Fatigue-related gait adaptations in children with cerebral palsy
Abstract
Aim
To obtain insights into the effects of fatigue on the kinematics, kinetics, and energy cost of walking (ECoW) in children with cerebral palsy (CP).
Method
In this prospective observational study, 12 children with CP (mean age 12 years 9 months, SD 2 years 7 months; four females, eight males) and 15 typically developing children (mean age 10 years 8 months, SD 2 years 4 months; seven females, eight males) followed a prolonged intensity-based walking protocol on an instrumented treadmill, combined with gas analysis measurements. The protocol consisted of consecutive stages, including a 6-minute walking exercise (6MW) at comfortable speed, 2 minutes of moderate-intensity walking (MIW) (with a heart rate > 70% of its predicted maximal), and 4 minutes walking after MIW. If necessary, the speed and slope were incremented to reach MIW. Outcomes were evaluated at the beginning and end of the 6MW and after MIW.
Results
With prolonged walking, Gait Profile Scores deteriorated slightly for both groups (p < 0.01). Knee flexion increased during early stance (p = 0.004) and ankle dorsiflexion increased during late stance (p = 0.034) in children with CP only. Negligible effects were found for kinetics. No demonstrable change in ECoW was found in either group (p = 0.195).
Interpretation
Kinematic deviations in children with CP are progressive with prolonged walking. The large variation in adaptations indicates that an individual approach is recommended to investigate the effects of physical fatigue on gait in clinical practice.
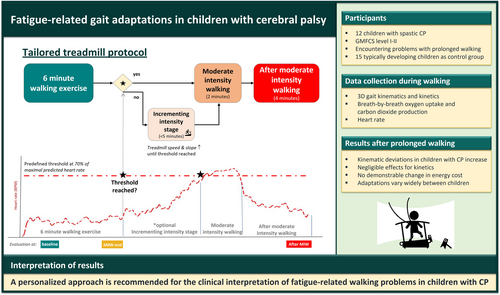
Graphical Abstract
Abbreviations
-
- 6MW
-
- 6-minute walking exercise
-
- ECoW
-
- energy cost of walking
-
- GPS
-
- Gait Profile Score
-
- MIW
-
- moderate-intensity walking
-
- RER
-
- respiratory exchange ratio
-
- RMSE
-
- root mean square error
What this paper adds
- A tailored intensity-based protocol allows the study of fatigue-related gait adaptations.
- Kinematic gait deviations in children with cerebral palsy increase with prolonged walking.
- Kinematic changes with prolonged walking vary widely between children.
Children with cerebral palsy (CP) encounter activity limitations attributed to a non-progressive injury of the fetal or infant brain.1 As the combined result of impaired selective motor control, contractures, spasticity, bony deformities, and muscle weakness, CP can cause deviations in gait pattern and related walking problems, such as diminished walking distance and walking speed.1, 2 Even at diminished speed, many children with CP walk at an intensity exceeding their ventilatory threshold,2 and the energy expenditure per distance travelled of children with CP can be threefold greater than the energy cost of walking (ECoW) reported in typically developing children.3 Consequently, many children with CP have difficulties keeping up with typically developing peers. Walking-induced physical fatigue is frequently reported,4-6 restricting activities of daily living and participation.4-6
Physical fatigue refers to a suboptimal condition caused by physical exertion.6 This results in loss of performance and increased effort of an individual to function at the desired level.6, 7 Factors related to loss of performance while walking are commonly quantified by assessing decline in muscle force production and coordination or an increase in ECoW.6 Yet, the effects of walking-induced fatigue on gait adaptations in children with CP are not fully understood. Recent studies in children with CP reported changes of the gait pattern towards more knee flexion during the early stance phase accompanied by signs of muscle fatigue after a 6-minute walking exercise (6MW) in children who walk in a crouched8, 9 or jump gait pattern.10 This supports the idea that gait deviations progress with prolonged walking because of physical fatigue. Moreover, because minimization of ECoW is an important criterion for gait pattern optimization,11 the results of these studies raise the question whether gait pattern changes that occur after prolonged walking would also result in a further increase in ECoW in children with CP. Such an increase in ECoW could result in a vicious circle, leading to further progression of initial gait problems and further increased ECoW after prolonged walking.
