The cost of respiratory hospitalizations in children with cerebral palsy
Abstract
Aim
To establish the burden of respiratory illness in cerebral palsy (CP) on the Western Australian health care system by quantifying the costs of respiratory hospitalizations in children with CP, compared with non-respiratory hospitalizations.
Method
A 2-year (2014–2015) retrospective study using linked hospital data (excluding emergency department visits), in a population of children with CP in Western Australia aged 18 years and under (median age at hospitalization 7 years; interquartile range 5–12 years).
Results
In 671 individuals (57% male) there were 726 emergency hospitalizations, and 1631 elective hospitalizations. Although there were more elective hospitalizations, emergency hospitalizations were associated with longer stays in hospital, and more days in an intensive care unit, resulting in a higher total cost of emergency hospitalizations than elective hospitalizations (total costs: emergency AU$7 748 718 vs elective AU$6 738 187). ‘Respiratory’ was the leading cause of emergency hospitalizations, contributing to 36% of all emergency admission costs. For a group of high-cost inpatient users (top 5% of individuals with the highest total inpatient costs) the most common reason for hospitalization was ‘respiratory’. Where non-respiratory admissions were complicated by an additional respiratory diagnosis, length of stay was greater.
Interpretation
Respiratory hospitalizations in CP are a significant driver of health care costs. In the paediatric group, they are a burden for a subgroup of children with CP.
What this paper adds
- Respiratory illness is the most costly area for unplanned, emergency hospitalizations for children and young people with cerebral palsy.
- The top 5% of individuals with the highest total inpatient costs account for a disproportionate amount of health care costs.
What this paper adds
- Respiratory illness is the most costly area for unplanned, emergency hospitalizations for children and young people with cerebral palsy.
- The top 5% of individuals with the highest total inpatient costs account for a disproportionate amount of health care costs.
Abbreviations
-
- EOC
-
- episode of care
-
- ICD-10 AM
-
- International Statistical Classification of Diseases and Related Health Problems, 10th Revision Australian Modifications
-
- ICU
-
- intensive care unit
-
- LOS
-
- length of stay
-
- NHCDC
-
- National Hospital Cost Data Collection
-
- WARDA
-
- Western Australian Register of Developmental Anomalies
Cerebral palsy (CP) is one of the most common physical disabilities in childhood, occurring in approximately 1 in 700 live births in Australia.1 It is defined as a motor disability due to a brain injury primarily affecting posture and movement and may be accompanied by sensory, communication, and cognitive impairments.2 Many children with CP have comorbidities, some requiring continuing medical management.3, 4 Comorbidities can be classified as either co-causal (associated with underlying aetiology of the CP), a complication of CP, or co-occurring (along with the CP). Comorbidities (including co-occurring disorders) are more common in children with CP than in the general population.3
Comorbidities, particularly those with progressive consequences, are associated with increased emergency department presentations and hospital admissions.5-7 Children with CP present to hospital with more diagnoses and with longer lengths of stay (LOS) than children without CP.5, 8 Hospital admissions reduce health-related quality of life for the individual and their family and are costly for the health system.9-11 Health resources are often concentrated disproportionately on a small group of high-cost users.12, 13 Children with complex chronic conditions account for a large proportion of readmissions and prolonged LOS, leading to high inpatient costs.9-11, 14 This pattern of high-cost users is likely to be replicated in CP, given its chronicity and frequency of comorbidities. Gaining knowledge of the common reasons for hospital admissions, readmissions, and prolonged LOS is important as it enables health administrators and clinicians to ensure access to timely and appropriate health care that will reduce this burden on individuals and the health system.7, 8
A significant comorbidity (complication) from CP is respiratory disease.3, 5, 6, 15 Complications from respiratory disease are the leading source of premature death in CP, with respiratory failure identified as the cause of approximately 59% of deaths.16 It is a major reason for emergency department presentations and hospital admissions.5-7, 15, 17 Repeated hospitalizations for respiratory illness are common in children with CP, with approximately half readmitted again within 1 year.17 There are several risk factors linked to respiratory hospital admissions, including potentially modifiable factors: oropharyngeal dysfunction, difficulty managing saliva, gastro-oesophageal reflux disease, respiratory symptoms with meals, frequent respiratory symptoms, seizures, and nightly snoring. By identifying which individuals with CP are at risk of respiratory illness and targeting modifiable risk factors, there is an opportunity to reduce admissions and medical costs and improve health-related quality of life through preventive strategies.8, 14
Although respiratory illness is recognized as a common reason for hospitalization in CP, the economic burden for health services is unknown. The aim of this study was to establish the burden of respiratory illness in CP on the Western Australian health care system by quantifying the costs of respiratory admissions in children with CP, compared with non-respiratory admissions. Secondary aims were to establish whether there was a subgroup of health care users contributing disproportionately to hospital costs and to investigate the contribution of respiratory disease to admissions for other (non-respiratory) comorbidities.
