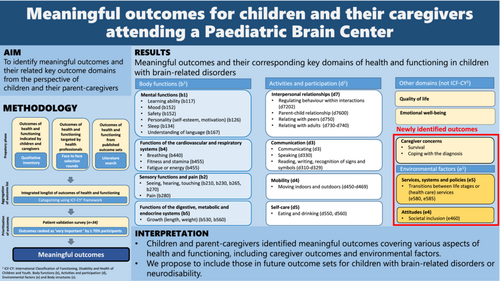
Meaningful outcomes for children and their caregivers attending a paediatric brain centre
Abstract
Aim
To identify meaningful outcomes of children and their caregivers attending a paediatric brain centre.
Method
We compiled a long list of outcomes of health and functioning of children with brain-related disorders such as cerebral palsy, spina bifida, (genetic) neurodevelopmental disorders, and acquired brain injury. We incorporated three perspectives: patients, health care professionals, and published outcome sets. An aggregated list was categorized using the International Classification of Functioning, Disability, and Health: Children and Youth version in a patient validation survey for children and parent-caregivers to prioritize outcomes. Outcomes were considered meaningful when ranked ‘very important’ by 70% or more of the participants.
Results
We identified 104 outcomes from the three perspectives. After categorizing, 59 outcomes were included in the survey. Thirty-three surveys were completed by children (n = 4), caregivers (n = 24), and parent-caregivers together with their child (n = 5). Respondents prioritized 27 meaningful outcomes covering various aspects of health and functioning: emotional well-being, quality of life, mental and sensory functions, pain, physical health, and activities (communication, mobility, self-care, interpersonal relationships). Parent-caregiver concerns and environmental factors were newly identified outcomes.
Interpretation
Children and parent-caregivers identified meaningful outcomes covering various aspects of health and functioning, including caregiver concerns and environmental factors. We propose including those in future outcome sets for children with neurodisability.
What this paper adds
- Outcomes that children with brain-related disorders and their parent-caregivers consider to be the most meaningful cover a wide range of aspects of functioning.
- Involving these children and their parent-caregivers resulted in the identification of important outcomes that were not covered by professionals and the literature.
- Parent-caregiver-related factors (coping, burden of care) and environmental factors (support, attitudes, and [health care] services) were identified as meaningful.
What this paper adds
- Outcomes that children with brain-related disorders and their parent-caregivers consider to be the most meaningful cover a wide range of aspects of functioning.
- Involving these children and their parent-caregivers resulted in the identification of important outcomes that were not covered by professionals and the literature.
- Parent-caregiver-related factors (coping, burden of care) and environmental factors (support, attitudes, and [health care] services) were identified as meaningful.
Meaningful outcomes in children and their caregivers with brain-related disorders (such a cerebral palsy, brain injury and genetic neurodevelopmental disorders) were identified using a online patient validation survey assessing salient outcomes. The survey was based on the integrated outcomes from the perspectives of families, health-care professionals and literature.
Video Podcast: https://youtu.be/j9S3atd3LqM
This original article is commented on by Geboers on pages 1419–1420 of this issue.
There is a letter to the editor on this original article by Oakeshott et al. on page 1531
Abbreviations
-
- ICF
-
- International Classification of Functioning, Disability and Health
-
- ICF-CY
-
- International Classification of Functioning, Disability and Health: Children and Youth version
-
- ICHOM
-
- International Consortium for Health Outcomes Measurement
-
- PBC
-
- Pediatric Brain Center
The outcomes of health and functioning, that matter most to patients, are important as they reflect each patient's priority in evaluating their own health care and health outcomes. Using such meaningful outcomes is an inherent aspect of value-based health care.1 Incorporation of the patients' perspective is a key factor because patients or their representatives do not necessarily share the same values as health care professionals and researchers.
