Reference curves of motor function outcomes in young steroid-naïve males with Duchenne muscular dystrophy
This original article is commented on by Baranello on pages 557–558 of this issue.
Abstract
Aim
To investigate functional motor performance in a large cohort of young steroid-naïve males with Duchenne muscular dystrophy (DMD) and typically developing males, and to develop specific reference curves for both groups. Also, to describe associations between anthropometric values and functional motor outcomes.
Method
Cross-sectional data of 196 steroid-naïve males with DMD aged 4 to 8 years and 497 typically developing males aged 2 years 6 months to 8 years were included. Both groups were evaluated with the time to rise from the floor test, 10-metre walk/run test, 6-minute walk test, and North Star Ambulatory Assessment. Reference curves with centiles 5%, 10%, 25%, 50%, 75%, 90%, and 95% were estimated using quantile regression.
Results
Males with DMD scored significantly worse on all functional motor outcomes than age-matched typically developing males (p < 0.001): 89% to 95% of the males with DMD scored below the 5th centile of the typically developing males. No or weak correlations exist between anthropometric values and functional motor outcomes.
Interpretation
The estimated reference curves can support consultation with families of young males with DMD and can support the evaluation of treatment for reaching motor skills and functional motor outcomes compared with typically developing males.
Graphical Abstract
This study provides a detailed picture of functional motor outcomes in young steroid-naïve males with Duchenne muscular dystrophy (DMD) compared to typically developing controls. This study was the first to establish DMD specific reference curves for functional motor outcomes: time to rise from floor (TRF), 10-metre walk/run test, 6-minute walk test, and North Star Ambulatory Assessment. Motor outcome reference curves clearly differ between males with DMD and typically developing controls.
This original article is commented on by Baranello on pages 557–558 of this issue.
Abbreviations
-
- 6MWD
-
- 6-minute walking distance
-
- 6MWT
-
- 6-minute walk test
-
- 10 m walk/run
-
- 10-metre walk/run test
-
- DMD
-
- Duchenne muscular dystrophy
-
- FOR-DMD
-
- Finding the Optimum corticosteroid Regime for Duchenne Muscular Dystrophy study
-
- NSAA
-
- North Star Ambulatory Assessment
-
- TRF
-
- time to rise from the floor
What this paper adds
- There is an increasing gap in performance between males with Duchenne muscular dystrophy (DMD) and typically developing males with age.
- Functional motor outcome reference curves for DMD show tipping points at certain ages.
- Functional motor outcome curves for typically developing males show improvement between 2 years 6 months and 8 years.
- Higher variability in DMD motor performance is observed with increasing age.
- Anthropometric values and functional motor outcomes do not correlate in steroid-naïve males with DMD.
Duchenne muscular dystrophy (DMD) is an X-linked recessive neuromuscular disease which affects 1:5000 live newborn males.1 Delay in gross motor milestones is commonly reported as a presenting symptom of DMD. The three motor milestones most likely to be delayed in DMD are sitting alone, walking, and climbing stairs.2, 3 Although many studies report gains in motor function over the first years, young males with DMD do not achieve the same functioning level compared with typically developing children and, after the age of 7 years, motor functions start to decline.4-6 However, the time when males with DMD reach a plateau in motor skills or when they start declining is not yet fully defined and varies from individual to individual and for different functional skills.7
Several outcome measures have been applied to assess functional motor performance of males with DMD.8, 9 Timed function tests, time to rise from the floor (TRF), and the 10-metre walk/run test (10 m walk/run) are often used in clinical practice and research to assess motor function in young males with DMD as these measures seem to be sensitive to detecting changes over time.5, 10, 11 The 6-minute walk test (6MWT) is a further tool that is widely used to assess functional capacity and submaximal endurance in paediatric populations, including ambulant males with DMD.12-14 The North Star Ambulatory Assessment (NSAA) was developed specifically for DMD and is used to monitor disease progression and treatment effects both in clinical settings and in investigational trials.7, 15, 16
Only two studies, including small numbers of participants, have compared different motor outcomes in young, steroid-naïve males with DMD with those in age-matched typically developing males.17, 18 Most studies on functional motor outcomes in young males with DMD include those receiving corticosteroids or do not include a comparison group.19, 20 Reference curves for typically developing males are available for some functional motor outcomes.21 However, we know that young males with DMD develop motor skills in a different way and at a different pace.19 No reference curves specific to DMD exist at the moment. Therefore, the primary objective of this study was to compare motor performance of a large cohort of young, steroid-naïve males with DMD and that of age-matched typically developing males, using different standardized and reliable outcome measures. Second, we aimed to develop DMD-specific reference curves for each outcome measure. These estimated reference curves, based on reliable and standardized collected data, will help in understanding where on the ‘spectrum’ the performance of a male of a certain age at steroid-naïve stages is located compared with peers with DMD of the same age. Finally, we investigated the associations between anthropometric values (height, weight, and body mass index [BMI]) and motor performance in both groups.