METHOD
Study design and population
The population consisted of all people with CP in Western Australia aged 18 years and under who were admitted to hospital in Western Australia over a 2-year period, from 1st January 2014 to 31st December 2015.
Linked data from the Western Australian Register of Developmental Anomalies (WARDA) and the Hospital Morbidity Data System were obtained from the Data Linkage Unit of Western Australia. WARDA is a statutory register that includes the Western Australian CP register with population-based data of all children diagnosed with CP in Western Australia. The Hospital Morbidity Data System is managed by the Western Australian Health System and includes all episodes of care from Western Australian public acute hospitals, Western Australian public psychiatric hospitals, private acute hospitals (licensed by the Western Australian Health System), private psychiatric hospitals (licensed by the Western Australian Health System), and private day surgeries (licensed by the Western Australian Health System). Data linkage was performed using probabilistic linkage using full name, date of birth, and address.
Ethical approval was granted by the Princess Margaret Hospital for Children Ethics Committee, the Department of Health Western Australian Human Research Ethics Committee, and Curtin University Ethics Committee.
Hospitalizations and clinical groupings
Diagnosis codes were grouped according to the International Statistical Classification of Diseases and Related Health Problems, 10th Revision Australian Modifications (ICD-10 AM) codes. Clinical areas were grouped using conventional ICD chapters with J00 to J99 representing respiratory illnesses (Table S1). Hospitalizations for conditions originating in the perinatal period (P00–P96) were excluded as these are not likely to be related to CP and occur before a diagnosis of CP can be made.
For the primary aim the principal ICD-10 code was used to determine the primary reason for the hospitalization. When a patient is admitted to hospital one principal ICD-10 code is assigned, indicating the main reason for admission and representing the start of an episode of care (EOC). An admitted patient completes an EOC by discharge, transfer to another hospital, change of type of care, or death. One admission may involve one EOC, where the patient is admitted and then discharged under the one principal ICD-10 code. However, other admissions consist of multiple EOC where there is an interhospital transfer or a change of type of care (e.g. from acute care to rehabilitation). For this study we report EOC, not admissions, and refer to them as hospitalizations or EOC. Emergency department visits are not captured in this study. Patients may have been seen in the emergency department immediately before admission, but this does not constitute part of an EOC.
To identify those with significant mobility limitations CP severity from the WARDA database, where CP severity is classified as minimal, mild, moderate, or severe and relates to the worst affected limb. Severe CP is described as little purposeful voluntary action, although function may be acquired, IQ permitting.
To address the secondary aim of examining the contribution of respiratory disease to non-respiratory hospitalizations, both principal and additional diagnostic codes were reviewed. Up to 20 additional diagnoses were provided for each EOC. The principal ICD-10 AM code determined the non-respiratory EOC, with additional codes classifying whether the individual was also actively managed in hospital for respiratory reasons. Each EOC was categorized as having (1) only a primary diagnosis (principal non-respiratory ICD-10 AM only, no additional ICD-10 AM codes present), (2) multiple non-respiratory reasons (principal and additional non-respiratory ICD-10 AM codes present), or (3) EOC complicated by respiratory illness (non-respiratory principal ICD-10 AM code combined with additional respiratory diagnoses).
Resource unit and costs
The primary resource unit for this study was LOS with the total bed-days for the 2-year period determined for each clinical area by emergency and elective EOC. An emergency EOC is the admission of a patient for care or treatment which, in the opinion of the treating clinician, is necessary and should occur within 24 hours. An elective EOC can be delayed for at least 24 hours and includes hospitalization from a waiting list. Bed-days were further broken down into same-day, subacute, overnight, and intensive care unit (ICU), as each of these incurs different costs.
