Neonatal brachial plexus palsy and hand representation in children and young adults
Abstract
enAim
To assess the impact of neonatal brachial plexus palsy (NBPP) on higher-order hand representation.
Method
Eighty-two left-handed children and adolescents with and without right-sided NBPP were recruited. Thirty-one participants with NBPP (mean age [SD] 11y 4mo [4y 4mo]; age range 6y 2mo–21y 0mo; 15 females; C5–6, n=4, C5–7, n=12, C5–T1, n=11, C5–T1 with Horner sign, n=4) were assessed along with 30 controls (mean age 11y 5mo [4y 4mo]; age range 6y 7mo–21y 7mo; 14 females). Participants’ estimated hand size and shape on measure of implicit and explicit hand representation was assessed. A linear mixed model (LMM) was used to investigate the effect of condition, sensorimotor impairment, and age.
Results
Individuals with NBPP showed a significant difference in implicit hand representation between affected and non-affected hands. LMM confirmed a significant influence of the severity of sensorimotor injury. Only the estimated implicit hand representation was associated with age, with a significant difference between 6- to 8-year-olds and 9- to 10-year-olds.
Interpretation
The effect of sensorimotor impairment on central hand representation in individuals with NBPP is specific due to its implicit component and is characterized by finger length underestimation in the affected hand compared to the characteristic underestimation in the unaffected hand. Neither NBPP nor age impacted the explicit hand estimate. This study confirms the importance of sensorimotor contribution to the development of implicit hand representation.
Parálisis del plexo braquial neonatal y representación de las manos en niños y adultos jóvenes
esObjetivo
Evaluar el impacto de la parálisis del plexo braquial neonatal (BBPN) en la representación de la mano de orden superior.
Método
Se reclutaron 82 niños y adolescentes zurdos con y sin BBPN del lado derecho. Treinta y un participantes con BBPN (edad media [DE] 11 años 4 meses [4 años 4 meses]; rango de edad 6 años 2 meses – 21 años 0 meses; 15 mujeres; C5–6, n = 4, C5–7, n = 12, C5 – T1, n = 11, C5 – T1 con signo de Horner, n = 4) junto con 30 controles (edad media 11 años 5 meses [4 años 4 meses]; rango de edad 6 años 7 meses – 21 años 7 meses; 14 mujeres). Se evaluó el tamaño y la forma estimada de la mano de los participantes en la medida de la representación de la mano implícita y explícita. Se utilizó un modelo lineal mixto para investigar el efecto de la condición, el deterioro sensoriomotor y la edad.
Resultados
Los individuos con BBPN mostraron una diferencia significativa en la representación de la mano implícita entre las manos afectadas y no afectadas. El modelo lineal mixto confirmó una influencia significativa de la gravedad de la lesión sensitivomotora. Solo la representación implícita estimada de la mano se asoció con la edad, con una diferencia significativa entre los niños de 6 a 8 años y los de 9 a 10 años.
Interpretación
El efecto de la alteración sensoriomotora en la representación de la mano central en individuos con BBPN es específico debido a su componente implícito y se caracteriza por una subestimación de la longitud del dedo en la mano afectada en comparación con la subestimación característica en la mano no afectada. Ni el BBPN ni la edad afectaron la estimación manual explícita. Este estudio confirma la importancia de la contribución sensoriomotora al desarrollo de la representación implícita de la mano.
Abstract
ptOBJETIVO
Avaliar o impacto da paralisia neonatal do plexo braquial (PNPB) na representação de ordem superior da mão.
MÉTODO
Foram recrutadas 82 crianças e adolescentes canhotos com e sem PNPB do lado direito. Trinta e um participantes com PNPB (idade média [SD] 11 anos 4 meses [4 anos 4 meses]; faixa etária 6 anos 2 meses–21 anos 0 meses; 15 mulheres; C5–6, n=4, C5–7, n=12, C5–T1, n=11, C5–T1 com sinal de Horner, n=4) foram avaliados juntamente com 30 controles (idade média de 11 anos e 5 meses [4 anos 4 meses]; faixa etária de 6 anos 7 meses a 21 anos 7 meses; 14 mulheres). O tamanho e a forma estimados da mão dos participantes na medida da representação implícita e explícita da mão foram avaliados. Um modelo linear misto (MLM) foi usado para investigar o efeito da condição, deficiência sensório-motora e idade.
