Multicenter study of autoimmune gastritis in Japan: Clinical and endoscopic characteristics
Abstract
Background and Aim
In Japan, the prevalence of autoimmune gastritis (AIG) is assumed to be very low. With the recent rapid decrease in Helicobacter pylori (Hp) prevalence, reports on AIG are increasing. This multicenter registry study aimed to clarify the characteristics of AIG, especially its endoscopic appearance.
Methods
A total of 245 patients with AIG from 11 institutions in Japan from January 2010 to October 2016 were included, and their clinical and endoscopic findings were evaluated.
Results
Mean age was 67.2 ± 11.4 years, and 63.7% of the participants were women. The most common approach to diagnose AIG was endoscopic examination. Repeated incorrect treatment for Hp infection, due to a false-positive result in 13C-urea breath test, ranked third among the basis for diagnosis of AIG. Associated gastric lesions were type 1 neuroendocrine tumor (11.4%), adenocarcinoma (9.8%), and hyperplastic polyps (21.1%). Corpus pan-atrophy was the most common appearance (90.1%); however, remnant oxyntic mucosa was found in 31.5% of the patients (flat, localized type, 48.6%). Sticky adherent dense mucus and scattered minute whitish protrusions were also observed in approximately 30% of the patients. Despite the prevailing presumption of the antral mucosa remaining normal, 42.3% of the patients presented with various extents of atrophy, and patchy redness and circular wrinkle-like patterns were both observed in approximately 20% of the patients.
Conclusions
The present study showed some prominent clinical characteristics and endoscopic findings of AIG. We believe that our study will facilitate the diagnosis of potential AIG.
Introduction
Autoimmune gastritis (AIG) is a subtype of chronic gastritis.1 Strickland and Mackay2 were the first to describe AIG, which is characterized by autoimmunity to parietal cells leading to oxyntic mucosa-restricted inflammation and atrophy, resulting in hypergastrinemia. AIG and its clinical manifestation, pernicious anemia, were once reported to be dominant in elderly women of northern European ethnicity;3, 4 however, subsequent studies have indicated that there appears to be no racial specificity but considerable diversity in age at clinical presentation of illness.5, 6 Moreover, a recent survey7 showed that gastric dysbiosis associated with modern improved sanitation could cause a relatively increased AIG risk.
In Japan, the prevalence of AIG was assumed to be very low until about a decade ago.8 However, possibly on the background of a recent dramatically rapid decrease in Helicobacter pylori (Hp) prevalence,9 reports on AIG are increasing.10, 11 This multicenter registry study aimed to clarify the characteristics of AIG in Japan and explore its endoscopic appearances.
Methods
- Endoscopic corpus predominantly severe atrophic gastritis;
- Presence of anti-parietal cell antibody (PCAb), or anti-intrinsic factor antibody (IFAb), or pernicious anemia; and
- Hypergastrinemia (>350 pg/mL).
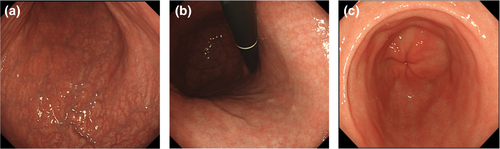
“Endoscopic corpus predominantly severe atrophic gastritis” was defined as discolored mucosa with marked vascular visibility observed not only on the lesser curvature, but also on the entire area of the greater curvature of the corpus along with the disappearance of folds without an atrophic border,12 which is called O-p (or O-4) atrophy (Fig. 1a,b), accompanied by non- or less-atrophic patterns in the antrum (Fig. 1c). In addition, cases with open type12 other than O-p or patchy distribution of corpus atrophy were included when obvious non- or less atrophic antrum was seen.
Pernicious anemia was defined as vitamin B12 (VB12) <233 pg/mL, mean corpuscular volume (MCV) >80 fl, and hemoglobin (Hb) <13.0 g/dL (male) or 11.4 g/dL (female).
Diagnosis of AIG was established when all three criteria were met.