METHOD
Participants
Steroid-naïve males with DMD were recruited at 32 sites in five countries (USA, Canada, UK, Germany, and Italy) between January 2013 and September 2016 as part of the Finding the Optimum corticosteroid Regime for Duchenne Muscular Dystrophy (FOR-DMD) study.22 Main study inclusion criteria were males with proximal muscle weakness and confirmed DMD mutation; aged 4 years to 7 years 11 months; ability to rise from the floor; willingness and ability of parent or legal guardian to give informed written consent; and willingness and ability to comply with scheduled visits, drug administration plans, and study procedures. Detailed eligibility criteria have been reported elsewhere.22 The FOR-DMD study was registered at www.clinicaltrials.gov (identifier NCT01603407).22
Typically developing males between 2 years 6 months and 8 years old were recruited from 20 convenient selected nursery and primary schools in Flanders, Belgium, between January 2012 and October 2020, to assess the effect of development on motor function across a broad age range. Parents were asked to complete a health-related questionnaire, created by the authors for this study, before enrolment to exclude cardiovascular, respiratory, neurological, and/or musculoskeletal disorders. The aim of this questionnaire was to exclude any condition that could affect the functional outcome results of the typically developing group. A translation of this questionnaire is given in Appendix S1. Included males had to be able to understand and cooperate with the study procedures. Ethical approval was obtained by the Ethics Committee Research UZ/KU Leuven (S53812, S60777, S59068). Informed written consent was obtained from all institutional boards of the participating schools and parents.
Outcome measures
Timed function tests, TRF, and 10 m walk/run test were used to evaluate functional strength. The 6MWT was used to evaluate submaximal endurance. The NSAA is a disease-specific test including more complex motor skills, such as hopping, jumping, and running, that are generally never fully achieved in untreated males with DMD but only in a proportion of those treated with steroids.16 A ceiling effect with the NSAA has been reported in typically developing children, with 85% of 4-year-old children reaching the full score.18 Instructions on how to administer the described functional motor outcome measures have been previously published.23-25
The timed function tests, 6MWT, and NSAA have proved reliable and valid functional outcomes of motor performance in patients with DMD.10, 16, 18 The reliability of the timed tests has been confirmed starting from the age of 2 years 6 months.21, 26 The 6MWT is valid and reliable for those with DMD starting from the age of 4 years.17 The NSAA can be used in DMD starting from the age of 3 years to assess early functional changes.27
Test procedure
The males with DMD were evaluated cross-sectionally with TRF, 10 m walk/run, NSAA, and 6MWT at the screening (date of consent) and baseline visits as part of the FOR-DMD study. The baseline values were included in this paper; if a baseline value was missing, then the screening value, if available, was substituted for the baseline value.