RESULTADOS
Indivíduos com PNPB apresentaram diferença significativa na representação implícita da mão entre as mãos afetadas e não afetadas. O MLM confirmou uma influência significativa da gravidade da lesão sensório-motora. Apenas a representação implícita estimada da mão foi associada à idade, com diferença significativa entre crianças de 6 a 8 anos e de 9 a 10 anos.
INTERPRETAÇÃO
O efeito do comprometimento sensório-motor na representação central da mão em indivíduos com PNPB é específico devido ao seu componente implícito e caracteriza-se pela subestimação do comprimento dos dedos na mão afetada em comparação com a característica subestimação na mão não afetada. Nem a PNPB nem a idade afetaram a estimativa de mão explícita. Este estudo confirma a importância da contribuição sensório-motora para o desenvolvimento da representação implícita da mão.
Abstract
enAbbreviations
-
- AHA
-
- Assisting Hand Assessment
-
- LMM
-
- Linear mixed model
-
- NBPP
-
- Neonatal brachial plexus palsy
What this paper adds
- Sensorimotor impairment in individuals with neonatal brachial plexus palsy (NBPP) affects implicit hand representation.
- The underestimation of implicit finger length changed with age in both control and NBPP groups.
- There is evidence of plasticity in implicit hand representation.
- Explicit hand shape was not affected by either NBPP or age.
- Forced and naturally left-handed individuals had similar hand shape estimations of the left hand.
Efficient and rapidly adaptive fine hand manipulations exemplify an accurate representation of hand size and shape in the brain. Spatial information about the limbs depends on input from the visual, proprioceptive, tactile, auditory, vestibular, and motor systems.1, 2 Multiple input signals are integrated into unified central hand representations that have both implicit and explicit components.3-5 While the explicit component is a conscious representation of the way the hand appears from the outside and is dominated by visual input, the implicit component covers a more unconscious representation, with predominant reliance on the integration of proprioceptive signals. Information recruitment from the different representations is weighted in proportion to the reliabilities within the context of a task.2, 6, 7 Central hand representations are tightly integrated with motor control systems.8 Motor control models hypothesize a continuous matching of information about the predicted hand position with estimates of current hand position using feedback from hand representations, such as a hand map of size and shape. In contrast to the explicit component, the implicit metric component of hand representation is misperceived systematically. Typically developing children and adults alike significantly underestimate their finger length and overestimate their hand width compared to their actual sizes.1, 5, 9-11 Despite a growing interest in the development of hand representations, studies focusing on the impact of sensorimotor impairment on central hand representation in a paediatric clinical context are scarce.12
Neonatal brachial plexus palsy (NBPP) is a birth injury to the brachial plexus with high heterogeneity in incidence, lesion extent, and severity.13 This injury affects a developing nervous system at a critical moment of sensorimotor development. Recovery of motor and sensory function in NBPP is attributed to axonal regeneration followed by original target reinnervation. Due to the developing and highly neuroplastic nervous system of infants, their axons can connect with end organs that differ from the original innervated end organ because of misrouting.14 This results in absent or inappropriate afferent input and defective motor unit recruitment.15 Sensorimotor deprivation or misconnection during the critical central maturation period can disturb the development of central motor programmes, leading to dyspraxia.16 NBPP provides a unique opportunity to test the influence of sensorimotor impairment present since birth on the development of a central hand representation in an intact central nervous system. A better understanding may provide new insights into early central reorganization after NBPP and empower initial interventional therapy strategies.
This case–control study explored the impact of NBPP on the implicit and explicit representation of the hand. In NBPP, the right hand is affected more often due to frequent left occiput anterior vertex presentation placing the right shoulder behind the pubic symphysis during labour. In contrast to an approximately 10% prevalence of left-handed or mixed-handed individuals in the general population, 76% of children with NBPP whose right side is affected are left-handed.17 To control the effect of handedness,5 we chose to include children with NBPP with left hand preference only and compare them with typically developing left-handed individuals.
Since visual information is predominant for the explicit component and proprioceptive information underpins the implicit component of hand representation, we hypothesized that the inappropriate afferent input and impaired motor output in children with NBPP are likely to impact the implicit but not the explicit representation of the affected hand. Consequently, atypical sensibility and strength in NBPP are hypothesized to have an adverse influence on implicit hand representation.
