Early referral to multidisciplinary specialty centers to optimize outcomes in children with neonatal brachial plexus palsy
Abstract
Aim
To demonstrate the trajectory of long-term recovery of upper-extremity movement and determine optimal timing of evaluation at multidisciplinary specialty centers in children with neonatal brachial plexus palsy (NBPP).
Method
All children with conservatively managed NBPP seen at one institution from 2005 to 2020 were considered for inclusion. The cohort was divided according to age at formal evaluation (≤30 or > 30 days). Active range of motion (AROM) for shoulder and elbow movements collected at each appointment were compared in local age windows between early and late cohorts. Locally estimated scatterplot smoothing was used to demonstrate the trajectory of recovery for the overall cohort.
Results
More than 13 000 prospectively collected data points for 429 children (220 males, 209 females) were analysed. Elbow flexion improved to nearly full AROM for both groups over the course of the study. Shoulder abduction, forward flexion and external rotation, and forearm supination improved for the entire cohort, although greater absolute improvement, particularly at the shoulder, was seen in the early cohort (age at formal evaluation ≤30 days). AROM for elbow extension remained roughly stable for the early cohort but decreased for the late cohort (age at formal evaluation >30 days). AROM for forearm pronation decreased over time for both cohorts.
Interpretation
Our data demonstrate good long-term functional recovery for children with conservatively managed NBPP. However, early referral to multispecialty brachial plexus centers may optimize outcomes.
What this paper adds
- Many children with conservatively managed neonatal brachial plexus palsy have good long-term shoulder and elbow outcomes.
- Early referral to multidisciplinary clinics may maximize long-term shoulder and elbow recovery and optimize outcomes.
What this paper adds
Abbreviations
-
- AROM
-
- active range of motion
-
- NBPP
-
- neonatal brachial plexus palsy
Neonatal brachial plexus palsy (NBPP) is a perinatal condition with an incidence of 0.9 to 1.5 per 1000 live births that results in weakness and sensory disturbances in the upper extremity.1-3 More than 30% of patients develop lifelong impairments,4 including impaired extremity function, behavioral challenges, musculoskeletal and cosmetic deformity, and socioeconomic limitations.5, 6 Most children present with Erb palsy, reflecting upper trunk and nerve root injury, but nearly all patients with NBPP have some degree of impairment of shoulder and elbow movement.
Management of these children ranges from rehabilitation and therapy alone to surgical nerve or muscle reconstruction. Historically, the paradigm that ‘all NBPP recovers’ guided treatment. However, with the advent of safe and efficacious nerve reconstruction options, surgery has become a potential treatment for NBPP. While indications for surgery are controversial,7, 8 most surgeons view the goal of surgical intervention as exceeding the outcomes achieved by conservative means, thus maximizing functional recovery and limiting persistent disability. Notably, there is a paucity of published studies regarding outcomes after conservative management; the studies that are available are limited by their retrospective nature, small overall numbers, and short follow-up times.9-11 In their systematic review aimed at determining the natural history of nonoperative NBPP, Pondaag et al.2 concluded that ‘although the natural history of [NBPP] has been described in a large number of studies, no study had the width of scope necessary to answer the question posed’.
Optimal timing of referral of patients to multidisciplinary specialty centers, which provide access to occupational therapy, rehabilitation providers, and nerve surgeons, is also unclear, particularly if the child's primary physician is waiting for and anticipating spontaneous recovery. Several groups have advocated for early referral, but to date the impact of early management at a specialty center on functional recovery has not been demonstrated.3, 12-14
In this study, we interrogated a prospectively collected database of conservatively managed children with NBPP evaluated or treated at a single multidisciplinary specialty NBPP center over a 15-year period to demonstrate the trajectory of recovery of active range of motion (AROM) at the shoulder and elbow over time. Specifically, we tested the hypothesis that nonsurgically treated patients with NBPP spontaneously recover full AROM with time, and we ask whether early referral to a specialty center alters the trajectory or maximal extent of recovery (or both).
METHOD
Participants
All patients who were referred to a single tertiary, multidisciplinary brachial plexus clinic for NBPP from November 2005 to November 2020 were included in the initial data set. All children were considered for surgical intervention according to the University of Michigan NBPP Treatment Pathway; those who underwent nerve surgery for NBPP were excluded from the analysis.8 To avoid including patients with delayed presentation who may have been candidates for surgery at a younger age, we excluded patients initially seen after 2 years of age, which is our age cutoff for nerve reconstruction. This is because the neuromuscular junction is nonfunctional after about 18 months of denervation, meaning that no motor recovery is possible even with nerve regeneration.15, 16 This study was approved by the institutional review board of the University of Michigan (HUM00208187).