Average costs per bed-day for 2014 to 2015 for same-day (AU$2414), subacute (AU$2171), overnight (AU$2554), and ICU (AU$4949) were obtained from the Business Intelligence Unit at Perth Children's Hospital and taken as representative of costs incurred in similar health care settings in Western Australia contemporaneously.
Statistical analysis
Continuous data are presented as medians, interquartile ranges (IQR), and ranges as data were skewed in distribution. To determine the total costs for each clinical area, bed-days for same-day, subacute, overnight, and ICU were aggregated and multiplied by average costs per day for each bed-day type. The clinical areas were then ranked from highest to lowest for LOS and total cost. This was performed separately for elective and emergency EOC, with the 10 most costly clinical areas reported. To establish the robustness of the findings, a sensitivity analysis was conducted using three alternative methods. The first two sensitivity analyses used the same resource units described above but applied to alternative costings. The two data sources were the Royal Children's Hospital for Medicare ineligible patients and the National Hospital Cost Data Collection (NHCDC) report from 2014 to 2015.18, 19 Costs from the Royal Children's Hospital Medicare ineligible patients cost data were available for same-day (AU$1500), overnight (AU$1950), and ICU (AU$4800) bed-days. Royal Children's Hospital Medicare ineligible patients cost data provided no subacute cost, so the overnight cost (AU$1950) was substituted in this analysis. The NHCDC costs were applied using the combined average of a paediatric and adult rate for Western Australia, because detailed costings by bed-day type for paediatrics only (subacute, overnight, same-day) were not available. The NHCDC costs provided no ICU cost; therefore the ICU cost was estimated at three times the average overnight rate.20 The NHCDC costs data were subacute (AU$1313), same-day (AU$1670), overnight (AU$2614), and ICU (AU$7842).18, 19 For the final sensitivity analysis, different resource units were used. Detailed costing information was obtained from the Perth Children's Hospital Business Intelligence Unit where separate costs were provided for emergency and elective EOC by conventional ICD chapters, with EOC classified as same-day, subacute, overnight without an ICU stay, and overnight with an ICU stay. With this alternative costing model, the ICU cost was bundled in with overnight stays and not calculated as a separate ICU cost.
High-cost users were identified using the definition by Calver et al.12 as the top 5% of individuals. For each individual, a total cost for the duration of this study was assigned. The individuals were then ranked from highest to lowest for total inpatient costs, with the top 5% identified as high-cost users. The reasons for EOC in this small group were compiled, along with the number of EOC, LOS, and costs.
For non-respiratory admissions, we examined differences in LOS between overnight EOC (excluding same-day) with and without an additional ICD-10 respiratory code. Information is presented for the top five primary diagnoses with respiratory additional diagnoses, where sample sizes were above n = 5. EOC were classified into three types: (1) EOC with only a principal non-respiratory diagnosis, (2) EOC with multiple non-respiratory diagnoses, and (3) EOC complicated by respiratory illness. Mean (SD) and median (range) are reported and comparisons made between each type of EOC. A negative binomial model was used, producing incidence rate ratios and their corresponding 95% confidence intervals. This model was chosen as the data were overinflated.
Cells with n < 5 were suppressed for confidentiality. Statistical significance level was set at p < 0.05. All statistical analysis was performed using Stata release 16 (StataCorp, College Station, TX, USA).
RESULTS
The cohort consisted of 671 individuals with CP with hospitalizations from 2015 to 2016. There was one individual with two entries in the WARDA database, which did not affect hospitalization data, but did when determining CP severity. For this duplicated entry, one had missing CP severity information, while the other had a recorded value which was therefore assigned to this individual for this study. There were missing data for CP severity for another two individuals.
Fifty-seven per cent of the cohort were male, with 31% having severe CP. The median age at hospitalization was 7 years (IQR 5–12), ranging from birth to 18 years.
There were a total of 2357 EOC, of which 1.4% involved the transfer of an individual to another hospital or a change in type of care. There were 298 individuals with 726 emergency EOC and 588 individuals with 1631 elective EOC (Tables 1 and 2). Although there were more elective EOC, emergency hospitalizations were associated with more bed-days (LOS: emergency 2807 vs elective 2648), with individuals experiencing an emergency EOC staying for longer (mean LOS: emergency 3.9 days vs elective 1.6 days). Same-day EOC made up almost half of elective hospitalizations (47%), but only 5% of all emergency days in hospital. ICU days in hospital were higher for emergency EOC (256 days) than for elective EOC (83 days).