Also, the data of the typically developing males were cross-sectional. Two hundred and seventy-seven typically developing males performed the timed tests. A randomly selected subgroup of typically developing males between 2 years 6 months and 6 years old also performed the NSAA. A second group of 220 typically developing males aged 5 to 8 years performed the 6MWT. Height and weight absolute values and centiles were calculated in both groups according to the Centres for Disease Control and Prevention recommendations and growth charts, and BMI was calculated.28 Males were grouped by age: 2 years 6 months to younger than 3 years; 3 to younger than 4 years; 4 to younger than 5 years; 5 to younger than 6 years; 6 to younger than 7 years, and 7 to 8 years old.
The males with DMD were evaluated by experienced physiotherapists, who received standardized and face-to-face training as required by the FOR-DMD study protocol. Quality assessment of the data was performed and all included assessments met the criteria for validity on the basis of expert physiotherapist review.
Evaluations of the typically developing males were performed by three experienced physiotherapists or students of the master's programme in Rehabilitation Sciences and Physiotherapy at KU Leuven, under direct supervision of a neuromuscular expert physiotherapist. All evaluators received intensive face-to-face training in test procedures.
Statistical analysis
Age and anthropomorphic characteristics (height, weight, and BMI) were summarized for the total group and different age groups using means, standard deviations (SDs), and ranges. Medians, interquartile ranges (IQR), and total ranges were calculated for the functional motor outcomes. Comparisons of the functional outcomes between the DMD group and typically developing males were made for the different age groups using a Mann–Whitney U test.
The precision of the estimated centiles was deemed acceptable when about 40 children per age group were included in the study. Detailed information about the calculation methods can be found in the previously published normative data papers.13, 21 To construct reference curves, the following centiles of the functional tests were estimated for different ages in months using a quantile regression analysis: 5%, 10%, 25%, 50%, 75%, 90%, and 95%. The interior points algorithm as proposed by Lustig et al. was used to estimate the regression parameters.29 The explanatory variable age was included using restricted cubic splines so that no assumptions had to be made about the type of association with the results on the functional tests. Second, the individual DMD test results were plotted on the curves. Both the reference curves of the typically developing males and the DMD-specific reference curves were estimated from cross-sectional data values. To confirm that the precision of the curves was acceptable, we investigated the 95% confidence intervals.
Finally, associations between the anthropometric values (height, weight, and BMI) and motor outcomes were investigated for both groups. First, absolute values of height and weight were converted to z-scores based on the corresponding centiles. Spearman correlation coefficients were calculated between the z-scores of the anthropometric values (height and weight), BMI, and the functional outcomes. A level of significance of 0.05 was used for hypothesis testing. We used SPSS Statistics 28 (IBM Corp., Armonk, NY, USA) for statistical analysis.
RESULTS
Descriptive statistics
In total, 196 steroid-naïve males with DMD, aged between 4 and 8 years, and 497 typically developing males, from 2 years 6 months up to 8 years, were enrolled in the two studies respectively. Table 1 provides an overview of the characteristics and functional outcomes of both groups.
| DMD | Typically developing | |||
|---|---|---|---|---|
| n | Mean (SD) or median (Q1–Q3) | n | Mean (SD) or median (Q1–Q3) | |
| Anthropometric values | ||||
| Height (cm) | 196 | 110.05 (7.27) | 277 | 109.67 (11.63) |
| Weight (kg) | 196 | 20.02 (3.64) | 277 | 19.20 (4.01) |
| Body mass index (kg/m2) | 196 | 16.46 (1.66) | 277 | 15.86 (1.30) |
| Timed tests | ||||
| Age | 196 |
5 years 9 months (1 year) Range: 4 years 1 month–8 years |
277 |
4 years 10 months (1 year 6 months) Range: 2 years 6 months–8 years |
| TRF (seconds) | 196 | 5.70 (4.30–7.55)a | 277 | 2.35 (1.84–3.15) |
| 10 m walk/run (seconds) | 196 | 6.00 (5.18–7.00)b | 277 | 2.67 (2.23–3.09) |
| 6MWT | ||||
| Age | 149 |
6 years 2 months (10 months) Range: 5–8 years |
164 |
6 years 6 months (10 months) Range: 5–8 years |
| 6MWD (m) | 149 | 347 (302.50–381) | 164 | 508.95 (475–553.88) |
| North Star Ambulatory Assessment | ||||
| Age | 196 |
5 years 9 months (1 year) Range: 4 years 1 month–8 years |
134 |
4 years 3 months (11 months) Range: 2 years 7 months–6 years |
| NSAA (total score) | 196 | 21 (18–25) | 134 | 33 (30–34) |
- a TRF: two males (ages 7 years 1 month and 7 years 9 months) were not able to perform the TRF and one value was missing.