Primary outcome
The primary outcome for this study was AROM for shoulder abduction, shoulder forward flexion, shoulder external rotation, elbow flexion, elbow extension, forearm supination, and forearm pronation (Table S1). Normal ranges were defined as being within 10 degrees of full AROM for each movement. AROM data were collected at each clinic visit by one of three qualified occupational therapists using standardized clinical goniometry. Patients with full or sustained recovery were released from the clinic but were free to schedule follow-up appointments at the discretion of the parents and patient.
Data collection
Patient data included the primary outcome, patient demographic characteristics, and clinic-specific data, as well as date of birth and date of clinic appointment. All data were stored in an institutional review board-approved SQL database. Data were entered via a Web application encoded for by ColdFusion (Adobe, San Jose, CA, USA) that was written to an SQL data set, which was then queried using the appropriate inclusion and exclusion criteria. Data were then cleaned manually using pandas, an open-source data analysis and manipulation tool in Python (NumFOCUS, Austin, TX, USA; https://pandas.pydata.org/).
Statistical analysis and modeling
The data consisted of serially observed repeated measures of each muscle movement in each individual for each clinic visit. All AROM measurements were normalized to between 0 and 1, with 0 being no AROM and 1 being full AROM. We then stratified the AROM measurements into 20 windows based on the age of the individual, with the windows containing approximately equal numbers of observations. The selection of 20 windows provided 80% power to detect a difference in the cohorts of 0.6 to 0.7 SD, considered to be a moderate effect size. Within each age window, a regression model expressing the expected AROM as a linear function of treatment group was fitted using generalized estimating equations to compare early and late treatment groups. Specifically, this linear model included an intercept and main effects for treatment group and age. A Wald test was conducted based on this fitted model to assess for statistically significant differences in mean responses between individuals who were and were not treated early. The mean responses within each age window for the early and late treatment groups were plotted separately and windows with statistically significant differences between early and late treatment groups were denoted with a red asterisk. Locally estimated scatterplot smoothing was also used to visualize the trajectory of recovery for the group as a whole.17
Data visualization and model development was performed using open-source packages in Python, including NumPy v1.21 (https://numpy.org), statsmodels v0.13.5 (https://statsmodels.org), and Matplotlib v3.4.3 (https://matplotlib.org).
We also reported descriptive statistics for patient demographic data, with p < 0.05 considered statistically significant. All analyses were performed with SPSS v22 (IBM Corp., Armonk, NY, USA).
RESULTS
Six hundred and eighty-five patients were evaluated for NBPP at a single tertiary referral center between November 2005 and November 2020. Of these, 100 patients underwent nerve surgery and were excluded from the analysis. One hundred and fifty-four patients were seen initially after 2 years of age and two patients had no AROM recorded, leaving a total of 429 patients (220 males, 209 females) representing 441 injured arms (Figure S1).
To determine the long-term impact of age at presentation on recovery of AROM of the upper extremities, four age cutoffs were modeled: presentation to a specialty clinic before and after 30, 60, 90, and 120 days. The 30-day cutoff was the most predictive of differences in long-term outcomes (Figures S2 and S3); additional analyses focused on this cohort.
One hundred and thirty-one children were initially evaluated early (≤30 days), while 298 were evaluated later (>30 days). The mean (SD) follow-up was 23.44 (35.92) months. There was no difference in mean follow-up between the group who presented to the clinic at 30 days or earlier versus the group who presented to the clinic later than 30 days (25.84 months vs 22.39 months, p = 0.37). There were no differences in sex, ethnic grouping, side of injury, and extent of injury (Narakas classification) between the two groups (Table 1).