Patient data
Patients were tested for pepsinogen (PG) 1, 2, and 1/2, Fe, VB12, blood cell count, anti-thyroglobulin antibody (TGAb), and anti-Hp IgG antibody (HpAb). We used E-Plate EIKEN HpAb (Eiken Chemical Co., Ltd, Tokyo, Japan) with a standard cut-off titer of 10 U/mL. Medical records of each patient were reviewed to identify a clue to diagnosis of AIG. Concomitant diseases and associated gastric lesions, such as adenocarcinoma, adenoma, hyperplastic polyp, and neuroendocrine tumor (NET), were evaluated.
Assessment of endoscopic appearance
Corpus assessment included degree of atrophy, remnant oxyntic mucosa, mucus property, and scattered minute whitish protrusions (SMWP). Extent of the normal mucosa and mucosal patterns and local findings in the antrum were assessed.
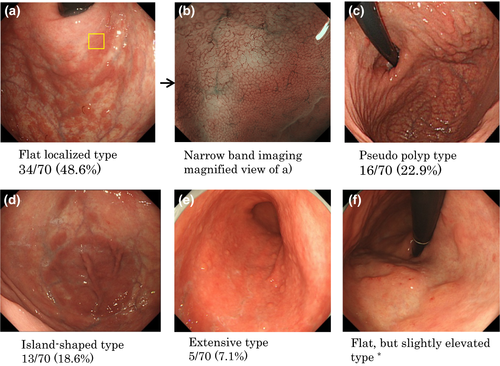
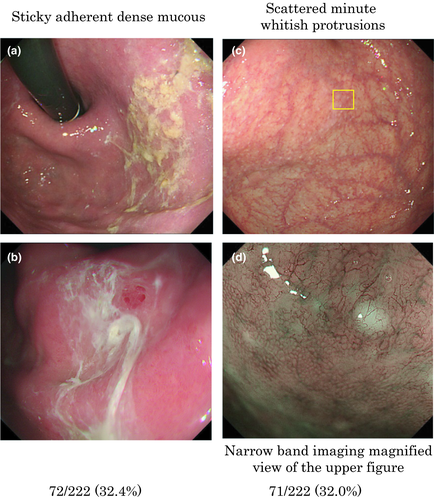
Remnant oxyntic mucosa was defined as normally colored and smooth surface patterns of oxyntic mucosal areas contrasted by the surrounding discolored atrophic mucosa (Fig. 2). Shapes of the remnant oxyntic mucosa were also evaluated. Sticky adherent dense mucus showed a denser creamy white-yellowish color and firmly adhered to the mucosa (Fig. 3a,b). SMWP was defined as minute hemispherical whitish protrusions scattered in the corpus mucosa (Fig. 3c), which were covered by epithelial capillaries (Fig. 3d). Magnified narrow-band imaging (NBI) method was not necessarily applied to all patients; however, it was adopted when the endoscopists felt the need for thorough observation.
For assessment of interobserver agreement, endoscopic images were assigned to three endoscopists (S.T., S.S., and R.A.), and they re-evaluated the images independently under the condition that they did not assess the images obtained in the endoscopic examination by himself or herself. Kappa values for identification agreement between the endoscopist and the evaluator were calculated using R 3.5.2 meta package (R Core Team [2018]). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria; https://www.R-project.org/).
Histological assessment
Histological gastritis was evaluated by biopsy sampling from the antrum and the greater curvature of the corpus according to the updated Sydney System,13 and neuroendocrine cell abnormality was also evaluated. Scores of the inflammation and atrophy grading were based on the visual analog scale indicated in the updated Sydney System, which were converted as normal, 0; mild, 1; moderate, 2; and marked, 3. This study was registered as UMIN000033785 and approved by the ethical committees of each participating institution.
Results
Number of subjects enrolled from each institution (institution number shown in parentheses) was as follows: 49 (1), 47 (2), 30 (3), 28 (5), 29 (6), 14 (7), 12 (8) 10 (4), 8 (9), 2 (10), and 16 (11). [Correction statement added on 10 October 2019, after first online publication: Institution numbers in parentheses have been corrected to reflect the order of author affiliations on the first page of this article.]