The identification of meaningful outcomes valued important by the patient is critical when selecting patient-reported outcomes for clinical care and research. Addressing those outcomes, which reflect the patient's current life situation about their expectations, health conditions, and its management, is considered the new standard.2 Meaningful outcomes may improve the recognizability for patients and facilitate shared decision-making. Incorporation of meaningful outcomes in research contributes to improving health care.3
Involvement of children and their parent-caregivers in developing standard (core) outcome sets is facilitated by the structured methodology of the International Consortium for Health Outcomes Measurement (ICHOM), Core Outcome Measures in Effectiveness Trials, and guides on how to develop the International Classification of Functioning, Disability, and Health (ICF) core sets.4-6 In the past decade, outcome sets have been developed for specific chronic conditions in paediatric health care.7-11 The ICHOM set ‘Overall Paediatric Health’ is an example of a more generic set based on meaningful outcomes for all infants, children, and young people from birth to 24 years of age, regardless of their underlying health condition.12, 13
In the Pediatric Brain Center (PBC) of the Erasmus MC—Sophia Children's Hospital, the Netherlands, multidisciplinary teams of health care professionals provide care to children with brain-related disorders, such as cerebral palsy, spina bifida, (genetic) neurodevelopmental disorders, or acquired brain injury resulting from various conditions. In the Child Brain Lab, a testing facility for brain development and function of children in several domains, we have developed a long-term systematic follow-up of these children to monitor their health and development using patient-reported outcomes measures and clinical tests. Identifying meaningful outcomes was one of the first steps in this process.
Children with brain-related disorders often face challenges in dealing with their disabilities and health complications because of the chronicity of their conditions and their perspectives on their quality of life.2, 14 Their limitations in daily functioning involve their mental and sensory functions, mobility, communication, self-care, and their community and social life. They share similar problems despite different underlying conditions. This diagnosis-overarching aspect of brain-related disability is captured by the term neurodisability.15 The current perspective on health and disability encompasses functional abilities and their contextual determinants as essential aspects of functioning.16 The Children and Youth version of the ICF (ICF-CY) provides a holistic framework to capture all aspects of health and functioning using a positive focus on abilities and a broad perspective, including the role of environmental and personal factors in a child's functioning.17 Involvement and engagement of parent-caregivers and family are essential as they represent the child's environmental factors in the ICF-CY. The introduction of family as one of the ‘F-words’ by Rosenbaum et al. illustrates this.18
Using the ICF-CY, Morris et al. developed a cross-diagnostic set of 12 key outcome domains for children with neurodisability.19, 20 A stakeholder prioritization of integrated outcomes from three perspectives was performed: children with neurodisability and their parent-caregivers; health care professionals; and a systematic review of patient-reported outcome measures that assessed various aspects of health and functioning. However, environmental and personal factors were not investigated.
Assuming that (1) environmental and personal factors might be identified as meaningful and (2) cultural factors may play a role in valuing outcomes by patients, we performed a new survey among children with brain-related disorders and their parent-caregivers who receive care from the PBC.
The present study aimed to identify outcomes that were valued as the most important by children and their parent-caregivers of the PBC.
METHOD
Participants
The participants of the advisory panel and the patient validation survey were parent-caregivers and their child attending regular consultations at one of the collaborating outpatient clinics of the PBC or Rijndam Rehabilitation (Rotterdam, the Netherlands) from 1st October 2020 to 1st March 2021. Participating departments from the Erasmus MC—Sophia Children's Hospital were neurology, neurosurgery, psychiatry, ear/nose/throat medicine, plastic surgery, general paediatrics, ophthalmology, orthopaedic surgery, and paediatric rehabilitation from Rijndam Rehabilitation. Parent-caregivers and their children were handed the information letter and the invitation for participation by their physician. At 8 and 16 weeks of the inclusion period, the primary contact professionals of the collaborating departments received a reminder e-mail to support exposure of the survey despite overloaded patient care and reduced outpatient visits because of the COVID-19 lockdown.
The following patient characteristics were collected in the survey: age, sex, diagnosis, duration of diagnosis, educational level, and health care facility where the child and their parent-caregivers were approached.
The Medical Ethics Committee of the Erasmus MC, University Medical Center Rotterdam, the Netherlands, approved the study. Informed consent was obtained from participants and/or their legal guardians.
Study design
The study design was based on the ICHOM methodology.21 In the preparatory phase (Figure S1), potentially important outcomes were collected from three perspectives. First, to gain insight in relevant topics from the child's perspective, parent-caregivers serving on an advisory panel of the PBC were asked to participate in an interview using a secure online platform for video consultation (FaceTalk, Qconferencing, Diemen, the Netherlands). The interviews were conducted by one of the authors (either MAH-K or AKKS), except for the first interview, which was conducted by both researchers to ensure standardization. A conventional content analysis was performed by MAH-K and AKKS independently to identify outcomes from the recorded interviews.22 Outcomes identified by one researcher were discussed and were added when consensus was reached.
