First human application of a flexible 3-D endoscope for gastrointestinal endoscopic submucosal dissection
Decades ago, rigid laparoscopy instrumented with 3-dimensional (3-D) view was introduced in minimally invasive surgery. Since then, there have been advancements in stereoscopic technology with implementation of higher resolution and illumination devices.1, 2 With the use of special glasses, modern 3-D technology allows the addition of depth perception to 2-D images taken with twin lenses and displayed on a 2-D monitor.2 In fact, 3-D-laparoscopy appears to improve performance with shortened operative time and reduced number of procedural errors or is at least non-inferior when compared to 2-D laparoscopy, as a result of its secure appreciation of depth.1 In addition, 3-D visualization can provide educational advantages for novices and trainees improving their learning curve under the limitation of practical opportunities.1 These 3-D-positive effects have also allowed the use of instruments in more complex procedures within small working spaces such as robot-assisted surgeries1, 3 and, hence, clinical application to endoluminal interventions can be expected, representative of endoscopic submucosal dissection (ESD).4 However, for purely endoscopic diagnostic application using excised ESD specimens, there is little information using flexible endoscopes with 3-D imaging.5 More recently, in an ex vivo study using a flexible upper gastrointestinal endoscope produced by Olympus Co. (Tokyo, Japan), Nomura et al.2 demonstrated the superiority of 3-D versus 2-D imaging in diagnostic accuracy of superficial gastric tumors with special reference to extent of disease, microsurface asperity and comprehensive recognition. In particular, its utility was apparent among physicians with less experience of endoscopy, as expected. Despite further heightened expectations, differential diagnosis of gastric tumors from non-tumors also remains underscored beyond the scope of this ex vivo study aim under limited statistical power with small sample sizes.2
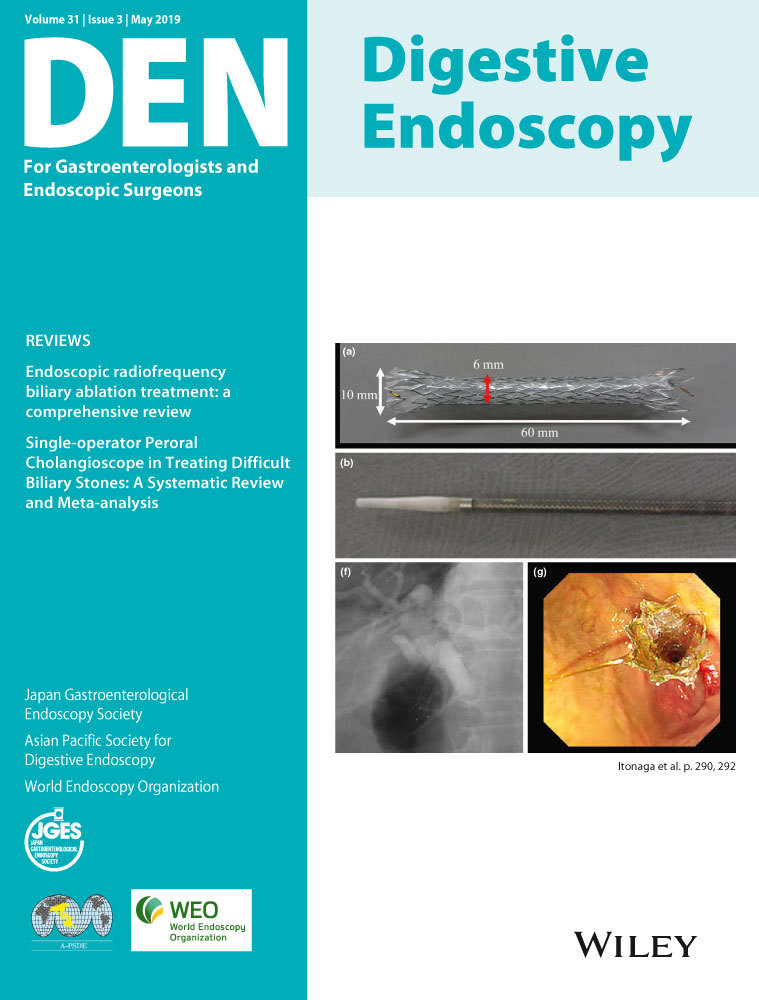
Endoscopic submucosal dissection is widely adopted as an advanced endoluminal procedure to allow en bloc resection of superficial gastrointestinal neoplasia, but is still technically challenging when using conventional endoscopes that rely solely on 2-D information, and thus lack depth appreciation.3, 4, 6 In this regard, an ex vivo study explored the feasibility of stereovision view using a 3-D flexible endoscope in the simulated setting of ESD.7 This pilot study showed that endoscopists with experience of 30 or more gastric ESD in clinical practice carried out five or more porcine gastric ESD procedures, and were then able to complete all of the procedures without any mechanical problems or perforation. Moreover, ratings of depth perception and stability were recorded on a 100-mm visual analog scale, and all of the participants reported a greater sense of security under 3-D than 2-D visualization.7 In the first part of ‘How Do I It?’ in the current issue, Chiu et al. reports a preclinical porcine model study to compare the use of the 3-D flexible endoscope (GIF-Y0083; Olympus Co.) on performance of gastric ESD between the experienced and the novice endoscopist. Virtual gastric lesions that were larger than 20 mm in size were removed in one piece by each endoscopist. Mean operative time per resected area was significantly less for the experienced than for the novice endoscopist. Procedural speed plateaued after the third ESD procedure for both the study participants,6 suggesting a potential benefit of education and training in ESD using the 3-D endoscope for novices or trainees, whereas expert trainers could compensate by converting 2-D images into stereoscopic configurations based on their skill and experience.