Clinical characteristics
Numbers of patients who underwent examinations for the following parameters were as follows: HpAb, 218; gastrin, 245; PG, 155; PCAb, 223; IFAb, 142; Fe, 90; VB12, 133; Hb and MCV, 202; and TGAb, 64. The main clinical and laboratory characteristics are listed in Table 1. The subjects were predominantly women and the elderly. In this study, 7.8% (17/218) were positive for anti-Hp Ab. Mean serum gastrin levels were very high and levels varied extensively. Decreased PG 1 levels and very low PG 1/2 ratio were also observed. With regard to anemia, pernicious anemia accounted for 39.1% of cases (52/133), and iron deficiency anemia accounted for 6.5% (13/199).
| Assessment type, n | |
|---|---|
| Age | 67.25 ± 11.4 (mean ± SD) |
| Male/female | 89/156 |
| Helicobacter pylori positive† (n = 218) | 17 (7.8%) |
| Gastrin (pg/mL; n = 245) | 2845 ± 2234 (mean ± SD) |
| Pepsinogen 1 (n = 152) | 8.24 ± 9.90 (mean ± SD) |
| Pepsinogen 2 (n = 152) | 9.53 ± 4.65 (mean ± SD) |
| Pepsinogen 1/2 ratio | 0.88 ± 0.69 (mean ± SD) |
| Anti-parietal cell Ab (n = 223) positive | 202 (90.6%) |
| Anti-intrinsic factor Ab (n = 142) positive | 72 (50.7%) |
| Pernicious anemia (n = 133) positive | 52 (39.1%) |
| Iron deficiency anemia (n = 199) positive | 13 (6.5%) |
| Anti-thyroglobulin Ab (n = 64) positive | 34 (53.1%) |
- †Hp-positive status is defined as Hp immunoglobulin G Ab >10 U/mL.
- Ab, antibody.
Detection of autoimmune gastritis
Medical records sufficient to identify the first clue to the diagnosis of AIG were obtained from 186 patients, and Table 2 presents these clues. The most common clue for AIG diagnosis was endoscopic appearance (58/186, 31.2%). Repeated incorrect treatment for Hp infection due to false-positive result in the 13C-urea breath test (13C-UBT) was seen in 28/186 patients (15.1%). (“Repeated” was defined as receiving treatment for Hp infection more than twice.)
| n (%) | |
|---|---|
| Endoscopic appearance | 58/186 (31.2) |
| Macrocytic anemia | 30/186 (16.1) |
| Repeated incorrect treatment for Hp due to 13C-UBT false positivity† | 28/186 (15.1) |
| Lower pepsinogen 1, 1/2 level & negative for Hp IgG Ab | 12/186 (6.5) |
| NET type 1 | 10/186 (5.4) |
| Health check-up endoscopy | 9/186 (4.8) |
| Iron deficiency anemia | 3/186 (1.6) |
| Screening barium fluoroscopy | 1/186 (0.5) |
- †13C-UBT positive was as <2.5‰.Ab, antibody; 13C-UBT, 13C-urea breath test; Hp, Helicobacter pylori; IgG, immunoglobulin G; NET, neuroendocrine tumor.
Concomitant diseases
Of the 245 patients, 55 cases were detected to be concomitant with other autoimmune diseases. Chronic thyroiditis with Ab to thyroglobulin (26/55; 47.2%) was the most common, followed by hyperthyroidism and other thyroid diseases (12/55; 21.8%). Other autoimmune diseases were observed in 17/55 (30.9%) patients.
Associated gastric lesions
Associated gastric lesions were evaluated in all 245 subjects, and abnormal lesions were found in 106 patients. Twenty-eight patients (11.4%) had type 1 NET and 24 (9.8%) had adenocarcinomas. Two patients had adenoma. Hyperplastic polyps were detected in 52/245 (21.2%) patients (Table 3).
| Diagnostic yield | n (%) |
|---|---|
| NET type 1 | 28/245 (11.4) |
| Adenocarcinoma | 24/245 (9.8) |
| Stage: early/advanced | 22/2 |
| Histology: intestinal/diffuse | 19/5 |
| Adenoma | 2/245 (0.8) |
| Hyperplastic polyp | 52/245 (21.2) |
- NET, neuroendocrine tumor.