- b 10 m walk/run: one male (age 7 years 7 months) was not able to perform the 10 m walk/run and one value was missing.
- Abbreviations: 6MWD, 6-minute walking distance; 6MWT, 6-minute walk test; 10 m walk/run, 10-metre walk/run test; DMD, Duchenne muscular dystrophy; SD, standard deviation; TRF, time to rise from the floor.
Functional outcomes by age group are reported in Table 2. The results of the timed tests (TRF and 10 m walk/run) of one male with DMD were missing. Two males with DMD (aged 7 years 1 month and 7 years 9 months respectively) were not able to perform the TRF within 30 seconds, and another child (7 years 7 months old) was not able to perform the 10 m walk/run, so they were excluded from the analyses.
| Functional motor outcome | Duchenne muscular dystrophy | Typically developing | |||||
|---|---|---|---|---|---|---|---|
| n | Median (Q1–Q3) | Range | n | Median (Q1–Q3) | Range | p | |
| 2 years 6 months to <3 years | |||||||
| TRF (seconds) | / | / | / | 43 | 3.70 (3.19–4.94) | 2.19–6.26 | NA |
| 10 m walk/run (seconds) | / | / | / | 43 | 5.09 (4.52–5.82) | 3.76–8.74 | NA |
| 6MWD (m) | / | / | / | / | / | / | NA |
| NSAA (total) | / | / | / | 15 | 27 (23–27) | 18–31 | NA |
| 3 to <4 years | |||||||
| TRF (seconds) | / | / | / | 52 | 2.97 (2.48–3.56) | 1.73–6.53 | NA |
| 10 m walk/run (seconds) | / | / | / | 52 | 4.57 (4.04–5.00) | 3.17–6.35 | NA |
| 6MWD (m) | / | / | / | / | NA | NA | NA |
| NSAA (total) | / | / | / | 40 | 30 (28.25–32) | 25–34 | NA |
| 4 to <5 years | |||||||
| TRF (seconds) | 47 | 5.90 (4.50–7.03) | 2.50–13.50 | 53 | 2.31 (2.03–2.68) | 0.90–5.21 | <0.001* |
| 10 m walk/run (seconds) | 47 | 6.50 (5.50–7.20) | 4.20–15.60 | 53 | 3.72 (3.43–3.97) | 2.58–6.15 | <0.001* |
| 6MWD (m) | 47 | 316 (258–351) | 100–396 | / | / | / | NA |
| NSAA (total) | 47 | 20 (16–24) | 11–31 | 41 | 34 (32–34) | 31–34 | <0.001* |
| 5 to <6 years | |||||||
| TRF (seconds) | 75 | 5.00 (3.80–6.70) | 2.10–13.6 | 58 | 1.93 (1.71–2.27) | 0.97–2.97 | <0.001* |
| 10 m walk/run (seconds) | 75 | 5.80 (5.20–6.40) | 3.80–9.80 | 58 | 3.43 (3.25–3.75) | 2.38–4.73 | <0.001* |
| 6MWD (m) | 75 | 331 (298–375) | 100–445 | 56 | 482.45 (445.50–506.53) | 375–560 | <0.001* |
| NSAA (total) | 75 | 21 (18–26) | 9–31 | 38 | 34 (34–34) | 33–34 | <0.001* |
| 6 to <7 years | |||||||
| TRF (seconds) | 44 | 5.25 (4.13–6.65) | 2.80–18.50 | 40 | 1.89 (1.34–2.42) | 1.00–4.13 | <0.001* |
| 10 m walk/run (seconds) | 44 | 5.90 (4.83–6.60) | 4.10–9.00 | 40 | 3.13 (2.82–3.51) | 2.38–3.89 | <0.001* |
| 6MWD (m) | 44 | 363.50 (325.25–383.50) | 225–475 | 52 | 521.80 (473.95–555.42) | 375–668 | <0.001* |
| NSAA (total) | 44 | 23 (20–27.25) | 11–32 | / | NA | ||
| 7 to 8 years | |||||||
| TRF (seconds) | 28 | 9.00 (5.65–14.05) | 2.80–30.60 | 31 | 1.83 (1.49–2.34) | 1.18–3.50 | <0.001* |
| 10 m walk/run (seconds) | 29 | 6.90 (5.60–8.00) | 4.50–11.40 | 31 | 2.83 (2.65–3.28) | 1.96–3.81 | <0.001* |
| 6MWD (m) | 30 | 348.50 (311.25–380.25) | 179–481 | 56 | 549.90 (522.25–602.17) | 400–719 | <0.001* |
| NSAA (total) | 30 | 20 (14.75–22.50) | 6–32 | / | NA | ||