To quantify the effects of walking-induced fatigue in individual children, appropriate choices with regard to the measurement protocol and outcome measures are critical.6 Performance decline is expected to occur first in the part of the body that is most heavily loaded during walking, which is dependent on the baseline gait pattern.12 Hence, it is uncertain whether alterations towards increased knee flexion as previously described in CP8 will also occur in children walking who walk with other gait patterns. Moreover, fatigue onset is also likely to be dependent on the experienced intensity of walking (i.e. a child's level of energy consumption) and on motor skills.1, 3, 12 Therefore, to investigate the effects of walking-induced fatigue in a heterogeneous group of children with CP with different impairment severities and gait patterns, standardization of the test protocol to measure the consequences of walking-induced fatigue should be based on how long a child exceeds a certain intensity level, rather than on the duration of the walking exercise. In this context, a tailored intensity-based protocol could be helpful because it controls for individual differences in baseline gait pattern, ECoW, and motor skills.
The aim of the present study was to investigate the effect of prolonged walking on Gait Profile Scores (GPS), gait kinematics, gait kinetics, and ECoW in children with CP with a variety of baseline gait patterns. To this end, a tailored protocol was developed in which a moderate-intensity (greater than the ventilatory threshold) exercise was set, creating circumstances previously associated with the development of walking-induced fatigue in CP.13 We hypothesized that prolonged moderate-intensity walking (MIW) would result in exaggerated gait deviations in children with CP but not in typically developing children. Moreover, we hypothesized that gait deterioration would be accompanied by a further increase in ECoW in children with CP compared to typically developing children after MIW.
METHOD
Participants
Children with CP were referred for clinical gait analysis at the outpatient rehabilitation department by their physician as part of clinical care between August 2019 and October 2021, with a treatment question related to walking-induced fatigue. The following inclusion criteria were used: age between 6 and 18 years; able to understand and follow verbal instructions; and able to walk independently without devices (e.g. orthoses, walker, cane) for at least 10 minutes. As a control group, 15 typically developing children were recruited via personal communication, including the children of colleagues, family, and acquaintances. For typically developing children, the exclusion criterion was a medical background that could affect walking performance. All parents, and children aged 12 years and older, provided written informed consent before study enrolment. The study was approved by the local medical ethics committee of the Vrije Universiteit University Medical Center Amsterdam and the local ethics committee of Vrije Universiteit Amsterdam, the Netherlands.
Study design
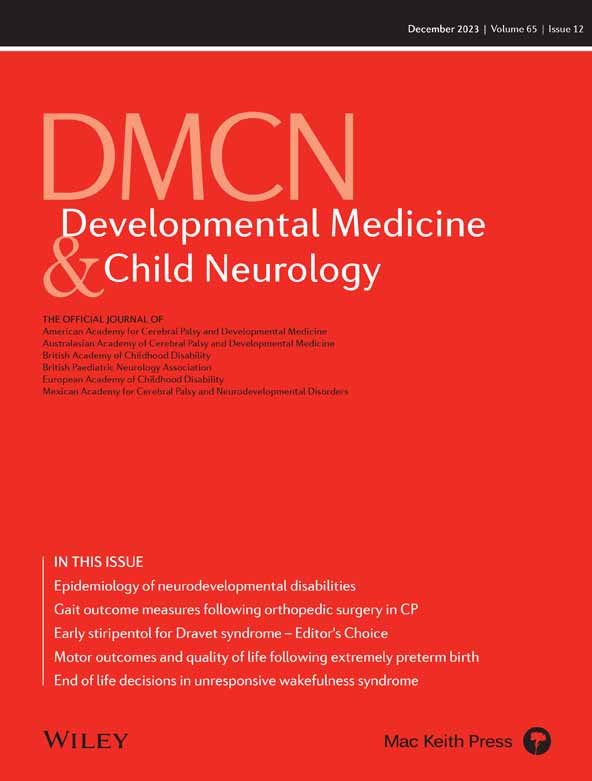
A schematic overview of the prolonged intensity-based walking protocol is presented in Figure 1. The protocol was performed on a split-belt instrumented treadmill that was placed in a speed-matched virtual environment projected on a 180-degree semi-cylindrical screen (Gait Real-time Analysis Interactive Lab system, Motek Medical, Houten, the Netherlands).
Before the start of the measurements, all participants performed a practice session on the treadmill (10 minutes) without any measurement equipment to familiarize themselves to treadmill walking. After this, a resting test was performed, during which children quietly sat down for 5 minutes while their oxygen uptake was measured. This was followed by an overground 6MW on an oval track at a self-selected comfortable walking speed conducted as part of clinical care. This overground speed, which was timed per round and averaged over 6 minutes, was then set on the treadmill. The overground walking exercise was followed by a preparation phase (>30 minutes) during which the measurement equipment was prepared and markers were attached to the skin while children recovered from the previous walking test. Thereafter, children performed the intensity-based walking protocol on the treadmill. This protocol was used as a proxy for a real-life situation in children with CP, with an exercise intensity severe enough to provoke signs of fatigue by walking at an intensity above the ventilatory threshold. Children were asked to walk in the middle of the treadmill on their own shoes without the aid of orthoses or assistive devices.