Considering that hand representation develops differently during childhood,5, 11 we predicted that age would influence implicit hand representation in participants with NBPP and controls, with reduced finger length underestimation in the youngest group.
METHOD
Study design
This case–control study was approved by the Medical Ethical Committee of Ghent University Hospital (no. B670201525721) and conducted at the multidisciplinary NBPP care unit of Ghent University Hospital Child Rehabilitation Centre (Belgium) between February 2016 and December 2018 (ClincialTrials.gov registration no. NCT04376372). The study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational studies. An a priori power and sample size calculation (v9.4) was performed for a difference in outcome between individuals with NBPP and controls on underestimation of finger length, based on α=025, a nominal power of 0.80, and equivalence bouts of +17 and −17 (based on SD=17.69 from the pilot study5). This yielded 28 individuals per group; considering a dropout rate of 15%, this yielded a required sample size of 24 individuals per group.
Participants
Participants with NBPP were recruited through the local database of Ghent University Hospital and via nationwide announcements to relevant health practitioners, schools, and youth and sport organizations. Eligibility criteria were: (1) right-sided NBPP (ICD-11 Mortality and Morbidity Statistics: KA44.Y); (2) left hand preference; (3) right-handed parents; (4) age between 6 and 21 years; (5) normal or corrected-to-normal vision.
Typically developing participants were recruited via announcements to relevant health practitioners, regular schools, youth organizations, and sport clubs, and personal acquaintances of colleagues. Inclusion criteria were: (1) left hand preference; (2) right-handed parents; (3) age between 6 and 21 years.
The main exclusion criterion for all participants was the presence of any (other) relevant locomotor, neurological, or psychiatric disorder.
A minimum age of 6 years was chosen to ascertain a clear understanding of test instructions. The age limit of 21 years was arbitrarily set to see how hand representation develops into young adulthood.
Directly or via their parents, written informed consent was obtained in accordance with the principles of the Declaration of Helsinki. All costs as a result of the study were reimbursed; participation effort was compensated by film tickets.
Procedure
The physical and rehabilitation medicine specialist and licensed child therapists from the NBPP care unit assessed participants according to a detailed protocol. Concerted effort was made to ensure that participants remained engaged throughout the testing procedure.
General characteristics
A questionnaire was used to register age, sex, handedness, medical history, medication intake, treatment history, school level and results, and leisure activities. Medical information was extracted from medical records if possible. A modified version of the Edinburgh Handedness Inventory18 was used to assess direction and degree of hand preference in 10 everyday activities, yielding a laterality quotient ranging from −100 (consistent left hand preference) to 100 (consistent right hand preference).
Sensory and motor evaluation
The Semmes–Weinstein monofilament basic kit (part no. A8352)19 was adopted to test pressure sensation in both hands on the dorsal and ventral sides (see Appendix S1, online supporting information, for a detailed description of the test). The results were condensed into five mean Semmes–Weinstein subscores corresponding to each finger, which were consequently binary-expressed as (a)typical. A score range of 2.83 to 3.60 was considered typical.20
Maximum isometric grip strength was measured bilaterally with the E-LINK Evaluation System (E-Link System Packages; Biometrics Ltd, Ladysmith, VA, USA). The software automatically calculates the average grip of three measurements. The grip strength ratio was calculated by dividing the average right by left grip strength.
The Bruininks–Oseretsky Test of Motor Proficiency, Second Edition21 was administered. For the purpose of this study, the running speed and agility and fine motor precision and integration subtests were analysed.
An electrodiagnostic investigation of the affected hand was performed in the group with NBPP by an experienced paediatric physician (RVDL). A CareFusion Nicolet electrodiagnostic system, with Synergy v20 software and 8-channel amplifier, was used (see Appendix S1 for a detailed description of the test). For the purpose of this study, the extent of nerve lesion was categorized in groups based on the Narakas classification.22 Presence of a Horner sign at birth was obtained from the medical files or parents’ anamnesis. The Assisting Hand Assessment (AHA), a video-based, standardized, and criterion-referenced test,23 was performed to quantify how effectively children with NBPP use their affected hand during bimanual play. The sum score was converted to interval logit measures called AHA units, ranging from 0 to 100, where a higher measure indicates higher ability. The test was evaluated by a certified scorer.