- For the TRF, a cut-off of 30 seconds was set as the maximum upper score to consider it as a valid test (McDonald et al.26).
- * Significant at p < 0.05 (Mann–Whitney U test).
- Abbreviations: /, no data available; 6MWD, 6-minute walking distance; 10 m walk/run, 10-metre walk/run test; NA, not applicable; NSAA, North Star Ambulatory Assessment; TRF, time to rise from the floor.
Between-group comparisons
Males with DMD in all age groups performed significantly worse on all functional motor outcomes than typically developing males (p < 0.001) (Table 2 and Appendix S2). The median times to perform the timed function tests in the typically developing males decreased over the total age range (Table 2). In the DMD group, median times first decreased between males aged 4 to 5 years, followed by slower times in males aged 6 to 7 years (Table 2). Consequently, the gap between typically developing males and males with DMD widened in the older age groups. Appendix S3 provides additional information on the corresponding velocities of the TRF and 10 m walk/run test. Median 6-minute walking distance (6MWD) in the typically developing group increased from ages 5 to 7 years. In the DMD group, median 6MWD also increased between males aged 4 to 6 years, followed by a decrease in the older males (Table 2). Finally, in the typically developing group, the median total NSAA scores increased from 27 to 34 between the youngest and oldest groups (Table 2). All but four 5-year-old typically developing males obtained the maximum score of 34. Four males scored 33 out of 34: one male used compensation while standing on one foot (left), two males lifted the head only partly or with compensation, and one male was not able to raise both feet completely while standing on heels. The median NSAA scores of the DMD group first increased between the 4- and 6-year-olds and then decreased. None of the steroid-naïve males with DMD achieved the maximum total score of 34 at any age (Table 2). Items that were difficult for them were rise from the floor, with only 2.6% of the males with DMD being able to do so without any compensation (NSAA-item 11: score 2) and 94.4% using compensatory movements (score 1); lifts head (NSAA-item 12), with only 17.3% receiving a score 2; getting to sitting position, with 76.5% of the males with DMD using a modified method (NSAA-item 10: score 1); hopping, with only 8.2% to 9.2% being able to hop with the left or right leg respectively without any compensation (NSAA-items 15 and 16: score 2); and 44% to 46% of the males unable to hop (score 0) (Appendix S4).
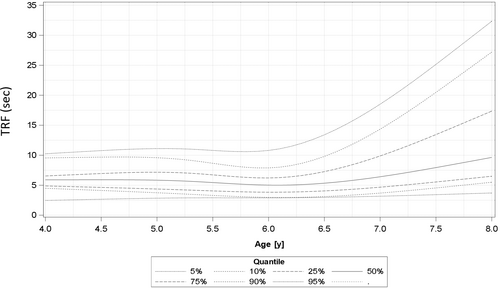
Individual results of timed function tests and 6MWT from males with DMD are plotted on the typically developing estimated reference curves in Figure 1. Males with DMD showed a wider variability in performance than typically developing males. No reference curve was made for the NSAA because 89.5% of the typically developing males received the maximum total NSAA score by the age of 5 years.