The prolonged walking protocol consisted of three or four consecutive stages, including a 6MW, with an optional increased-intensity stage, MIW, and after-MIW stage. During the 6MW, participants walked on the treadmill for 6 minutes at a constant speed, which was their overground comfortable walking speed from the previous test, and a slope of 0 degrees. Then, we determined whether their heart rate exceeded the predefined threshold for MIW, defined as 70% of the predicted maximal heart rate as an estimation of ventilatory threshold.13, 14 The predicted maximal heart rate in children was assumed to be 195 bpm and to be the same for children with CP and typically developing children.13 If the threshold for MIW was not reached during the 6MW, the speed and slope of the treadmill were increased in an additional stage, using block-wise steps as used in the Fitkids Treadmill Test.15 For all children, the threshold should have been reached within 5 minutes. When the threshold was reached, participants walked for 2 minutes at this MIW. Finally, the treadmill slope and speed were returned to the original 6MW settings for the final 4 minutes (after MIW). When the threshold had already been reached during the 6MW, no changes were made to the treadmill slope or speed and 2 minutes of MIW and the after-MIW stage followed immediately after the 6MW. At the end of the 6MW and after the MIW, the rate of perceived exertion was scored using an OMNI scale (range: 0–10).16
Data collection and analysis
Three-dimensional motion data were captured using passive retroreflective markers and infrared cameras (Vicon, Oxford, UK) to assess joint angles (kinematics), combined with the ground reaction forces measured from the embedded force plates in the treadmill to calculate joint moments and power (kinetics). Breath-by-breath oxygen uptake (VO2) and carbon dioxide production (VCO2) values were collected with a portable gas analysis system (K5, Cosmed, Rome, Italy) combined with a chest heart rate monitor (Garmin, Olathe, KS, USA). Children were asked not to eat or drink (except for water) for at least 90 minutes before the start of the test.
Kinematic and kinetic data were processed using the Gait Offline Analysis Tool v4.2 (Motek Medical, Houten, the Netherlands) and custom MATLAB scripts (MathWorks, Natick, MA, USA), according to the updated version of the human body model.17, 18 For children with CP, strides were evaluated for the most affected leg, while for typically developing children strides were evaluated for a leg selected randomly. Strides were excluded when kinematics exceeded 3SD from a child's mean, to remove excessive outliers in case of tripping, children who stood still or poor data quality. For the kinetic analyses, clean force plate strikes were selected based on visual inspection. Spatiotemporal parameters, and maximum and minimum outcomes for kinematic and kinetic gait parameters, were averaged over the second minute of the 6MW (baseline), the final minute of the 6MW (6MW end), and the final minute after the MIW. In cases where the number of valid kinetic strides was fewer than five, this time span was extended to 90 seconds or until at least five clean strides were included. To assess the deviations of kinematic curves, the root mean square error (RMSE) over all points of the time-normalized curves was calculated with regard to an independent set of reference data from typically developing children.19 Subsequently, the RMSE values representing different joints and planes were averaged to calculate the GPS,20 which is a commonly used outcome measure to measure gait quality,20 with higher values indicating larger gait deviations from the reference.
Breath-by-breath data were interpolated to a 1-Hz time base and filtered using a moving-average filter (10 seconds). Data were then averaged over 1-minute steady-state walking, between the second and third minute of the 6MW (baseline), the final minute of the 6MW (6MW end), and the final minute after the MIW. The criteria for steady state were: minimal change in VO2 (slope of the linear curve fit <0.00025 mL/kg/second);21 fluctuations in VO2, VCO2, and a ventilatory equivalent of 10% or less of the mean; and respiratory exchange ratio (RER) less than 1.0. Using the mean steady state VO2 and RER, gross energy consumption (J/kg/minute) was calculated according to the following formula: (4.940 × RER + 16.040) × VO2. Gross ECoW (J/kg/minute) was calculated as gross energy consumption divided by speed.22
Statistical analysis
Differences in age and anthropometric characteristics between groups (children with CP vs typically developing children) were analysed with independent-sample t-tests. For gait outcomes, differences between groups (children with CP vs typically developing children), evaluation phases (baseline, 6MW end, after MIW), as well as interactions (group × evaluation phase) were analysed with a repeated-measures analysis of variance (ANOVA) (SPSS v26, IBM Corp., Armonk, NY, USA). Additionally, for the kinematic and kinetic curves, a statistical parametric mapping repeated-measures ANOVA was performed in MATLAB. If data for a participant were missing due to measurement errors, said participant was left out of the analysis for the affected outcome measure. Significance level was set at p < 0.05. For all statistical analyses, we checked if data were normally distributed. If the assumptions of sphericity were violated, a Huyn–Feldt (ε > 0.75) or Greenhouse–Geisser (ε < 0.75) correction was used. The results of the post hoc tests were Bonferroni-corrected to account for multiple comparisons.