Implicit map of hand size: localization task
The procedure used was like that employed by Van der Looven et al.5 (Fig. 1a). Participants were seated and placed one hand palm down, aligned with the midline of their body, with fingers straight and slightly spread on the semi-transparent paper (Fig. 1b). The actual hand circumference was drawn on the paper by the researcher (Fig. 1b, inset). Subsequently, the participant’s hand was occluded by moving the middle plate. Participants were verbally cued to judge the location of 10 easily identifiable landmarks (in random order), indicating them on the white paper on top of the middle plate with their contralateral hand (Fig. 1c). The landmarks – the five knuckles and fingertips – were demonstrated and clearly named on the examiner’s hand before the start of the trial. The researcher marked the estimated landmarks on the white paper with an ultraviolet pen. Before and after each trial, a picture was taken without the occluding board. To ensure independent responses, participants moved their contralateral hand back to the original position between the two trials. The procedure was repeated twice for each hand.
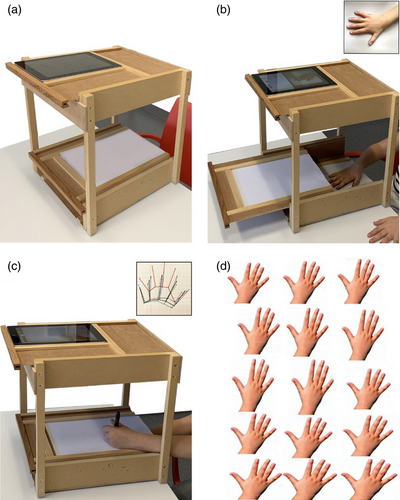
One examiner transferred the actual and estimated landmarks (two trials) on A4 graph paper using a light box and ultraviolet light, making the estimated marks visible. The actual hand map was constructed from the actual landmarks, while the estimated hand map was derived from the average (i.e. half the distance between each point) of the two estimated trials. The graph paper allowed precise distance measuring (Fig. 1c, inset) in millimetres. Data were normalized by expressing the estimated values of finger length and hand width as percentage overestimation as follows: 100 × ([average estimated length − actual length]/actual length). Note that a negative value means underestimation, whereas a positive value indicates overestimation.
Explicit hand shape: template selection task
The procedure used was like that employed by Van der Looven et al.,5 modelled on the method by Gandevia and Shegan.24 Four A4 sheets were created with 15 random images of the dorsum of the right hand (Fig. 1d). One of the images on each sheet resembled the normal proportions of an average-looking hand, while the other images were distortions of this image (seven images progressively 5% wider and seven images progressively 5% narrower). Each sheet was presented once to each participant who was asked to select the hand image that was most like the perceived shape of their own right hand. To ensure independence, one sheet at a time was presented after each localization test trial (localization test left hand/template selection task sheet 1/localization test right hand/template selection task sheet 2, and so on). From the four selected hand images, the average explicit hand shape index was calculated to assess hand shape. The shape index was defined as 100 × (hand width/length of index finger).
Cognition
The short form25 of the Wechsler Intelligence Scale for Children, Third Edition, using four subtests (picture completion, vocabulary, block design, and similarities), was used to calculate a full-scale IQ and was administered by a certified neuropsychologist. The subtest scores were transformed into derived IQs, based on the mean intercorrelations from the standardization sample.
Statistical analysis
All data were analysed using SPSS v26.0 (IBM Corporation, Armonk, NY, USA) with the significance level set at α<0.05. Reported p-values are two-tailed.
Participants with NBPP and controls were matched exactly for sex and running speed and agility. For age, the maximum difference was set at 8 months. A propensity score was applied to obtain a higher number of individuals with NBPP to be matched.
The study population is presented using descriptive statistics for clinical variables. Group differences were tested with an independent samples t-test for normally distributed (indicated by a Kolmogorov–Smirnov test) continuous variables; a Mann–Whitney U test was used for non-normally distributed continuous variables; a χ2 test was used for categorical variables.
Implicit hand representation data were addressed first. Principal component analyses for the finger length of all digits were performed for each hand to investigate the possibility of clustering in fewer components. The principal component analysis of actual finger length (including all fingers with equal weight) resulted in one component explaining 89.10% of the variance for the left and 92.27% of the variance for the right finger length respectively. Subsequently, percentage overestimation of finger length was averaged and introduced as a single variable in further analyses.