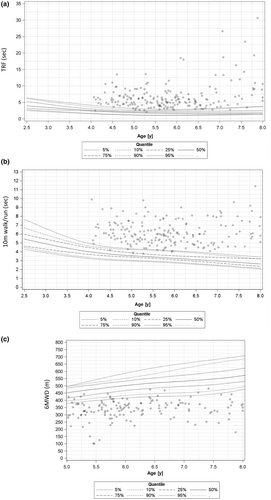
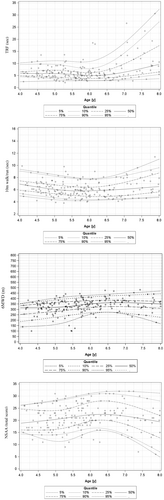
Figure 2 shows DMD-specific estimated reference curves for the timed function tests, 6MWT, and NSAA with individual data plots of the males with DMD. Clean DMD-specific estimated reference curves for clinical use are shown in Appendix S5.
Associations between anthropometric values and functional motor outcomes
For the males with DMD, no correlations were found between the z-scores of anthropometric values (height and weight), BMI, and the functional motor outcomes. Also, only weak correlations were found in the comparison group (Table 3).
| DMD | Typically developing | DMD | Typically developing | DMD | Typically developing | |
|---|---|---|---|---|---|---|
| Height z-score | Height z-score | Weight z-score | Weight z-score | BMI | BMI | |
| TRF (seconds) | −0.01 | −0.15 | −0.03 | 0.000 | −0.04 | 0.18* |
| p = 0.86 | p = 0.011 | p = 0.71 | p = 0.996 | p = 0.58 | p = 0.002 | |
| Velocity, TRF | −0.01 | −0.15 | 0.01 | 0.000 | 0.05 | −0.18* |
| p = 0.89 | p = 0.011 | p = 0.86 | p = 0.996 | p = 0.49 | p = 0.002 | |
| 10 m walk/run (seconds) | −0.12 | −0.17* | −0.15 | −0.03 | −0.16 | 0.17* |
| p = 0.09 | p = 0.005 | p = 0.03 | p = 0.68 | p = 0.03 | p = 0.006 | |
| Velocity, 10 m walk/run | 0.12 | 0.17* | 0.15 | 0.03 | 0.16 | −0.10* |
| p = 0.09 | p = 0.005 | p = 0.03 | p = 0.68 | p = 0.03 | p = 0.006 | |
| 6MWD (m) | 0.04 | 0.03 | −0.01 | 0.08 | −0.05 | 0.17 |
| p = 0.56 | p = 0.74 | p = 0.87 | p = 0.24 | p = 0.46 | p = 0.01 | |
| NSAA (total score) | 0.01 | −0.016 | 0.05 | −0.009 | 0.08 | −0.04 |
| p = 0.87 | p = 0.86 | p = 0.49 | p = 0.91 | p = 0.26 | p = 0.65 |
- * Significant at p < 0.01.
- Abbreviations: 6MWD, 6-minute walking distance; 10 m walk/run, 10-metre walk/run test; BMI, body mass index; DMD, Duchenne muscular dystrophy; NSAA, North Star Ambulatory Assessment; TRF, time to rise from the floor.
DISCUSSION
This study provides a detailed picture of functional motor outcomes in young steroid-naïve males with DMD compared with typically developing males. In addition, the estimated reference curves for functional outcomes will enable assessment of a young male with DMD in relation to the expected performance in aged-matched typically developing males as well as other males with DMD.