RESULTS
Twelve children with bilateral (n = 10) or unilateral (n = 2) spastic CP (Gross Motor Function Classification System levels I [n = 3] and II [n = 9]; mean age 12 years 9 months, SD 2 years 7 months; four females, eight males), and 15 typically developing children (mean age 10 years 8 months, SD 2 years 4 months; seven females, eight males) participated. The detailed characteristics of participants are presented in Table 1. Relevant clinical information of children with CP, such as diagnosis and Gross Motor Function Classification System level, was provided by the referring physician. The baseline gait patterns in the group with CP ranged from children walking with excessive knee flexion and ankle dorsiflexion throughout the stance phase, to children walking with ankle plantar flexion and excessively extended knees, with other gait patterns in between. To address this range of gait patterns, lines of individual gait curves are shown in Figure 2; two typical examples are presented in Appendix S1. Because not all the data of the kinematic and kinetic waveforms were normally distributed, statistical non-parametric mapping was used for the gait curve outcomes; this method is based on permutation tests.
| Typically developing children | Children with CP | p | |
|---|---|---|---|
| Sex, n | 7 females, 8 males | 4 females, 8 males | – |
| Age, years:months | 10:8 (2:4) | 12:9 (2:7) | 0.04 |
| Height, cm | 146.8 (15.0) | 158.8 (19.0) | 0.08 |
| Weight, kg | 38.8 (11.4) | 47.3 (18.9) | 0.16 |
| Treadmill speed, m/second | 1.17 (0.18) | 1.01 (0.24) | 0.05 |
| Distribution of CP, n | NA | Bilateral: 10, unilateral: 2 | – |
| GMFCS level, n | NA | I: 3; II: 9 | – |
| Incrementing intensity stage applied, n | Yes: 15 | Yes: 7 | – |
| Δ Slope, degrees | 2.6 (1.1) | 1.6 (1.12) | – |
| Δ Speed, m/second | 0.54 (0.76) | 0.1 (0.12) | – |
- Group results are presented as the mean (SD). Gait pattern classification was based on sagittal knee angles during the stance phase. Note that statistical tests were performed to assess group differences in sex, or speed and slope incrementation during the exercise protocol.
- Abbreviations: Δ, difference; CP, cerebral palsy; GMFCS, Gross Motor Function Classification System; NA, not applicable.
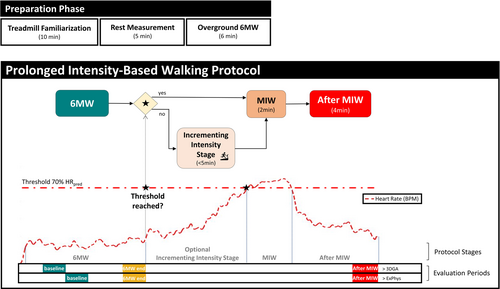
Group median joint kinematic curves before and after prolonged moderate-intensity walking (MIW) in children with cerebral palsy (CP) and typically developing (TD) peers. The curves represent averaged kinematics for the second minute of a 6-minute walking exercise (6MW) (baseline), the final minute of a 6MW (6MW end), and the final minute at the end of the MIW protocol (after MIW). The shaded curves in the background represent the individual curves of children with CP. The vertical bars represent the difference in root mean square error (ΔRMSE) between baseline and after MIW for both groups compared to independent reference data. For RMSE, positive values indicate development further away from the reference data after MIW or increased deviations. Abbreviations: abd, abduction; add, adduction; ant, anterior; dflx, dorsiflexion; endo, endorotation; exo, exorotation; ext, extension; flex, flexion; plfx, plantar flexion; post, posterior; protr, protracted; retr, retracted; SNPM, statistical non-parametric mapping.