Second, the PBC professionals focused on the following areas of health and functioning: structure of the brain, brain and related functions, growth (the physical aspect of development), cognition and behaviour, speech function and communication, motor function and mobility, daily activities, and quality of life. Ten expert groups with four to eight professionals of different clinical backgrounds were dedicated to a specific area and met three times to decide on the most relevant outcomes for each area. Each expert group consisted of at least one physician, one psychologist/psychiatrist, one therapist (physiotherapist/speech and language therapist), and one researcher.
Third, a literature search in PubMed was performed in February 2020 to identify outcomes from published outcome sets and ICF core sets in comparable patient groups.
Next, the identified outcomes of health and functioning from these three sources were aggregated into a longlist. The ICF-CY was used to categorize and compare all identified outcomes of the longlist, according to published linking rules.23 Outcomes that were not covered by the ICF-CY framework were described and included as ‘no ICF category’. The outcomes of the longlist were combined when they conceptually overlapped and, in the next step, they were aggregated from third- and fourth-level categories to their common second-level category. This resulted in a reduced number of distinct outcomes (i.e. the outcome shortlist).
From this outcome shortlist the patient validation survey was composed. Participants, parent-caregivers, and/or their child were asked to prioritize each outcome. In line with Dutch law, which gives children aged 12 to 15 years partial autonomy and young people from age 16 years complete autonomy in medical decision-making, parent-caregivers of children aged under 12 years were invited to complete the online survey. Children aged 12 to 15 years without intellectual disabilities were invited to participate in the survey together with their parent-caregivers. Children aged 16 years and older without intellectual disability were invited to complete an individual survey as well as their parent-caregivers. An Open Source survey tool (LimeSurvey GmbH, Hamburg, Germany) was used to conduct the survey.
A 9-point Likert scale was used for ranking the importance of the outcomes by adults, and a traffic-light system (3-point Likert scale) by children aged under 12 years in which the scores 1 to 3 were represented by a red box labelled as ‘not that important’, scores 4 to 6 as an orange box labelled as ‘important’, and scores 7 to 9 as a green box labelled ‘very important’.24, 25 Each item was provided with an additional scoring option ‘don't know’, and a free text box to add missing outcomes of health and functioning.
The 70/15 consensus definition, used by Harman et al. from the COMET handbook version 1.0., was applied: outcomes were labelled ‘meaningful’ when a minimum of 70% of the respondents scored ‘very important’ (7–9 on a 9-point Likert scale for parent-caregivers and green traffic light for children) and less than 15% scoring ‘not that important’ (1–3 on the 9-point Likert scale and red traffic light for children).25, 26
In the final step, the meaningful outcomes were aggregated in outcome domains of the corresponding ICF first-level chapter in order to abstract the overhead domains of health and functioning (i.e. so-called key domains of health).
Statistical analysis
Descriptive statistics were used to calculate scores from the 9- and 3-point Likert scale. Data analysis was conducted with SPSS, version 24.0 (IBM Corp., Armonk, NY, USA).
RESULTS
Participants
Qualitative interviews
Six families consisting of two mother–father dyads, one mother–father–child (12 years old) triad, two mothers, and one foster mother participated in the qualitative inventory. The six children were aged between 3 years and 12 years (mean 8 years 2 months) and four were male. They were diagnosed with Angelman syndrome, Apert syndrome, acquired brain injury, epilepsy, myelomeningocele, and cleft palate. As all study participants were anonymous, it was unknown whether any of these six families also participated in the patient validation survey.
Online survey
Thirty-three surveys of 31 unique children were completed. The characteristics are presented in Table 1. The surveys were completed by four children, five caregivers together with their child, and 24 parent-caregivers.
| Characteristic | |
|---|---|
| Age, years:months | |
| Mean | 8:7 |
| SD | 6:2 |
| Range | 0:2–20:1 |
| Duration of neurodisability diagnosis, years:months | |
| Mean | 5:11 |
| SD | 5:3 |
| Range | 0–17:0 |
| Sex | n (%) |
| Male | 16 (51.6) |
| Diagnosis | n (%) |
| Apert syndrome | 2 (6.4) |
| Cerebral palsy | 11 (35.5) |
| GRIN2B | 3 (9.7) |
| Brain tumoura | 4 (12.9) |
| Otherb | 9 (29.0) |
| unknown | 2 (6.4) |
| Age category, years | n (%) |
| 0–<5 | 14 (45.2) |
| 5–<12 years | 6 (19.3) |
| 12–20 years | 11 (35.5) |
| Education type | n (%) |
| Mainstream schoolc | 8 (25.8) |
| Special education school | 13 (41.9) |
| Preschool education or kindergarten | 3 (9.7) |
| Not attending school (age <4 years)d | 6 (19.4) |
| Centre | n (%) |
| Rijndam Rehabilitation | 5 (16.1) |
| Erasmus MC—Sophia Children's Hospital | 15 (48.4) |
| Both centres | 11 (35.5) |
- a Ganglioglioma (n = 2), craniopharyngioma, neurocytoma.