We found that males with DMD needed significantly more time to complete the timed function tests and walked less distance in 6 minutes than their typically developing peers. For example, 91% and 95% of the males with DMD needed more time than the 5% slowest typically developing males for the TRF and 10 m walk/run respectively. Similarly, starting from the age of 5 years, 89% of the males with DMD walked a shorter 6MWD than the 5th centile of the typically developing males. Males with DMD, as young as 4 years, received significantly lower scores on the NSAA than typically developing males. These results are in line with previous findings.4-6 We also found that young males with DMD between 4 and 8 years old were not able to attain the maximum score on the NSAA, whereas 89.5% of the 5-year-old typically developing males did. Our findings confirm results of previous studies showing that young steroid-naïve males with DMD have a delay in reaching some motor milestones, such as standing on one leg, while they rarely achieve other motor skills, such as hopping and rising from the floor without compensation, irrespective of age (Appendix S4).18, 30 An explanation of the lower scores on functional outcomes in young males with DMD might be muscle weakness that is already present in males with DMD between 4 and 7 years old.31 Beenakker et al. showed that a small reduction in muscle force can be accompanied by a large reduction in functional ability.11 Also, the more general developmental delay, often seen in DMD, might affect their performance at the early stages as well as the presence of contractures at the ankle.32-34 Young males with DMD show a functional plateau or decline in functioning starting from the age of 6 years to 6 years 6 months old, whereas typically developing males show better scores in all motor functional outcomes with increasing age. Consequently, there is an increasing gap in performance between males with DMD and their typically developing peers with increasing age. This supports the importance of the development of DMD-specific estimated reference curves to assess how a male with DMD performs compared with peers with DMD.
The DMD-specific estimated reference curves were developed on the basis of the cross-sectional FOR-DMD data. Younger males up to the age of 6 years to 6 years 6 months performed better in the timed function tests and the NSAA than older children. On the 6MWT higher variability was observed, with some 7-year-olds with DMD walking longer distances. These results confirm those of previous studies, including both steroid-treated and -naïve males, which showed that early functional improvements in young males with DMD were followed by waning performance with advancing age caused by disease progression.4, 19, 20 The timed function tests primarily measure muscle strength, whereas the 6MWT was developed to evaluate cardiopulmonary function and endurance. While children with DMD are expected to show muscle weakness starting from a young age, cardiopulmonary function and endurance are not expected to be compromised in these young males. Moreover, the 6MWT requires attention and child compliance which can improve with age and practice. A higher variability in all the motor performances was also observed in the older groups, aged 6 years to 6 years 6 months and above, compared with the younger males. The increasing variability in performance over time can be explained by DMD disease progression which affects each male differently.4
Current care recommendations for DMD support the initiation of corticosteroids before the functional decline starts.15 Moreover, early treatment seems to be associated with better long-term effects on motor outcomes.15 Our study confirms that males with DMD already show a functional plateau or decline from the age of 6 years, supporting the initiation of corticosteroids at a young age. An early initiation of steroids in males on the lower centiles for their age group might be considered to optimize motor function benefits. While a comprehensive evaluation of motor skills in young children remains key to drive clinical management, our study suggests that timed function tests might be more sensitive in detecting early signs of functional decline than the NSAA and 6MWT.
Finally, no or weak associations were found between the anthropometric values and functional motor outcomes in both groups. This indicates that in young, steroid-naïve males with DMD other factors such as age and the associated maturational effects might be important explanatory factors for the evolution of the functional motor outcomes. Slight differences in correlations might be explained by the fact that males with DMD do not follow the same growth curves as typically developing males. Moreover, the improvement in motor performance with maturation in typically developing children might not be seen in those with DMD as maturational improvements might be overtaken by progressive disease-related loss of functional capacity. In typically developing children, a strong association is found between height and stride length which can be captured in the 6MWD and 10 m walk/run. Change in stride length is a major determinant of change in 6MWD over time.4 McDonald et al. indicated that young males with or without disease may show improvements in 6MWD, presumably because of the increasing stride lengths in association with greater height and strength-to-bodyweight ratios.4 However, starting from around the age of 7 years these gains seem to be eclipsed by disease progression in males with DMD. Males with DMD will then lose stride length despite increasing height.4 Also, BMI seems not to be associated with functional motor outcome in typically developing males or males with DMD aged 4 to 8 years.
