003 |
| Presence of pre-ulcer (% (n)) | 0.012 | |||
| Yes | 72% (n = 43) | 91% (n = 20) | 61% (n = 23) | |
| No | 28% (n = 17) | 9% (n = 2) | 39% (n = 15) | |
| Living alone (% (n)) | 0.957 | |||
| Yes | 45% (n = 27) | 45% (n = 10) | 45% (n = 17) | |
| No | 55% (n = 33) | 55% (n = 12) | 55% (n = 21) | |
| Use of walking aid (% (n)) | 0.002 | |||
| Yes | 23% (n = 14)b | 45% (n = 10) | 11% (n = 4) | |
| No | 77% (n = 46) | 55% (n = 12) | 89% (n = 34) | |
| Employed (% (n)) | 0.171 | |||
| Yes | 43% (n = 26) | 32% (n = 7) | 50% (n = 19) | |
| No | 57% (n = 34) | 68% (n = 15) | 50% (n = 19) | |
| Education level (% (n)) | 0.788 | |||
| Low | 27% (n = 16) | 32% (n = 7) | 24% (n = 9) | |
| Medium | 25% (n = 15) | 23% (n = 5) | 26% (n = 10) | |
| High | 48% (n = 29) | 45% (n = 10) | 50% (n = 19) | |
| Foot deformities (% (n))c | 0.498 | |||
| Absent | 0% (n = 0) | 0% (n = 0) | 0% (n = 0) | |
| Mild | 3% (n = 2) | 0% (n = 0) | 5% (n = 2) | |
| Moderate | 82% (n = 49) | 82% (n = 18) | 82% (n = 31) | |
| Severe | 15% (n = 9) | 18% (n = 4) | 13% (n = 5) | |
| Amputation (% (n)) | 0.367 | |||
| Above ankle | 3% (n = 2) | 5% (n = 1) | 3% (n = 1) | |
| Below ankle | 35% (n = 21) | 45% (n = 10) | 29% (n = 11) | |
| No | 62% (n = 37) | 50% (n = 11) | 68% (n = 26) | |
| Footwear type (% (n))d | 0.515 | |||
| Fully custom-made | 63% (n = 38) | 73% (n = 16) | 58% (n = 22) | |
| Semi custom-made | 25% (n = 15) | 18% (n = 4) | 29% (n = 11) | |
| Not custom-made | 12% (n = 7) | 9% (n = 2) | 13% (n = 5) | |
| Possessing indoor custom-made footwear (% (n)) | 0.789 | |||
| Yes | 20% (n = 12) | 18% (n = 4) | 21% (n = 8) | |
| No | 80% (n = 48) | 82% (n = 18) | 79% (n = 30) | |
| Self-selected walking speed (m/s) | 1.07 (SD 0.25) | 0.94 (SD 0.28) | 1.14 (SD 0.21) | 0.002 |
| Timed up and go test duration (s)a |
12.5 [IQR 11.0; 14.9] (n = 59) |
14.4 [IQR 11.3; 15.9] (n = 21) |
12.4 [IQR 10.6; 13.3] | 0.069 |
- Note: Continuous data are mean (SD standard deviation) or median [interquartile range (IQR) 25th interquartile; 75th interquartile], and discrete data are percentage (number).
- Abbreviation: HbA1c, glycated haemoglobin.
- a Mann–Whitney test used for statistics.
- b Walking aids used were a cane (n = 10), mobility scooter (n = 3), rollator (n = 4) and other walking aids (n = 3). Some participants used multiple walking aids; therefore, the number of walking aids does not correspond to the number of participants who used a walking aid.
- c Foot deformity was classified as absent, mild, moderate and severe.8
- d Fully custom-made footwear = custom insoles in custom shoes, semi custom-made footwear = custom insoles in off-the-shelf extra-depth shoes, and regular = off-the-shelf shoes.