- b n = 1: hydrocephalus, Doose syndrome, corpus callosum agenesia, acquired brain injury due to meningitis and Apert syndrome, Trio syndrome, severe hearing loss, depressive disorder, encephalopathy after resuscitation, developmental delay.
- c Mainstream school: primary and secondary school.
- d In the Netherlands children attend primary school from the age of 4 years.
Inventories of important outcomes
In the qualitative interviews, the parent-caregivers reported 83 outcomes, while the health care professionals of the PBC reported 51 outcomes. The literature search identified 57 outcomes from 10 publications concerning outcome sets for comparable patient groups: five publications on ICHOM standard sets of patient-centred outcome measures, three published core outcome sets, and two publications on meaningful outcomes in neurodisability.7-11, 13, 19, 20, 25, 27, 28
In total, 104 unique outcomes were identified from these three sources, which we refer to as the longlist. Children and parent-caregivers reported 83 outcomes, the professionals reported 52 outcomes, and the published outcome sets gave 64 outcomes. All three perspectives shared 35 outcomes, 24 outcomes were identified by two out of three. Children and parent-caregivers reported 30 unique outcomes, the professionals reported six unique outcomes, and published outcome sets gave 10 outcomes.
Combining overlapping outcomes and categorizing the outcomes of the longlist according to their corresponding ICF-CY categories resulted in 59 distinct outcomes that were used in the patient validation survey (see Table 2). Among these, the outcomes ‘coping with your child's diagnosis’, ‘caregiver burden of care’, and ‘transition of stages of life or (health care) services’ were presented to parent-caregivers only.
| Health and functioning outcomes of patient validation study | Percentage of participants rating ‘Very important'a (n = 33) | Identified by C/P/Ob | Categorized ICF-CYc component b/d/e/s |
|---|---|---|---|
| Emotional well-being | 97 | C/P/O | –d |
| Personality (self-esteem, motivation) | 91 | C/P/O | b |
| Mood | 91 | C/P/O | b |
| Safety | 91 | C/P/O | b |
| Quality of life | 91 | O | – |
| Communicating | 88 | C/P/O | d |
| Parent–child relationship | 85 | P | d |
| Speech | 82 | P | b |
| Relating with peers | 82 | C/P/O | d |
| Growth (length, weight) | 79 | C/P/O | b |
| Control behaviour | 79 | P | d |
| Hearing, seeing, sensing | 79 | C/P/O | b |
| Breathing | 79 | O | b |
| Societal attitudes and societal inclusion | 79 | C/P/O | e |
| Pain | 76 | C/P/O | b |
| Survival | 76 | C/P/O | – |
| Coping with the diagnosis | 75 | C/P/O | – |
| Sleep | 73 | C/P/O | b |
| Understanding of language | 73 | C/P/O | b |
| Reading, writing, recognition of signs and symbols | 70 | C/P/O | d |
| Fitness and stamina | 70 | C/P/O | b |
| Fatigue or energy | 70 | C/P/O | b |
| Learning ability | 70 | C/P/O | b |
| Moving indoors and outdoors | 70 | C/P/O | d |
| Eating and drinking | 70 | C | d |
| Relating with adults | 70 | C/P/O | d |
| Transition of stages of life or (health care) services | 70 | C | e |
| Body image | 67 | O | b |
| Muscle strength | 67 | C/P/O | b |
| Let me decide | 67 | C/P/O | d |
| Daytime activities such as (pre)school or work | 67 | C/P/O | d |
| Leisure activities | 67 | C/P/O | d |
| Dental health | 67 | O | s |
| Social support and access to health care | 67 | C/P/O | e |
| Structures of the nervous system | 64 | C/P/O | s |
| Walking ability | 64 | C/P/O | – |
| Caregiver burden of care | 64 | C | – |
| Support and relationships | 63 | C/P/O | e |
| Sense (organ) | 61 | C/P/O | s |
| Chewing and swallowing | 61 | C/P/O | b |
| Performing daily routines, general tasks, and demands | 58 | C/P/O | d |
| Cope with normal stresses of life | 58 | O | d |
| Manipulating objects | 55 | C/P/O | d |
| Organs | 55 | C/P/O | s |
| Structures involved in voice and speech | 55 | C/P/O | s |