Endoscopic appearance
Of the 245 cases, the endoscopic images of 222 cases were assessed including interobserver agreement for each endoscopic finding.
Corpus-dominant advanced atrophy was the most common endoscopic appearance (Fig. 1). With respect to the degree of atrophy, type O-p was the most commonly observed (200/222, 90.1%). A few patients presented slightly less atrophic patterns (O1, O2, or O3 type; 13/222, 5.9%; Table 4).
| (%) | |
|---|---|
| Degree of atrophy (atrophic border) | |
| O1–O3 | 13/222 (5.9) |
| O4 (O-p) | 200/222 (90.1) |
| Indeterminable | 9/222 (4.1) |
| Corpus | |
| Remnants of oxyntic mucosa | |
| Present | 70/222 (31.5) |
| Absent | 145/222 |
| Indeterminable | 7/222 |
| Shapes of remnants of oxyntic mucosa | |
| Flat, localized | 34/70 (48.6) |
| Pseudopolyp like | 16/70 (22.9)† |
| Island-shaped | 13/70 (18.6) |
| Extensive | 5/70 (7.1) |
| Granular | 2/70 (2.9) |
| Sticky adherent dense mucus | |
| Present | 72/222 (32.4) |
| Absent | 149/222 |
| Indeterminable | 1/222 |
| Scattered minute whitish protrusions | |
| Present | 71/222 (32.0) |
| Absent | 148/222 |
| Indeterminable | 3/222 |
| Antrum | |
| Extent of normal mucosa | |
| Whole area: normal | 97/222 (43.7) |
| Around half of the antrum | 19/222 (8.6) |
| Only adjacent to pylorus | 54/222 (24.3) |
| Whole area: discolored | 21/222 (9.5) |
| Whole area: reddish | 29/222 (13.1) |
| Indeterminable | 2/222 |
| Mucosal patterns and local findings | |
| Patchy redness | 49/222 (22.1) |
| Circular wrinkle-like pattern | 49/222 (22.1) |
| Red streak | 23/222 (10.4) |
| Raised erosion | 8/222 (3.6) |
| Absent of the above four | 88/222 |
| Indeterminable of the above four | 5/222 |
- †Four cases with pseudopolyp-like type included two cases accompanied by flat-localized type and two cases with island-shaped type.
Remnant oxyntic mucosa was found in 70/222 (31.5%) patients. This finding was categorized into five types based on their shapes as follows: flat localized (with various shapes, Fig. 2a), pseudo-polyp (Fig. 2c), island-shaped (flat, laterally spreading, Fig. 2d), extensive type (Fig. 2e), and granular type, and these were detected in 34/70 (48.6%), 16/70 (22.9%), 13/70 (18.6%), 5/70 (7.1%), and 2/70 (2.9%) cases, respectively. The flat but slightly elevated type (Fig. 2f) was categorized as a flat localized type. A magnified NBI view of the flat type (Fig. 2b) showed normal or nearly normal oxyntic mucosal pattern.
Sticky adherent dense mucus (Fig. 3a,b) was found in 72/222 (32.4.0%). In addition, Hp IgG Ab with sticky adherent dense mucus was positive only in 2/72 (2.8%) patients. SMWP was found in 71/222 (32.0%) patients.
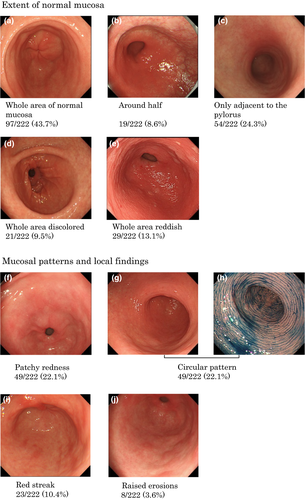
As to extent of normal coloration of antral mucosa, the following five categories were identified: whole area (97/222, 43.7%, Fig. 4a), around half (19/222, 8.6%, Fig. 4b), only adjacent to the pylorus (54/222, 24.3%, Fig. 4c), none (whole area was discolored; 21/222, 9.5%, Fig. 4d), and whole area being reddish (29/222, 13.1%, Fig. 4e). With regard to the local findings in the antrum, patchy redness (49/222, 22.1%, Fig. 4f), circular wrinkle-like pattern (49/222, 22.1%, Fig. 4g,h), red streak (23/222, 10.4%, Fig. 4i), and raised erosions (8/222, 3.6%, Fig. 4j) were also detected.