| Clinical area | ICD-10 AM | Individuals | Severe CP | EOC | LOS summary | LOS number | Cost (AU$) | Percentage/rankings | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | n (%) | n | Median (IQR) | Range | Same day | Subacute | Overnight | ICU | Total | Total | LOS (%) | LOS rank | Cost (%) | Cost rank | ||
| Respiratory | J00–J99 | 86 | 59 (68.6) | 182 | 3 (1–5) | 1–154 | 10 | 0 | 889 | 93 | 992 | 2 754 903 | 35.3 | 1 | 35.6 | 1 |
| Nervous system | G00–G99 | 102 | 46 (45.1) | 180 | 1 (1–3) | 1–43 | 58 | 0 | 519 | 67 | 644 | 1 797 121 | 22.9 | 2 | 23.2 | 2 |
| Injury, poisoning | S00–T88 | 50 | 20 (40.0) | 66 | 1 (1–3) | 1–22 | 15 | 0 | 207 | 7 | 229 | 599 531 | 8.2 | 3 | 7.7 | 3 |
| Abnormal findings | R00–R99.99 | 70 | 32 (45.7) | 101 | 1 (1–2) | 11–26 | 19 | 0 | 205 | 0 | 224 | 569 436 | 8.0 | 4 | 7.3 | 4 |
| Congenital | Q00–Q99.9 | 5 | <5 | 5 | 1 (1–21) | 1–52 | 1 | 0 | 2 | 73 | 76 | 368 799 | 2.7 | 8 | 4.8 | 5 |
| Certain infectious and parasitic diseases | A00–A99.99, B00–B99.99 | 42 | 17 (40.4) | 52 | 1 (1–3) | 1–15 | 8 | 0 | 124 | 4 | 136 | 355 804 | 4.8 | 5 | 4.6 | 6 |
| Musculoskeletal | M00–M99.9 | 14 | 7 (50.0) | 18 | 2 (1–4) | 1–61 | 6 | 0 | 98 | 0 | 104 | 264 776 | 3.7 | 6 | 3.4 | 7 |
| Circulatory | I00–I99.0 | 7 | <5 | 7 | 1 (1–21) | 1–55 | 2 | 0 | 79 | 2 | 83 | 216 492 | 3.0 | 7 | 2.8 | 8 |
| Digestive system | K00–K99.9 | 26 | 15 (57.6) | 30 | 2 (1–2) | 1–10 | 5 | 0 | 56 | 6 | 67 | 184 788 | 2.4 | 10 | 2.4 | 9 |
| Urinary | N00–N99.9 | 15 | 6 (40.0) | 29 | 2 (1–3) | 1–8 | 2 | 0 | 70 | 0 | 72 | 183 608 | 2.6 | 9 | 2.4 | 10 |
| All EOC | NA | 298 | 125 (41.9) | 726 | 2 (1–154) | 1–154 | 130 | 40 | 2381 | 256 | 2807 | 7 748 718 | 100 | NA | 100 | NA |
- Abbreviations: CP, cerebral palsy; EOC, episode of care; ICD-10 AM, International Statistical Classification of Diseases and Related Health Problems, 10th Revision Australian Modifications; ICU, intensive care unit; IQR, interquartile range; LOS, length of stay; NA, not applicable.