3.2 Prediction of plantar foot ulceration by CPTS
CPTS level was not significantly different between the plantar ulcer and plantar-ulcer-free groups (1.35 [IQR 0.74; 1.95] vs. 1.36 [IQR 0.89; 2.17] GPa.s/day, respectively, p = 0.560, Figure 1). Furthermore, no significant group differences were found for the level of barefoot and in-shoe plantar pressure, weight-bearing activity and footwear adherence (all p > 0.05, Table 2).
| All participants (n = 60) | Participants with plantar foot ulcer (n = 22) | Participants plantar-ulcer-free (n = 38) | p-value | |
|---|---|---|---|---|
| CPTS (GPa.s/day) | 1.36 [IQR 0.86; 2.12] | 1.35 [IQR 0.74; 1.95] | 1.36 [IQR 0.89; 2.17] | 0.560 |
| Barefoot plantar pressure | ||||
| Walking PTI (kPa.s) | 444 [IQR 251; 669] | 537 [IQR 244; 799] | 384 [IQR 239; 644] | 0.125 |
| Standing PTI (kPa.s) | 186 [IQR 141; 300] | 185 [IQR 139; 335] | 189 [IQR 138; 278] | 0.866 |
| Walking PPP (kPa) | 919 [IQR 611; 1207] | 1060 [IQR 709; 1260] | 889 [IQR 594; 1179] | 0.249 |
| Standing PPP (kPa) | 186 [IQR 141; 300] | 185 [IQR 139; 335] | 189 [IQR 138; 278] | 0.866 |
| In-shoe plantar pressure | ||||
| Walking PTI (kPa.s) | 79 [IQR 66; 97] | 82 [IQR 70; 114] | 77 [IQR 59; 92] | 0.177 |
| Standing PTI (kPa.s) | 70 [IQR 48; 100] | 71 [IQR 51; 101] | 70 [IQR 47; 100] | 0.613 |
| Walking PPP (kPa) | 192 [IQR 151; 251] | 188 [IQR 169; 232] | 194 [IQR 138; 259] | 0.890 |
| Standing PPP (kPa) | 79 [IQR 58; 111] | 87 [IQR 58; 108] | 78 [IQR 56; 112] | 0.707 |
| Weight-bearing activity (per day) | ||||
| Number of steps | 5087 [IQR 2699; 7916] | 4508 [IQR 1812; 6915] | 5745 [IQR 3389; 8942] | 0.149 |
| Day-to-day variation in stepsa | 1674 [IQR 911; 2717] | 1783 [IQR 862; 2529] | 1669 [IQR 913; 2953] | 0.895 |
| Standing duration (min) | 119 [IQR 82; 140] | 113 [IQR 71; 141] | 121 [IQR 83; 145] | 0.500 |
| Adherence to wearing footwear (% per day) | ||||
| Walking | 71 [IQR 54; 81] | 71 [IQR 59; 75] | 71 [IQR 53; 82] | 0.759 |
| Standing | 65 [IQR 51; 78] | 63 [IQR 53; 76] | 65 [IQR 51; 79] | 0.976 |
- Note: Continuous data are median [interquartile range (IQR) 25th interquartile; 75th interquartile].
- Abbreviations: CPTS, cumulative plantar tissue stress; PTI, pressure–time integral; PPP, peak plantar pressure.
- a Calculated as the standard deviation of the number of steps per day using data from all valid days.
Together with the level of CPTS, ‘time since last ulcer healed’, ‘presence of pre-ulcer’ and ‘self-selected walking speed in the laboratory’ were included in the regression analysis (based on significant group differences found, Table 1, and sufficiently low correlations and variance inflation factors, Appendix S6). The baseline characteristic ‘use of walking aid’ was excluded due to high correlation with walking speed (r = −0.57). The interaction terms were not included in the analysis (all p > 0.05).
CPTS (in GPa.s/day) was not a significant predictor of plantar foot ulceration (odds ratio (OR) = 0.90 (95% confidence interval (CI): 0.50–1.59), Beta coefficient (β) = −0.11 (standard error (SE) = 0.29), p = 0.705). Significant predictors of plantar foot ulceration were pre-ulcer presence (OR = 9.97 (95%CI: 1.41–70.65), β = 2.30 (SE = 1.00), p = 0.021) and walking speed (in m/s) (OR = 0.01 (95%CI: 0.00–0.32), β = −4.43 (SE = 1.67), p = 0.008). The AUC was 0.82 (SE = 0.06), indicating good discriminative ability (Figure 2).
The regression analysis performed using CPTS in the forefoot region, selected based on clinical history and showed comparable results (Appendix S2).
3.3 Association of CPTS and pre-ulcers
CPTS was significantly higher in forefoot regions with a pre-ulcer at baseline compared to regions without (0.93 [IQR 0.49; 1.48] vs. 0.58 [IQR 0.35; 0.88] GPa.s/day, respectively, p < 0.001). In the generalised estimating equations analysis, higher CPTS was significantly associated with pre-ulcers (OR = 2.38 (95%CI: 1.02–5.54), β = 0.87 (SE = 0.43), p = 0.045).