| n = 429 | Presented at ≤30 days (n = 131) | Presented at >30 days (n = 298) | p | |
|---|---|---|---|---|
| Mean age at initial visit, months (SD) | 3.81 (4.61) | 0.47 (0.3) | 5.28 (4.84) | <0.001 |
| Follow-up period, months (SD) | 23.44 (35.92) | 25.84 (35.5) | 22.39 (36.11) | 0.37 |
| Sex, n (%) | ||||
| Male | 220 (51) | 64 (49) | 156 (52) | 0.51 |
| Female | 209 (49) | 67 (51) | 142 (48) | |
| Ethnicity, n (%) | 0.71 | |||
| White | 286 (67) | 89 (68) | 197 (66) | |
| Other | 143 (33) | 42 (32) | 101 (34) | |
| NBPP-involved side, n (%) | 0.46 | |||
| Left | 208 (49) | 60 (54) | 148 (50) | |
| Right | 221 (52) | 71 (46) | 150 (50) | |
| Narakas classification, n (%) | 0.42 | |||
| Levels I and II | 310 (72) | 98 (75) | 212 (72) | |
| Levels III and IV | 116 (28) | 32 (25) | 84 (28) |
- Abbreviation: NBPP, neonatal brachial plexus palsy.
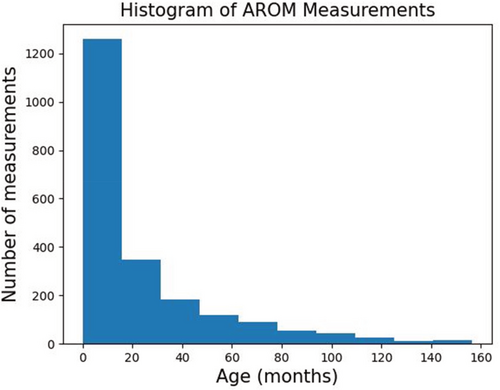
A total of 13 139 AROM measurements were collected for shoulder abduction, forward flexion, and external rotation and elbow flexion, extension, supination, and pronation and plotted against patient age for the group who presented to the clinic early (n = 4572) and the group who presented to clinic later (n = 8567). A histogram was plotted to demonstrate the distribution of patient age at the time of AROM measurement (Figure 1).
The plots of normalized AROM against patient age for shoulder abduction, forward flexion, and external rotation are shown in Figure 2 (Tables S2–S4). For the overall group, AROM recovery for shoulder abduction and forward flexion largely improved in a parallel fashion as patient age increased, although there was some tapering at the later time points. Importantly, despite a lower starting AROM, there was a statistically significant difference in long-term AROM between the two groups, with 27.8% more AROM in shoulder abduction (162° vs 113°, p = 0.01) and 23.1% more AROM in shoulder forward flexion (156° vs 114°, p = 0.049) for the early group than for the late group. Regarding shoulder external rotation, the greatest improvement in AROM for the overall group occurred within the first 20 months, again with some tapering and stabilization of recovery over time. The group who presented to the clinic early had significantly better AROM than the group who presented to the clinic later, between 28 and 33 months, 40 and 48 months, and 61 and 73 months, although significance did not persist at the latest time points.
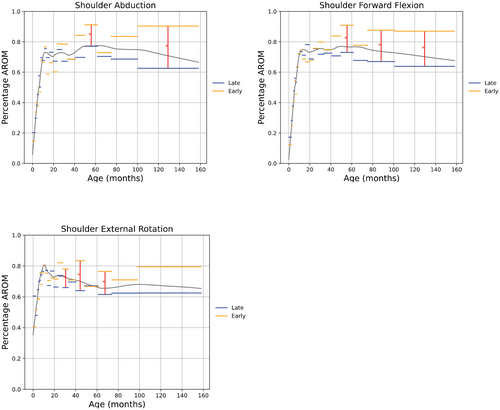
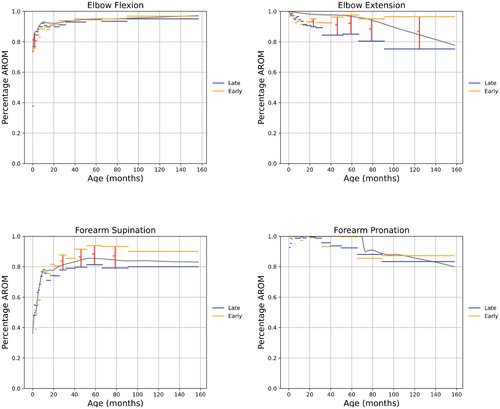
Figure 3 shows the plots of normalized AROM for elbow flexion, elbow extension, forearm supination, and forearm pronation (Tables S5–S8). For the overall cohort, AROM for elbow flexion demonstrated near-complete recovery by approximately 5 years of age. Forearm supination AROM also improved with age, although to a lesser extent than elbow flexion, while the AROM for elbow extension and forearm pronation decreased over time. For elbow extension, there was a statistically significant difference in long-term AROM between the early and late groups, with 21.2% more AROM for the early group than for the late group (−3.2° vs −22.2°, p < 0.001). For forearm supination, there was a statistically significant difference in AROM between the groups from 25.8 to 31.9 months of age (67.9° vs 50.2°, p = 0.02), 40.7 to 51.6 months (74.7° vs 53.6°, p = 0.003), 51.6 to 66.4 months (78.8° vs 56.5°, p = 0.008), and 66.4 to 90.9 months (78° vs 52.6°, p = 0.002). However, the significance did not persist at the latest measured time points. For elbow flexion, the late group outperformed that early group from 1.5 months of age to 2.4 months of age (127.7° vs 113.5°, p = 0.05) but there was no significant difference between the groups at the later time points. For forearm pronation, there was no significant difference between the groups at any time point.