| Clinical area | ICD-10 AM | Individuals | Severe CP | EOC | LOS summary | LOS number | Cost (AU$) | Percentage/rankings | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | n (%) | n | Median (IQR) | Range | Same day | Subacute | Overnight | ICU | Total | Total | LOS (%) | LOS rank | Cost (%) | Cost rank | ||
| Nervous system | G00–G99 | 397 | 117 (29.5) | 935 | 1 (1–1) | 1–41 | 819 | 0 | 399 | 12 | 1230 | 3 055 500 | 46.5 | 1 | 45.3 | 1 |
| Musculoskeletal | M00–M99.9 | 176 | 70 (39.8) | 217 | 1 (1–2) | 1–20 | 138 | 0 | 306 | 10 | 454 | 1 164 146 | 17.1 | 2 | 17.3 | 2 |
| Factors influencing health status | Z00–Z99.9 | 52 | 28 (53.8) | 71 | 1 (1–2) | 11–23 | 28 | 103 | 47 | 3 | 181 | 426 193 | 6.8 | 3 | 6.3 | 3 |
| Respiratory | J00–J99 | 17 | 6 (35.3) | 22 | 1 (1–9) | 1–28 | 3 | 22 | 54 | 40 | 119 | 390 902 | 4.5 | 5 | 5.8 | 4 |
| Digestive system | K00–K99.9 | 102 | 37 (36.3) | 114 | 1 (1–1) | 1–7 | 102 | 0 | 27 | 1 | 130 | 320 135 | 4.9 | 4 | 4.8 | 5 |
| Congenital | Q00–Q99.9 | 27 | 9 (33.3) | 34 | 1 (1–2) | 1–22 | 14 | 0 | 68 | 9 | 91 | 252 009 | 3.4 | 6 | 3.7 | 6 |
| Abnormal findings | R00–R99.99 | 40 | 16 (40.0) | 49 | 1 (1–1) | 1–14 | 18 | 0 | 70 | 0 | 88 | 222 232 | 3.3 | 7 | 3.3 | 7 |
| Injury, poisoning | S00–T88 | 11 | <5 | 11 | 1 (1–7) | 1–36 | 4 | 0 | 55 | 0 | 59 | 150 126 | 2.2 | 8 | 2.2 | 8 |
| Urinary | N00–N99.9 | 17 | 5 (29.4) | 26 | 1 (1–2) | 1–11 | 8 | 0 | 44 | 1 | 53 | 136 637 | 2.0 | 9 | 2.0 | 9 |
| Ear | H60–H95.9 | 34 | 8 (23.5) | 46 | 1 (1–1) | 1–4 | 42 | 0 | 8 | 2 | 52 | 131 718 | 2.0 | 10 | 2.0 | 10 |
| All EOC | NA | 588 | 178 (30.4) | 1631 | 1 (1–1) | 1–41 | 1256 | 125 | 1184 | 83 | 2648 | 6 738 187 | 100 | NA | 100 | NA |
- Abbreviations: CP, cerebral palsy; EOC, episode of care; ICD-10 AM, International Statistical Classification of Diseases and Related Health Problems, 10th Revision Australian Modifications; ICU, intensive care unit; IQR, interquartile range; LOS, length of stay; NA, not applicable.
Costs for emergency EOC (Table 1) over this 2-year period were estimated at AU$7 748 718 with respiratory the highest cost area. ‘Respiratory’ accounted for 36% of emergency costs, 35% of emergency bed-days, and the highest number of overnight and ICU days. Of the 298 individuals with CP who had an emergency EOC, 82 were admitted for a respiratory reason, of whom 68.6% had severe CP. The ‘nervous system’ was the second highest cost area with 23% of emergency costs, with other clinical areas each contributing 0.1% to 8.2% of the total emergency costs, with 45.1% of those with ‘nervous system’ hospitalizations having severe CP.
Elective EOC costs (Table 2), over this 2-year period, were less than emergency EOC, with an estimated total of AU$6 738 187. The ICD-10 AM principal diagnostic area of ‘nervous system’ was the highest cost area, with 45% of elective costs, 46% of elective days in hospital, and the highest number of same-day and overnight days. There were 819 same-day EOC observed for ‘nervous system’, with 697 (85%) of these consisting of the primary diagnosis of ‘cerebral palsy and other paralytic syndromes’ (G80–G83) combined with a botulinum neurotoxin procedure code. ‘Musculoskeletal’ was the second highest cost area with 17% of elective costs. ‘Respiratory’ had the highest number of ICU days for elective admissions but was only ranked fourth for costs and fifth for LOS.
The results from the sensitivity analysis are shown in Figure 1 and Tables S2 to S5.
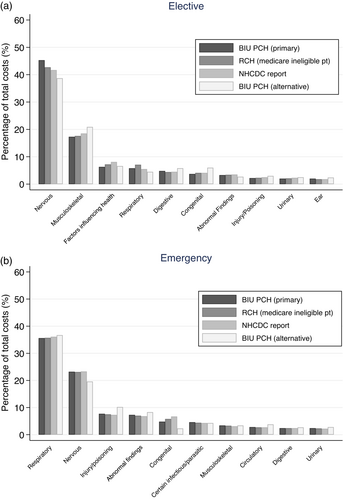
Sensitivity analysis showing the percentage of all costs for the top 10 most costly clinical areas using four different costing models for (a) elective and (b) emergency admissions. Data presented for the primary analysis (BIU PCH) and sensitivity analyses (RCH Medicare ineligible patient, NHCDC report and alternative BIU PCH costings).
