Gastric volvulus related to upside-down stomach that was successfully treated by endoscopic repositioning
Abstract
Watch a video of this article
BRIEF EXPLANATION
Upside-down stomach (UDS) is the rarest type of hiatal hernia (<5%). It is characterized by herniation of the entire stomach or most gastric portions into the posterior mediastinum.1 UDS is associated with a risk of incarceration as well as volvulus, and these complications may cause gastric bleeding, ischemia, and perforation.2 Endoscopy is a necessary initial step for gastric volvulus to select the optimal treatment strategy, and endoscopic repositioning is often effective.3 We encountered a patient with gastric volvulus related to UDS that was successfully treated by endoscopic repositioning.
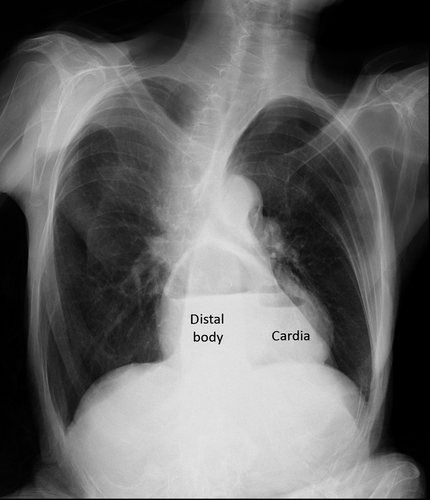
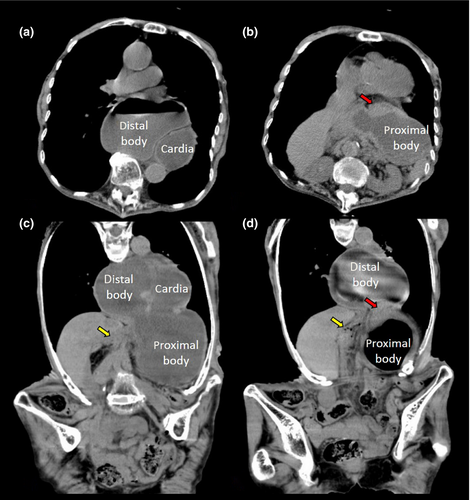
An 82-year-old female with a kyphotic spine presented to our hospital with continuous vomiting from the previous day. Upright chest radiography showed a dilated stomach with an air fluid level in the mediastinum (Fig. 1). Computed tomography (CT) revealed migration of the antrum and body of the stomach into the mediastinum. The body and cardia of the stomach were dilated, while the antrum of the stomach and the duodenum had collapsed (Fig. 2). Based on these findings, we diagnosed the patient with UDS with mesenteroaxial volvulus. After decompression of the stomach by a gastric tube, we attempted endoscopic repositioning of the stomach. Esophagogastroduodenoscopy showed circumferential erosion in the lower esophagus without ischemic changes. The body of the stomach was dilated, while the antrum of the stomach and the duodenum had collapsed. After inserting the endoscope into the descending part of the duodenum, we pulled it with counterclockwise rotation. Endoscopic repositioning was successful without complications (Video S1). Prophylactic treatments, such as the laparoscopic repair of hernias and gastropexy, were not selected because this was the first time the patient had developed gastric volvulus related to UDS and her general condition was poor. After the treatment, the patient’s symptoms resolved. At the 20-month follow-up, she was alive with no recurrence.
Authors declare no conflicts of interest for this article.