To account for missing data, confounding variables, and the collection of more than one data point from each participant across the same and different experimental conditions (dependency), a linear mixed model (LMM) was used with model selection based on the Akaike information criterion.26 Overestimation in percentage finger length and hand width was inserted separately as an outcome measure. The random effect specified the random intercept for each participant.
To answer the primary hypothesis, participant group and hand side were introduced as fixed factors. To investigate the effect of sensorimotor impairment, the Semmes–Weinstein monofilament test, lesion extent grouping, and AHA scores were selected as fixed factors in the LMM. Then, the explicit shape index was submitted to a univariate analysis of variance (ANOVA) with participant group as the fixed factor.
The second hypothesis was examined using age categories: (1) 6 to 8 years; (2) 9 to 10 years; (3) 11 to 16 years; (4) 17 to 21 years, with age as a fixed factor in the LMM and univariate ANOVA. Age categorization was based on a previous study.5
For significant main effects and interactions, post hoc analyses were conducted using independent samples t-tests applying Bonferroni corrections for multiple comparisons.
RESULTS
Participants and behavioural data
Eighty-two individuals were assessed for eligibility (Fig. S1, online supporting information). Four did not meet the inclusion criteria, resulting in 78 participants completing the full assessment. The final sample for propensity score matching was 76 due to low-quality data for two individuals. Consequently, 31 participants with NBPP (mean age [SD] 11y 4mo [4y 4mo]; age range 6y 2mo–21y 0mo; 15 females; C5–6, n=4, C5–7, n=12, C5–T1, n=11, C5–T1 with Horner sign, n=4) were assessed along with 30 controls (mean age 11y 5mo [4y 4mo]; age range 6y 7mo–21y 7mo; 14 females). Descriptive statistics are reported in Table 1.
| Variables | Individuals with NBPP (n=31) | Controls (n=30) | Significance |
|---|---|---|---|
| Male/female, n (%) | 16 (52)/15 (48) | 16(53)/14 (47) | 0.893a |
| Age (y:mo) | 9:8 (7:6–16:3) | 9:10 (7:8–16:0) | 0.896b |
| Derived IQ | 98.30 (12.71) | 110.56 (12.44) | <0.001 c |
| EHI (%) | −74.79 (20.05) | −55.41 (42.17) | 0.137c |
| BOT-2 (n) | |||
| Running speed and agility 1/2/3 | 0/0/31 | 0/0/30 | N/A |
| Fine motor precision 1/2/3 | 8/22/1 | 5/23/2 | 0.394d |
| Fine motor integration 1/2/3 | 13/18/0 | 7/22/1 | 0.031 d |
| Actual finger length (cm) | |||
| Right hand | 6.2 (5.2–6.8) | 6.05 (5.12–7.05) | 0.817b |
| Left hand | 6.36 (0.97) | 6.28 (1.22) | 0.772c |
| Grip strength | |||
| Ratio | 0.70 (0.35–0.87) | 1.06 (0.86–1.27) | 0.001b |
| Semmes–Weinstein monofilament test atypical/typical (n) | |||
| Digit I left hand | 0/31 | 0/29 | N/A |
| Digit I right hand | 5/26 | 0/29 | 0.001 d |
| Digit II left hand | 1/30 | 0/29 | 0.4964 |
| Digit II right hand | 6/25 | 0/29 | 0.000 d |
| Digit III left hand | 2/29 | 0/29 | 0.1204 |
| Digit III right hand | 5/26 | 0/29 | 0.001 d |
| Digit IV left hand | 1/30 | 1/28 | 1.0004 |
| Digit IV right hand | 5/26 | 0/29 | 0.001 d |
| Digit V left hand | 0/31 | 0/29 | N/A |
| Digit V right hand | 5/26 | 0/29 | 0.001 d |
| Pattern of atypical Semmes–Weinstein monofilament test right hand, n (%) | |||
| Digits I, II, and III | 1 (17) | ||
| Digits II, IV, and V | 1 (17) | ||
| All fingers | 4 (66) | ||
| Lesion level, n (%) | |||
| C5–C6 | 4 (13) | ||
| C5–C7 | 12 (39) | ||
| C5–T1 | 11 (35) | ||
| C5–T1 + Horner | 4 (13) | ||
| Primary nerve surgery (yes/no), n (%) | 10 (32)/21 (68) | ||
| Secondary upper extremity surgery (yes/no), n (%) | 18 (58)/13 (42) | ||
| SNAP right atypical/typical (n) | |||
| Digit I right hand | 13/18 | ||
| Digit II right hand | 11/20 | ||
| Digit III right hand | 8/23 | ||
| Digit IV right hand | 8/23 | ||
| Digit V right hand | 3/28 | ||
| Atypical SNAP right hand, n (%) | 17 (55) | ||
| Pattern of atypical SNAP right hand, n (%) | |||
| Digit I | 4 (23) | ||
| Digits I and II | 3 (18) | ||
| Digits I, II, and IV | 2 (12) | ||
| Digits II, III, and IV | 2 (12) | ||
| All fingers | 2 (12) | ||
| Other combinations | 4 (23) | ||
- Bold type indicates statistical significance. aχ2 test. bMann–Whitney U test. cIndependent samples t-test. dFisher’s exact test. Data are presented as the mean (SD) except for the Mann–Whitney U test (presented as the median [25th–75th centile]). NBPP, neonatal brachial plexus palsy; EHI, Edinburgh Handedness Inventory; BOT-2, Bruininks–Oseretsky Test of Motor Proficiency, Second Edition; N/A, not applicable; SNAP, sensory nerve action potential.