Abbreviations: BIU, Business Intelligence Unit; NHCDC, National Hospital Cost Data Collection; PCH, Perth Children's Hospital; pt, patient; RCH, Royal Children's Hospital.
For emergency EOC, the 10 most costly clinical areas remained unchanged, with the top four cost rankings consistent with the primary analysis. ‘Respiratory’ continued to be the leading cause of emergency hospitalizations, accounting for 35.5% to 36.7% of all emergency costs. For elective EOC, the top 10 most costly clinical areas also remained unchanged, with the top three rankings consistent with the primary analysis, and ‘nervous system’ remaining the lead cause of elective EOC. Respiratory hospitalizations ranked fourth among elective EOC for three of the cost models and sixth for the model where ICU admissions were bundled in with hospitalizations with overnight stays.
The 5% of highest cost users (Table 3) consisted of 34 individuals, with 397 EOC (17% of all EOC), 2409 days (48% of all bed-days), at a total cost of AU$6 767 968 (47% of all costs). Of these 34 individuals, 70.6% (n = 24) had severe CP. The most common reason for hospitalization in this group was ‘respiratory’, followed by ‘nervous system’. In this group, ‘respiratory’ contributed to 18% of all costs and 15% of all LOS (830 days), whereas ‘nervous system’ contributed to 12% of all costs and 10% of all LOS (545 days). ‘Respiratory’ and ‘nervous system’ combined in these 34 individuals contributed 30% of all costs for this 2-year period.
| Primary diagnosis | EOC | LOS | Cost | ||||
|---|---|---|---|---|---|---|---|
| Clinical area | ICD-10 AM | n | Percentage of all EOC | n | Percentage of all LOS | Total (AU$) | Percentage of all costs |
| Respiratory | J00–J99 | 91 | 3.9 | 830 | 15.2 | 2 400 791 | 17.9 |
| Nervous system | G00–G99 | 90 | 3.8 | 546 | 10.0 | 1 554 824 | 11.6 |
| Injury, poisoning | S00–T88 | 27 | 1.1 | 181 | 3.3 | 469 179 | 3.5 |
| Musculoskeletal | M00–M99.9 | 24 | 1.0 | 163 | 3.0 | 431 947 | 3.2 |
| Congenital | Q00–Q99.9 | 5 | 0.2 | 78 | 1.4 | 373 907 | 2.8 |
| Abnormal findings | R00–R99.99 | 33 | 1.4 | 122 | 2.2 | 311 448 | 2.3 |
| Factors influencing health status | Z00–Z99.9 | 26 | 1.1 | 133 | 2.4 | 300 848 | 2.2 |
| Circulatory | I00–I99.0 | 5 | 0.2 | 100 | 1.8 | 260 050 | 1.9 |
| Urinary | N00–N99.9 | 32 | 1.4 | 81 | 1.5 | 208 849 | 1.6 |
| Certain infectious and parasitic diseases | A00–A99.99, B00–B99.99 | 22 | 0.9 | 68 | 1.2 | 175 367 | 1.3 |
- Abbreviations: EOC, episode of care; ICD-10 AM, International Statistical Classification of Diseases and Related Health Problems, 10th Revision Australian Modifications; LOS, length of stay.
Table 4 compares the contribution of respiratory disease to admissions for non-respiratory reasons. For overnight stays, clinical areas with only a primary non-respiratory diagnosis had the lowest average LOS, followed by those with a non-respiratory additional diagnosis, with the highest mean LOS observed in EOC with a respiratory additional diagnosis (mean [SD] all diagnoses: 1.8 [1.4] vs 3.7 [5.3] vs 8.4 [9.6] respectively; p < 0.001). The rate of hospitalizations was more than 5 times higher in those with a respiratory additional diagnosis than in those with a primary non-respiratory diagnosis only (incidence rate ratio 5.7, 95% CI 4.6–7.0; p < 0.001). The trend of increasing mean LOS from primary non-respiratory diagnosis only, to additional non-respiratory diagnoses, to those with respiratory diagnosis was consistent across clinical areas. Clinical areas with a respiratory additional diagnosis had statistically significant higher rates of LOS than those with a primary diagnosis only (all p < 0.05), ranging from 5.2 to 7.0 times the LOS.