All typically developing children required an optional incrementing-intensity stage to reach MIW, whereas this applied to only 6 of 12 children with CP. One child with CP was not able to complete the whole protocol. Because the heart rate of this child was more than 150 bpm throughout the 6MW, the data from the 6MW end was used as the after-MIW also. In another child with CP, the heart rate belt did not function. For this participant, the protocol was applied based on perceived exertion (OMNI scale), which correlates highly with heart rate,23 and continued until the child and parents confirmed complaints that were representative of walking longer distances. Increased OMNI scores with prolonged walking (p < 0.001) confirmed that both groups perceived greater exertion at successive evaluation phases (Table 2, p < 0.001), but no group difference was found (p = 0.358).
| Baseline | 6MW end | After MIW | Statistics | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | Phase | Interaction | |||||||||||
| Typically developing children | Children with CP | Typically developing children | Children with CP | Typically developing children | Children with CP | p | η 2 | p | η 2 | p | η 2 | Post hoc CP | |
| Stride length, m | 1.2 (0.20) | 1.09 (0.24) | 1.22 (0.20) | 1.10 (0.26) | 1.23 (0.19) | 1.12 (0.26) | 0.202 | 0.064 | <0.001 | 0.398 | 0.296 | 0.047 | AC, ABC |
| Step width, cm | 9.2 (1.9) | 14.3 (4.6) | 9.5 (3.0) | 14.0 (3.7) | 8.9 (2.4) | 12.1 (4.1) | <0.001 | 0.359 | 0.062 | 0.105 | 0.433 | 0.033 | |
| GPS | 6.0 (1.0) | 10.9 (3.2) | 6.1 (1.11) | 11.2 (3.4) | 6.2 (1.2) | 11.7 (3.4) | <0.001 | 0.540 | <0.005 | 0.298 | 0.087 | 0.104 | ABC |
| RMSE sagittal hip angles | 6.9 (2.0) | 10.0 (5.9) | 7.1 (1.9) | 10.3 (5.9) | 7.4 (2.1) | 11.0 (5.7) | 0.049 | 0.146 | 0.012 | 0.203 | 0.438 | 0.027 | |
| RMSE sagittal knee angles | 5.8 (1.5) | 15.3 (7.6) | 5.9 (1.4) | 15.4 (7.6) | 6.1 (1.8) | 15.8 (8.0) | <0.0001 | 0.479 | 0.050 | 0.129 | 0.528 | 0.021 | |
| RMSE sagittal ankle angles | 5.6 (2.7) | 8.6 (3.9) | 5.6 (2.5) | 9.4 (4.8) | 5.8 (2.3) | 9.7 (5.1) | 0.017 | 0.207 | 0.005 | 0.223 | 0.058 | 0.119 | ABC |
| Ankle (stance) | |||||||||||||
| Peak dorsiflexion, degrees | 13.1 (3.4) | 17.3 (8.7) | 13.2 (3.5) | 18.4 (9.6) | 13.6 (3.5) | 19.2 (9.8) | 0.084 | 0.115 | <0.001 | 0.358 | 0.044 | 0.129 | AB, AC, ABC |
| Peak moment, Nm/kg | 1.39 (0.19) | 1.18 (0.20) | 1.41 (0.18) | 1.18 (0.22) | 1.41 (0.20) | 1.18 (0.20) | 0.033 | 0.182 | 0.697 | 0.016 | 0.626 | 0.020 | |
| Peak power, W/kg | 2.2 (0.7) | 1.3 (0.6) | 2.3 (0.7) | 1.4 (0.8) | 2.3 (0.7) | 1.2 (0.5) | <0.005 | 0.308 | 0.330 | 0.046 | 0.420 | 0.036 | |
| Knee (stance) | |||||||||||||
| Peak flexion, degree | 19.9 (4.2) | 34.9 (11.3) | 20.2 (4.6) | 35.5 (11.4) | 20.2 (5.1) | 36.9 (11.5) | <0.001 | 0.423 | 0.002 | 0.226 | 0.012 | 0.190 | AB, BC, AC |
| Peak moment, Nm/kg | 0.39 (0.13) | 0.66 (0.34) | 0.40 (0.16) | 0.67 (0.32) | 0.39 (0.13) | 0.70 (0.33) | 0.020 | 0.213 | 0.722 | 0.014 | 0.499 | 0.030 | |
| RPE (OMNI 1–9) | – | – | 2.9 (2.2) | 3.5 (2.1) | 4.4 (2.7) | 5.5 (2.7) | 0.358 | 0.028 | <0.001 | 0.382 | 0.401 | 0.001 | BC |
| Heart rate, bpm | 107 (10) | 136 (22) | 108 (9) | 140 (21) | 117 (9) | 141 (21) | 0.012 | 0.354 | <0.001 | 0.840 | 0.057 | 0.174 | AC, BC, ABC |