4 DISCUSSION
In 12 months, 22 of the 60 participants developed a plantar foot ulcer, a recurrence rate of 37% that is consistent with previous studies.1 Contrary to our hypothesis, the level of CPTS at baseline did not predict plantar foot ulceration during the 12-month follow-up. This shows that ulcers can develop in high-risk individuals with low CPTS, while others remain ulcer-free despite high CPTS. Significant predictors of plantar foot ulceration were pre-ulcer presence and a lower walking speed—both assessed at baseline—the latter being a novel finding. Additionally, at baseline, CPTS was significantly associated with pre-ulcer presence in the forefoot region. Our findings increase our understanding of plantar foot ulcer development in high-risk people with diabetes, provide new evidence for the mechanical pathway of plantar ulceration and show two easy-to-obtain strong parameters for predicting plantar foot ulceration.
CPTS is more representative of the mechanical load on the foot than the individual foot-loading factors that determine CPTS because it combines plantar pressure, weight-bearing activity and footwear adherence to represent cumulative mechanical load.4, 7, 8 However, its use did not improve ulcer prediction. Our findings align with Waaijman and colleagues,8 who found no significant difference in CPTS between people who developed a plantar foot ulcer and those who did not. Possible explanations for the lack of predictive value of CPTS may include limitations in CPTS-model accuracy. Our CPTS model did not include shear stress because validated measurement equipment does not exist, despite its suggested role in plantar foot ulceration.4 Secondly, we modelled CPTS based on 1-week measurements. The lack of continuous measurement of CPTS and dependency on models may affect representation of the true and current mechanical stress on the foot.4 While smart systems for continuous plantar pressure monitoring exist,23 their validity and reliability are still unknown; spatial resolution is low, and pressure is not measured directly at the skin.24 Thirdly, we did not measure load-bearing capacity, that is the ability of the skin and underlying soft tissue to tolerate mechanical stress without breaking down.25 The load-bearing capacity differs among individuals and may affect the association between CPTS and ulceration.26, 27 While regional plantar pressures, pre-ulcers (i.e. tissue damage) and lower walking speed (reflecting lower general health) may act as surrogates of load-bearing capacity, direct assessment will likely improve ulcer prediction. Lastly, latent aspects within the foot-loading factors may influence CPTS or ulceration, which traditional statistical techniques cannot identify; machine learning techniques may help to identify such associations.
Pre-ulcer presence and lower walking speed at baseline were strong predictors of plantar foot ulceration (ORs of 10 and 0.01, respectively). The AUC was 0.82, which is high for just two parameters. In comparison, previous models using five biomechanical and clinical predictors and seven easy-to-obtain clinical predictors found AUCs of 0.68 and 0.66, respectively.13, 14 Pre-ulcer presence was a predictor in these models.13, 14 A lower walking speed was found in people with diabetes-related foot ulcers compared to people without ulcers or diabetes.28 However, walking speed was not considered in previous prediction models, making it a novel factor strongly increasing predictive power. Lower walking speed reflects a lower general health or pre-frailty status in older adults,29 suggesting that people with diabetes at high ulcer risk who walk slower may be physically more deconditioned and frailer, increasing the vulnerability of their plantar soft tissue to break down.26 An increase in weight-bearing activity during follow-up may potentially increase the risk of ulceration due to reduced tolerance of plantar tissue to mechanical loading; however, the relationship between weight-bearing activity and foot ulceration is not straightforward and requires further investigation, including assessment of plantar tissue tolerance, as we have discussed in a recent review.5 Our findings highlight pre-ulcers and a lower walking speed as important clinical markers for identifying those at highest risk for plantar foot ulceration. Clinically, walking speed and pre-ulcer presence should be assessed, with pre-ulcers closely monitored and treated to improve prediction and prevention of plantar foot ulcers in high-risk people.
Higher CPTS levels were significantly associated with pre-ulcer presence in forefoot regions at baseline. This was expected, as pre-ulcers have been reported to develop as a result of mechanical stress; however, this had not yet been experimentally proven.1, 2 Our combined findings of an association between CPTS levels and pre-ulcers, and pre-ulcers being a strong predictor of plantar foot ulceration, support the mechanical pathway of diabetes-related foot ulceration.1, 2 While providing valuable insights, these results do not yet imply causation, as CPTS and pre-ulcers were assessed cross-sectionally. Future studies should include pre-ulcers as outcomes over time, to further support the mechanical pathway of plantar foot ulceration.