Unlike the scores for the Bruininks–Oseretsky Test of Motor Proficiency, Second Edition, Edinburgh Handedness Inventory, and actual finger length, a significant difference was found for derived IQ, ratio grip strength, and Semmes–Weinstein monofilament test scores of individuals with NBPP compared to controls. According to the Semmes–Weinstein monofilament test, a significant difference was found for each finger of the right hand between participants with NBPP and controls but not for the left hand.
Experimental tasks
The results of percentage overestimation and shape index are presented in Table S1 (online supporting information). The mean (SD) underestimation of finger length was −20.31% (21.15) for the left and −19.90% (22.04) for the right hand in controls versus −28.83% (21.53) for the left and −16.20% (28.58) for the right hand in individuals with NBPP. The mean (SD) overestimation of hand width was 36.80% (29.92) for the left and 38.58% (33.95) for the right hand in controls versus 23.82% (25.48) for the left and 32.33% (29.09) for the right hand in participants with NBPP. For percentage underestimation of finger length, but not for hand width, the LMM revealed a significant group-hand side interaction (F=5.298; df=58.242; p=0.025; Fig. 2a), with a significant difference (p=0.001) between left- and right-hand side in the group with NBPP. Exploring the sensory outcome measurements, the Semmes–Weinstein monofilament test score of the right index finger correlated most strongly with the Semmes–Weinstein monofilament test score of the other digits. After insertion of the Semmes–Weinstein monofilament test score of the right index finger as a fixed factor, the group-hand side-Semmes–Weinstein monofilament test interaction was significant (F=8.403; df=55.458; p=0.001). In the group with NBPP, percentage overestimation of right finger length was significantly different (p<0.01) between individuals with typical (−26.09%) and atypical Semmes–Weinstein monofilament test scores (10.83%). Logically, individuals with NBPP with an atypical Semmes–Weinstein monofilament test score of the index finger showed a significantly different (p<0.01) percentage finger length underestimation between left and right hands (−24.23% vs 10.83%; Fig. 2b). The analysis revealed no significant differences between individuals with NBPP and controls for typical index Semmes–Weinstein monofilament test scores. To explore the effect of sensorimotor lesion severity, lesion extent and AHA logits were introduced as fixed factors. LMM analysis revealed a hand side-lesion extent interaction effect (F=2.593; df=26.490; p=0.041), with a significant difference (p<0.01) in percentage underestimation of right-sided finger length (−5.80%) compared to left-sided finger length (−53.65%) in lesion extent in the C5–T1 with Horner sign group. A main effect of AHA (F=4.285; df=26; p=0.049) on percentage underestimation of finger length (Fig. 2c) was found.
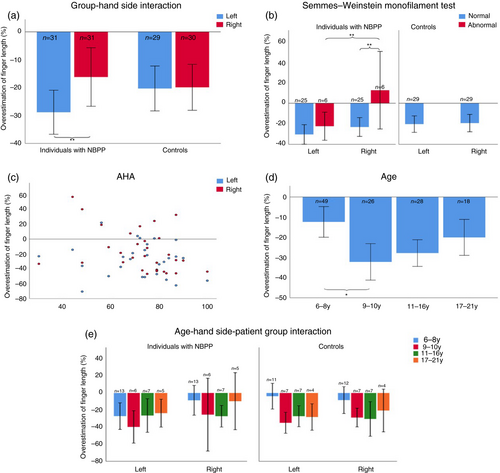
Univariate ANOVA of explicit hand shape did not reveal a main effect of the population group (p=0.860).