Kappa values for identification of agreement of each endoscopic finding were as follows: 0.705, degree of atrophy; 0.780, remnant of the oxyntic mucosa; 0.724, sticky adherent dense mucus; 0.604, SMWP; 0.314, extent of normal coloration of the antrum; 0.620, patchy redness in the antrum; 0.616, circular wrinkle-like pattern in the antrum; 0.749, red streak in the antrum; 0.656, raised erosions in the antrum.
Pathological characteristics
Biopsy sampling to evaluate histological gastritis was carried out in 162 patients, and evaluation of neuroendocrine cell abnormality was done in 139 patients. Histological scores of inflammation in the antrum and corpus greater curvature were 0.41 ± 0.51 (mean ± SD) and 0.63 ± 0.75, respectively. Atrophy scores in the antrum and corpus greater curvature were 1.00 ± 0.89 and 2.29 ± 0.91, respectively. Both advanced oxyntic gland atrophy (atrophy score: 3) and pyloric gland preservation (atrophy score: 0) were observed in 132/162 (82.0%) patients. Intraglandular enterochromaffin-like cell (ECL) hyperplasia was detected in 103/139 (74.1%), and extraglandular endocrine cell micro nest (ECM) was detected in 89/139 (64.0%) patients.
Discussion
As large-scale surveys on AIG have not been conducted in Japan, no comprehensive data on AIG in Japan are available. To our knowledge, this study is the first to examine the characteristics of AIG in Japan. Another notable strength of the present study is that all patients underwent detailed endoscopic examinations.
Similar to the results in Western and other Asian countries,5, 14 the results of this study showed that AIG is dominant in women and in the elderly. Findings of decreased PG 1 levels and very low PG 1/2 ratio also corresponded to a previous study.15 The prevalence of pernicious anemia (39.1%, 52/133) was consistent with that of the previous reports,16, 17 and the lower prevalence of iron deficiency anemia (6.5%, 13/199) in our older cohort (67.5 years) was also in accordance with that of the latter report.17 The association between Hp infection and AIG has been discussed previously;18-20 however, the prevalence of the coexistence of the two has not been clarified. The result that 7.8% (17/218) of patients were positive to the anti-Hp IgG Ab test is apparently low, considering the persistently high prevalence of Hp infection in the elderly in Japan.
Diagnosis of AIG typically depends on biopsy sampling that supplements other laboratory data or clinical manifestations.21 However, in the present study, endoscopic appearance was first considered as the basis for the diagnosis (58/186, 31.2%) prior to any other diagnostic features. An intriguing and newfound basis were the incorrect repeated treatments for Hp infection due to the false-positive results in 13C-UBT. Some of the patients who underwent treatment were considered to have been incorrectly classified as Hp-positive. A previous report11 suggested that proliferations of urease-positive bacteria other than Hp under non-acidic circumstances possibly resulted in positive 13C-UBT test results. Thus, such misclassification leads to unnecessary treatment for Hp.
Approximately one-quarter of the patients with AIG had concomitant autoimmune diseases and chronic thyroiditis was the most commonly observed (26/55, 47.3%). This manifestation corresponded to those of previous reports.22, 23
Autoimmune gastritis is associated with an increased risk of gastric cancer.24 One of the noteworthy findings of this study is that 9.8% (24/245) of the accompanying gastric lesions were noncardiac gastric adenocarcinoma; this incidence is higher than that in previous reports.25, 26 In one study27 of 257 patients with pernicious anemia, 15 (5.8%) had gastric cancer, which could be the highest reported rate in Japan prior to the present study. Type 1 NET is also one of the representative associated gastric lesions of AIG. The reported prevalence of type 1 NET in AIG varies. One review reported a prevalence of NET in AIG ranging from 5.2% to 11%.28 A histological survey conducted in the USA29 showed a NET prevalence of 9.97% and a Chinese study14 reported 4.37%. Our study presented a slightly higher prevalence (28/245, 11.4%) than those reports.