A strength of our study was the objective measurement of all foot-loading factors using validated equipment and the most comprehensive CPTS model available, given the available equipment.10 However, measuring foot-loading parameters and calculating CPTS is challenging and labour-intensive because it requires multiple sensors, complex algorithms and technically skilled people, limiting its clinical application.30 By contrast, the strong predictors—walking speed and pre-ulcer presence—are both easily accessible in any foot care practice worldwide. Lastly, this study focused on recurrent plantar foot ulcers in high-risk people with diabetes, where known predictors like neuropathy and ulcer history were not included, potentially affecting CPTS's predictive power. Larger studies are needed to assess CPTS's predictive power in first-ever plantar foot ulceration and should be initiated in the field.
In conclusion, our study showed that baseline CPTS did not predict plantar foot ulceration during 12-month follow-up in high-risk people with diabetes, implying a lack of direct association. The presence of pre-ulcers and a lower walking speed at baseline were, however, strong predictors of plantar foot ulceration, the latter being a novel finding. In addition, CPTS was associated with pre-ulcer presence, providing support for the mechanical pathway of plantar foot ulceration via pre-ulcers, although causality requires further investigation. Our results emphasise the importance of assessing walking speed and early identification and treatment of pre-ulcers to better predict and prevent plantar foot ulcers in people with diabetes at high ulcer risk.
AUTHOR CONTRIBUTIONS
According to the CRediT statement: C.M.H., J.J.v.N., M.P. and S.A.B. contributed to the conceptualisation; C.M.H., J.J.v.N., M.P. and S.A.B. contributed to the methodology; C.M.H. contributed to the software; C.M.H., J.J.v.N., M.P. and S.A.B. contributed to the validation; C.M.H., J.J.v.N., M.P. and S.A.B. contributed to the formal analysis; C.M.H. and J.J.v.N. contributed to the investigation; C.M.H., J.J.v.N., T.E.B.W., L.W.E.S. and E.J.G.P. contributed to the resources; C.M.H. and J.J.v.N. contributed to the data curation; C.M.H. contributed to writing—original draft; J.J.v.N., T.E.B.W., L.W.E.S., E.J.G.P., M.P. and S.A.B. contributed to writing—review and editing; C.M.H. contributed to visualisation; J.J.v.N., M.P. and S.A.B. contributed to the supervision; C.M.H. and J.J.v.N. contributed to the project administration; J.J.v.N., T.E.B.W., L.W.E.S., E.J.G.P., M.P. and S.A.B. contributed to the funding acquisition. All authors approved the final version of the manuscript. J.J.v.N. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
ACKNOWLEDGEMENTS
The authors thank Angela de Jeu, Jettie Klein-van Daalen, Rimke Lagrand, Karin van de Kamp and Tim van Dun of Amsterdam UMC Centre for Diabetic Foot Complications (ACDC), Amsterdam; and Nicolette van Kooten of podiatry practice ‘Voeten op Texel’, De Cocksdorp, for their help in recruiting participants for the DIALOAD study. The authors thank Angela de Jeu, podiatrist, Amsterdam UMC, Amsterdam, for scoring photos for the presence of pre-ulcers on the foot. The authors thank shoe technicians Jan Pulles and Ghizella Szabo, Livit Ottobock Care, Amsterdam, and Toos Rook, Wittepoel, Rotterdam, for securing the temperature sensors in the insoles of participants' footwear. The authors thank Maartje Dekker, Kim Tijhuis, Caroline Oosterhof, Abe Funnekotter and Jonne van der Poel, all master students Human Movement Sciences of the Vrije Universiteit, Amsterdam, for their help during the measurements of the DIALOAD study. None of the individuals mentioned above received financial support for their help.
FUNDING INFORMATION
This study was supported by research grants from the Amsterdam Movement Sciences research institute and ZGT Wetenschapsfonds.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ARTIFICIAL INTELLIGENCE-ASSISTED TECHNOLOGIES
The authors declare that they have not used any type of generative artificial intelligence for the writing of this manuscript, nor for the creation of images, graphics, tables or their corresponding captions.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding authors upon reasonable request.