| Primary diagnosis (ICD-10) | LOS | Non-respiratory additional diagnoses vs primary only | Respiratory additional diagnoses vs primary only | Respiratory additional diagnoses vs non-respiratory additional diagnoses | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| EOC (n) | Total | Median (IQR) | Range | IRR (95% CI) | p | IRR (95% CI) | p | IRR (95% CI) | p | ||
| Nervous system (G00–G99) | Primary diagnosis only | 66 | 108 | 1 (1–2) | 1–8 | ||||||
| Additional diagnoses: non-respiratory | 135 | 559 | 2 (1–5) | 1–43 | 2.5 (1.9–3.4) | <0.001 | 5.5 (3.8–7.9) | <0.001 | 2.2 (1.6–2.9) | <0.001 | |
| Additional diagnoses: respiratory | 37 | 330 | 7 (3–9) | 1–41 | |||||||
| Musculoskeletal (M00–M99.9) | Primary diagnosis only | 10 | 29 | 2 (1–5) | 1–7 | ||||||
| Additional diagnoses: non-respiratory | 73 | 251 | 3 (1–4) | 1–12 | 1.2 (0.7–2.0) | 0.539 | 5.8 (2.9–11.3) | <0.001 | 4.9 (3.0–7.8) | <0.001 | |
| Additional diagnoses: respiratory | 8 | 134 | 11 (7–17) | 2–61 | |||||||
| Injury, poisoning, and external causes (S00–T88) | Primary diagnosis only | 18 | 42 | 1 (1–3) | 1–8 | ||||||
| Additional diagnoses: non-respiratory | 33 | 159 | 2 (1–5) | 1–32 | 1.6 (0.9–2.8) | 0.103 | 6.4 (3.0–13.6) | <0.001 | 4.0 (2.0–7.9) | <0.001 | |
| Additional diagnoses: respiratory | 7 | 104 | 13 (2–22) | 1–36 | |||||||
| Congenital (Q00–Q99.9) | Primary diagnosis only | 5 | 6 | 2 (1–2) | 1–2 | ||||||
| Additional diagnoses: non-respiratory | 16 | 104 | 2 (1–5) | 1–26 | 4.3 (1.0–19.5) | 0.056 | 7.0 (1.1–42.7) | 0.035 | 1.6 (0.4–6.0) | 0.473 | |
| Additional diagnoses: respiratory | 5 | 42 | 10 (1–20) | 1–22 | |||||||
| Urinary (N00–N99.9) | Primary diagnosis only | 5 | 5 | 1 (1–1) | 1–1 | ||||||
| Additional diagnoses: non-respiratory | 34 | 79 | 2 (1–3) | 1–7 | 2.3 (0.9–6.0) | 0.083 | 5.2 (1.9–14.3) | 0.002 | 2.2 (1.3–3.7) | 0.002 | |
| Additional diagnoses: respiratory | 6 | 31 | 5 (1–8) | 1–11 | |||||||
| All primary diagnoses combined (excluding respiratory) | Primary diagnosis only | 168 | 294 | 1 (1–2) | 1–8 | ||||||
| Additional diagnoses: non-respiratory | 520 | 1903 | 2 (1–4) | 1–55 | 2.0 (1.7–2.4) | <0.001 | 5.7 (4.6–7.0) | <0.001 | 2.8 (2.4–3.3) | <0.001 | |
| Additional diagnoses: respiratory | 92 | 774 | 6 (1–10) | 1–61 | |||||||
- Abbreviations: CI, confidence interval; EOC, episode of care; ICD-10, International Classification of Diseases; IQR, interquartile range; IRR, incidence rate ratio; LOS, length of stay.
DISCUSSION
Although CP is not a respiratory condition, the leading cause of emergency hospitalization among this group was due to respiratory illness. ‘Nervous system’ was the second most common reason for emergency hospitalizations, with a similar number of episodes of care compared with emergency respiratory hospitalizations; however, individuals with respiratory hospitalizations tended to stay longer in hospital, leading to higher costs. In emergency hospitalizations, those with respiratory diagnoses had the highest number of days in hospital, accounting for 36% of all emergency admission costs. This relatively small group (n = 86) of individuals, many of whom had severe CP, had the highest number of days in ICU, further driving up costs.