Contrary to the prevailing presumption regarding the endoscopic image of AIG,1 we showed various findings. First, the shapes and forms of the remnant unaffected oxyntic mucosa showed diversity, and the most common type was not the pseudo-polyp type, but the flat localized type (34/70, 48.6%). Some reports have referred to the pseudo-polyp lesions as a typical form of the remnant of the unaffected oxyntic mucosa.1, 30 However, there are few reports on whole images of the remnant oxyntic mucosa and those on the flat type are even fewer. As for the magnified NBI method on the pseudo-polyp type, one study31 suggested a pattern of closely arranged, small round pits clearly demarcated by a pattern of small round and oval pits. However, as shown in Figure 2b, a flat type showed gradual change in the pit patterns. Thus far, the present study is the first report presenting the whole image of the remnant oxyntic mucosa. Second, sticky adherent dense mucus is an intriguing and confusing finding. This appearance should be distinguished from the sticky mucus32 observed in currently Hp-positive gastric mucosa, which usually shows a whitish clouded pattern. One review30 presented an image and a brief description of the “mucus covering of the gastric mucosa” which appears similar to the sticky adherent dense mucus; however, no previous report focuses on mucus analysis. The low positivity of Hp in those with this mucus (2/72, 2.8%) may suggest the possibility that the mucus is closely related to urease-positive bacteria other than Hp in a non-acidic environment of AIG. Third, the finding of SMWP observed in 71 of 222 (32.0%) cases requires attention. This finding may have been similar to the “white globe appearance” referred to in the literature.33 However, because of the limited number of procedures in the magnified NBI method, details regarding the similarities and differences between SMWP and white globe appearance is beyond the scope of this study and warrants further investigation. Fourth, the endoscopic appearance of the antrum unexpectedly showed various atrophic patterns. Although 43.7% (97/222) showed whole normal (non-atrophic) pattern, 42.3% (94/222) were found to demonstrate various degrees of atrophy. With regard to the mucosal patterns and local findings in the antrum, the most common types were the patchy redness pattern and the circular wrinkle-like pattern (49/222, 22.1%, both). These two findings may be characteristic of AIG. Based on a PubMed search, there has been no report on antral endoscopic findings of AIG. Therefore, to the best of our knowledge, this is the first report on the endoscopic picture of the antrum. The obtained kappa values suggested that our endoscopic observation held almost satisfactory objectivity except for the extent of normal mucosa in the antrum.
Histological scores showed that inflammation and atrophy were more dominant in the greater curvature of the corpus than in the antrum; these results support the validity of our inclusion criteria. Contrary to the common knowledge of the absence of inflammation in the antral mucosa,34 mild to moderate inflammation and atrophy were seen. These results are partly in accordance with a histological study.35 Our findings also showed that intraglandular ECL hyperplasia was more common than extraglandular ECM formation.
This study had some limitations. First, it was a retrospective study and may have had a selection bias, which might have affected the number of patients with repeated Hp treatments and some endoscopic appearances. Various stages of AIG included at entry might affect the incidence rate of concomitant diseases and associated gastric lesions, especially the incidence of gastric cancer and type 1 NET. Second, diagnosis of Hp status was assessed by Hp IgG Ab only; therefore, estimation of the prevalence of associated Hp gastritis might have been lower than the actual prevalence. Third, endoscopic appearances were not supported by targeting histology. Further research is warranted to determine the histologic basis of various endoscopic findings in this study.
In conclusion, the present study introduced some prominent clinical and endoscopic characteristics. We believe that the newly unveiled endoscopic findings will facilitate the diagnosis of potential AIG and provide new insights to the study of gastritis.
Acknowledgments
This study was carried out in collaboration with CARP, and all authors are members of this group. Histological validity for AIG was supervised by Dr. Hidenobu Watanabe (Pathology & Cytology Laboratories: PCL Japan).
Conflicts of Interest
Authors declare no conflicts of interest for this study.