| Structures related to movement | 55 | C/P/O | s |
| Concentration, memory | 55 | C/P/O | b |
| Self-care and hygiene | 52 | C/P/O | d |
| Continence | 45 | O | b |
| Constipation | 42 | C/P/O | b |
| Obtaining admission or transfer to school education levele | 42 | C | d |
| Products and technology for personal use in daily livinge | 42 | C/P/O | e |
| Salivation | 42 | O | b |
| Change body position | 36 | C/P/O | d |
| Interacting according to social rules | 36 | C/P/O | d |
| Day caree | 36 | C/P/O | e |
| Sexual healthe | 27 | C/P/O | b |
| Skin, hair, and nails | 27 | C/P/O | b |
| Household tasks | 27 | P/O | d |
- a A 9-point Likert scale was used to prioritize for adults and a traffic-light scale for children; ‘very important’ was defined as 7–9 on the Likert scale for parent-caregivers and as a green traffic light for children.
- b Children and caregivers (C), professionals (P), and published outcome sets (O).
- c International Classification of Functioning, Disability and Health: Children and Youth version, ICF-CY: Body functions (b), Activities and participation (d), Environmental factors (e), and Body structures (s).
- d No ICF-CY category available.
- e ≥15% of the participants scored ‘don't know’.
Patient validation study
Parent-caregivers and children with brain-related disorders prioritized 27 of the 59 outcomes of the longlist (46%) as meaningful (Figure 1). These meaningful outcomes addressed a broad spectrum of domains of health and functioning following the ICF-CY, except for the ICF-component ‘body structure’. Four meaningful outcomes addressed other key domains that could not be categorized in the ICF-CY: ‘quality of life’, ‘emotional well-being’, ‘survival’, and ‘coping with the diagnosis’ (the latter two were combined in the key domain ‘caregivers concerns’). Participants reported five additional outcomes in the free text box: ‘body position and balance’, ‘personal development’, ‘humour and putting things into perspective’, ‘acceptance by the community’, and ‘explanation of diagnosis to siblings’.
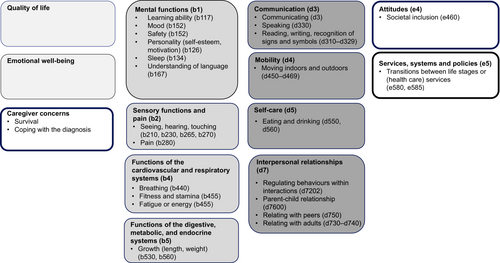
Meaningful outcomes and their corresponding key health and functioning domains for children with brain-related disorders.
International Classification of Functioning, Disability and Health: Children and Youth version (ICF-CY)17 letters refer to: Body functions (b), Activities and participation (d), Environmental factors (e); numbers refer to chapter and corresponding 2nd/3rd/4th subcategory.
DISCUSSION
In this study, we determined which outcomes of health and functioning matter most to parent-caregivers and their children with brain-related disorders in the PBC. We were interested in environmental and personal factors as we expected these to be important. We performed a patient validation survey based on a longlist of outcomes identified by three perspectives: patients, health care professionals, and published outcome sets. The meaningful outcomes were prioritized by parent-caregivers and their children and addressed a diversity of aspects of health and functioning, such as emotional well-being, quality of life, mental/sensory/digestive/cardiovascular functions, and activities, such as communication, mobility, and self-care. The results also indicated the importance of environmental factors concerning support and relationships, attitudes, and services, systems, and policies. Additionally, parent-caregivers identified ‘coping with the diagnosis’ as meaningful. The outcomes ‘social support and access to health care’ and ‘caregiver burden of care’ were prioritized respectively by 67% and 64% (Table 1), which suggests these outcomes are also important. No outcomes concerning the ICF chapter ‘body structure’ were prioritized as very important. The ranking scores of the outcomes ‘dental health’ (67%), ‘structures of the nervous system’ (64%), ‘sense (organ)’ (61%), and ‘chewing and swallowing’ (61%) suggest their importance as well.