This study has some limitations. The estimated reference curves were developed using cross-sectional and not longitudinal data. Subsequently, the group of males with DMD was very heterogeneous, which might have affected the generalizability of the data. Larger collaborative studies, including steroid-naïve males between 4 and 8 years from different sources and natural history studies, could address this limitation and validate the findings of this study. Also, related to the sample size, we acknowledge that the confidence intervals of the lower and upper quantiles that are far from the median, especially of the males with DMD, are large. So, the estimators of these quantiles have to be interpreted with caution. The curves only show the behaviour of functional outcome measures in steroid-naïve males with DMD. Performance of males treated with corticosteroids might deviate from the centiles shown in these curves. However, these data can be used as a reference to describe how far treated males are developing from age-matched steroid-naïve males with DMD, with the caveat that these males, especially the older ones, are a highly select subset given their steroid-naïve status. Reproducing the analyses using longitudinal data from steroid-treated males with DMD, after adjusting for covariates such as steroid regime and age of onset of steroid treatment, could complement the present work and be used as a reference for males with DMD treated with either steroids or novel drugs intended to restore dystrophin. Data on functional outcomes were available for typically developing males from the age of 2 years 6 months, but only from the age of 4 years for those with DMD. The data from the younger typically developing males are helpful for comparing the motor function of males with DMD with that of younger typically developing males, because we know that infants and young males with DMD achieve several motor milestones later than typically developing children. It is also of added value to know how the functional motor outcomes evolve in typically developing children. However, it might also be interesting to include young males with DMD starting from the age of 2 years 6 months in future studies. Another possible limitation is that the typically developing males were evaluated by master's students. Intensive face-to-face training was provided to each master's student before the assessment; moreover, each master's student was supervised by a neuromuscular expert physiotherapist during the evaluation. However, master's students might not have the same level of expertise as specialist neuromuscular physiotherapists. Finally, we did not consider other factors that might affect motor performance in young children (previous medical history, other illnesses, mutation type, environmental factors, cognitive impairment, etc.). However, the FOR-DMD eligibility criteria exclude males with previous significant medical history and severe learning difficulties; and no association between outcome measures and mutation types could be detected in this steroid-naïve population at baseline.35
Despite the limitations, this study has demonstrated significant differences in motor function outcomes between a large cohort of young steroid-naïve males with DMD between 4 and 8 years old and typically developing males. This study is also the first to establish DMD-specific estimated reference curves for the TRF, 10 m walk/run time, 6MWD, and NSAA in a cohort of steroid-naïve males with DMD. The different estimated reference curves can show the functional motor performance of a young male with DMD in relation to typically developing males as well as within the heterogeneous group of males with DMD. These curves can support the consultation with families at the time of diagnosis. They can also aid in decision-making about time to treatment initiation based on assessment of baseline, pre-steroid functional motor performance compared with the expected motor performance in males with DMD. Moreover, the estimated curves can support the evaluation of treatment for reaching motor skills and functional motor outcomes compared with typically developing males.
ACKNOWLEDGEMENTS
We acknowledge all evaluators and physiotherapists for their participation in this study. We especially thank Ann Belmans, from the Leuven Biostatistics and Statistical Bioinformatics Centre (L-Biostat), who contributed to the sample size calculations and the construction of the reference curves. Finally, we thank all parents and children for their participation.
CONFLICT OF INTEREST STATEMENT
The other authors declare no conflicts of interest.
FUNDING INFORMATION
Jasmine Hoskens has received a grant by Duchenne Parent Project, NL and the Stichting Marguerite-Marie Delacroix during the conduct of the study. Marianela Schiava has received a grant by Duchenne UK through Newcastle University. Katrijn Klingels has received a grant by Duchenne Parent Project, NL during the data-acquisition the study.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on reasonable request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.