‘Nervous system’ was the most common and costly reason for elective EOC, with a large proportion of same-day presentations for botulinum neurotoxin procedures. The second most common reason for elective admission was ‘musculoskeletal’. Admissions for botulinum neurotoxin and musculoskeletal procedures are not unexpected in children with CP as these are planned proactively to improve function and prevent complications, with evidence of their efficacy.21 This differs from respiratory admissions, which are frequently non-elective and reactive, and therefore lacking coordinated management.5-7, 17, 22, 23 Srivastava et al.24 reported that children with medical complexity have fragmented, uncoordinated, and crisis-driven care, aligning with the findings of a recent audit reporting that CP respiratory admissions often lack certainty about the specific diagnosis, which can lead to costly and inefficient management.25
Within this cohort, 34 individuals (5% highest cost users), of whom 71% had severe CP, accounted for almost half of both LOS and total (emergency plus elective) costs, with respiratory diagnoses being the most common reason for admission. Our findings are consistent with other studies where a relatively small number of individuals can have a large impact on overall expenditure.13, 26 Given the significant costs associated with a small group of individuals, there are opportunities to reduce health care costs through targeted, coordinated care, and consistent management.7, 8, 11, 14, 25, 27, 28
Non-respiratory admissions were complicated by respiratory disease, with admissions associated with an additional respiratory diagnosis associated with consistently longer LOS. It is unknown whether individuals were admitted with respiratory symptoms, developed a hospital acquired infection, had an exacerbation of their respiratory disease, or aspirated while inpatients. Regardless of the primary reason for presentation, proactive respiratory support for children with CP during all inpatient stays, especially those with known CP respiratory risk factors, should become routine care.27
This study focused on costs to health services, but hospitalization is also costly for patients and families, both monetarily and through reduced quality of life, especially unplanned hospital stays. During paediatric hospitalizations, families commonly participate in providing the routine care for their child, while managing work and family commitments. There are increased personal expenses, with parents incurring travel and meal costs in addition to loss of income.11, 29 Avoiding hospitalizations and reducing LOS would reduce health care costs, the cost to families, and improve the lives of individuals with CP.8-11
It has been argued that reducing LOS has limited cost-saving potential for health services, as a high proportion of costs are both fixed and accrued in the first days of admission. Although some costs are fixed, managing respiratory conditions, such as pneumonias, is particularly resource intensive.30 Respiratory admissions can involve costly interventions such as mechanical ventilation and expensive laboratory and consumable items.31 Reducing respiratory admissions and LOS would allow the reinvestment of precious health resources elsewhere.30
Recently a consensus statement for preventing and managing respiratory disease in children with CP was developed, encouraging a proactive approach with early identification of respiratory risk factors, continuing surveillance, and multidisciplinary management.32 Given these findings, implementing respiratory management in hospital and community settings for high-risk individuals is supported by the present study. Coordinated care in any setting, especially for those with respiratory risk factors, will have a positive impact on health care costs and families.
A strength of this study is the use of a population-based database of individuals with CP to link CP diagnosis to hospital admission data. Studies relying on ICD codes to identify children with CP fail to capture those children with CP not assigned a CP code.8 Among the limitations are using LOS as the resource unit to calculate costs. This does not account for resources such as medications, emergency department costs, surgery, and ventilation. The primary aim of our study depended on the principal diagnosis. However, children are often hospitalized with multiple diagnoses, and determining the principal diagnosis is difficult in complex admissions.8 Diagnostic coding is also prone to errors, and codes may be assigned to areas of high reimbursement in preference to codes with lesser reimbursement.33
CONCLUSION
Respiratory hospitalizations in CP are a significant driver of health care costs. In the paediatric age group, they are a burden for a subgroup of children with CP. In accordance with the consensus statement for preventing and managing respiratory disease, children with CP require respiratory surveillance and management of risk factors. Respiratory review should become routine with coordinated, evidence-based multidisciplinary management to reduce respiratory hospitalization.
ACKNOWLEDGMENTS
We thank the staff at the Western Australia Data Linkage Branch, the Hospital Morbidity Data Collection, and Western Australia Register of Developmental Anomalies. We also thank the Business Intelligence Unit at Perth Children's Hospital for providing costings data. Open access publishing facilitated by Curtin University, as part of the Wiley - Curtin University agreement via the Council of Australian University Librarians.
FUNDING INFORMATION
The Perth Children's Hospital Foundation and the Cerebral Palsy Alliance.
CONFLICT OF INTEREST STATEMENT
The authors have stated that they had no interests that might be perceived as posing a conflict or bias.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.