Second, the insertion of age as a fixed factor in the LMM showed a significant main effect of age (F=3.352; df=55.677; p=0.025) on implicit percentage underestimation of finger length but not on percentage hand width. Post hoc analysis revealed significantly (p<0.001) less percentage underestimation of finger length for the youngest (5–8y) compared to the second youngest age group (9–10y): −12.59 versus −32.29% (Fig. 2d,e). Univariate analysis showed that age has no influence on explicit hand shape (p=0.619).
DISCUSSION
This study examined, for the first time, the role of inappropriate afferent input and impaired motor output in children and young adults with NBPP, and their the development of implicit and explicit hand representation.
Reported misperceptions of implicit hand metrics were replicated,1, 5, 9-11 with a systematic mean underestimation of actual finger length and a substantial overestimation of hand width for both groups. Interestingly, the affected hand in individuals with NBPP showed significantly less finger length underestimation compared to the non-affected hand. In contrast, the control group did not show any difference between hands (Fig. 2a). As for the potential mechanism underlying this representational difference in individuals with NBPP, a modulatory effect by afferent and motor information, as suggested earlier,27 can be assumed. To test this, we examined the impact of sensory impairment by evaluating the effect of Semmes–Weinstein monofilament test scores on implicit finger length. Regarding the affected hand in individuals with NBPP, a significant difference in misperception was found between individuals with typical and atypical pressure sensation: actual finger length was overestimated by 10.83% in the presence of an atypical Semmes–Weinstein monofilament test score. In contrast, atypical sensation in the non-affected hand did not influence implicit hand representation and was comparable to the implicit hand metrics of participants with NBPP and controls with typical pressure sensation (Fig. 2b). These results are consistent with studies where cutaneous anaesthesia of a body part led to an immediate increase in its perceived size.24, 28 The functional link between somatosensory input and stereotyped, modality-specific distortions in the primary sensory cortex is well established.29 However, less is known about the interdependence of sensory feedback on somatosensory perception. A hierarchy has been proposed extending from primary somatosensory sensation to somatosensory perception and finally somatosensory representation.1 Somatosensory sensation is a necessary condition for somatosensory perception. Our data underscore the importance of typical sensory input to implicit hand map development. In addition to sensory loss, NBPP often causes negligence of the affected hand, delayed learning of new motor tasks, which leads to additional progressive loss of sensorimotor interaction and activity-dependent changes in the central nervous system, resulting in more functional disability in coordinated, goal-oriented motor behaviour.
The impact of sensorimotor lesion severity was explored by grouping lesion extent. Implicit finger length representation in the C5–T1 with Horner sign group showed significantly less underestimation in the affected compared to the non-affected hand, although the group was small, resulting in higher standard SDs. Notably, the specificity30 and timing of electrodiagnostic investigations could partly be responsible for the higher prevalence of C5–C7 and total palsies compared with previous studies.22, 31
The influence of functional hand use on implicit hand metrics was demonstrated by the main effect in AHA: a higher AHA score corresponded to a smaller finger length implicit representation in most participants with NBPP. Unfortunately, since AHA units are a continuous measure, exploratory post hoc analysis could not be performed. Nevertheless, these results point to the modulatory effect of higher manual ability, where more specific sensorimotor information is gained on the perceived hand size.
As hypothesized, the explicit metric component of hand representation was not affected by NBPP. Interestingly, experiments manipulating the explicit body representation, for example, by visual distortion, have been shown to modulate basic somatosensory sensation32, 33 and tactile size perception of those body parts.34 Looking at a body part can enhance tactile acuity in that body part, even in pathological conditions with somatosensory impairment.32, 35 Areas of the somatosensory cortex are more active when an object is perceived tactilely and visually at the same time,36 suggesting that both visual and tactile information inform the perception of tactile spatial resolution.