DISCUSSION
In this study, we analysed the AROM for seven discrete and relevant upper-extremity movements measured during clinic visits over the course of 15 years for 429 children with nonoperative NBPP and illustrated the trajectory of recovery of AROM of each movement for the overall cohort over time. The overall cohort had nearly complete recovery of elbow flexion AROM, while recovery to approximately 60% to 80% of full AROM was seen for shoulder abduction, forward flexion, and external rotation, and in forearm supination. Loss of AROM was also noted for elbow extension and forearm pronation. These findings refute the hypothesis that patients with conservatively managed NBPP eventually achieve full AROM. However, we found that children referred to a specialty clinic within 30 days of birth had better overall recovery of AROM for shoulder abduction, forward flexion, and external rotation, and forearm supination, with reduced loss of elbow extension AROM (Figures 2 and 3).
Historically, recovery of shoulder function has lagged behind recovery at the elbow. However, a recent study of adults with brachial plexus injury showed a direct correlation between shoulder AROM and real-world use of the arm as measured using wearable technology, emphasizing the importance of adequate shoulder movement to spontaneous, patient-initiated use of the arm in everyday life.18, 19 These studies underscore the importance of our findings that children evaluated at a specialty center within 30 days have significantly better long-term AROM in shoulder abduction and forward flexion. While not statistically significant at the latest time point, shoulder external rotation AROM for the early group was consistently better than for the later group.
We were not surprised to see that elbow extension AROM decreased for the overall cohort over time. Elbow flexion contracture is a well-known complication of NBPP, with prevalence reported between 25% and 89%.20 Elbow extension has an important role in stabilizing the arm while lifting, carrying, pushing, pulling, and throwing; contractures greater than 30 degrees interfere with activities of daily living.21, 22 Additionally, children and adolescents with NBPP have reported concerns about the cosmetic appearance of elbow flexion contracture.23 The etiology of elbow flexion contracture is controversial; however, recent evidence from mouse models suggests that denervation of flexor muscles in the arm results in decreased growth of muscle sarcomeres and shortening of the muscle, which in turn leads to musculoskeletal contracture.20
However, we were very surprised to see that children seen within 1 month had almost no loss of elbow extension over time. Taken together, these data suggest that early specialized rehabilitation may help prevent potentially disabling elbow flexion contracture, possibly by preventing sarcomere shortening of the biceps muscle.
We also noted loss of forearm pronation for the overall cohort. Like elbow flexion contracture, supination contracture is a known complication of NBPP, with an overall incidence in one series of 7% that rises to 23% in patients with injury involving the entire brachial plexus.24 Our data argue for vigilance in recognizing and addressing the development of supination contractures in this patient population.
Initiation and duration of therapy
Occupational therapy techniques, including stretching to maintain passive range of motion and avoid joint contracture, motor and sensory stimulation to avoid developmental apraxia,25 encouragement of bimanual activity,26 use of electrostimulation and kinesiology tape,27 muscle strengthening, and development of coordination and fine motor skills,28 are used extensively in our clinic for conservative management of NBPP. Historically, early initiation of therapy or passive range of motion exercises was discouraged to allow for nerve recovery; however, we previously demonstrated that no increased shoulder subluxation occurs with early initiation of range of motion exercises.29 Unfortunately, knowledge of appropriate treatment of patients with NBPP is still lacking in the community; in a study of pediatric providers, including occupational and physical therapists, 71% reported discomfort with the diagnosis and management of NBPP.30 Thus, while some of the children seen later than 30 days probably received physical or occupational therapy before evaluation at our clinic, it is unlikely that they received therapies aimed specifically at NBPP.