In the second part, endoscopists demonstrated successful translation of 3-D endoscopic technology from bench to bedside during clinical performance of ESD.6 To our knowledge, this is the first report on the clinical application of 3-D endoscopy to carry out ESD. According to case series experience conducted by one experienced endoscopist, the initial outcomes of 10 consecutive cases consisting of four gastric, two duodenal and four colorectal intramucosal neoplasia were feasible without complications, whereas ESD failed in one patient who had gastric neoplasia at anastomosis. Reason for failure was dense adhesions with oozing, which caused loss of view during the procedure.6 The 3-D endoscope was equipped with water jet function,2, 6 possibly facilitating ESD by removal of sticky mucus or blood during on-going ESD, but massive liquid collection by irrigation or arterial bleeding related to the procedure could hinder 3-D visualization.7 However, the prototype flexible 3-D endoscope equipped with narrow band imaging lacking magnifying function was useful for identifying tumor margins, and to allow clear vascular identification (i.e. penetrating arterioles), linking to pre-emptive control of hemorrhage by cautery of visible arterioles under 3-D visualization.6 Moreover, the study participant achieved better differentiation between the submucosal and the muscularis propria layer through 3-D images to avoid accidental perforation.6 In particular, 3-D images have a potentially beneficial impact on colonic ESD over flexures and haustrations. Despite only two cases of experience, the study participant felt it was more difficult to carry out duodenal rather than gastric or colorectal ESD even using a 3-D endoscope.6 Nevertheless, enhanced visual differentiation of the submucosal plane by stereovision would serve as substantially important elements for safe performance with special reference to duodenal ESD. Meanwhile, 3-D endoscopic imaging might improve procedural certainty in such advanced natural orifice transluminal endoscopic surgery as peroral endoscopic myotomy or when carrying out common or straightforward endoscopic procedures including snare polypectomy, endoscopic mucosal resection or endoscopic injection sclerotherapy through the enhancement of depth perception.7
Limitations included authors not comparing the performance of 3-D against 2-D visualization.6 Further clinical studies are necessary to evaluate the superiority of 3-D against 2-D for performance of ESD ideally in the randomized prospective way. Most studies to date, however, assessed 3-D over 2-D imaging superiority in simulated settings, not equivalently reflecting the complexity of real-life clinical conditions, even in the precedence of randomized clinical trials for laparoscopic surgery.1 The clinical impact has not yet been explored and convincing results remain to be reproduced among diverse surgical or endoluminal procedures.1 Patient-related outcomes including morbidity and mortality are the optimal goal but such studies would require enrolment of extremely high numbers of subjects undergoing ESD.
The expert participating in this first human application of 3-D ESD did not experience intolerable side-effects, whereas the nurse assistant who also wore 3-D eyeglasses and hence could experience similar 3-D information to the operator (a merit for staff education), had some motion sickness upon prolonged ESD procedure.6 In aforementioned ex vivo studies, the participants complained of eye strain or headache.2 Among subjective assessments in relation to 3-D vision technology, discomfort, dizziness, nausea and tiredness were usually listed in most simulated settings.1, 8 Additional physical side-effects including hemodynamic burden or psychomental stress requiring intensive concentration might limit general application of 3-D endoscopy,8 in particular time-consuming labored procedures. We agree with the authors’ conclusive perspective that ‘3-D ESD may not be necessary for all cases where 2-D can achieve similar safety and efficacy’,6 whereas it evidently has advantages in some situations requiring more complex tasks such as duodenal or distant colonic ESD. Next-generation 3-D flexible endoscope will be instrumented with the system capable of switching from 2-D to 3-D view upon the push of a button similar to narrow band imaging,7 albeit frequent switching between 2-D and 3-D may risk worsening nausea, eye strain or headache. More importantly, further optimization of the endoscope as for mechanical functions including thinner diameter and multi-bending maneuver can enable safe and efficacious performance throughout the overall ESD procedure or even in each process of tumor demarcation, marginal marking, cutting and dissection. Ideal instrument of a combination of 3-D flexibility under further secure depth appreciation, reversibility between 2-D and 3-D images at any time, and robotic-assistance, especially for countertraction,3, 9 can provide comfortable performance for endoscopists, ultimately minimizing complication risks even in more complex and difficult settings of this innovative treatment modality.
Authors declare no conflicts of interest for this article.