| ECoW, J/kg/minute | 6.0 (1.1) | 9.9 (3.8) | 5.9 (1.8) | 9.6 (3.8) | 6.3 (1.3) | 9.7 (3.8) | 0.024 | 0.267 | 0.195 | 0.092 | 0.652 | 0.025 | |
| ECS, J/kg/minute | 439 (66) | 528 (151) | 423 (55) | 513 (133) | 453 (71) | 520 (138) | 0.141 | 0.123 | 0.098 | 0.127 | 0.586 | 0.031 | |
| RER | 0.74 (0.06) | 0.86 (0.07) | 0.79 (0.06) | 0.88 (0.06) | 0.82 (0.07) | 0.89 (0.07) | 0.005 | 0.385 | <0.001 | 0.598 | 0.250 | 0.079 | AB, AC, ABC |
| Walking speed, m/second | 1.17 (0.18) | 1.01 (0.24) | a | a | a | a | 0.049 | 0.383 | – | – | – | – | – |
- Results are presented as the group mean (SD). Joint moments refer to the peak internal ankle plantar flexion and knee extension moments. Peak ankle moments and power were calculated during the second half of the stance phase. Walking speed was constant for the evaluation phases. p < 0.05 was statistically significant. Effect sizes are presented as partial η2. Inter: interaction effect group × evaluation phase. Post hoc: significant post hoc effect (tested only for children with CP) between evaluation phases respectively: AB, difference between baseline and 6MW end; BC, difference between 6MW end and after MIW; AC, difference between baseline and after MIW; ABC, main effect over all phases. RMSE was averaged over the time points of time-normalized gait cycles.
- a Walking speed is identical for the evaluation phases, as speed was kept constant.
- Abbreviations: 6MW; 6-minute walking exercise; bpm, beats per minute; ECoW, energy cost of walking; ECS, energy consumption; GPS, Gait Profile Score; MIW; moderate-intensity walking; RER, respiratory exchange ratio; RMSE, root mean square error; RPE, rate of perceived exertion.
The GPS and RMSE of individual joint curves increased slightly with prolonged walking in both groups (mean difference GPS between baseline and after MIW: children with CP = 0.8 vs typically developing children = 0.2 degrees), indicating a change further away from the reference data, although no interaction effects were found (Table 2). In three children with CP, the increase in GPS exceeded the minimal clinically important difference of 1.6 degrees.24 For children with CP, large individual differences were observed concerning baseline gait patterns (Figures 2 and 3) and gait alterations after prolonged walking. The results of two typical examples can be found in Appendix S1.
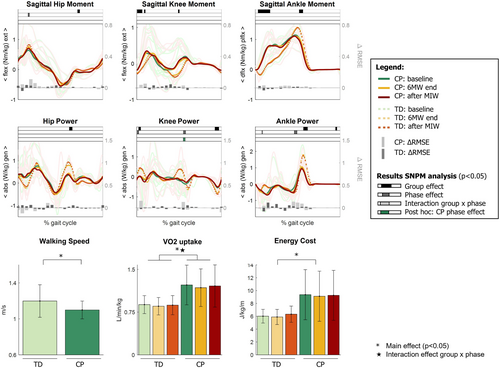
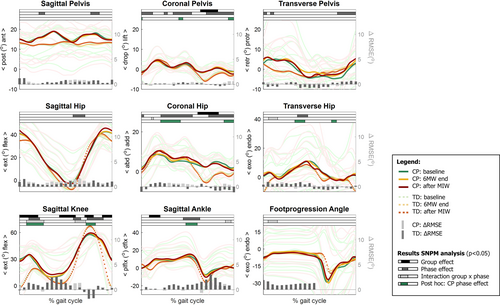
Group median kinetic gait curves before and after prolonged moderate-intensity walking (MIW) in children with cerebral palsy (CP) and typically developing (TD) peers. The shaded curves in the background represent the individual curves of children with CP. The vertical bars represent the difference in root mean square error (ΔRMSE) between the baseline and after MIW, with positive values indicating increased deviations from the reference data. Top: internal sagittal joint moments. Middle: joint power. Bottom: walking speed, oxygen consumption, and energy cost of walking. Walking speed was fixed between evaluation phases. The significant effects (p < 0.05) for the bottom row are indicated with a single asterisk for group effect and a star symbol for the evaluation phases. Abbreviations: abs, power absorption; dflx, dorsiflexion; ext, extension; flex, flexion; gen, power generation; plfx, plantar flexion; SNPM, statistical non-parametric mapping.