Although the prioritization methodology of the present study differed from the cross-disorder study by Morris et al., the results are very similar except for caregiver concerns and environmental factors found in our study.19 Both studies identified meaningful outcomes involving activities regarding communication, mobility, self-care (including toileting), and relationships; various domains of mental functioning, including mental health, sleep, behaviour, safety, and pain; and emotional well-being. In contrast, the present study did not identify independence as a key outcome. In fact, we considered this outcome related to activities as communication, mobility, self-care, and interpersonal relationships. Recently, the ICHOM set for children with neurodevelopmental disorders (attention-deficit/hyperactivity disorder, communication disorders, motor disorders, or specific learning disorders) was published.29 Caregiver coping was included in this set.
Our work supports the importance of including parent-caregiver related outcomes, such as coping, burden of care, self-efficacy and parental stress, and environmental factors in outcome sets for children with brain-related disorders or neurodisability. First, this might encourage health care professionals to apply a broad focus when evaluating and monitoring the child patient's health and functioning. Supporting the parental role and finding ways to decrease the burden of care of parent-caregivers is likely to contribute to improvement of the child's health and functioning.30 Second, since participation in research can be a burden in itself for parent-caregivers, minimizing this burden can be accomplished by combining research and clinical care. In the PBC, we aim to feed back the results of the patient related outcome measurements directly to parent-caregivers in regular health care visits. This allows for discussing experienced burden and for offering psychosocial support, for example by involving a social worker and a psychologist.
This study has some limitations. We recruited a small sample of children with heterogenic brain-related disorders and their parent-caregivers. This might be because of the COVID-19 pandemic at the time of the study. Lockdowns in the Netherlands resulted in fewer outpatient consultations. We suspect the influence of the COVID-19 pandemic on the identified outcomes to be limited. The children of the PBC have chronic conditions and it seems likely that parent-caregivers view the health and functioning of their child beyond the relatively short period of the pandemic in the winter of 2021. We succeeded in including a heterogenic survey sample, although cerebral palsy diagnoses were overrepresented, which might have influenced the present results.
The present set of key health and functioning domains based on the identified meaningful outcomes will be incorporated into long-term systematic follow-up, as we aimed to develop a harmonized overarching outcome assessment for all multidisciplinary teams of the PBC. Additionally, we propose including our new findings, parent-caregiver concerns, and environmental factors in future outcome sets for children with brain-related disorders or neurodisability.
Although a small group of patients was recruited for this study, we will continue to test the relevance of these meaningful outcomes in the PBC.
This study concerned the first step in the process of knowing what to measure by identification and incorporation of meaningful outcomes. The next step, however, might be more challenging: how to measure these outcomes and which patient-reported outcome measures or measurements to select. In this process, researchers and health care professionals must find a careful balance between incorporating the perspectives of the patient and their interests, while avoiding burdening participants with overlong questionnaires.
Conclusion
This study confirms the importance of active involvement of children and their parent-caregivers in identifying meaningful health and functioning outcomes in children with brain-related disorders or neurodisability. Their prioritization of outcomes is crucial input when selecting outcomes of interest that are intended to be recognizable for children and their families, both in clinical care and research. The identified meaningful outcomes cover multiple aspects of health and functioning, including emotional well-being, quality of life, mental functioning, sensory functioning and pain, physical health, and activities such as communication, mobility, self-care, and interpersonal relationships. Additionally, our study is among the first to identify parent-caregiver concerns as well as environmental factors regarding support and relationships, attitudes, services, systems, and policies as meaningful. We propose including these aspects in future outcome sets for children with brain-related disorders or neurodisability.
ACKNOWLEDGMENTS
This study was funded by Rijndam Rehabilitation, Rotterdam, the Netherlands. We thank the children and parent-caregivers who participated in the advisory panel for working with us to develop the online survey questionnaire. We also thank the families that participated in the patient validation survey. We thank the Friends of the Sophia Hospital Foundation for their support, the professionals of the Paediatric Brain Centre for their input, and our colleagues for recruiting children and their parent-caregivers in their consultation, both at the Erasmus MC—Sophia Children's Hospital and Rijndam Rehabilitation.
Open Research
DATA AVAILABILITY STATEMENT
Data available on request from the authors