The second hypothesis supposed an influence of age on implicit but not on explicit hand size representation. Indeed, significantly less misperception in the youngest group (6–8y) compared to the next age category (9–10y) was demonstrated for individuals with NBPP and controls (Fig. 2d,e). This age effect has been previously demonstrated in typically developing children5, 11 but not yet in a paediatric clinical context. Non-linear maturation is the result of accelerated improvement of proprioceptive ability, peaking around 8 to 10 years but continuing throughout adolescence.37, 38 Furthermore, a rather late (after the age of 8y) cross-sensory integration7 has been attributed to the continuous need for recalibration of the diverse sensory systems involved with spatial perception during growth. Additionally, although it should be interpreted with caution because of the small and unequally balanced number of participants across age categories, our data hint at a different developmental trajectory between participants with NBPP and controls (Fig. 2e). The impaired sensorimotor experience in the affected hand of children with NBPP seemed to cause less underestimation and less adaptation across all age categories. In contrast, the non-affected hand, which is used more unilaterally at a young age in individuals with NBPP, shows a tendency of earlier development towards the final expected value of finger length underestimation. Mirroring previous findings in typically developing children and adults, the explicit estimation of hand shape, measured by a template selection task, was not influenced by age. Since visual information constitutes the first sensory reference frame for explicit hand representation, this result was expected. Together with previous results,5, 35 our data confirm the possibility that explicit hand representation develops early in life, while implicit hand representation adjusts continuously through development as the hand grows and its sensorimotor experiences change profoundly.
The traditional view of NBPP as a problem of decreased ‘motor output’ with minimal sensory deficits is hereby challenged. It is important to note that peripheral nerve injury leads to deficits in the use of sensory feedback, thereby compromising motor function.39 Our study adds to this insight through the impact of a sensorimotor lesion at birth on the development of implicit hand mapping. The implicit hand map, for instance, mediates tactile registration and perception. Early in life, tactile localization and cross-modal orienting to tactile stimulation develop together with the motor schemas that underlie peripersonal exploration to integrate with goal-directed grasping behaviour.40 The misperception found in our study could impact on haptic ability, dextral performance, and everyday hand function. Problems with calibrating grasp and locating perceived stimuli can thus be expected.
Limitations and perspectives
Although both groups were recruited via similar information channels, a significant difference was found in derived IQ that could be attributed to sampling bias. For the group with NBPP, sampling bias is suspected since our sample represented a rather high percentage of lesion extent in the C5–T1 group (35%) and the C5–T1 with Horner sign group (13%), with a consequently higher percentage (32%) of children undergoing primary nerve surgery (Table 1). This bias does not affect the research question but suggests caution for future comparison of study results in NBPP.
Naturally, assessing individuals during the developmental period poses many challenges. Age, cognition, and attention capacity may have affected performance in our test battery. For this reason, Peters and Goldreich41 recommended against including tests from 6- and 7-year-old groups requiring tactile demanding tasks. However, an exploratory sensitivity analysis that excluded this age group did not affect our results.
Sample size imbalance among different age categories and lesion severity groups, together with the small number of participants in some subcategories, limits the wider applicability of the post hoc analyses. Nevertheless, this limitation does not affect the answers to the primary research questions. Beyond this recognition, potential applications to influence or circumvent these limitations in future systematic and large-scale studies are available.
CONCLUSION
Our results confirm the complex formation of different higher-order hand representations with the metric component of hand representation affected at the implicit, but not explicit, level in left-handed children and young adults with right-sided NBPP.
Crucially, the study emphasizes the dominant contribution of both sensory and motor impairment in NBPP to the central reorganization of implicit hand mapping. These activity-dependent changes in the young central nervous system may deteriorate the motor control ability of the hand.
Although maximization of peripheral motor and sensory nerve recovery is a primary goal in children with NBPP, new insights in plastic central reorganization are vital to empower early interventional treatment designs aimed at maintaining a typical unified hand representation with an effect on affected hand use.
ACKNOWLEDGMENTS
The authors thank all the children and their parents for their voluntary study participation. We thank the therapists of the Child Rehabilitation Centre at University Hospital Ghent for performing the testing and Miguel Deschrijver for his help as part of his research report for the Master of Medicine in Medicine. This study is funded by a clinical research grant (no. HA/RP/2017/004 dd 19/12/16) from Ghent University Hospital. The funding source was not involved in study design, data collection, data analysis, data interpretation, writing of the manuscript, or the decision to submit it for publication. The authors certify that there are no conflicts of interest with any financial organization regarding the material discussed in the manuscript.