For the kinematic curves, multiple group differences and several systematic pattern changes occurred with prolonged walking (Figure 2). Among others, for the sagittal knee angle, a significant interaction effect between evaluation phase and group was found at 60% to 71% of the gait cycle (p < 0.001), with post hoc tests indicating increased knee flexion in children with CP between baseline and after MIW at 8% to 26% of the gait cycle (p = 0.002) and at 72% to 82% of the gait cycle (p = 0.016). Furthermore, increased hip adduction was found with prolonged walking in both groups, with post hoc tests indicating significant changes in children with CP at 20% to 42% of the gait cycle (p = 0.018) and 89% to 100% of the gait cycle (p = 0.010). Finally, a small increase in dorsiflexion was found during the late stance (48%–60% of the gait cycle, p = 0.002) for children with CP.
Kinetic results are based on 24 children (children with CP, n = 12; typically developing children, n = 12) because clean force plate foot strikes were not always available in typically developing children. Statistical non-parametric mapping analysis indicated main group effects for sagittal knee and ankle moments during the early stance and ankle power generation around push-off; however, the effects between evaluation phases were negligible (Figure 3). Likewise, analysis of discrete values revealed smaller peak internal plantar flexion moments and ankle power in children with CP than in typically developing children, while peak internal knee extensor moments were larger in children with CP (Table 2). No effects of the evaluation phases or interaction effects were found (Table 2).
ECoW was established for 21 children (children with CP, n = 10; typically developing children, n = 11). Data for some children were excluded because there was a low ventilation flow (<15 L/minute, typically developing children, n = 2) or suspected mask leakage (children with CP, n = 1). In three other children, no reliable steady state was reached (children with CP, n = 1; typically developing children, n = 2). Finally, one child with CP did not meet the criteria for steady state in the third minute of the 6MW; therefore, the fourth minute was used as the baseline for this child. Main group effects were found, indicating increased ECoW in children with CP compared to typically developing children (Table 2), as well as increased heart rate and RER. Although an increase in heart rate and RER with evaluation phases for both groups (both p < 0.001) was found, no differences were observed for ECoW and no interaction effects were found (Table 2).
DISCUSSION
This study was conducted to obtain an insight into the effects of walking-induced fatigue on gait kinematics and kinetics and ECoW in children with CP. To this end, a tailored prolonged intensity-based treadmill protocol was used to ensure moderate intensity during walking. This protocol resulted in progression of deviations in gait pattern in children with CP with prolonged walking; kinetics and ECoW were not demonstrably affected.
We included a heterogeneous group of participants with CP, considering their baseline gait pattern, unilateral or bilateral involvement, and ECoW level. From the individual gait curves in participants with CP (Figure 2), we observed that variation between participants ranged from excessive knee extension in mid-stance in some children to continuous knee flexion in others. Likewise, the angle of foot progression and hip endorotation and exorotation varied by more than 40 degrees between participants. In line with our hypothesis, these large interindividual differences were also translated to many observed gait adaptations with prolonged walking. Hence, the number of systematic pattern changes in the statistical parametric mapping analysis was relatively small as this variation was lost when averaging the curves.19 Because of the small sample size, it was not possible to investigate whether adaptations were related to predefined gait patterns, although this would be an interesting step for future studies. Nevertheless, in our current study, the GPS and RMSE of individual joints increased slightly (approximately 1 degree) with prolonged walking (Table 2). This indicates that although individual adaptations in gait patterns occurred in sometimes opposite directions and contrasting phases of the gait cycle, these changes were systematically further away from the reference curves. While the average change was below the minimal clinically important difference for GPS and therefore not likely to result in worse scores on functional motor scales,24 it supports our hypothesis of increasing gait deviations with prolonged walking.
Compared to typically developing children, increased knee flexion in early stance and increased ankle dorsiflexion in late stance were found in children with CP with prolonged walking (Figure 2 and Table 2), which is in line with earlier studies in children with CP by Parent et al.8, 10 Because the present study included a more heterogeneous group of children with CP regarding their gait pattern, our results indicate that these adaptations are not restricted to children walking with excessive knee flexion and ankle dorsiflexion throughout the stance phase (crouch gait) or jump gait, as investigated by Parent et al.8, 10 In contrast to the increase in knee flexion and ankle dorsiflexion angles, we found negligible changes in kinetics associated with prolonged walking (Figure 3). This suggests that participants may have compensated, for example, to prevent excessive loading on the ankle and knee joint as muscle fatigue could have developed.9, 25 In a recent study on a subset of the children included in the present work,26 we observed the development of signs of muscle fatigue during the protocol. While investigating the relationship between muscle fatigue, gait pattern adaptations, and ECoW is beyond the scope of the present study, this is an interesting direction for further investigation.