Currently, no consensus exists regarding the optimal duration of therapy. Our data show that, remarkably, recovery may continue even many years after injury, supporting earlier case study observations of improved upper-extremity function in a 17-year-old with right-sided NBPP after a home-based movement therapy training program.31 Continued improvement in arm function reflects, in part, the plasticity of the central nervous and neuromuscular systems in response to movement-related sensory feedback arising from therapy or spontaneous arm use (or both). Thus, these observations support a role for the early initiation of and continued therapy in patients with persistent deficits long after the initial presentation.
Parental satisfaction
It is important for providers who manage patients with NBPP to recognize the importance of caring for both patient and caregivers. The birth of children with disability can be traumatic for parents, with reactions resembling a bereavement response.32 In their study of parents of children with NBPP, Bellew and Kay33 found a high level of dissatisfaction with communication of the diagnosis, primarily reflecting a perceived lack of knowledge about NBPP by the diagnosing provider. Thus, they recommended early referral to a specialist center to maximize support for parents. These data, together with our findings, suggest that early referral to a clinic specialized in the care of NBPP can optimize the care of both patients and their families.
Strengths and limitations
The strengths of this work include the relatively large cohort of 429 patients representing 441 injured arms and over 13 000 AROM measurements. Data were collected prospectively over the course of 15 years, with a mean follow-up of nearly 5 years.
This study has several important limitations. Patients with full or sustained recovery were free to leave the clinic; thus, not every patient was evaluated for the entire time course represented on our plots (including patients seen at only one visit). This is reflected in our histogram, which shows that most measurements were performed within the first 5 years of life (Figure 1). Additionally, some patients may have been lost to follow-up before being released from the clinic. We hypothesize that patients who chose not to return to the clinic before formal release were probably less impaired than those who continued to be seen. For these reasons, our plots may be biased pessimistically, in that patients with persistent deficits are probably overrepresented at later time points.
We also acknowledge the challenge of obtaining accurate AROM measurements in very young children. To mitigate the impact of this difficulty on our results, one of only three certified occupational therapists, with over 10 years of pediatric experience, evaluated each child over the course of the entire study, increasing the reliability and reproducibility of our results. We note, however, that the key findings of the study relate to the long-term impact of early evaluation at a specialty clinic, at which age children are better able to participate in examinations.
Additionally, children who are referred to and continue to present to a multidisciplinary clinic over the course of years may represent the far end of the spectrum in terms of impairment. However, as our goal was to minimize severe disability in the overall cohort, the conclusions drawn from these analyses are still useful.
The use of AROM as our primary outcome is another potential limitation. While useful in assessing longitudinal improvements in a specific aspect of upper-extremity function, AROM does not necessarily reflect real-life use of the arm to participate in activities of daily living.34 We recently demonstrated the feasibility of wearable motion sensors to better assess true, real-world arm function in adults with brachial plexus injury;18, 19 the use of accelerometry data to determine patient outcomes in this population is another important direction for future work.19 Additionally, we did not investigate differences in passive range of motion between cohorts. Most early therapies are focused on stretching to preserve joint mobility; it is possible that the improvements in AROM seen in the early cohort are reflective in part of maintenance of passive range of motion. This is another important area for further study.
Finally, we note that our data are collected from a single multidisciplinary clinic. Understanding the generalizability of these findings to other centers is an important future direction for this work.
Conclusions
Patients with NBPP who are deemed to be nonoperative candidates do not necessarily go on to have full recovery of upper-extremity AROM, suggesting the possibility of broader and additional indications for early therapeutic efforts. However, patients referred to a multidisciplinary program within 30 days of birth have better long-term outcomes than those with later initial evaluations. Our data support the critical significance of early referral to a clinic specialized in the care of NBPP to optimize long-term functional recovery.
ACKNOWLEDGMENTS
We acknowledge the contributions of Consulting for Statistics, Computing & Analytics Research of the University of Michigan, and in particular Kerby Shedden, for assistance with the statistical analyses.
Open Research
DATA AVAILABILITY STATEMENT
Data available on request due to privacy/ethical restrictions