While we expected that prolonged walking would result in increased ECoW, this was not the case (Figure 3 and Table 2). In fact, the results of children with CP suggest the opposite, showing a decrease in ECoW with prolonged walking, although this effect was not significant. Several factors could have a role in this. First, even though participants had a practice session before the start of the experiments, habituation to treadmill walking may have continued throughout the protocol. In particular, this may have affected the results on ECoW because this outcome takes longer to stabilize than kinematics and kinetics.27, 28 Second, little is known about how the ECoW is regulated in CP.3, 29 It is unclear whether the gait pattern of children with CP is indeed optimized to metabolic efficiency because other factors might also have a role in gait optimization.3, 30-32 This is an interesting direction for future investigation. Finally, measurements of metabolic gas exchange have some restrictions in their reliability and sensitivity, especially in children with CP.33 Therefore, while assessment of ECoW is an accepted tool in the rehabilitation management of children with CP,2, 11 this outcome measure may not be sensitive enough to detect fatigue-related gait adaptations in this relatively small and heterogeneous sample of participants.
The observed changes in gait kinematics and kinetics are not a direct measure for a ‘decreased performance’ or ‘increased effort’ according to the definition of physical fatigue that was adopted in this study.4, 7 Furthermore, there is no such thing as one clear definition of the concept ‘fatigue’ and the term covers a wide spectrum of physical and cognitive aspects.7, 34 To quantify the rate of subjective perceived exertion, OMNI scores were included. Despite the limitations of such subjective measures in children, the outcomes confirmed that both groups experienced fatigue after completing the protocol;16 therefore, we believe that the current findings can be attributed to the development of physical fatigue to at least some extent.23 Since manifestation of physical fatigue is highly context dependent,35 assessment of prolonged walking with a tailored protocol like the one introduced in the current study, can be a useful addition to conventional clinical gait analysis because it can help to identify specific problems that emerge when walking longer distances.
Several limitations should be considered when interpreting the present study. First, we only investigated a small heterogeneous sample and not all data were available for all children. Moreover, our statistical analyses included many outcome parameters, thus introducing the risk of type I errors. Furthermore, the protocol could not always be followed strictly. As we handled missing data conservatively, the current results might represent an underestimation of real-life situations. Although we believe that some data loss is inevitable given the set-up of the study and the equipment used, it highlights the limitations of conducting extensive measurements in this population. Additionally, while we strived to apply objective criteria to determine steady state, deciding how long the stabilization of outcomes should last to be able to speak of a stable situation is still a subjective process. Finally, the predicted heart rate threshold as a proxy of ventilation threshold, which was used to guide the protocol, was estimated based on the group average data reported in the literature, although heart rate and ventilation threshold are known to differ widely between individuals.14 However, as we were mainly interested in within-subject changes, we do not believe this variation affected the conclusions of our study.
Conclusions
The present study shows that gait deviations in children with CP progress with prolonged walking, as reflected by a higher GPS, increased knee flexion and ankle dorsiflexion, and the RMSE of individual joint curves in this group. Limited systematic pattern changes were found, indicating that adaptations with prolonged walking were highly individual but resulted in worse gait quality for most children. Interestingly, this was not accompanied by a demonstrable increase in ECoW or changes in joint kinetics. These findings may provide a better insight into the relationship between gait kinematics and walking-induced fatigue. Furthermore, assessment of prolonged walking can be useful to improve diagnostics and a personalized approach to the treatment of fatigue-related walking.
ACKNOWLEDGMENTS
This work was supported by HandicapNL under grant no. R201605435; Phelps Stichting voor Spastici under grant no. 2017.015; Stichting Johanna Kinderfonds under grant no. 20170006; Cornelia-Stichting; and Kinderrevalidatie Fonds Adriaanstichting, as part of the MOVING-CP project. The authors thank all participating children and their parents. We generously thank Annet Dallmeijer for helping in designing the protocol and experimental set-up. We also thank Kirsten Veerkamp for assisting with the measurement protocol, Eefje Muselaers and Eline Bolster for their help with data interpretation, and Jorinde Scholten and Julien Pronk (Cosmed) for their technical support.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.